Abstract
Background
Older adults are at risk for greater chronic stress and cognitive decline. Mindfulness meditation training may help reduce stress and thus cognitive decline in older adults, but little research has explored this.
Objective
The primary aim was to evaluate the feasibility and acceptability of an internet mindfulness meditation intervention and an internet health and wellness education program for a sample of older adults (65–90 years old). The secondary aims were to collect preliminary pre-post data on mood and cognitive function.
Design and Setting
Baseline and endpoint assessments occurred in participants’ homes. Participants were randomized to the meditation or education program taught how to access and complete their allocated intervention at their home.
Participants
16 participants completed the study (8 receiving each intervention), and five dropped out (76% completion rate). Mean age was 76.2, 88% Caucasian, 50% Female.
Intervention
Both the meditation and education interventions had a one-hour online session each week for six weeks with 30 minutes daily home practice.
Primary Outcome Measures
Feasibility and acceptability were measured through adherence and a Client Satisfaction Questionnaire. Mood and cognitive outcomes were evaluated before and after the interventions.
Results
Of 21 people enrolled, 16 participants completed the study with 8 in each arm (76% completion rate). There were no significant between-arm differences on important demographic and other characteristics. Acceptability was high for the interventions based on above average scores on the Client Satisfaction Questionnaire. The IMMI participants completed 4.25 ± 2.4 sessions (range 0–6), 604 ± 506 (range 0–1432) home practice minutes, and 21.3 ± 15.5 days of practice (range 0–46). The Education participants completed an average of 4.75 ± 1.8 sessions (range 2–6), 873 ± 395 (range 327–1524) home practice minutes and 25.6 days of practice (range 11–35). Feasibility of the intervention formats and appropriateness of the control group was demonstrated. As expected due to the pilot nature of the study, there were no group differences on mood or cognitive outcomes.
Conclusions
Administering interventions via the internet to older adults is feasible. The two interventions were acceptable and equal in regards to perceived credibility and acceptability. Future randomized controlled trials are planned to evaluate the clinical efficacy of these two interventions.
Keywords: internet, meditation, older adults, stress
Introduction
Psychological stress contributes to age-related cognitive decline. Psychological health affects health in general and the brain specifically. Chronic psychological stress contributes to cognitive decline, hippocampal injury, and neurodegenerative diseases either directly or through stress mediators.1–7 The negative effect of psychological stress on cognitive function may be greater with aging.8–11 Older adults have less physiological reserves and are more likely to be affected by stress.8–10 Results from a recent study examining the health of older adults documents increased rates of chronic disease with the likelihood of increased health care needs and costs compared to previous generations.12
Mindfulness meditation (MM) aims to help modify individuals’ stress responses. Clinical research studies show that group MM is effective for stress and mood improvement,13,14 and it may be effective for offsetting normal age-related cognitive decline or even improving certain aspects of cognition in older adults.15 In general, MM is an attractive intervention because of the relatively low cost, low physical and emotional risk, ease of implementation, and potential for empowering patients to take a more active role in their treatment.16 MM interventions (MMI) consistently improve a spectrum of mental health measures,17 including anxiety,18,19 sleep disturbances,20 stress,21 and chronic pain.22 MMI have been used in older adults and have also been shown to improve cognition.15,23–25 Easily accessible interventions that can be used by older adults to improve health and well-being are needed and are an important public health issue.26
For older adults who are interested in learning MM, traditional group formats may be a barrier to care, and shorter individual or internet interventions may be preferred. The most commonly used interventions, Mindfulness-Based Stress Reduction and Mindfulness-Based Cognitive Therapy,27,28 are taught in a group setting and are time intensive (both include a two-hour class once a week for eight weeks, as well as daily home practice). This standardized group format may be problematic for people with sensitive diagnoses, aversions to public sharing, or limited ability to attend a class because of distance or access to transportation. Others, for whom local groups are simply not available, may also benefit from non-group formats.29 The best way to administer MMI is uncertain, and preferences vary from one individual to the next. An online survey about format preferences for MMI suggested that older adults may prefer individual or internet interventions rather than groups. Of 500 survey participants, 44 were older adults between the ages of 60 and 90 years. Within this subset, internet was rated as the first-choice format (Internet 43%, Individual 39%, Group 15%), and 10% of participants said they would refuse a group format.30 While the online administration of this survey could bias the results, the data lend support for evaluating internet delivery formats.
Background
Little is known of alternative formats for MMI. Brief clinical cases of individual delivery applications have been reported,30,31 and internet programs are just beginning to be studied. Beginning studies have demonstrated a reduction in a variety of outcomes including anxiety, depression, insomnia, stress, and improvement in mindfulness, self-transcendence, and psychological well-being in mostly controlled trials with no adverse events.32–35 Feasibility and efficacy has also been established in distressed cancer survivors.36 The present study builds on this previous research on online MMI and applies it to older adults, asking whether online delivery is feasible and acceptable for adults 65–90 years of age.
The internet MMI used in this project is modeled after Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction, two standardized, well-studied, 8-week group programs that have strong evidence for their effectiveness.14 The online MMI used in this study was developed from a series of modifications, beginning with an abbreviated group format, progressing to a one-on-one intervention, and then resulting in an online version, called IMMI (Internet Mindfulness Meditation Intervention). The group and one-on-one interventions were six weeks in length, with weekly 90-minute trainings and daily home practice of approximately 45 minutes. The group format was utilized in a RCT of 31 caregivers of family members with dementia (mean age 63), in which MM was compared with both active and passive controls— an education group and a respite care-only group. Analyses of cognitive measures yielded significant differences between the group MMI and the active control arm.25 In an effort to improve recruitment and retention, as well as remove the social aspect that potentially confounds efficacy evaluation, a one-on-one format of the same MMI was developed and implemented in an ongoing RCT that demonstrated significant improvement in stress-related questionnaires.30,37 IMMI used in the present study was developed to be as similar as possible to the one-on-one MMI.
