Abstract
Objective
Epidemiological evidence suggests an association between the use of hormonal contraception and an increased risk of acquiring sexually transmitted diseases including HIV-1. We sought to elucidate the biological mechanisms underlying the effect of hormonal contraception on the immune system.
Design
Cross-sectional study.
Methods
To delineate the biological mechanisms underlying the effect of hormonal contraceptives on the immune system, we analyzed the functional capacity of circulating plasmacytoid dendritic cells (pDCs), the distribution of vaginal immune cell populations, and the systemic and genital levels of immune mediators in women using depot medroxyprogesterone acetate (DMPA), NuvaRing, or combined oral contraceptives (COC).
Results
The use of DMPA or NuvaRing was associated with reduced capacity of circulating pDCs to produce IFNα and TNFα in response to TLR-9 stimulation. Systemic levels of IFNα and cervicovaginal fluid levels of IFNα, CXCL10, MCP-1, and G-CSF were significantly lower in DMPA users compared to control volunteers not using hormonal contraception. The density of CD207+ Langerhans cells in the vaginal epithelium was reduced in NuvaRing and COC users but not in DMPA users.
Conclusions
The presented evidence suggests that the use of some types of hormonal contraception is associated with reduced functional capacity of circulating pDCs and altered immune environment in the female reproductive tract.
Keywords: contraception, HIV-1, AIDS, DMPA, immune system, progestin
Introduction
Access to safe, effective, and affordable methods of contraception is a critical component of preventive health care. Contraception provides women with a means of control over their reproductive health, reduces the number of abortions and unintended pregnancies and, in effect, decreases maternal and infant morbidity and mortality. Injectable contraceptives including DMPA are increasingly popular due to their ease of use, effectiveness, and affordability 1,2. Areas with high use of injectables often overlap with areas of high HIV-1 incidence, particularly in eastern and southern Africa 3. Unfortunately, several studies have suggested that the use of hormonal contraceptives, particularly DMPA, is associated with an increased risk of acquiring and transmitting HIV-1 4-10. A recent observational study among HIV-1 serodiscordant couples indicated that the risk of acquiring HIV-1 was increased 2 to 3.9-fold in women using DMPA compared to non-hormonal contraception users 6,11. It has been estimated that injectable contraceptives may be responsible for 27,000-130,000 HIV-1 infections per year globally 3. However, the issue remains controversial as several studies failed to observe an overall effect of hormonal contraception on the incidence of HIV-1 infection or disease progression 9. Importantly, it has been estimated that removal of injectables from use in African countries without the majority of women switching to an equally effective contraception would lead to an increase in maternal deaths, outnumbering the number of HIV-1 infections averted 3,12. The World Health Organization has called for further research on possible links between hormonal contraceptives and HIV-1 acquisition and transmission 4.
Multiple studies have sought to understand the biological mechanisms underlying the effect of hormonal contraception on HIV-1 acquisition (reviewed in 7,13,14). Hormonal contraception use has been linked to changes in the frequencies of immune cells in genital mucosae 15-21 and altered levels of cytokines, chemokines, and antiviral factors in cervicovaginal fluid 22,23. Hormonal contraception use is associated with increased acquisition of cervical candidiasis, C. trachomatis, N. gonorrhoeae, and M. genitalium infections, which may independently facilitate HIV-1 acquisition and transmission 10,24-27. Studies using non-human primate models demonstrated that DMPA enhances the risk of simian immunodeficiency virus (SIV) acquisition via vaginal exposure (reviewed in 7,13). Medroxyprogesterone acetate (MPA), the contraceptive component of DMPA, was shown to suppress systemic regulators of cellular and humoral immunity, reduce cytokine production by plasmacytoid dendritic cells (pDCs), and increase the replication of HIV-1 in activated peripheral blood mononuclear cells (PBMCs) in vitro 28-32.
This study addresses the systemic and genital immune milieu in pre-menopausal women using DMPA, NuvaRing, or COCs. Circulating pDCs isolated from DMPA or NuvaRing users display decreased capacity to produce IFNα and TNFα following TLR-9, but not TLR7/8 stimulation. Furthermore, DMPA and NuvaRing use is associated with altered levels of immune mediators both systemically and in the cervicovaginal fluid. The presented data demonstrate that the use of contraceptives is linked to significant alterations of systemic and local immune environment; however, the implications of the observed changes for the transmission of HIV-1 warrant further investigation.
