Abstract
Parental empathy is generally held as a positive characteristic; however, might there be contexts in which parental empathy is actually harmful? The present study examined whether adolescents’ depressive symptoms might have immunologic costs for more empathic parents. One hundred forty three parents and their children completed self-report measures of empathy and depressive symptoms, respectively. One year later, production of four pro-inflammatory cytokines in parents’ blood was measured in response to in vitro exposure to a bacterial product. Significant interactions across all inflammatory markers emerged, such that parents who were higher in empathy showed greater inflammatory cytokine production if their children also reported high levels of depressive symptoms, but lower cytokine production if their children reported low levels of symptoms. Less empathic parents showed the opposite pattern. These results provide support for the hypothesis that parents high in empathy may be especially sensitive physiologically to their children’s psychopathologic symptoms.
Empathy—the broad tendencies of a person to both affectively experience emotions of concern at the suffering of others and to cognitively adopt the perspective of another—is a highly valued, prosocial trait that has been shown to relate to abundant positive outcomes (Davis, 1983; Eisenberg & Miller, 1987). In the context of child rearing, the ability of parents to empathize with their children is considered fundamental to healthy, skillful parenting (Dix, 1992; Kochanska, 1997) and is believed to facilitate better psychological development for children (Eisenberg, Fabes, Schaller, Carlo, & Miller, 1991; Feshbach, 1987; Soenens, Duriez, Vansteenkiste, & Goossens, 2007; Strayer & Roberts, 2004). Not surprisingly, parental empathy is held as a prized and positive characteristic; however, may there be contexts in which parental empathy is actually harmful?
Although the tendency of parents to understand and compassionately care about the lives of their children may be beneficial to their loved ones, it is possible that greater empathy may also make parents more sensitive to the effects of —and burdened by— times when their children are suffering. Through greater perspective-taking and more emotional investment, highly empathic parents may be better oriented to the emotional climates of their loved ones (Kochanska, 1997). However, when this climate becomes fraught with greater distress, it is possible that empathy may amplify the burden that parents experience, much as individuals in empathically demanding professions report experiences of vicarious trauma and burnout (Zapf, Seifert, Schmutte, Mertini, & Holz, 2001).
If empathy sensitizes parents to the suffering of their children, one salient context for witnessing this phenomenon may be when children are experiencing greater distress, for example, elevations in depressive symptomatology. Depression in children and adolescents is a prevalent, recurrent, and frequently chronic disorder (Birmaher, Ryan, Williamson, Brent, & Kaufman, 2005; Costello et al., 2002), with approximately 20% of individuals meeting full diagnostic criteria for major depressive disorder at least once by age 18 (Lewinsohn, Rohde, Seeley, & Fischer, 1993). In addition to placing youths at increased risk for substance use, suicide, and other comorbid diagnoses (Galaif, Sussman, Newcomb, & Locke, 2007), depression also exposes youths’ support systems to greater strain, including more frequent negative interactions with family members and greater emotional burden on parents (Angold et al., 1998; Kashani, Burbach, & Rosenberg, 1988).
As parents strive to support loved ones and subvert their own needs, it is possible that with greater child distress comes a greater physiological cost for empathic parents. Specifically, as greater empathy motivates parents to provide a supportive and non-reactive environment (Larson & Yao, 2005), it may require parents to suppress their own feelings, such as of judgment or frustration. Here, children with depressive symptoms may necessitate more frequent support and thus more emotional suppression by parents. Engaging in emotional suppression, however, has been found to increase physiological responses (Gross, 1998; Gross & Levenson, 1993). In addition, research by Appleton et al. (2013) has demonstrated that individuals who more frequently engage in emotional suppression as an emotion regulation strategy show higher levels of chronic, low-grade inflammation. Moreover, other seemingly positive psychological traits that require ongoing effort (such as self-control or goal-persistence) have been shown to relate to negative physiological processes, including greater physiological wear-and-tear and greater chronic inflammation (Brody et al., 2013; Miller & Wrosch, 2007). Likewise, empathic responding may require effort that ultimately comes at a physical cost.