The primary aim of this pilot randomized controlled study was to evaluate the feasibility and acceptability of IMMI and an internet health and wellness education program for a sample of older adults (65–90 years old). The secondary aims were to collect preliminary data on mood and cognitive function before and after the two interventions. Mood and mood-related outcomes collected for this trial were depression symptoms, positive and negative affect, perceived stress, and sleep quality because of their potential sensitivity to mindfulness in this population and interaction with mood and chronic stress and also to collect preliminary data on them for a larger clinical trial.38 Similarly, cognitive measures of executive function, attention, working and verbal memory, and reaction time were chosen as outcomes for the study. We hypothesized that IMMI would be feasible and acceptable. Due to the small sample size and pilot nature of the study, we expected no differences between arms on mood and cognition outcomes (the data collected in this pilot study will be used to conduct sample size and power calculations for a future clinical trial).
Methods
Participants
Older adults aged 65–90 years old were recruited from the Portland, Oregon, Metropolitan Area through an informational talk and flyers at a retirement community, flyers posted at OHSU and older adult community locations, and referrals by OHSU physicians. Participants who expressed interest underwent a telephone screening, which included a script that described the study procedures, as well as questions to determine eligibility. Broad inclusion criteria were used to aide in recruitment and maximize the generalizability and public health relevance of the study. Exclusion criteria were minimized and based primarily on screening out participants with an underlying illness that may limit the benefit of the intervention, confound outcomes, or increase the likelihood of dropout. Inclusion criteria were as follows: at least somewhat stressed (≥ 9 on the Perceived Stress Scale (PSS);39 stable on medications six weeks prior to and during study; willing to learn to learn and use study technology; able to hear and understand instructions; willing to accept randomization scheme and agree to follow the study protocol; cognitively able to give consent and follow the protocol (≥26 on the Modified Telephone Interview of Cognitive Status (mTICS);40 no acute medical illness that would decrease likelihood of study completion such as person with current cancer diagnosis undergoing chemotherapy (subjective); no significant, untreated depression, as assessed by Center for Epidemiologic Studies Depression Scale (CESD-5)41 >16 and interview; and no current daily meditation practice (≥5 min/day daily for at least 30 days in the last 6 months).
Procedures
In general, participants had a telephone screening, a Baseline Visit, a 6-week intervention period, and an Endpoint Visit. The study was approved through the Oregon Health & Science University Institutional Review Board and all participants signed informed consent forms.
Screening
Telephone screenings were arranged with interested volunteers. During the call, eligibility was determined by asking questions about medical history and medications and administering the PSS, mTICS, and the CESD-5. Eligible and interested volunteers scheduled a Baseline Visit and received consent forms for review prior to their visit.
Baseline Visit
The research assistant (RA) who was blinded to condition arrived at the volunteer’s home and conducted the consenting procedure, where the purpose, procedures, risks and discomforts, benefits, confidentiality and liability of the study were explained both in writing and verbally before participants signed the consent. Inclusion and exclusion criteria were then confirmed. The participant completed subjective questionnaires on expectancy and credibility of the interventions, mood, positive and negative affect, sleep quality, perceived stress, and mindfulness. Participants then completed cognitive tasks: Simple Reaction Time, Flanker, Letter-Number Sequencing, Verbal Fluency-Letter,42 and the Rey Auditory-Verbal Learning Test (see Measures for additional details on the subjective questionnaires and cognitive tasks).
Interventions
After the Baseline Visit, participants were randomized to receive either IMMI or internet Education, which served as a time and attention control.
An RA who was unblinded to condition visited the participants’ homes and taught them how to access their allocated intervention online with either an internet-enabled iPad (Apple, Inc, Cupertino, CA) or their own computer. They explained how to log onto and complete the session online and do the home practice with both verbal and written older adult user-friendly instructions. Both interventions had 1-hour session/week for six weeks with 30 minutes daily home-practice, and the sessions included enquiry about the content delivered. Enquiry entailed questions being presented online and answered by typing answers into a text space. Participants completed sessions 2–6 on their own at their convenience. The RA called participants weekly to remind them to complete their sessions and see if they had any questions. They were given RA and principal investigator phone numbers if they needed any assistance with technology or content.
IMMI
IMMI is a standardized and structured program based on Mindfulness Based Cognitive Therapy and Mindfulness Based Stress Reduction28,43 and has been piloted in our laboratory.44 IMMI’s objectives were to 1) help participants understand their personal reactions to stress, 2) teach them skills to modify their stress reactions, and 3) promote their desire for self-care and feelings of competence and mastery. Each session included 1) didactic instruction and discussion on stress, relaxation, meditation, and mind-body interaction, 2) instruction and practice in formal and informal MM, and 3) enquiry about problem-solving techniques regarding success and difficulty in practicing mindfulness (see Wahbeh, 2012 for full curriculum).44 Formal meditation instruction included a mindful Body Scan and Sitting Meditation (awareness of breath, body sensations, cognitive and emotional processes). Informal practice of mindful daily activities (e.g., washing dishes) was also taught to generalize mindfulness beyond the formal meditations. A 3-minute meditation was offered as a quick coping strategy, and it could be practiced with or without a guided recording.