Methods
Volunteers and study design
A total of 84 female volunteers were recruited for this study from May 2011 to May 2012. Eligibility criteria included: age 19-40 years, using Depo Provera (intramuscular injection, 150 mg depot medroxyprogesterone acetate), combined oral contraceptives (COC) (ethinyl estradiol and variable progestin component), NuvaRing (vaginal ring, 0.12 mg etonogestrel and 0.015 mg ethinyl estradiol daily, on average) or not using any form of hormonal contraceptive (control group). Within the control group, 12 volunteers were assessed at the follicular and 12 at the luteal phase of the estrous cycle based of self-reported time since last menstrual period and 17β-estradiol (E2) and progesterone (P4) levels in plasma; 1 was not determined. Exclusion criteria included abnormal vaginal discharge, significant macroscopic vaginal pathology, any sign of bacterial vaginosis or infection, pregnancy, or current usage of an intrauterine device (IUD). The University of Alabama at Birmingham Institutional Review Board approved the study protocol and all subjects signed informed consent forms. Demographic, contraceptive, and STI histories were collected on standardized forms at enrollment. 20 mL of acid citrate dextrose (ACD)-treated blood was collected. A color pHast indicator strip (EMD Chemical, Gibbstown, NJ) was applied to the vaginal wall to determine intravaginal pH. Cervicovaginal lavage (CVL) was obtained by vigorous flushing of the cervix and vagina with 5 mL of sterile saline. The lavage fluid was subsequently mixed with protease inhibitors (5 ug/mL aprotinin, 1 ug/mL leupeptin, 1 ug/mL antipain, 1 ug/mL pepstain, 200 ug/mL sodium azide and 1 mM phenylmethylsulfonyl flouride; Sigma, St. Louis, MO) and cleared by centrifugation at 14,000 g for 5 minutes prior to cryopreservation.
Analysis of vaginal biopsies
A 1 cc lidocaine injection was applied and a full thickness biopsy was obtained from the lateral vaginal wall with Acu-Punch 8mm biopsy punch tool (Acuderm, Ft. Lauderdale, FL, USA). Biopsies were immediately washed with HBSS and orientated in OCT compound (Tissue-Tek, Sakura, Zoeterwoude, The Netherlands). Samples were snap-frozen by immersion in pre-cooled isopentane in an acetone bath encased with dry ice. Flash freezing of tissue used in this study has been noted to retain antigenicity, reduce tissue distortion, and preserve overall architecture 33. Samples were stored at -80°C until use. All sectioning was performed on a Leica CM1900 UV cryostat using pre-cleaned slides.
Immunofluorescence staining was performed to determine the location and density of immune cells in the vaginal epithelium. Sections were allowed to thaw for 30 seconds and blocked with a BSA-containing saponin buffer (2.5g BSA, 0.25g saponin per 250 mL phosphate buffered solution) for 1 hour. 30 μm sections from each biopsy were stained for Langerin (CD207 PE, Beckman Coulter, Brea, CA) and CD3 (rabbit anti-human C7930, Sigma, St. Louis, MO). 12 μm sections were stained for CD3 and CD4 (mouse anti-human NCL-CD4-368, Leica Microsystems, Milton Keynes, UK) or CD3 and CD8 (mouse anti-human NCL-CD8-4B11, Leica). Slides were incubated with primary antibodies at 4°C overnight, washed and incubated with secondary antibody (goat anti-rabbit Alexa 488 for CD3 or goat anti-mouse Alexa 555 for CD4/CD8, Invitrogen, Carlsbad, CA) for 2 hours at room temp, with subsequent fixation in 4% PFA for 10 min, 5 min Hoescht nuclear stain (Fisher Scientific, Pittsburgh, PA) and mounting in Flouro-Gel with TES buffer (EMS, Hatfield, PA). Images were taken on a Zeiss A1 Confocal microscope with Z stack analysis at 10x magnification. A minimum of 2 images at 10x magnification were analyzed per biopsy per stain. Reference points were plotted on each image along the apical side of the epithelium at 30 μm intervals. Coordinates for each Langerin+, CD3+, CD3+CD4+, or CD3+CD8+ cell were compared against the apical epithelium reference points to determine the distance using shortest distance using a specifically designed algorithm (http://shortdistance.imagejs.googlecode.com/git/shortdistance.html). Image analysis was performed with ImageJ64 open source software.