One biological system of particular relevance to the psychological burdens experienced by caregivers is the immune system, which is exquisitely responsive to an individual’s social and psychological environments (e.g. Lovell & Wetherell, 2011; Miller, Chen, & Parker, 2011; Segerstrom & Miller, 2004). The immune system functions in part to detect pathogens, and when it does, it releases cytokines—such as interleukin 6 (IL-6) and tumor necrosis factor alpha (TNF-α)—that coordinate an inflammatory response. Although acute immune activation is necessary to destroy infections and repair tissue damage, these processes can also be triggered and compounded by psychological threats (Maes et al., 1998; Segerstrom & Miller, 2004), and over-activation of these responses over a prolonged period of time can lead to negative health consequences (Kiecolt-Glaser & Glaser, 2002; Kiecolt-Glaser, McGuire, Robles, & Glaser, 2002). For example, caregivers of patients with chronic illnesses show elevations in markers of chronic inflammation and reduced sensitivity to the regulatory effects of glucocorticoids (Lovell & Wetherll, 2011; Miller et al. 2008), as well as increasing levels of chronic inflammation over time (Rohleder, Marin, Ma, & Miller, 2009). Here, psychological stressors are thought to prime the immune system to exhibit heightened inflammatory responses in the presence of pathogens, which if experienced repeatedly, may lead to elevations in chronic, low-grade inflammation and to dysregulation of counter-regulatory immune mechanisms (Miller et al., 2011).
To the extent that empathic parents are more attuned to the suffering of their children, it is possible that this greater empathy may potentiate the effect of interpersonal stressors on their own immune functioning. Theories of biological sensitivity to context (Boyce & Ellis, 2005) and differential susceptibility (Belsky & Pluess, 2009) propose that individuals may differ in the extent to which their psychological and physiological processes are responsive to their environments. Here, for better or worse, more receptive individuals respond to both the positive and negative elements of their experiences more than less receptive individuals, for example, becoming more impaired by stressful life events but also more responsive to positive social environments (Hankin et al., 2011). In a similar manner, if empathy encourages a greater sensitivity to one’s social context, it too may be associated with differences in inflammatory responses depending on the distress levels found within that social context.
The present study sought to test whether parental empathy would amplify the physiological costs for parents of their adolescent children experiencing greater depressive symptomatology. Specifically, it examined whether child depressive symptoms and parents’ dispositional empathy (assessed at baseline) interacted to predict parents’ immune responsivity one year later. Parents’ immune responses were measured by exposing parental blood in vitro to a bacterial stimulus and then measuring the magnitude of inflammatory responses, as indicated by the production of pro-inflammatory cytokines resulting from this exposure. It was hypothesized that as child depressive symptoms increased, the association between parental empathy and cytokine production would become increasingly positive, such that empathic parents would demonstrate greater pro-inflammatory cytokine production when their children were high in depressive symptoms, but less cytokine production if their children were low in depressive symptoms. Parents low in empathy were not expected to show differences in cytokine production as their children’s depressive symptoms increased.
Method
Participants
Parents and their adolescent children (ages 13–16) were recruited through advertisements in local media as part of a larger study on psychosocial contributors to cardiovascular disease risk (Human et al., 2014; Schreier, Roy, Frimer, & Chen, 2014). One adolescent and one parent from each family participated. All participants were required to be free of any chronic or acute medical illness and to be English-speaking. Data from two time-points were considered: psychosocial measures taken at baseline and blood drawn one year later. Complete data on psychosocial and biomarker variables were available for 143 dyads (76% mothers; 50% daughters). The mean age for parents was 45.5 years (SD=5.53) and the mean age for adolescents was 14.5 years (SD=1.07) at baseline. Fifty-five percent of families identified as being of European descent, 38% were Asian descent, 4 % were Hispanic descent, 1% was African descent, and 2% identified as “other.” Family income ranged from less than $5000 to more than $200,000, with mean income in the 50,000–75,000 Canadian dollars range. The mean level of education for parents was some college education.
Procedure
As part of the baseline laboratory visit, parents and adolescents provided written consent, as overseen by the Institutional Review Board, and completed self-report questionnaires described below. One year later, families returned for a follow-up visit, and blood samples were obtained from parents. Covariates related to inflammation, including waist circumference and demographic variables, were also recorded at this time.
Measures
Parental Empathy
Parents completed the Empathic Concern and Perspective Taking subscales of the Interpersonal Reactivity Index (Davis, 1983) at baseline, a widely used measure of dispositional empathy. This measure has previously been shown to have a two-year test-retest correlation of r=.58 and to relate to other measures of empathy, as well as to predict self-esteem and sensitivity to others (Davis, 1983; Davis & Franzoi, 1991). The Empathic Concern subscale captures affective dimensions of empathy, assessing emotional experiences stemming from sympathy or compassion for others, such as having “tender, concerned feelings for people less fortunate than me” (α=.76, current sample). The Perspective Taking subscale probes for cognitive dimensions of empathy, gauging one’s tendency to adopt the psychological viewpoint of others, such as “[trying] to understand my friends better by imagining how things look from their perspective” (α=.76, current sample). A single composite score (labeled “Empathy”) was computed by summing standardized scores on each scale, as responses on the two scales were significantly correlated (r(141)=.52, p<.01), with higher scores indicating greater empathy.