Internet Education Control
The Education control was matched for session time and home practice. The internet sessions included a general health video and questions about the material. For home practice, the participants listened to podcasts about the same topic. The session topics were 1) Healthy Eating, 2) Healthy Exercise, 3) Healthy Sleep, 4) Healthy Brain, 5) Healthy Mood, and 6) Community Involvement.
Adherence
Participant adherence was measured by session completion, subjective home-practice logs, and objective iMINDr data. iMINDr is a custom software application for use with an iPod Touch (Apple, Inc., Cupertino, CA) to accurately track home-practice adherence.45 iMINDr collects all actions performed (date, time, action [start, stop, pause, volume change]). Participants were trained on iMINDr, which was installed on the study iPad or iPod Touch at their first session with verbal and graphical instruction. Adherence was defined as session attendance (online training completion), the number of home-practice days (frequency), and the average practice time per day (duration).
Endpoint Visit
After the six-week intervention period, the RA who was blinded to condition visited the participant’s home to complete the Endpoint Visit, which proceeded in the same manner as the Baseline Visit. In addition, participants completed a satisfaction questionnaire. All participants received a CD with the study guided meditations on it after the study was complete, regardless of randomization.
Measures
The outcomes used in this study are widely used, validated, and sensitive to stress and/or MM.
Subjective questionnaires in alphabetical order.
Center for Epidemiologic Studies Depression Scale (CESD)
Depression was assessed during the screening procedure with a 5-item subset of the original 20-item scale (CESD-5). The CESD-5 raw score was multiplied by 4 for cutoff score criteria determination. The CESD-5 has demonstrated very good sensitivity (>0.84), specificity (≥0.80), and high validity (>0.90) for in identifying patients classified as depressed by the full 20-item scale.46 The full version was used to evaluate depression symptoms at the Baseline and Endpoint Visits. The CESD is a commonly used subjective measure of depressive symptoms. It asks participants about how they felt or behaved in the past week, yielding global scores ranging from 0–60, with higher scores indicating greater depression.47
Client Satisfaction Questionnaire (CSQ-8)
The eight-item Client Satisfaction Questionnaire (CSQ)48 was administered at the Endpoint Visit. It is an 8-item questionnaire used to assess satisfaction with the intervention. The questionnaire has demonstrated high internal consistency (α = .93) and strong construct validity, evidenced by correlation with service utilization and clinical outcomes.48
Credibility/Expectancy Questionnaire
The Credibility/Expectancy Questionnaire is a standardized instrument that assesses participant intervention expectancy and rationale credibility in clinical outcome studies.49 The wording was minimally modified to assess attitudes towards the mindfulness and education interventions. The scale has a high internal consistency (α = .84) and good test-retest reliability (.75 credibility; .82 expectancy). Expectancy assessment is essential in controlled intervention studies.50
Five-Facet Mindfulness Questionnaire (FFMQ)
Mindfulness was measured with the FFMQ, which assess five elements of a general tendency to be mindful in daily living: observing, describing, acting with awareness, nonjudging of inner experience, and nonreactivity to inner experience.51 The questionnaire presents a series of 39 statements and asks participants to respond according to “what is generally true for you” using a Likert scale ranging from 1 (never or very rarely true) to 5 (very often or always true). The five facets can be combined to yield a composite score that reflects a global measure of mindfulness.
Positive and Negative Affect Schedule (PANAS)
Positive and negative affect was measured with the PANAS, a 20-item subjective instrument that measures affect.52 The survey is composed of 10 words that represent positive feelings (i.e. inspired, determined) and 10 words that represent negative feelings (i.e. hostile, nervous). Participants are asked to indicate the extent to which they “generally feel this way” or “feel on average” using a Likert scale. A composite score between 10 and 50 is generated for both positive and negative affect, with higher numbers indicating more of that affect.
Pittsburgh Sleep Quality Index (PSQI)
Sleep quality and disturbances in a one-month time span was measured with this instrument with 19 items that yield seven component scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction.53 The global score ranges from 0 to 21, with higher scores indicating greater difficulty in all areas. Sleep quality suffers with chronic stress and is known to affect health and also be improved by mind-body interventions such as mindfulness meditation.38
Perceived Stress Scale (PSS)
Perceived stress was measured using the PSS, a commonly used 10-item subjective instrument that measures respondents’ perceived stress in the past week.39 It has good internal reliability (α = .76) and strong construct validity. The global score ranges from 0 to 36, with higher scores indicating greater perceived stress.
The cognitive tasks administered in alphabetical order. The cognitive tasks were administered to collect preliminary data on effect of mindfulness meditation on cognitive function in older adults.