Cytokine and Ig analysis
Concentrations of 26 cytokines and chemokines in cervicovaginal lavage and plasma were determined using the 26-plex MILLIPLEX Human Cytokine/Chemokine Panel kit (Millipore, Billerica, MA). Samples were analyzed on a Bioplex 100 system with Bioplex Manager Software 5.0 (Biorad, Hercules, CA). IFNα levels in controls, DMPA, and COC users reported in this study partially overlap with a previously published data set 28. Concentrations of total IgA, IgM and IgG in CVL were determined with sandwich ELISA. In brief, 96 well plates were coated with 1 ug/ml polyclonal goat F(ab’)2 fragments of anti-human IgG, IgA, or IgM (Jackson Immunoresearch, West Grove, PA) in PBS, 100 µl per well, overnight at 4°C. Plates were washed with PBS containing 0.05 % Tween-20 (PBST), and blocked with 5% goat serum in PBST for IgA and IgM, or 1% BSA for IgG, 200 µl/well, 2 hours at room temperature. Samples and standards (Microgenetics, Fremont, CA) were prepared at appropriate dilutions in 2% goat serum in PBST for IgA and IgM, or 1% BSA in PBST for IgG. Block buffer was removed and sample and standard added, 100 µl per well, and incubated overnight at 4°C. After washing, biotinylated F(ab’)2 fragments of goat anti-human IgA (1:5000, KPL, Gaithersburg, MD), IgM (1:5000, KPL) or IgG (1:8000, Invitrogen, Camarillo, CA) were added, 100µl per well, and incubated for 1 hour at room temperature. Plates were washed followed by the addition of Streptavidin-conjugated peroxidase, (1:5000, Invitrogen, Carlsbad, CA), 100 µl per well, incubated at room temperature for 30 minutes. After the final wash SureBlue TMB peroxidase s ubstrate (KPL) was added, 100µl per well, incubated for 15 minutes at room temperature, after which the reaction was stopped by the addition of 100µl 1N HCl. Optical density values were determined at 450 nm.
Determination of hormonal concentration
400 uL plasma and 200 uL CVL samples from each patient were analyzed at the Obstetrics and Gynecology Laboratory at the University of Alabama at Birmingham to determine levels of 17β-estradiol (E2) and progesterone (P4). P4 and E2 were determined by the Access Progesterone assay and the Access Estrogen Assay respectively, (Beckman Coulter).
pDC activation and intracellular cytokine staining assay
pDC activation and cytokine production assays were performed as described 28,30. In brief, PBMCs (1.5 × 106 cells/ml) were stimulated with 5 µg/ml TLR7/8 ligand R848 (Invivogen, San Diego, CA) or 2 µM TLR9 ligand CpG ODN2216 (Hycult Biotech, Uden, The Netherlands) in the presence of 1 µl/ml of GolgiPlug (BD biosciences, San Diego, CA). After 20 hrs, cells were collected and stained for pDC markers (CD123-PE-Cy7 (eBioscience, San Diego, CA) and CD303-APC (BCDA-2; Miltenyi, Auburn, CA)). Cells were permeabilized using the Cytofix/Cytoperm kit (BD) and stained intracellularly with IFNα-PE (BD) and TNFα-FITC (eBioscience) mAbs. Samples were analyzed on LSR-II flow cytometer (BD) and data analysis was performed using the FACSDiva software (BD).
Analysis of memory and effector T cell subsets
0.5 × 106 isolated PBMCs were stained with anti-CD3-eFluor450, CD4-APC-eFluor780, CD8-PerCP-CY5.5, CD27-APC, CD45RO-PE, CD57-FITC, CD38-PE-Cy7 (eBioscience) to distinguish subsets. Appropriate isotype controls were used to determine the percentages of cells expressing the respective markers (Biolegend, San Diego, CA). Samples were analyzed on LSR-II flow cytometer (BD) and data analysis was performed using the FACSDiva software (BD).
Statistical Analysis
All data was stored in Microsoft Excel 2007 (Microsoft, Redmond, WA) and exported to GraphPad Prism (GraphPad Software, La Jolla, CA) for analysis. Statistical significance of the difference between experimental groups was determined using Mann-Whitney U test; correlations were determined using Spearman rank correlation test. A standard level of statistical significance α = 0.05 was used; all reported p-values are two-sided.
Results
To study the effect of hormonal contraception on the systemic and genital immune environment, 22 female volunteers using DMPA, 17 NuvaRing users, 17 combined oral contraceptives (COC) users, and 25 volunteers not using any form of hormonal contraceptives were recruited. Demographic data of the study population are listed in Table 1. The average age of the study population was 28 ±5.6 years; average BMI 31.1 ±8.4. Eleven (50%) of the women using DMPA had experienced amenorrhea for at least one month and up to 3 years before the date of sample collection. Women using any of the three forms of hormonal contraception displayed significantly reduced serum estrogen levels compared to controls (Table 1, p < 0.0001 for all groups). There were no significant correlations between collected immunological parameters and the demographic data.
Table 1.
Demographic data of study participants
| Control | DMPA | NuvaRing | COC | ||
|---|---|---|---|---|---|
| N | 26 | 22 | 17 | 17 | |
|
Median Age
(Range; Years) |
30 (19-39) | 26 (20-36) | 24 (19-39) | 29 (21-37) | |
|
Length of Contraceptive Use
(Range; Months) |
N/A | 20.6 (1-96) | 26.3 (3-96) | 70.0 (3-204) | |
| BMI | 32 ± 7.8 | 34 ± 9.7 | 28 ± 7.0 | 29 ± 8.1 | |
| History of Smoking | 8 (32%) | 5 (24%) | 4 (25%) | 1 (0.063%) | |
| Race | W* | 11 (42%) | 4 (18%) | 10 (59%) | 9 (53%) |
| B‡ | 15 (58%) | 18 (82%) | 7 (41%) | 8 (47%) | |
| BV§ History | 5 (19%) | 5 (23%) | 5 (29%) | 1 (0.6%) | |
| Vaginal pH | 5.1 ± 0.9 | 4.9 ± 0.9 | 4.5 ± 0.6 | 4.6 ± 0.4 | |
| Serum E2 (pg/mL) | 304 ± 130 | 141 ± 62.0 | 98 ± 35.1 | 139 ± 109 | |
| Serum P4 (ng/mL) | 5.5 ± 5.3 | 0.5 ± 0.5 | 0.4 ± 0.4 | 1.3 ± 0.8 | |
Unless otherwise indicated, data are presented as mean ± SD.