Child Depressive Symptoms
During the baseline lab visit, adolescents completed the Center for Epidemiological Studies Depression Scale Short Form (Bjorgvinsson, Kertz, Bigda-Peyton, McCoy, & Aderka, 2013), a widely used self-report depression screen that assesses the frequency of ten depressive symptoms over the course of the previous week and is appropriate for use with adolescents (Bradley, McGrath, Brannen, & Bagnell, 2010). Its reliability and validity have been established in both clinical and community samples, showing convergence with other self-report measures of depression as well as clinical diagnoses of major depressive disorder (Anderson, Malmgren, Carter, & Patrick, 1994; Bjorgvinsson et al., 2013). Higher scores on this measure indicate higher levels of depressive symptoms (α=.67, current sample).
Parenting Behaviors
To clarify the unique contribution of parental empathy versus more general parenting behaviors, child-reported positive parenting behaviors were also assessed at baseline. Using items developed by Brody et al. (2001), adolescents reported on how frequently their parents acted supportively or lovingly toward them, such as by letting their children know they appreciated them or helping them with an important task. The one-year test-retest correlation on this measure has been reported as r=.41 (H. Kim, Ji, & Kao, 2011). Here, nine items were rated on four-point scales, with higher scores on this measure reflecting more positive parenting behaviors (α=.89, current sample). Although formal validation studies of this measure have not been published, this collection of items has previously been demonstrated to relate positively to the frequency of nurturing caregiving behaviors as reported by both children and their parents and to relate negatively to increases in child psychopathology symptoms over time (Brody et al., 2001; Kim et al., 2003).
Inflammatory Markers
One year after the baseline visit, peripheral blood was drawn from parents using antecubital venipuncture into sodium heparin vacutainer tubes, which were diluted with 10% isotonic saline solution. Blood was then mixed with 400uL of saline solution and 50ng/mL lipopolysaccaride (LPS)—a bacterial stimulus—and then incubated for 6 hours at 37°C at 5% CO2. The production of four cytokines were measured: Interleukin 1-beta (IL-1β), Interleukin 6 (IL-6), Interleukin 10 (IL-10), and Tumor Necrosis Factor-alpha (TNF-α). IL-1, IL-6, and TNF-α are considered classic pro-inflammatory cytokines. IL-10, although considered anti-inflammatory, is typically released when pro-inflammatory cytokines become high, and thus often relates to outcomes in the same way as pro-inflammatory cytokines. (In the current study, all four cytokines were significantly and positively correlated, rs(141)>.42, ps<.001.) Cytokine production was measured using Meso Scale Discovery human pro-inflammatory 7-plex base kit (Meso Scale Discovery, Gaithersburg, MD). Enzyme-linked immunosorbent assay plates were analyzed using the Sector Imager 2400 from Meso Scale Discovery. (Mean intra-assay CV=3.46.) Values were log-transformed prior to analysis in order to normalize their distribution.
Covariates
Demographic variables and variables known to affect inflammation were also assessed at the time of the blood draw and included as covariates. These included parent gender, age, ethnicity, and waist circumference (an indicator of adiposity).
Statistical Analyses
Multiple regression analyses were conducted in which stimulated cytokine values were regressed onto parental empathy, child depressive symptoms, and their interaction. Parental empathy and child depressive symptoms were centered before calculating the interaction term, and recommendations for testing interactions with two continuous variables outlined by Aiken & West (1991) were followed. Models were repeated while covarying demographic and adiposity variables. Secondary analyses examined whether similar patterns of results were obtained when substituting a more general measure of positive parenting behaviors for parent empathy, as well as simultaneously including positive parenting behaviors and its interaction with child depressive symptoms into regressions with parental empathy and its interaction.
Results
Empathy and Depressive Symptom Interactions
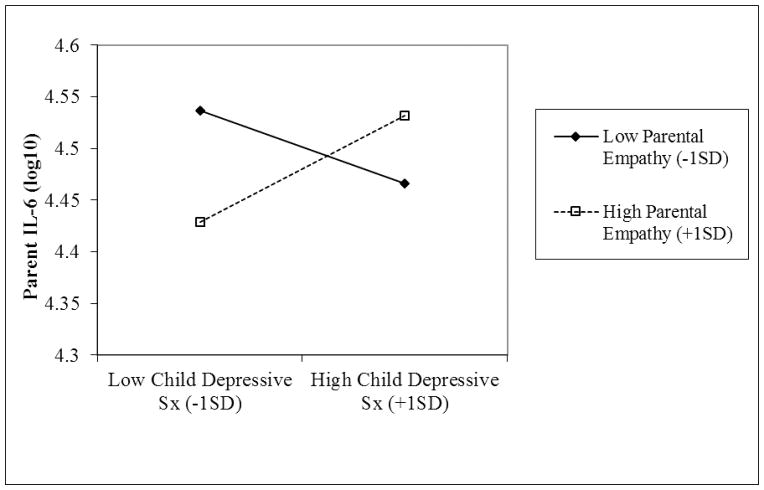
As presented in Table 1, regression analyses revealed no main effects of parental empathy or child depressive symptoms on stimulated cytokine production. However, significant interactions emerged across all markers, as well as their composite (created by summing z-scored cytokine values). In support of our hypothesis, parents higher in empathy showed greater cytokine production as child depression symptoms increased (see Figure 1). Parents lower in empathy showed the opposite pattern. In addition, all interactions remained significant when including covariates of parental age, gender, ethnicity, and waist circumference (Standβs>.24, ps<.05, semipartialr2s>.05).
