Death during sport or physical activity is a tragic and unexpected event. However, with appropriate evidence-based policies in place, death can often be prevented. The top causes of sudden death in sport and physical activity are sudden cardiac arrest (SCA), exertional heat stroke (EHS), head injuries, and exertional sickling. Studies1–3 suggest that more than 90% of sudden deaths in sport are attributable to these 4 causes, with SCA accounting for about 75% of sudden death during sport participation. Although sudden death from the aforementioned causes is not 100% preventable, the implementation of evidence-based safety policies such as emergency planning and access to automated external defibrillators (AEDs), heat acclimatization, instruction on proper tackling techniques (such as the “Heads Up Football” educational program), and sickle cell trait (SCT) screening in targeted populations can dramatically reduce overall risk. American football presents a unique risk profile for head injuries, EHS, and exertional sickling, which have driven many of the policy changes, but best practices for sport safety and emergency planning are relevant across all sports.
In 2012, the National Athletic Trainers' Association (NATA) released a position statement on the prevention of sudden death in athletes.4 Similarly, in 2013, the NATA released an interassociation task force document on preventing sudden death, specifically in the secondary school setting.5 The purposes of these documents were to provide evidence-based minimum best-practice recommendations to prevent, recognize, and treat the leading causes of death in sport and physical activity. To further focus efforts on preventing sudden death in the secondary school setting, the NATA, along with the American Medical Society for Sports Medicine and the Korey Stringer Institute, held the first annual “Collaborative Solutions for Safety in Sports” meeting in March 2015, at which a representative from each state's secondary school athletics association and a representative from each state's sports medicine advisory committee convened to discuss sport safety best practices and policy changes relevant to secondary school athletics. The second annual meeting in March 2016 will continue to provide state representatives with information and guidance for implementing evidence-based policies to protect their student-athletes.
HEAT ACCLIMATIZATION: AN EXAMPLE OF POLICY CHANGE THAT WORKS
In 2003, the National Collegiate Athletic Association (NCAA) implemented heat-acclimatization policies for preseason August football practices, requiring the phasing in of both activity and protective equipment during the hottest portion of the calendar year, when student-athletes are at highest risk of suffering EHS. Before heat-acclimatization policies were implemented, 1 or 2 EHS-related deaths occurred in NCAA student-athletes during August practices each year.1 Implementation of heat acclimatization at the collegiate level has been hugely successful, reducing the total number of August EHS-related deaths to just 1 (total) since the 2003 policy- enactment date, a 95% reduction. This simple policy change that cost no money to implement has spared the life of an estimated 20 collegiate football players and has also likely reduced the number of instances in which an athlete survived EHS but had long-term complications. The NCAA heat-acclimatization policy is a great example of a policy change that can make a difference in student-athlete safety.
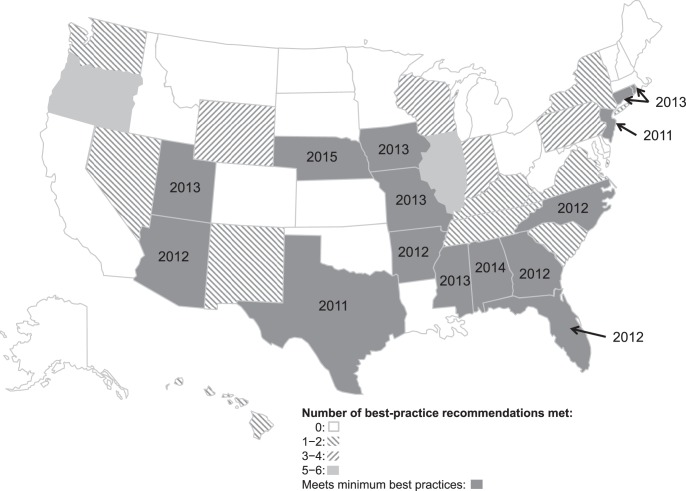
Casa et al,6 in 2009, published heat-acclimatization guidelines specific to high school athletes in an effort to reduce the number of deaths from EHS. Since 2011, 15 states have adopted heat-acclimatization policies as mandated by each state's high school athletics association (Figure). During high school preseason practices from 1980 to 2015 (a total of 488 preseasons), 22 of the 44 EHS deaths occurred in these 15 states before implementation of heat-acclimatization policies. Since implementation (a total of 50 preseasons), no student-athletes have died of EHS in these 15 states when schools followed the mandated heat-acclimatization guidelines. However, there was an EHS death at a Florida school in violation of state-mandated heat-acclimatization policies, thus emphasizing the importance of (1) implementing evidence-based heat-acclimatization policies for preseason practices and (2) complying with these policies to mitigate risk.7
Figure. .