Self-identified race as W = White
Self-identified race as B = Black,
Self-identified race as BV = Bacterial Vaginosis.
Previous data from our laboratory have implicated MPA and etonogestrel, the progestin components of DMPA and NuvaRing, respectively, in impairing the cytokine response of pDCs to TLR-7/8 and TLR-9 stimulation in vitro 28,30. To assess pDC function in hormonal contraception users, PBMCs were isolated and stimulated with TLR-9 (CpG) or TLR-7/8 (R848) ligand for 20 hours. Intracellular production of IFNα and TNFα in CD123+ CD303+ pDC population was determined using polychromatic flow cytometry (Fig. 1A). pDCs from DMPA and NuvaRing users displayed impaired capacity to produce IFNα and TNFα following TLR-9 stimulation (Figure 1B,C). In contrast, hormonal contraceptive use did not affect pDC cytokine production following TLR-7/8-specific stimulation (Figure 1D, E). Within the control group, no statistically significant difference in pDC response was detected between volunteers in the follicular versus luteal phases of the menstrual cycle. No statistically significant correlation between 17β-estradiol (E2) and progesterone (P4) levels in plasma and pDC responses was detected in any of the experimental groups. Within the COC group, direct correlations between BMI and pDC production of IFNα (R = 0.67; p = 0.02) and TNFα (R = 0.6; p = 0.04) were observed; no correlations between BMI and pDC responses were observed in any other experimental group. Since pDCs represent the predominant immune cell producers of IFNα 34, we investigated whether the use of hormonal contraception alters plasma levels of IFNα or other chemokines and cytokines. The plasma levels of IFNα (Fig. 2A, p = 0.02) and IL-8 (Fig. 2B, p = 0.01) were significantly reduced in DMPA users. A marginally significant decrease in plasma levels of IL-6 was observed (data not shown); no alterations in plasma levels of IL-1β, IL-2, IL-10, IL-12, TNFα, IFNγ, G-CSF, CXCL10, or MCP-1 were detected. Within the DMPA group, direct correlations between the plasma levels of IL-8 and E2 (R = 0.5; p = 0.02) and between plasma levels of IL-8 and time since DMPA injection (0-90 days; R = 0.48; p = 0.03) were detected; no other correlations between plasma E2 and P4 and plasma cytokines levels in any of the experimental groups were observed. A direct correlation between the overall length of DMPA treatment (1 week to 36 months) and plasma GM-CSF was observed (R = 0.56; p = 0.03); no other cytokine has been correlated to the overall length of DMPA treatment. Hormonal contraception was not associated with any significant alterations in the distribution between naïve, effector, central memory, and effector memory subsets within the CD4+ and CD8+ T cell populations (Supplemental Figure 1). NuvaRing use was associated with an increased expression of activation marker CD38 on central memory (p = 0.006), effector memory (p = 0.006), and effector (p = 0.006) CD8+ T cell subsets; no alteration in the expression of T cell senescence marker CD57 was observed in any of the experimental groups (data not shown).
Figure 1. Plasmacytoid dendritic cells (pDCs) from NuvaRing and DMPA users display reduced ability to produce IFNα and TNFα in response to stimulation via TLR-9.
PBMCs were isolated from 20 control volunteers not using any form of hormonal contraception, 17 DMPA users, 14 NuvaRing users, and 13 COC users, and stimulated with 2 µM TLR-9 ligand CpG ODN2216 or 5µg/mL TLR-7/8 ligand R848. A) Gating strategy for the analysis of intracellular production of IFNα and TNFα in pDCs identified as CD123+ CD303+ population. B-E) Intracellular cytokine staining for IFNα (B, D) or TNFα (C, E) in pDCs was performed in PBMCs stimulated with CpG (B,C) or R848 (D,E). Values are corrected for background staining of unstimulated cells. Bars indicate median values; statistical significance was determined using the Mann-Whitney U test.
Figure 2. DMPA use is associated with lower levels of plasma IFNα and IL-8.
Plasma from 21 control volunteers, 19 DMPA, 14 NuvaRing, and 14 COC users were analyzed for the concentrations of IFNα (A) and IL-8 (B). Bars indicate median values; significance was determined using the Mann-Whitney U test.