Auditory-Verbal Learning Test (AVLT)
The AVLT evaluates verbal memory in adult patients. For trial 1, the examiner reads a list of 15 words. The participants then say back as many words as they remember. The list is then reread for trial 2–5. The examiner reads a different list of 15 words and asks participants to repeat back as many as they remember. For trial 6, the examiner repeats the first list of 15 words and asks the participants to repeat back as many as they can remember. The score for each trial is the number of words correctly recalled. A total score is the sum of trials 1–6. Thirty minutes after administration of the lists, the participant is asked if they recall any of the words from the list for a delay retention score (delay recall/trial 5 recall). A different list was used for Baseline and Endpoint to reduce the learning effect.54
Controlled Oral Word Association (COWA)
Participants were given a letter and asked to say as many words as they can think of that start with that letter in one minute (Baseline- FAS; Endpoint- CFL).55
Flanker Task (FT)
The FT yields reliable estimates of executive function, and thus frontal cortex activity, because the task requires inhibition of a response to distracting stimuli. The participant views a monitor and presses a button to report the direction of the middle of five arrows when they see an image flash on the screen. The images consist of arrows either all facing the same (congruent) or different (incongruent) directions. The conflict effect score is indexed by subtracting performance measures on congruent target trials from those on incongruent target trials. The result of the paired subtraction is the conflict effect score. Thus, a lower score represents increased frontal cortex activity and has been reported in detail.56
Letter-Number Sequencing (LNS)
The LNS measures working memory and is a scale in the Wechsler Memory Scale-III. The examiner presents combinations of letters and numbers, from 2 to nine letter-number combinations. The participant repeats each series by, first, repeating the numbers in ascending order, then the letters in alphabetical order (e.g., 9-L-2-A; correct response is 2-9-A-L).57
Simple Reaction-Time Task
In the Simple Reaction Time Task, participants were instructed to respond to a circle stimulus presented at the center of the screen. Participants were asked to maintain fixation and respond as quickly as possible with a button press when they saw the circle flash on the screen.
Statistical Analysis
Power calculations were not conducted for this pilot study, as the data collected from it will be used to inform sample size estimation and power analysis for a future clinical trial. Sample size was determined by available resources. Missing data was addressed at the participant level to minimize attrition and incomplete data. Participants were considered “dropouts” if they completed fewer than half of the sessions (<3/6) and missed the Endpoint Visit.58 The study continued until there were eight completers in each arm. As with most mind-body interventions, traditional double-blinding was not feasible. The RA who conducted the outcome assessments was blinded to participant intervention assignment. The RA teaching participants how to access the intervention and PI were unblended to condition. The RA who was unblinded to condition implemented the randomization and informed participants of their assignments. Randomization was conducted by the RA unblinded to allocation with a dynamic randomization approach to help ensure that there were eight completers in each arm and that the arms were matched on age, gender, and depression score, and to reduce selection bias.59,60
Participant characteristics at baseline were assessed with the χ2 test for discrete variables or the two-sample Kruskall-Wallis test for non-normally distributed data. Feasibility data was evaluated in a descriptive fashion (e.g. recruitment rates and drop-outs). The Client Satisfaction Questionnaire was qualitatively reviewed for participant acceptability, and group differences on this measure were assessed with Kruskall-Wallis test. Preliminary evaluation of outcomes was evaluated with the Kruskall-Wallis test assuming non-normally distributed data. Analysis was conducted on the completer cohort. Since the pilot study is not powered to assess differences between groups, these evaluations were exploratory and provided data to perform power analyses and sample size estimation for a larger clinical trial. Statistical analyses use SPSS 20.0 (IBM, USA) and STATA 12.0 (Statacorp, LP, USA).
RESULTS
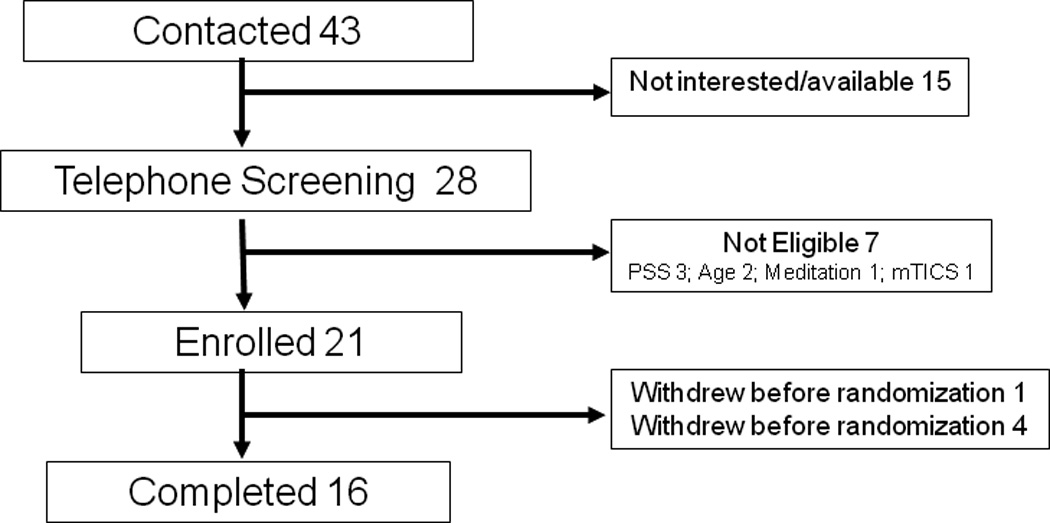
Twenty-one participants were consented and enrolled. One participant dropped out before randomization. Four participants dropped out after randomization. (Three participants were randomized to IMMI and one was randomized to Education. All four dropped out before the end of the first intervention visit.) All five drop outs stated that once they understood and contemplated all the study activities, they realized they did not have the time to commit to the study (Figure 1). There was no difference in age, gender, education, marital status, socioeconomic status, depression symptoms, levels of stress, or cognitive function between those that dropped out and participants who completed the study. Participants reported no adverse events or side effects from either intervention.
Figure 1.
Sixteen participants were randomized and completed the study—eight in the Education arm and eight in the IMMI arm. There was also no difference in age, gender, education, marital status, socioeconomic status, depression symptoms, levels of stress, or cognitive function between the Education and IMMI arms (all p’s <0.05). Participants’ mean age was 76.2 ± 7.4 years, and they had an average of 18 years ± 3 of education. They were 88% Caucasian, 50% Female, and 69% Married or in Domestic Partnership, and there were a wide range of socioeconomic statuses (annual household income before taxes [$15,000–29,999 (1); $30,000–44,999 (4); $45,000–59,999 (3); $60,000–74,999 (1), $75,000–89,999 (2); $90,000 or higher (5)]. At baseline, there was no difference between arms on depression symptoms (CESD), perceived stress (PSS), or cognitive status (mTICS) (Table 1). Perceptions of credibility and expectancy of each training was the same for participants in both arms before randomization (all p’s >0.33).