Map of the United States portraying those states meeting evidence-based minimum best practices for heat acclimatization.1 States in gray correspond to those with mandated heat-acclimatization policies for preseason practices and the year in which this policy was mandated. The remaining meet less than the minimum best practices as shown; the total number of recommendations is 7.
SICKLE CELL TRAIT SCREENING LEADS TO INCREASED AWARENESS
In NCAA Division I collegiate football, the leading cause of death during training in the past decade has been an exertional sickling event in those with SCT.8 Division I collegiate football players with SCT are 37 times more likely to die during exertion than those without SCT.8 In response to an exertional sickling-related death of an athlete in 2006, the NCAA enacted a bylaw beginning August 1, 2010, at the Division I level, requiring all institutions to offer SCT identification through either screening or documentation of prior screening in all student-athletes. During the 2000–2001 through 2009–2010 academic years, 10 of 21 Division I collegiate nontraumatic football deaths were attributed to an exertional sickling episode (an average of 1.0 deaths/year).9 During the 2010–2011 through 2014–2015 academic years, nontraumatic exertional sickling-related deaths were significantly reduced, with only 1 of 14 deaths attributed to an exertional sickling episode. This suggests that a policy change fostering knowledge of SCT status in high-risk athletes, coupled with targeted education and tailored precautions, should be considered at other collegiate levels to reduce the risk of sudden death during participation for athletes with SCT.9
NO DEBATE: AEDS SAVE LIVES
Sudden cardiac arrest is the leading cause of sudden death in young athletes during sport and physical activity.10 Early recognition, early cardiopulmonary resuscitation (CPR), and prompt defibrillation are the key factors responsible for increasing survival after SCA. Survival rates decrease approximately 10% for each minute defibrillation is delayed,11 and prior researchers12–16 demonstrated an increase in survival when the time to defibrillation was minimized. Current consensus standards5,17,18 for emergency preparedness in school and athletic settings recommend that an AED be readily available for use within 1–3 minutes to optimize the chance of survival after SCA. In a study14 of SCA on high school campuses, 89% of student-athletes who sustained SCA during exercise survived with prompt recognition and treatment. Thus, SCA in competitive athletes is largely a survivable event through immediate recognition, early CPR, and access to an AED, preferably within 1 minute.
For any athlete who has collapsed and is unresponsive, SCA should be assumed and the emergency action plan activated.7 Critical aspects of a comprehensive policy pertaining to SCA are (1) in every sport venue, easy access to an AED that can be retrieved and used within 1–3 minutes; (2) training of all medical staff, coaches, and other appropriate personnel in CPR and AED use and the location of AEDs; and (3) a sport-specific emergency action plan outlining the emergency response to an athlete or spectator who has collapsed that is rehearsed at least annually by all relevant persons and potential first responders.
THE CHALLENGE OF REDUCING HEAD INJURIES IN SPORT
With increasing scrutiny over head injuries and concussions in football players, steps have been and are currently being taken to address this concern through both education and practice modification. Recent research19 has shown the benefits of proper tackling education to reduce overall head impacts during American football. In addition, USA Football, the governing body for youth football, has been at the forefront of these efforts, launching its “Heads Up Football” program in 2012. The program was created with 6 pillars, or educational components, addressing tackling and blocking techniques, equipment fitting, and reducing player contact during practice, as well as SCA, exertional heat illness, and concussion.20
Recent investigators21 examining injury rates in American youth football found a decline in all injuries, including concussion, when the “Heads Up Football” program and contact restrictions during practice were implemented. Injury rates during practices and games were significantly lower when both coaching education was provided and contact restrictions were enforced (0.97/1000 and 3.42/1000 athlete-exposures [AEs], respectively) compared with coaching education alone (2.42/1000 and 13.76/1000 AEs, respectively) or no coaching education or contact restrictions (7.32/1000 and 13.42/1000 AEs, respectively). When the authors examined types of injuries, coaching education and contact restrictions resulted in fewer injuries of all types, including concussions, than the other 2 groups. Establishing programs that offer proper education to coaches, players, and parents and implementing proper technique can create a safer environment for athletes at all levels.
THE PATH FORWARD
Although sudden death in sport cannot be completely prevented, establishing policies that conform to evidence-based best practices will reduce the overall risk of death and catastrophic injury. Medical professionals (eg, athletic trainers, physicians) should continue to work in conjunction with governing bodies—state high school athletics associations, the National Federation of State High School Associations, and youth sport governing bodies—to develop and implement appropriate policies for athletes at all levels of sport.