As alterations to the immune milieu of the female reproductive tract (FRT) may have a significant effect on HIV-1 acquisition and transmission 35, the effects of hormonal contraception on the genital immune milieu were investigated. Analysis of cytokine and chemokine levels in the cervicovaginal lavage (CVL) of hormonal contraception users demonstrated that DMPA use is associated with significantly reduced levels of IFNα (p = 0.03), CXCL10 (p = 0.008), MCP-1 (p = 0.0009), and G-CSF (p = 0.006; Figure 3). Within the control group, no statistically significant difference in the levels of these cytokines was detected between volunteers in the follicular versus luteal phases of the menstrual cycle. The concentration of other immune mediators detected at high levels in the CVL, including IL-1β, IL-8, IL-6, and MIP-1β, did not differ among experimental groups (Supplemental Figure 2A). DMPA use was associated with decreased CVL levels of IgG (p = 0.02); COC use was associated with decreased levels of IgA (p = 0.02) (Supplemental Figure 2B). No statistically significant correlation between the FRT levels of immunoglobulins and E2 and P4 levels in plasma was detected. Within the control group, significant negative correlations were detected between the plasma level of P4 and CVL levels of G-CSF (R = -0.57; p = 0.01), GM-CSF (R = -0.51; p = 0.02), 1-12 p40 (R = -0.49; p = 0.03), IL-12 p70 (R = -0.47; p = 0.04), IL-15 (R = -0.7; p = 0.0008), IL-17 (R = -0.66; p = 0.01), MCP-1 (R = -0.55; p = 0.01), and TNFα (R = -0.49; p = 0.03). No other statistically significant correlations between plasma levels of E2 and P4 and cytokine levels in CVL were observed in any of the experimental groups. A positive correlation between the BMI and IFNα level in the CVL was observed in the control group (R = 0.64; p = 0.004). Within the DMPA group, CVL levels of MCP-1 correlated with the time since last DMPA injection (R = 0.47; p = 0.04); no other statistically significant correlation between the time from last DMPA injection or the overall length of DMPA treatment versus cytokine production by pDCs or cytokine levels in plasma and cervicovaginal fluid was observed.
Figure 3. DMPA use is associated with lower levels of IFNα, CXCL10, MCP-1, G-CSF, TIMP-1 and TIMP-2 in the cervicovaginal fluid.
Cervicovaginal lavages from 21 controls, 20 DMPA, 14 NuvaRing, and 14 COC users were analyzed for chemokine, cytokine, MMP-7 and -9, and TIMP-1 and -2 concentrations. Bars indicate median values; significance was established using Mann-Whitney U test.
Matrix metalloproteinase (MMPs) and their tissue inhibitors (TIMPs) affect chemokine processing and epithelial tissue remodeling 36. MMPs and TIMPs are highly expressed in reproductive tissues and are hormonally regulated throughout the menstrual cycle 37. In CVLs of subjects of all experimental groups, the predominant metalloproteinases were MMP-9, MMP-7, MMP-2, MMP-12, and MMP-10, in descending order of concentration, (Figure 3G-H and data not shown). The use of DMPA was associated with reduced CVL levels of TIMP-1 (Figure 3E, p = 0.02) and TIMP-2 (Figure 3F, p = 0.02); NuvaRing users displayed reduced levels of TIMP-2 (Figure 3F, p = 0.01). TIMP-1 and TIMP-2 display broad inhibitory activity against most MMPs 38; thus, a decrease in TIMP concentration is consistent with an increase in the overall activity of MMPs in the genital tract. Within the control group, no statistically significant correlations between the CVL levels of MMPs and TIMPs and plasma levels of E2 and P4 were detected. A positive correlation between the BMI and CVL TIMP-1 level was observed in the control group (R = 0.64; p = 0.01).