Table 1.
Baseline characteristics of participants. There were no differences between arms on these important variables.
| IMMI n=8 Mean (sd) |
Education n=8 Mean (sd) |
|
|---|---|---|
| CESD | 8.0 (3.7) | 8.5 (6.6) |
| PSS | 10.8 (3.9) | 13.6 (5.5) |
| mTICS | 36.9 (2.6) | 38.4 (4.4) |
| Age | 76.9 (9.0) | 75.5 (5.6) |
| Education | 18.9 (2.4) | 16.6 (2.5) |
CESD-Center for Epidemiologic Studies Depression Scale; PSS- Perceived Stress Scale, mTICS-modified Telephone Interview for Cognitive Status.
The IMMI participants completed 4.25 ± 2.4 sessions (range 0–6), 604 ± 506 (range 0–1432) home practice minutes, and 21.3 ± 15.5 days of practice (range 0–46). The Education participants completed an average of 4.75 ± 1.8 sessions (range 2–6), 873 ± 395 (range 327–1524) home practice minutes and 25.6 days of practice (range 11–35). There were no differences between arms on session or home practice adherence (p’s>0.30).
The participants found both interventions acceptable (Table 2). On average, participants in the IMMI arm rated the intervention higher on each question than participants in the Education arm. There were no significant differences between arms on each question (all p’s>0.16).
Table 2.
Client Satisfaction Questionnaire results by question. Each question on the CSQ is listed here with the range of answer choice on the Likert Scale. There were no significant differences between arms on each question.
| Question and scale of answer | IMMI n=8 Mean (sd) |
Educ n=8 Mean (sd) |
|---|---|---|
| 1. How would you rate the quality of service you received in the study? | 3.6 (0.5) | 3.3 (0.7) |
| Excellent -4 → Poor -1 | X2(1) =0.99; p=0.32 | |
| 2. Did you get the kind of service you wanted? | 3.6 (0.5) | 3.6 (0.5) |
| No, definitely not -1 → Yes, definitely -4 | X2(1) =0.03; p=0.86 | |
| 3. To what extent has our study met your needs? | 2.9 (0.6) | 2.3 (1.0) |
| Almost all of my needs have been met -4 → None of my needs have been met -1 | X2(1) =1.93; p=0.16 | |
| 4. If a friend were in need of similar help, would you recommend our study to him? |
3.4 (1.1) | 2.7 (1.3) |
| No, definitely no -1 → Yes, definitely -4 | X2(1) =1.3; p=0.25 | |
| 5. How satisfied are you with the amount of help you received? | 3.6 (0.5) | 3.4 (0.7) |
| Quite dissatisfied -1 → Very satisfied -4 | X2(1) =0.33; p=0.56 | |
| 6. Have the services you received helped you to deal more effectively with your problems? |
3.4 (0.7) | 3.0 (0.8) |
| Yes, they helped a great deal -4 → No, they seemed to make things worse -1 | X2(1) =0.75; p=0.38 | |
| 7. In an overall, general sense, how satisfied are you with the service you received? |
3.5 (0.5) | 2.9 (1.1) |
| Very satisfied -4 → Quite dissastisfied -1 | X2(1) =1.1; p=0.29 | |
| 8. If you were to seek help again, would you come back to the study? | 3.0 (1.1) | 2.3 (1.1) |
| No, definitely not -1 → Yes, definitely -4 | X2(1) =1.5; p=0.22 | |
Mood and related outcomes were evaluated before and after the interventions. As expected, there were no differences between arms on the depression symptoms, positive and negative affect, perceived stress, and sleep quality (all p’s>0.32; Table 3). Interestingly the mindfulness total score increased for both arms, although the differences between arms was not significant (X2(1) =1.0; p=0.32).
Table 3.
Mood and related measures. Mean values and standard deviations are listed by arm on mood and related outcomes evaluated before and after intervention.
| IMMI | Education | |||
|---|---|---|---|---|
| Before Mean (sd) |
After Mean (sd) |
Before Mean (sd) |
After Mean (sd) |
|
| CESD | 6.3 (6.0) | 6.6 (5.0) | 6.8 (5.1) | 5.8 (7.5) |
| PANAS_P | 36.6 (6.8) | 33.8 (7.1) | 36.9 (6.6) | 35.5 (5.7) |
| PANAS_N | 13.8 (6.6) | 14.1 (4.3) | 13.6 (4.2) | 16.4 (9.0) |
| PSS | 11.0 (7.0) | 14.4 (4.6) | 10.9 (3.4) | 14.4 (6.3) |
| PSQI | 6.9 (5.0) | 7.6 (6.4) | 6.1 (4.9) | 6.4 (3.3) |
| Mindfulness | 134.8 (20.9) | 145.1 (19.7) | 136.4 (20.6) | 146.9 (22.1) |
CESD-Center for Epidemiologic Studies Depression Scale; PANAS-Positive and Negative Affect Scale; PSS- Perceived Stress Scale; PSQI-Pittsburgh Sleep Quality Index.
Cognition and related outcomes were evaluated before and after the intervention. As expected, there were no significant differences between arms on the Simple Reaction Time, Flanker Task Conflict Effect Score, Letter Number Sequencing, Verbal Fluency (letter), or the AVLT (all p’s>0.20; Table 4).