Table 1.
Multiple Regression Models for Parental Empathy, Child Depressive Symptoms, and Their Interaction Predicting Parent Stimulated Inflammatory Cytokines
| Predictor Variable | R | R2 | F | Sig | Standβ | t | p | sr2 |
|---|---|---|---|---|---|---|---|---|
| Model IL-1β | .26 | .07 | 3.41 | .02 | ||||
| Empathy | −.07 | −.88 | .38 | .01 | ||||
| Child Depressive Sx | −.02 | −.19 | .85 | .00 | ||||
| Empathy x Depressive Sx | .26 | 3.14 | .00 | .06 | ||||
|
| ||||||||
| Model IL-6 | .27 | .07 | 3.55 | .02 | ||||
| Empathy | −.06 | −.76 | .45 | .00 | ||||
| Child Depressive Sx | .04 | .43 | .67 | .00 | ||||
| Empathy x Depressive Sx | .39 | 4.32 | .00 | .07 | ||||
|
| ||||||||
| Model TNF-α | .27 | .07 | 3.69 | .01 | ||||
| Empathy | −.13 | −1.53 | .13 | .02 | ||||
| Child Depressive Sx | .01 | .16 | .87 | .00 | ||||
| Empathy x Depressive Sx | .24 | 2.89 | .00 | .06 | ||||
|
| ||||||||
| Model IL-10 | .23 | .05 | 2.66 | .05 | ||||
| Empathy | −.14 | −1.64 | .10 | .02 | ||||
| Child Depressive Sx | −.06 | −.71 | .48 | .00 | ||||
| Empathy x Depressive Sx | .18 | 2.13 | .04 | .03 | ||||
|
| ||||||||
| Model Inflammation Composite | .30 | .09 | 4.59 | .00 | ||||
| Empathy | −.12 | −1.44 | .15 | .01 | ||||
| Child Depressive Sx | −.01 | −.10 | .92 | .00 | ||||
| Empathy x Depressive Sx | .27 | 3.35 | .00 | .07 | ||||
Note. IL-1 β= Interleukin 1 Beta,; IL-6= Interleukin 6; IL-10= Interleukin 10; TNF-α= Tumor Necrosis Factor-Alpha; sr2=semi-partial r-squared. All inflammatory markers were log-transformed prior to analysis. The inflammation composite reflects the sum of z-scored IL-1 β, IL-6, IL-10, and TNF-α levels. Similar results were obtained when including participant age, ethnicity, gender, and waist circumference as covariates.
Figure 1. Interaction between Parental Empathy and Child Depressive Symptoms Predicting Parents’ Interleukin-6 (IL-6) Production.
Note. Similar results were obtained for stimulated IL-1ra, IL-10, TNF-α, and the inflammation composite
Secondary Analyses
It is possible that associations with parental empathy are not specific to empathy per se, but rather reflect more general parenting characteristics such as positive parenting behaviors. (Although not statistically significant, parental empathy and positive parenting behaviors were positively correlated r(141)=.11, p=.17.) To test for this possibility, regression analyses were first rerun substituting positive parenting for parental empathy, along with its interaction with child depressive symptoms and adiposity and demographic covariates, in predicting inflammatory markers. There were no significant main effects of positive parenting behaviors or child depressive symptoms, and no interaction effects (Standβs< .16, ps>.05, spr2s<.03). Second, multiple regression analyses were run including positive parenting and its interaction with child depressive symptoms simultaneously with parental empathy and its interaction with depressive symptoms, in addition to covariates. All interactions between parental empathy and child depressive symptoms remained significant (Standβs>.22, ps<.05, spr2s>.04) and there were no additional independent contributions of positive parenting or its interaction (Standβs< .10, ps>.05, spr2s<.02), suggesting that parental empathy uniquely interacts with child depressive symptoms to predict parents’ cytokine production.
Discussion
These results provide support for the hypothesis that parents with higher levels of empathy may be especially affected – physiologically—by the depressive symptoms of their adolescent children. Specifically, across four markers of inflammation, parents who were higher in empathy showed heightened cytokine production to in vitro stimulation by a bacterial product as their children’s depressive symptoms increased. In contrast, for parents lower in empathy, there was a negative association between children’s depressive symptoms and stimulated cytokine production. Moreover, these associations do not appear to be accounted for by adiposity- or demographic-related variables or by more general positive parenting behaviors.