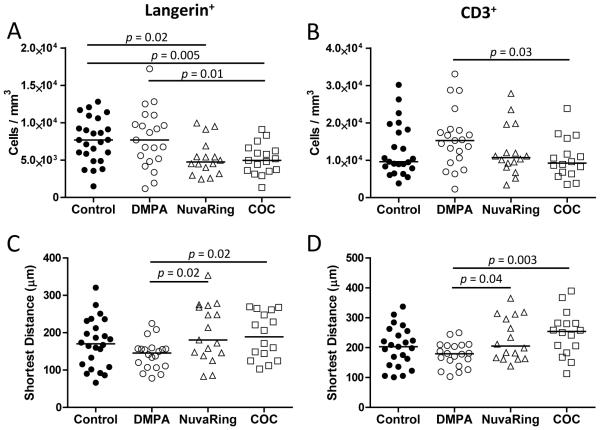
Langerhans cells (LCs) represent the main dendritic cell population of the vaginal epithelium 39. Experimental evidence suggests that vaginal LCs pass infectious HIV virions to CD4+ T cells without being productively infected; however, the issue remains controversial 40. To address the effect of hormonal contraception on immune cell populations in the lower FRT, the frequency and distribution of vaginal intraepithelial CD207+ LCs (Fig. 4A, C) and CD3+ T cells (Fig. 4B,D) were determined in vaginal biopsies of hormonal contraceptive users. The frequency of intraepithelial LCs was significantly decreased in both COC and NuvaRing users compared to either DMPA users or controls (Figure 4A). However, no significant difference in LC density was detected between DMPA users and controls, consistent with previous studies 19-21,41. A trend toward increased CD3+ cell density in DMPA users compared to controls was detected (Figure 4C); however, the trend did not reach statistical significance. Specific analysis of the frequency of CD3+CD4+ and CD3+CD8+ T cell subsets did not reveal any statistically significant differences between controls and the experimental groups (Supplemental Figure 3). LCs and CD3+ cells were localized closer to the apical epithelial surface in women using DMPA compared to women using NuvaRing or COCs (Figure 4B); the difference compared to control group did not reach statistical significance. Within the control group, no statistically significant correlations between the intraepithelial immune cell frequencies, plasma levels of E2 and P4, BMI, and age were detected. No differences were observed among volunteers in the follicular versus luteal phases of the estrous cycle, in concordance with previous studies 16,21.
Figure 4. Density and shortest apical distance of vaginal intraepithelial Langerhans and CD3+ T cells are altered in users of hormonal contraception.
Vaginal biopsies obtained from DMPA, NuvaRing, and COC users and control volunteers were sectioned at 30 µm and stained for CD207+ Langerhans cells (A, C) and CD3+ T cells (B,D). Intraepithelial density (A,B) and shortest distance to the apical epithelial surface (C,D) of Langerin+ (A, C) and CD3+ (B, D) cells was analyzed. Bars indicate median value for each group; significance was determined using Mann-Whitney U test.
Discussion
In light of multiple studies implicating hormonal contraception use with increased susceptibility to HIV-1 infection 5-11, identifying safe and effective contraceptives is a critical public health issue 4. This study examined alterations to systemic and local immune mediators associated with extended use of hormonal contraception in order to delineate biological mechanisms that may affect the susceptibility to HIV-1 and other sexually transmitted diseases. The study reveals four major findings: (i) The use of DMPA or NuvaRing is associated with reduced capacity of circulating pDCs to produce IFNα and TNFα in response to stimulation via TLR-9; (ii) Systemic and cervicovaginal levels of IFNα are lower in DMPA users compared to controls not using hormonal contraception; (iii) Cervicovaginal levels of CXCL10, MCP-1 and G-CSF are lower in DMPA users; and (iv) The frequency of CD207+ Langerhans cells in the vaginal epithelium is reduced in NuvaRing and COC users.
pDCs play a key role in the early recognition of viral and bacterial infections and represent a major source of IFNα in vivo 34,42,43. IFNα-producing pDCs accumulate in the genital lamina propria one day following SIV infection in macaques 34. Previous research from our laboratory demonstrated that in vitro incubation of pDCs with physiological concentrations of MPA results in an impaired response to stimulation via TLR7/8- and TLR9. In contrast, etonogestrel, the progestin component of NuvaRing, exerted inhibitory effect only at high concentrations 28,30. Data presented here demonstrate that pDCs freshly isolated from DMPA or NuvaRing users display an impaired IFNα or TNFα response following TLR9 but not TLR7/8 stimulation. This observation, corroborated by lower plasma and CVL levels of IFNα in DMPA users (Figure 2A), indicates partial functional impairment of pDCs in DMPA and NuvaRing users. Suppression of pDC function may tip the balance between the proliferation of a founder viral population and early immune control during the acute phase of infection in favor of the transmitted virus. The reasons for the observed differences between the effect of various progestins on immune mechanisms in vitro and in vivo are unclear. Plausible causes include differences in serum concentration, bioavailability, and differences in affinities of binding to glucocorticoid receptor and other members of the steroid receptor family 7,28,30,44-46.
Levels of cervicovaginal CXCL10, G-CSF, MCP-1, TIMP-1 and TIMP-2 were reduced in DMPA users. CXCL10, G-CSF and MCP-1 play a role in recruiting monocytes, neutrophils, and T lymphocytes to sites of infection and are produced in significant quantities in the uterine and endocervical tissues 47. This data is consistent with previous observation that MPA inhibits CXCL10 and MCP-1 production by activated PBMCs 30. Reduced levels of these factors in the cervicovaginal fluid may result in an altered frequency and/or activation status of immune cells within the genital mucosae.