Table 4.
Cognition and related measures. Mean values and standard deviations are listed by arm on cognition and related outcomes evaluated before and after intervention.
| IMMI | Education | |||
|---|---|---|---|---|
| Before Mean (sd) |
After Mean (sd) |
Before Mean (sd) |
After Mean (sd) |
|
| Simple Reaction time | 366.9 (64.2) | 379.4 (64.2) | 351.3 (76.8) | 364.4 (78.8) |
| Flanker Task Conflict Effect | 68.4 (268.5) | −3.0 (239.1) | −34.5 (384.7) | 282.7 (280.1) |
| Letter Number Sequencing | 7.9 (2.4) | 7.8 (2.7) | 9.5 (2.6) | 8.8 (3.1) |
| COWA | 35.6 (11.6) | 37.8 (10.3) | 42.0 (14.4) | 42.5 (13.9) |
| AVLT trial 1–5 | 37.8 (8.2) | 40.8 (9.1) | 42.5 (12.1) | 42.4 (7.6) |
| AVLT delay retention | 0.6 (0.4) | 0.6 (0.3) | 0.7 (0.2) | 1.6 (2.6) |
COWA-Controlled Oral Word Association Test; AVLT-Rey Auditory-Verbal Learning Test
DISCUSSION
The current study was a pilot study examining the feasibility and acceptability of an internet mindfulness meditation intervention for older adults and secondarily collecting preliminary data on mood and cognitive function outcomes. Recruitment was feasible, with a 76% recruitment rate. The participants who dropped out underestimated the time commitment and did not want to continue in the study. Future studies will more clearly emphasize the time commitment required during the screening process. Our randomization was effective, and the two groups were similar in important demographic and other characteristics, such as depressions symptoms, perceived stress, and cognitive status.
There was no inherent bias in participant perceptions of expectancy of the two interventions. This, along with similar credibility scores, suggests research study staff had appropriate equipoise between the interventions. Participants were also adherent to the interventions. On average, participants were compliant with completing the total number online sessions (IMMI- 71% of sessions; Education- 80% of sessions). The home practice minutes were variable but again not different between groups. All but one participant did at least some home practice. The participants also found the interventions themselves acceptable, as observed in the Client Satisfaction Questionnaire scores. Both arms reported answers on the positive side of the Likert scale for most questions. While the scores were not significantly different between arms, the IMMI participants reported more positive values on all questions. Based on this feasibility and acceptability data, it is reasonable to conduct a larger randomized controlled trial evaluating efficacy. The similar credibility and expectancy scores, as well as comparable adherence, also suggest that that the Education program as a time and attention control for the IMMI program is feasible and could be used in the larger randomized controlled trial.
The mood and related outcomes were easily collected via questionnaires. The cognitive and related outcomes were also easily administered by the research assistant at the participant’s home verbally or through the laboratory laptop computer. As expected, there were no significant differences on cognitive and mood outcomes between arms. This was a pilot study and we did not expect to see a difference. The data collected will inform future studies and allow other researchers to use the data for aggregation into meta-analysis.
There were a number of questions about the methods the research team aimed to discover through this pilot. For example, is it reasonable to expect older adults to become comfortable with the use of an iPad to access the online program? We found that iPad’s were difficult to use for many of the participants. We decided to switch to using their own desktop or laptop computers to access the online programs and installing iMindr on an iPod Touch. This combination was more amenable to the participants. Participants needing to have a desktop or laptop would then require the participants to own one and thus, be more familiar with the technology. In addition to the delivery apparatus, we found that the sessions took longer than we expected because of the text enquiry included in the online programs. Participants were not familiar with the technology and typing, and thus, typing their answers to the questions in the text boxes took a great deal longer than we expected. The programs are now revised to include multiple choice questions rather than text-box questions to shorten the length of the sessions.
This pilot study had a number of limitations that should be considered when interpreting the results. The study addressed whether an internet MMI is feasible and acceptable to older adults and collected preliminary data to inform a larger RCT. The study was not powered to definitively assess outcome differences between IMMI and the Education control. Additionally, the study was designed to assess shorter-term effects of MM (6 weeks). Ideally, a study would assess sustained effects over a longer time-period. The study used novel technology that may be difficult for the older adult to use. Future trials of this nature should require older adults to have some basic knowledge of computers and how they work and have participants access online programs through their own computers.
In conclusion, administering interventions via the internet to older adults is feasible. The IMMI and Education programs were acceptable and equal in regards to perceived credibility and acceptability. Future RCTs are planned to evaluate the efficacy of these two interventions on mood and cognitive outcomes.
Acknowledgments
The authors would like to thank Tracy Zitzelberger for their help with this project. This work was supported by the Oregon Roybal Center for Translational Research on Aging and the National Institutes of Health [Grant number P30 AG024978] and the National Center for Complementary and Alternative Medicine of the National Institutes of Health [Grant number K24AT005121]. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
There are no potential or actual conflict of interests or financial disclosures related to this work for all authors.