While researchers have long acknowledged the profound influences of parental depression on children (Lieb, Isenee, Hofler, Pfister, & Wittchen, 2002; Singh et al., 2010), relatively less work has examined the reverse relationship, of the effects of child depression on parents. The present work suggests that empathic parents may be especially vulnerable to these effects. Specifically, parents who are better able to take the perspective of others and are more emotionally invested may more viscerally experience and be burdened by their children’s psychological distress. This mirrors research regarding the psychological costs of vicarious trauma in counselors and therapists (Schauben & Frazier, 1995), with the present study finding evidence for physiological costs of empathy in family members. An alternative explanation is that highly empathic parents may be more self-sacrificing in their caregiving of distressed children and may neglect protective health behaviors for themselves, such as getting adequate sleep, exercise, or nutrition, consistent with work documenting the physiological toll associated with taking care of others (Kiecolt-Glaser et al., 1991).
That parents who are higher in empathy showed reduced pro-inflammatory cytokine production when children were low in depressive symptoms but greater production when children were high in depressive symptoms suggests that empathy may confer a heighten biological sensitivity to context (Boyce & Ellis, 2005; Ellis & Boyce, 2011). In their seminal work, Boyce and Ellis (2005) suggest that individuals can differ in the extent to which their stress response systems react to input from their environments in ways that may be beneficial if the environment is good or detrimental if the environment is bad. With regards to the current work, one’s tendency to take the perspective of others and react with emotional concern may similarly amplify responding to social contexts such that empathy can be either positive or negative depending on the situation.
Because we saw effects on the functioning of immune cells (how they respond to a bacterial stimulus), over the long term, it is possible that these exaggerated immunological responses will lead to higher levels of chronic inflammation (Miller & Chen, 2010). In turn, this may then put empathic parents at elevated risk for a host of physical health problems linked to inflammation, including heart disease and certain cancers (Heikkilä et al., 2008; Ridker, Hennekens, Buring, & Rifai, 2000). Chronic inflammation may have repercussions for parents’ mental health as well, as several lines of research suggest that inflammation is implicated in the etiology of depression. For example, individuals with depression consistently show elevations in pro-inflammatory cytokines (Dowlati et al., 2010) and induction of an inflammatory response is associated with the onset of several symptoms of depression, including low mood (Eisenberger, Inagaki, Mashal, & Irwin, 2010). Through these inflammatory processes, it is possible, then, that child depression may transmit effects onto parents. Of course, the current study is limited by its single assessments of stimulated cytokine production, depressive symptoms, and empathy and is not able to address these possibilities directly. However, given that first onset of depressive disorders is often in adolescence (Burke, Burke, Rae, & Regier, 1991), it is possible that our associations are capturing the first stage in a cascade by which greater inflammatory responses lead over time to chronic inflammation more systemically and, ultimately, to heath risks for parents, if children’s depressive symptoms are not ameliorated.
There are several other limitations to the present investigation. For example, the present work focused on adolescents in a healthy, community sample in which depressive symptoms were generally low. Second, no formal validation study has been conducted for the parenting questionnaire, though this measure has been used repeatedly in other parent-adolescent research, has good reliability, and has been shown to predict changes in child psychopathology (Kim et al., 2003). Further, in this preliminary study, we were unable to assess possible mechanism variables—such as coping processes, enmeshment, health behaviors, or chronic strain—that may account for our results. It is also not yet clear whether our results are specific to youth depression or whether they would apply to other types of psychological symptoms as well. Lastly, it remains unclear why parents who are lower in empathy appear to show more adaptive inflammatory responses as child depressive symptoms increase.
Despite these limitations, the current work raises intriguing possibilities for future research. Although many interventions exist for treating depressive symptoms in children, we are unaware of studies that consider the impact of children’s treatment on parents. As family interventions aimed at reducing child psychological symptoms frequently seek to foment greater parental empathy (e.g. Marvin, Cooper, Hoffman, & Powell, 2002), assessing parental physiological functioning throughout these interventions would determine whether there are hidden costs embedded in expanding parents’ repertoire for empathic responding. It is possible that as children get better from treatment, parents may actually get worse, and thus we would need to modify treatment interventions to consider these effects. In addition, to more firmly establish whether empathy reflects a greater biological sensitivity to context, it would be interesting for future work to examine not only negative contexts such as child depression but also positive contexts and whether high parental empathy when children have positive life experiences is associated with more beneficial inflammatory profiles. For example, what might empathic parents’ immune functioning look like when positive events happen to their children, such as college acceptance, social successes, or extracurricular achievements?