Previous research on vaginal immune cell populations in hormonal contraception users has been conflicting, with some studies noting a decrease in CD1a+ Langerhans cell density in DMPA users 15 and other studies showing no change in CD1a+ Langerhans cells in COC or DMPA users 21. Topical progesterone was found to increase CD1a+ DC populations in the vaginal epithelium 18. Studies using S-100 as a marker for vaginal Langerhans cells have uniformly noted no difference between DMPA users and controls 19,20,41. The data presented here demonstrate significant decreases in CD207+ Langerhans cell density in NuvaRing and COC users, but not in DMPA users. As it has been previously suggested that subsets of vaginal LCs differ in their expression of CD207 40, differences in experimental approaches and population markers may account for the differences between this work and previous studies. Conflicting results have been reported regarding the alterations to vaginal lymphocytes in hormonal contraception users, with some studies finding an increase in vaginal CD3+, CD8+, and CD4+CCR5+ cells 16 and other reporting no change or decrease in the frequency of these populations 15,19-21. Here we report no significant alterations to vaginal CD3+, CD3+CD8+, or CD3+CD4+ lymphocyte population density or localization in DMPA users. Thus, DMPA does not appear to increase the frequency of HIV-1 target cells in vaginal mucosa.
Some of the observed changes in immune parameters in DMPA users may be related to chronic anovulation and reduced concentration of endogenous estrogen rather than a direct effect of DMPA. Furthermore, immune mechanisms may be affected by MPA concentration that peaks at 1-2 weeks post DMPA injection and decreases at the end of the 3 month administration period. This study addressed the effect of the overall length of DMPA use (1 week to 96 months) and the effect of the time since last DMPA injection. We observed a direct correlation between the overall length of DMPA treatment and plasma levels of GM-CSF and a correlation between the time since last DMPA injection and CVL levels of MCP-1; no other statistically significant correlations between the overall length of DMPA treatment and the time from last DMPA injection in relation to any other immune parameter including cytokine production by pDCs and immune cell population densities in vaginal mucosa were observed. A positive correlation between the plasma levels of E2 versus IL-8 was observed within the DMPA group. No other correlation between plasma E2 and plasma and CVL cytokines levels, pDC function, and intraepithelial layer cell frequencies were observed in any of the experimental groups.
This study is subject to limitations, including small sample size overall and within each contraceptive group. Volunteers were not eligible if macroscopic genital inflammation was detected; however, potential effects mediated by previous or ongoing genital infections cannot be excluded. Frequency or last instance of intercourse were not considered in the analysis; these factors may influence the localization and density of immune cells. There was a bias within DMPA users towards volunteers of African descent (82%). No significant correlations between race and immune parameters including cell density, cell localization, or cytokine and chemokine levels were observed.
In summary, the presented data suggest that hormonal contraceptives modulate pDC function and levels of systemic and genital immune mediators. This adds to the growing amount of evidence of the biological effect of progestins on the immune system and on the immune environment in lower FRT 7,13,14. However, it remains to be established whether the contraceptive-mediated alterations to systemic and genital immune mechanisms described here and in other studies exert an effect on the susceptibility to HIV-1 and other infections. Additional research into the biological effect of hormonal contraception on the immune system is critical for evidence-based selection of safe forms of contraceptives for women at risk of HIV-1. Women using hormonal contraceptives should be advised to use male or female condoms and practice additional HIV prevention strategies as recommended by WHO guidelines 4.
Supplementary Material
Acknowledgments
We thank Dr. Jonas Almeida at the University of Alabama at Birmingham for developing the macro used for image analysis of cell localization.
Financial support. This work was supported by National Institute of Allergy and Infectious Diseases of the National Institutes of Health under award number P01 AI083027 and AI103401. UAB Center for AIDS Research (funded by NIH grant P30 AI027767) Flow Cytometry Core was instrumental with flow cytometry and cytokine analyses. K.G.M. was supported in part by NIH grant 5T32A1007493-19. Biomedical research space used for this study was constructed with funds supported in part by NIH grant RR-20136.
This work was supported by National Institutes of Health grants AI083027, AI103401, AI027767, RR-20136, and A1007493-19.
Footnotes
Disclosure Summary: The authors declare no competing interests.
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.United Nations, Department of Economic and Social Affairs, Population Division World Contraceptive Use 2012. UN Report 2012. http://www.un.org/esa/population/publications/WCU2012/MainFrame.html. Accessed Jan 28, 2014.