C. Bibliography and References Cited
- 1.Lupien SJ, Nair NP, Briere S, et al. Increased cortisol levels and impaired cognition in human aging: implication for depression and dementia in later life. Reviews in the neurosciences. 1999;10(2):117–139. doi: 10.1515/revneuro.1999.10.2.117. [DOI] [PubMed] [Google Scholar]
- 2.Sapolsky RM. Glucocorticoids, stress, and their adverse neurological effects: relevance to aging. Experimental gerontology. 1999 Sep;34(6):721–732. doi: 10.1016/s0531-5565(99)00047-9. [DOI] [PubMed] [Google Scholar]
- 3.McEwen BS. Protective and damaging effects of stress mediators. The New England journal of medicine. 1998 Jan 15;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 4.Sapolsky RM. Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders. Archives of general psychiatry. 2000 Oct;57(10):925–935. doi: 10.1001/archpsyc.57.10.925. [DOI] [PubMed] [Google Scholar]
- 5.Esch T, Stefano GB, Fricchione GL, Benson H. The role of stress in neurodegenerative diseases and mental disorders. Neuro endocrinology letters. 2002 Jun;23(3):199–208. [PubMed] [Google Scholar]
- 6.McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Hormones and behavior. 2003 Jan;43(1):2–15. doi: 10.1016/s0018-506x(02)00024-7. [DOI] [PubMed] [Google Scholar]
- 7.Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature reviews. Neuroscience. 2009 Jun;10(6):434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- 8.Stawski RS, Sliwinski MJ, Smyth JM. Stress-related cognitive interference predicts cognitive function in old age. Psychology and aging. 2006 Sep;21(3):535–544. doi: 10.1037/0882-7974.21.3.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lupien SJ, Fiocco A, Wan N, et al. Stress hormones and human memory function across the lifespan. Psychoneuroendocrinology. 2005 Apr;30(3):225–242. doi: 10.1016/j.psyneuen.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 10.Oken BS, Fonareva I, Wahbeh H. Stress-related cognitive dysfunction in dementia caregivers. J Geriatr Psychiatry Neurol 22228825. 2011 Dec;24(4):191–198. doi: 10.1177/0891988711422524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harvey PD, Reichenberg A, Bowie CR. Cognition and aging in psychopathology: focus on schizophrenia and depression. Annual review of clinical psychology. 2006;2:389–409. doi: 10.1146/annurev.clinpsy.2.022305.095206. [DOI] [PubMed] [Google Scholar]
- 12.King DE, Matheson E, Chirina S, Shankar A, Broman-Fulks J. The status of baby boomers' health in the United States: the healthiest generation? JAMA Intern Med 23381505. 2013 Mar 11;173(5):385–386. doi: 10.1001/jamainternmed.2013.2006. [DOI] [PubMed] [Google Scholar]
- 13.Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA internal medicine. 2014 Mar;174(3):357–368. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khoury B, Lecomte T, Fortin G, et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clinical psychology review. 2013 Aug;33(6):763–771. doi: 10.1016/j.cpr.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 15.Gard T, Holzel BK, Lazar SW. The potential effects of meditation on age-related cognitive decline: a systematic review. Annals of the New York Academy of Sciences. 2014 Jan;1307:89–103. doi: 10.1111/nyas.12348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wahbeh H, Elsas SM, Oken BS. Mind-body interventions: applications in neurology. Neurology 18541886. 2008 Jun 10;70(24):2321–2328. doi: 10.1212/01.wnl.0000314667.16386.5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res 15256293. 2004 Jul;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 18.Tacon AM, McComb J, Caldera Y, Randolph P. Mindfulness meditation, anxiety reduction, and heart disease: a pilot study. Fam Community Health 12802125. 2003 Jan-Mar;26(1):25–33. doi: 10.1097/00003727-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry 1609875. 1992 Jul;149(7):936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- 20.Carlson LE, Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med 16262547. 2005;12(4):278–285. doi: 10.1207/s15327558ijbm1204_9. [DOI] [PubMed] [Google Scholar]
- 21.Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun 17521871. 2007 Nov;21(8):1038–1049. doi: 10.1016/j.bbi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 22.Price CJ, McBride B, Hyerle L, Kivlahan DR. Mindful awareness in body-oriented therapy for female veterans with post-traumatic stress disorder taking prescription analgesics for chronic pain: a feasibility study. Altern Ther Health Med 17985809. 2007 Nov-Dec;13(6):32–40. [PMC free article] [PubMed] [Google Scholar]
- 23.McHugh L, Simpson A, Reed P. Mindfulness as a potential intervention for stimulus over-selectivity in older adults. Research in Developmental Disabilities 19815376. 2010 Jan-Feb;31(1):178–184. doi: 10.1016/j.ridd.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 24.Zeidan F, Johnson SK, Diamond BJ, David Z, Goolkasian P. Mindfulness meditation improves cognition: evidence of brief mental training. Conscious Cogn. 2010 Jun;19(2):597–605. doi: 10.1016/j.concog.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 25.Oken BS, Fonareva I, Haas M, et al. Pilot controlled trial of mindfulness meditation and education for dementia caregivers. Journal of Alternative and Complementary Medicine. 2010;16:1031–1038. doi: 10.1089/acm.2009.0733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oken BS, Chamine I, Wakeland W. A systems approach to stress, stressors and resilience in humans. Behavioural brain research. 2015 Apr 1;282C:144–154. doi: 10.1016/j.bbr.2014.12.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kabat-Zinn J. Full Catastrophe Living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Delacourte Press; 1990. [Google Scholar]
- 28.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based Cognitive Therapy for Depression: A new approach to preventing relapse. New York: Guilford; 2002. [Google Scholar]
- 29.Lau MA, Yu AR. New developments in research on mindfulness-based treatments: introduction to the special issue. Journal of Cognitive Psychotherapy: An International Quarterly. 2009;23(3):179–184. [Google Scholar]