REFERENCES
- 1. Boden BP, Breit I, Beachler JA, Williams A, Mueller FO. Fatalities in high school and college football players. Am J Sports Med. 2013; 41 5: 1108– 1116. [DOI] [PubMed] [Google Scholar]
- 2. Reports. National Center for Catastrophic Sport Injury Research Web site. http://nccsir.unc.edu/reports. Accessed February 7, 2016. [Google Scholar]
- 3. Harmon KG, Asif IM, Maleszewski JJ, et al. Incidence, cause, and comparative frequency of sudden cardiac death in National Collegiate Athletic Association athletes: a decade in review. Circulation. 2015; 132 1: 10– 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Casa DJ, Guskiewicz KM, Anderson SA, et al. National Athletic Trainers' Association position statement: preventing sudden death in sports. J Athl Train. 2012; 47 1: 96– 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Casa DJ, Almquist J, Anderson SA, et al. The Inter-Association Task Force for Preventing Sudden Death in Secondary School Athletics Programs: best-practices recommendations. J Athl Train. 2013; 48 4: 546– 553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Casa DJ, Csillan D. Inter-Association Task Force for Preseason Secondary School Athletics Participants, et al. Preseason heat-acclimatization guidelines for secondary school athletics. J Athl Train. 2009; 44 3: 332– 333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Attanasio SM, Adams WM, Stearns RL, Huggins RA, Casa DJ. Occurrence of exertional heat stroke in high school football athletes before and after implementation of evidence-based heat acclimatization guidelines [abstract]. J Athl Train. In press. [Google Scholar]
- 8. Harmon KG, Drezner JA, Klossner D, Asif IM. Sickle cell trait associated with a RR of death of 37 times in National Collegiate Athletic Association football athletes: a database with 2 million athlete-years as the denominator. Br J Sports Med. 2012; 46 5: 325– 330. [DOI] [PubMed] [Google Scholar]
- 9. Adams WM, Huggins RA, Stearns RL, Anderson SA, Kucera KL, Casa DJ. Policy changes reduce exertional sickling related deaths in Division I collegiate football players [abstract]. J Athl Train. In press. [Google Scholar]
- 10. Harmon KG, Drezner JA, Wilson MG, Sharma S. Incidence of sudden cardiac death in athletes: a state-of-the-art review. Heart. 2014; 100 16: 1227– 1234. [DOI] [PubMed] [Google Scholar]
- 11. Larsen MP, Eisenberg MS, , Cummins RO, Hallstrom AP. Predicting survival from out-of-hospital cardiac arrest: a graphic model. Ann Emerg Med. 1993; 22 11: 1652– 1658. [DOI] [PubMed] [Google Scholar]
- 12. Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002; 347 16: 1242– 1247. [DOI] [PubMed] [Google Scholar]
- 13. Hallstrom AP, Ornato JP, Weisfeldt M, et al. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004; 351 7: 637– 646. [DOI] [PubMed] [Google Scholar]
- 14. Toresdahl BG, Harmon KG, Drezner JA. High school automated external defibrillator programs as markers of emergency preparedness for sudden cardiac arrest. J Athl Train. 2013; 48 2: 242– 247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Drezner JA, Rao AL, Heistand J, Bloomingdale MK, Harmon KG. Effectiveness of emergency response planning for sudden cardiac arrest in United States high schools with automated external defibrillators. Circulation. 2009; 120 6: 518– 525. [DOI] [PubMed] [Google Scholar]
- 16. Drezner JA, Toresdahl BG, Rao AL, Huszti E, Harmon KG. Outcomes from sudden cardiac arrest in US high schools: a 2-year prospective study from the National Registry for AED Use in Sports. Br J Sports Med. 2013; 47 18: 1179– 1183. [DOI] [PubMed] [Google Scholar]
- 17. Drezner JA, Courson RW, Roberts WO, Mosesso VN, Link MS, , Maron BJ. Inter-association task force recommendations on emergency preparedness and management of sudden cardiac arrest in high school and college athletic programs: a consensus statement. J Athl Train. 2007; 42 1: 143– 158. [PMC free article] [PubMed] [Google Scholar]
- 18. Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care: part 4. The automated external defibrillator: key link in the chain of survival. The American Heart Association in Collaboration with the International Liaison Committee on Resuscitation. Circulation. 2000; 102 suppl 8: I60– I76. [PubMed] [Google Scholar]
- 19. Swartz EE, Broglio SP, Cook SB, et al. Early results of a helmetless-tackling intervention to decrease head impacts in football players. J Athl Train. 2015; 50 12: 1219– 1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Heads Up Football; 2012. USA Football Web site. http://usafootball.com/headsup?gclid=COaRt7WmgcoCFYQfHwods6UJXw. Accessed December 29, 2015. [Google Scholar]
- 21. Kerr ZY, Yeargin S. Valovich McLeod TC, et al. Comprehensive coach education and practice contact restriction guidelines result in lower injury rates in youth American football. Orthop J Sports Med. 2015; 3 7: 2325967115594578. [DOI] [PMC free article] [PubMed] [Google Scholar]