Despite these unanswered questions, the present study has several important implications. Although a high level of empathy is often assumed to be an exclusively positive characteristic (e.g. Eisenberg & Miller, 1987), the current work suggests that, at least under certain circumstances, it may also make the person expressing empathy more vulnerable to inflammation-related health problems over time. Further, the present findings highlight the complex interpersonal context of depressive symptoms (not only from parent to child but also from child to parent) and emphasize important connections between physical and mental health processes in families, demonstrating that child depressive symptoms, in conjunction with parent trait qualities of empathy, “get under the skin” and relate to inflammatory processes in parents.
Acknowledgments
Support for this research was provided by the Canadian Institutes of Health Research grant 97872, National Heart, Lung, and Blood Institute grant R01 HL108723, and National Institute on Drug Abuse grant P30 DA027827.
Footnotes
Author Contributions
E.M. Manczak and E. Chen developed the study concept. E.M. Manczak performed data analysis and interpretation under the supervision of E. Chen. E.M. Manczak drafted the manuscript and D. Basu and E. Chen provided critical revisions. All authors approved the final version of the manuscript for submission.
Contributor Information
Erika M. Manczak, Northwestern University
Devika Basu, Northwestern University.
Edith Chen, Northwestern University.
References
- Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- Anderson EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventative Medicine. 1994;10:77–84. [PubMed] [Google Scholar]
- Angold A, Messer SC, Stangl D, Farmer EMZ, Costello EJ, Burns BJ. Perceived parental burden and service use for child and adolescent psychiatric disorders. American Journal of Public Health. 1998;88(1):75–80. doi: 10.2105/ajph.88.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleton AA, Buka SL, Loucks EB, Gilman SE, Kubzansky LD. Divergent associations of adaptive and maladaptive emotion regulation strategies with inflammation. Health Psychology. 2013;32(7):748–756. doi: 10.1037/a0030068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky J, Pluess M. Beyond diathesis stress: Differential susceptibility to environmental influences. Psychological Bulletin. 2009;135(6):885–908. doi: 10.1037/a0017376. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman JA. Childhood and adolescent depression: A review of the past 10 years, Part II. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;35(12):1575–1583. doi: 10.1097/00004583-199612000-00008. [DOI] [PubMed] [Google Scholar]
- Bjorgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20(4):429–436. doi: 10.1177/1073191113481998. [DOI] [PubMed] [Google Scholar]
- Boyce WT, Ellis BJ. Biological sensitivity to context: I. An evolutionary-developmental theory of the origins and functions of stress reactivity. Development and Psychopathology. 2005;17:271–301. doi: 10.1017/s0954579405050145. [DOI] [PubMed] [Google Scholar]
- Bradley KL, McGrath PJ, Brannen CL, Bagnell AL. Adolescents’ attitudes and opinions about depression treatment. Community Mental Health Journal. 2010;46(3):242–251. doi: 10.1007/s10597-009-9224-5. [DOI] [PubMed] [Google Scholar]
- Brody GH, Yu T, Chen E, Miller GE, Kogan SM, Beach SRH. Is resilience only skin deep?: Rural African Americans’ socioeconomic status-related risk and competence in preadolescence and psychological adjustment and allostatic load at age 19. Psychological Science. 2013;24(7):1285–1293. doi: 10.1177/0956797612471954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody G, Ge X, Conger R, Gibbons F, Murry VM, Gerrard M, Simmons RL. The influence of neighborhood disadvantage, collective socialization, and parenting on African American children’s affiliation with deviant peers. Child Development. 2001;72(4):1231–1246. doi: 10.1111/1467-8624.00344. [DOI] [PubMed] [Google Scholar]
- Burke KC, Burke JD, Jr, Rae DS, Regier DA. Comparing age at onset of major depression and other psychiatric disorers by birth cohorts in five US community populations. Archives of General Psychiatry. 1991;48:789–795. doi: 10.1001/archpsyc.1991.01810330013002. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Pine DS, Hammen C, SMJ, Plotsky PM, Weissman MM, et al. Development and natural history of mood disorders. Biological Psychiatry. 2002;52:529–542. doi: 10.1016/s0006-3223(02)01372-0. [DOI] [PubMed] [Google Scholar]
- Davis MH. Measuring individual differences in empathy: Evidence for a multidimensional approach. Journal of Personality and Social Psychology. 1983;44(1):113–126. [Google Scholar]