- 30.Wahbeh H, Svalina MN, Oken BS. Group, One-on-One, or Internet? Preferences for Mindfulness Meditation Delivery Format and their Predictors. Open Medicine Journal. 2014;1(1) doi: 10.2174/1874220301401010066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Lisle SM, Dowling NA, Allen JS. Mindfulness-based cognitive therapy for problem gambling. Clinical Case Studies. 2011;10(3):210–228. [Google Scholar]
- 32.Gluck TM, Maercker A. A randomized controlled pilot study of a brief web-based mindfulness training. BMC Psychiatry 22067058. 2011;11:175. doi: 10.1186/1471-244X-11-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boettcher J, Astrom V, Pahlsson D, Schenstrom O, Andersson G, Carlbring P. Internet-based mindfulness treatment for anxiety disorders: a randomized controlled trial. Behavior therapy. 2014 Mar;45(2):241–253. doi: 10.1016/j.beth.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 34.Krusche A, Cyhlarova E, Williams JMG. Mindfulness online: an evaluation of the feasibility of a web-based mindfulness course for stress, anxiety and depression. BMJ open. 2013;3(11):e003498. doi: 10.1136/bmjopen-2013-003498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morledge TJ, Allexandre D, Fox E, et al. Feasibility of an online mindfulness program for stress management—a randomized, controlled trial. Annals of Behavioral Medicine. 2013;46(2):137–148. doi: 10.1007/s12160-013-9490-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zernicke KA, Campbell TS, Speca M, McCabe-Ruff K, Flowers S, Carlson LE. A randomized wait-list controlled trial of feasibility and efficacy of an online mindfulness-based cancer recovery program: the eTherapy for cancer applying mindfulness trial. Psychosomatic medicine. 2014 May;76(4):257–267. doi: 10.1097/PSY.0000000000000053. [DOI] [PubMed] [Google Scholar]
- 37.Oken B, Miller M, Goodrich E, Wahbeh H. Effects of mindfulness meditation on self-rated stress-related measures: improvements in neuroticism and ecological momentary assessment of stress. The Journal of Alernative and Complementary Medicine. 2014;20:A64. [Google Scholar]
- 38.Neuendorf R, Wahbeh H, Chamine I, Yu Y, Hutchison K, Oken BS. The Effects of Mind-Body Interventions on Sleep Quality: A Systematic Review. Evidence-Based Complementary and Alternative Medicine. 2015 doi: 10.1155/2015/902708. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cohen S, Karmarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 40.Welsh KA, Breitner JCS, Magruder-Habib KM. Detection of dementia in the elderly using telephone screning of cognitive status. Neuropsychiatry, Neuropsychology, and Behavioral Neurology. 1993;6:103–110. [Google Scholar]
- 41.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. Journal of aging and health. 1993 May;5(2):179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 42.Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. Oxford University Press; 2004. [Google Scholar]
- 43.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Dell Publishing; 1990. [Google Scholar]
- 44.Wahbeh H, Lane JB, Goodrich E, Miller M, Oken BS. One-on-one mindfulness meditation trainings in a research setting. Mindfulness. 2012 Oct 31;5:88–99. doi: 10.1007/s12671-012-0155-9. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wahbeh H, Zwickey H, Oken BS. One method for objective adherence measurement in mind-body medicine. J Altern Complement Med. 2011 Feb;17(2):175–177. doi: 10.1089/acm.2010.0316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bohannon RW, Maljanian R, Goethe J. Screening for depression in clinical practice: reliability and validity of a five-item subset of the CES-Depression. Perceptual and motor skills. 2003 Dec;97(3 Pt 1):855–861. doi: 10.2466/pms.2003.97.3.855. [DOI] [PubMed] [Google Scholar]
- 47.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 48.Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann 10259963. 1982;5(3):233–237. doi: 10.1016/0149-7189(82)90074-x. [DOI] [PubMed] [Google Scholar]
- 49.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry 11132119. 2000 Jun;31(2):73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- 50.Oken BS. Placebo effect: clinical perspectives and potential mechanisms. In: Oken BS, editor. Complementary Therapies in Neurology. New York: Parthenon Publishing Group; 2004. [Google Scholar]
- 51.Baer RA, Smith GT, Lykins E, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008 Sep;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- 52.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988 Jun;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 53.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 2748771. 1989 May;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 54.Schmidt M. Rey Auditory and Verbal Learning Test: A Handbook. Los Angeles: Western Psychological Services; 1996. [Google Scholar]
- 55.Loonstra AS, Tarlow AR, Sellers AH. COWAT metanorms across age, education, and gender. Applied neuropsychology. 2001;8(3):161–166. doi: 10.1207/S15324826AN0803_5. [DOI] [PubMed] [Google Scholar]
- 56.Fan J, McCandliss BD, Sommer T, Raz A, Posner MI. Testing the efficiency and independence of attentional networks. Journal of cognitive neuroscience. 2002 Apr 1;14(3):340–347. doi: 10.1162/089892902317361886. [DOI] [PubMed] [Google Scholar]
- 57.Crowe SF. Does the letter number sequencing task measure anything more than digit span? Assessment. 2000 Jun;7(2):113–117. doi: 10.1177/107319110000700202. [DOI] [PubMed] [Google Scholar]
- 58.Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol 10965637. 2000 Aug;68(4):615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 59.Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics 1100130. 1975 Mar;31(1):103–115. [PubMed] [Google Scholar]
- 60.Cai H, Xia J, Xu D, Gao D, Yan Y. A generic minimization random allocation and blinding system on web. J Biomed Inform 16616696. 2006 Dec;39(6):706–719. doi: 10.1016/j.jbi.2006.02.015. [DOI] [PubMed] [Google Scholar]