- Davis MH, Franzoi SL. Stability and chance in adolescent self-consciousness and empathy. Journal of Research in Personality. 1991;25:70–87. [Google Scholar]
- Dix T. Parenting on behalf of the child: Empathic goals in the regulation of responsive parenting. In: Sigel IE, McGillicuddy-DeLisi AV, Goodnow JJ, editors. Parental belief systems: The psychological consequences for children. 2. Hillsdale, NJ: Lawrence Erlbaum Associates Publishers; 1992. pp. 319–346. [Google Scholar]
- Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, Lanctôt KL. A meta-analysis of cytokines in major depression. Biological Psychiatry. 2010;67(5):446–457. doi: 10.1016/j.biopsych.2009.09.033. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Miller PA. The relation of empathy to prosocial and related behaviors. Psychological Bulletin. 1987;101(1):91–119. [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Schaller M, Carlo G, Miller PA. The relations of parental characteristics and practices to children’s vicarious emotional responding. Child Development. 1991;62:1393–1408. [PubMed] [Google Scholar]
- Eisenberger NI, Inagaki TK, Mashal NM, Irwin MR. Inflammation and social experience: An inflammatory challenge induces feelings of social disconnection in addition to depressed mood. Brain, Behavior, and Immunity. 2010;24(4):558–563. doi: 10.1016/j.bbi.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis BJ, Boyce WT. Differential susceptibility to the environment: Toward an understanding of sensitivity to developmental experiences and context. Development and Psychopathology. 2011;23(01):1–5. doi: 10.1017/S095457941000060X. [DOI] [PubMed] [Google Scholar]
- Feshbach ND. Parental empathy and child adjustment/maladjustment. In: Eisenberg N, Strayer J, editors. Empathy and its development. Cambridge: Cambridge University Press; 1987. pp. 271–291. [Google Scholar]
- Galaif ER, Sussman S, Newcomb M, Locke TF. Suicidality, depression, and alcohol use among adolescents: A review of empirical findings. International Journal of Adolescent Medical Health. 2007;19(1):27–35. doi: 10.1515/ijamh.2007.19.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ. The emerging field of emotion regulation: An integrative review. Review of General Psychology. 1998;2:271–299. [Google Scholar]
- Gross J, Levenson R. Emotional suppression: Physiological, self-report, and expressive behavior. Journal of Personality and Social Psychology. 1993;64(6):970–986. doi: 10.1037//0022-3514.64.6.970. [DOI] [PubMed] [Google Scholar]
- Hankin B, Nederof E, Oppenheimer C, Jenness J, Young J, Abela J, Smolen A, Ormel J, Oldehikel A. Differential susceptibility in youth: Evidence that 5-HTTLPR x positive parenting is associated with positive affect ‘for better and worse.’. Translational Psychiatry. 2011:e44. doi: 10.1038/tp.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heikkilä K, Harris R, Lowe G, Rumley A, Yarnell J, Gallacher J, et al. Associations of circulating C-reactive protein and interleukin-6 with cancer risk: findings from two prospective cohorts and a meta-analysis. Cancer Causes & Control. 2008;20(1):15–26. doi: 10.1007/s10552-008-9212-z. [DOI] [PubMed] [Google Scholar]
- Human LJ, Chan M, DeLongis A, Roy L, Miller GE, Chen E. Parental accuracy regarding adolescent daily experiences. Psychosomatic Medicine. 2014;76(8):603–610. doi: 10.1097/PSY.0000000000000105. [DOI] [PubMed] [Google Scholar]
- Kashani JH, Burbach DJ, Rosenberg TK. Perception of family conflict resolution and depressive symptoms in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1988;27(1):42–28. doi: 10.1097/00004583-198801000-00007. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Glaser R. Depression and immune function: Central pathways to morbidity and mortality. Journal of Psychosomatic Research. 2002;53:873–876. doi: 10.1016/s0022-3999(02)00309-4. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Dura JR, Speicher CE, Trask OJ, Glaser R. Spousal caregivers of dementia victims: longitudinal changes in immunity and health. Psychosomatic Medicine. 1991;53(4):345–362. doi: 10.1097/00006842-199107000-00001. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser J, McGuire L, Robles TF, Glaser R. Emotions, morbidity, and mortality: New perspectives from psychoneuroimmunology. Annual Review of Psychology. 2002;53:83–107. doi: 10.1146/annurev.psych.53.100901.135217. [DOI] [PubMed] [Google Scholar]
- Kim H, Ji J, Kao D. Burnout and physical health among social workers: A three-year longitudinal study. Social Work. 2011;56(3):258–268. doi: 10.1093/sw/56.3.258. [DOI] [PubMed] [Google Scholar]
- Kim IJ, Ge X, Brody GH, Conger RD, Gibbons FX, Simons RL. Parenting behaviors and the occurrence and co-occurrence of depressive symptoms and conduct problems among African American children. Journal of Family Psychology. 2003;17(4):571–583. doi: 10.1037/0893-3200.17.4.571. [DOI] [PubMed] [Google Scholar]
- Kochanska G. Mutually responsive orientation between mothers and their young children: Implications for early socialization. Child Development. 1997;68:94–112. [PubMed] [Google Scholar]
- Larson EB, Yao X. Clinical empathy as emotional labor in the patient-physician relationship. Jama. 2005;293(9):1100. doi: 10.1001/jama.293.9.1100. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Fischer SA. Age-cohort changes in the lifetime occurrence of depression and other mental disorders. Journal of Abnormal Psychology. 1993;102:110–120. doi: 10.1037//0021-843x.102.1.110. [DOI] [PubMed] [Google Scholar]
- Lieb R, Isenee B, Hofler M, Pfister H, Wittchen HU. Parental major depression and the risk of depression and other mental disorders in offspring. Archives of General Psychiatry. 2002;59:365–374. doi: 10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- Lovell B, Wetherell MA. The cost of caregiving: Endocrine and immune implications in elderly and non elderly caregivers. Neuroscience & Biobehavioral Reviews. 2011;35(6):1342–1352. doi: 10.1016/j.neubiorev.2011.02.007. [DOI] [PubMed] [Google Scholar]
- Maes M, Song C, Lin A, De Jongh R, Van Gastel A, Kenis G, et al. The effects of psychological stress on humans: increased production of pro-inflammatory cytokines and Th1-like response in stress-induced anxiety. Cytokine. 1998;10(4):313–318. doi: 10.1006/cyto.1997.0290. [DOI] [PubMed] [Google Scholar]
- Marvin R, Cooper G, Hoffman K, Powell B. The Circle of Security project: Attachment-based intervention with caregiver-pre-school child dyads. Attachment & Human Development. 2002;4(1):107–124. doi: 10.1080/14616730252982491. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E. Harsh family climate in early life presages the emergence of a proinflammatory phenotype in adolescence. Psychological Science. 2010;21(6):848–856. doi: 10.1177/0956797610370161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Wrosch C. You’ve gotta know when to fold ‘em: Goal disengagement and systemic inflammation in adolescence. Psychological Science. 2007;18(9):773–777. doi: 10.1111/j.1467-9280.2007.01977.x. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin. 2011;137(6):959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Sze J, Marin T, Arevalo J, Doll R, Ma R, Cole S. A functional genomic fingerprint of chronic stress in humans: Blunted glucocorticoid and increased NF-κB signaling. Biological Psychiatry. 2008;64(4):266–272. doi: 10.1016/j.biopsych.2008.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. The New England Journal of Medicine. 2000;342(12):836–843. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- Rohleder N, Marin TJ, Ma R, Miller GE. Biologic cost of caring for a cancer patient: Dysregulation of pro- and anti-inflammatory signaling pathways. Journal of Clinical Oncology. 2009;27(18):2909–2915. doi: 10.1200/JCO.2008.18.7435. [DOI] [PubMed] [Google Scholar]
- Schauben LJ, Frazier PA. Vicarious trauma the effects on female counselors of working with sexual violence survivors. Psychology of Women Quarterly. 1995;19(1):49–64. [Google Scholar]
- Schreier HMC, Roy LB, Frimer LT, Chen E. Family chaos and adolescent inflammatory profiles: The moderating role of socioeconomic status. Psychosomatic Medicine. 2014;76(6):460–467. doi: 10.1097/PSY.0000000000000078. [DOI] [PubMed] [Google Scholar]
- Segerstrom SC, Miller GE. Psychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychological Bulletin. 2004;130(4):601–630. doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh AL, D’Onofrio BM, Slutske WS, Turkheimer E, Emery RE, Harden KP, et al. Parental depression and offspring psychopathology: a Children of Twins study. Psychological Medicine. 2010;41(07):1385–1395. doi: 10.1017/S0033291710002059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TW, Gallo LC. Hostility and cardiovascular reactivity during marital interaction. Psychosomatic Medicine. 1999;61:436–445. doi: 10.1097/00006842-199907000-00005. [DOI] [PubMed] [Google Scholar]
- Soenens B, Duriez B, Vansteenkiste M, Goossens L. The intergenerational transmission of empathy-related responding in adolescence: The role of maternal support. Personality and Social Psychology Bulletin. 2007;33(3):299–311. doi: 10.1177/0146167206296300. [DOI] [PubMed] [Google Scholar]
- Strayer J, Roberts W. Children’s anger, emotional expressiveness, and empathy: Relations with parents’ empathy, emotional expressiveness, and parenting practices. Social Development. 2004;13:229–254. [Google Scholar]
- Zapf D, Seifert C, Schmutte B, Mertini H, Holz M. Emotion work and job stressors and their effects on burnout. Psychology and Aging. 2001;16:527–545. doi: 10.1080/08870440108405525. [DOI] [PubMed] [Google Scholar]