- 2.Affandi B. Injectable contraceptives: a worldwide perspective. The journal of family planning and reproductive health care / Faculty of Family Planning & Reproductive Health Care, Royal College of Obstetricians & Gynaecologists. 2002;28:3–4. doi: 10.1783/147118902101195794. [DOI] [PubMed] [Google Scholar]
- 3.Butler AR, Smith JA, Polis CB, et al. Modelling the global competing risks of a potential interaction between injectable hormonal contraception and HIV risk. AIDS. 2013;27:105–113. doi: 10.1097/QAD.0b013e32835a5a52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hormonal contraception and HIV . Technical statement. World Health Organization; 2012. http://www.who.int/reproductivehealth/publications/family_planning/rhr_12_8/en/index.html. Accessed August 11, 2012. [PubMed] [Google Scholar]
- 5.Baeten JM, Benki S, Chohan V, et al. Hormonal contraceptive use, herpes simplex virus infection, and risk of HIV-1 acquisition among Kenyan women. AIDS. 2007;21:1771–1777. doi: 10.1097/QAD.0b013e328270388a. [DOI] [PubMed] [Google Scholar]
- 6.Heffron R, Donnell D, Rees H, et al. Use of hormonal contraceptives and risk of HIV-1 transmission: a prospective cohort study. The Lancet infectious diseases. 2012;12:19–26. doi: 10.1016/S1473-3099(11)70247-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hel Z, Stringer E, Mestecky J. Sex steroid hormones, hormonal contraception, and the immunobiology of human immunodeficiency virus-1 infection. Endocrine reviews. 2010;31:79–97. doi: 10.1210/er.2009-0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morrison CS, Chen PL, Kwok C, et al. Hormonal contraception and HIV acquisition: reanalysis using marginal structural modeling. AIDS. 2010;24:1778–1781. doi: 10.1097/QAD.0b013e32833a2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polis CB, Curtis KM. Use of hormonal contraceptives and HIV acquisition in women: a systematic review of the epidemiological evidence. The Lancet infectious diseases. 2013;13:797–808. doi: 10.1016/S1473-3099(13)70155-5. [DOI] [PubMed] [Google Scholar]
- 10.Wand H, Ramjee G. The effects of injectable hormonal contraceptives on HIV seroconversion and on sexually transmitted infections. AIDS. 2012;26:375–380. doi: 10.1097/QAD.0b013e32834f990f. [DOI] [PubMed] [Google Scholar]
- 11.Heffron R, Rees H, Mugo N, et al. Use of hormonal contraceptives and risk of HIV-1 transmission - Authors' reply. The Lancet infectious diseases. 2012;12:510–511. doi: 10.1016/S1473-3099(12)70115-9. [DOI] [PubMed] [Google Scholar]
- 12.Rodriguez M, Reeves M, Caughey A. Evaluating the competing risks of HIV acquisition and maternal mortality in Africa: a decision analysis. BJOG : an international journal of obstetrics and gynaecology. 2012;119:1067–1073. doi: 10.1111/j.1471-0528.2012.03402.x. [DOI] [PubMed] [Google Scholar]
- 13.Murphy K, Irvin SC, Herold BC. Research Gaps in Defining the Biological Link between HIV Risk and Hormonal Contraception. American journal of reproductive immunology. 2014 doi: 10.1111/aji.12209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hapgood JP. Immunosuppressive biological mechanisms support reassessment of use of the injectable contraceptive medroxyprogesterone acetate. Endocrinology. 2013;154:985–988. doi: 10.1210/en.2013-1066. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell CM, McLemore L, Westerberg K, et al. Long-term Effect of Depot Medroxyprogesterone Acetate on Vaginal Microbiota, Epithelial Thickness and HIV Target Cells. J Infect Dis. 2014 doi: 10.1093/infdis/jiu176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chandra N, Thurman AR, Anderson S, et al. Depot Medroxyprogesterone Acetate Increases Immune Cell Numbers and Activation Markers in Human Vaginal Mucosal Tissues. AIDS research and human retroviruses. 2012 doi: 10.1089/aid.2012.0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ghanem KG, Shah N, Klein RS, et al. Influence of sex hormones, HIV status, and concomitant sexually transmitted infection on cervicovaginal inflammation. J Infect Dis. 2005;191:358–366. doi: 10.1086/427190. [DOI] [PubMed] [Google Scholar]
- 18.Wieser F, Hosmann J, Tschugguel W, et al. Progesterone increases the number of Langerhans cells in human vaginal epithelium. Fertil.Steril. 2001;75:1234–1235. doi: 10.1016/s0015-0282(01)01796-4. [DOI] [PubMed] [Google Scholar]
- 19.Mauck CK, Callahan MM, Baker J, et al. The effect of one injection of Depo-Provera on the human vaginal epithelium and cervical ectopy. Contraception. 1999;60:15–24. doi: 10.1016/s0010-7824(99)00058-x. [DOI] [PubMed] [Google Scholar]
- 20.Bahamondes MV, Castro S, Marchi NM, et al. Human vaginal histology in long-term users of the injectable contraceptive depot-medroxyprogesterone acetate. Contraception. 2014 doi: 10.1016/j.contraception.2014.01.024. [DOI] [PubMed] [Google Scholar]
- 21.Ildgruben AK, Sjoberg IM, Hammarstrom ML. Influence of hormonal contraceptives on the immune cells and thickness of human vaginal epithelium. Obstet.Gynecol. 2003;102:571–582. doi: 10.1016/s0029-7844(03)00618-5. [DOI] [PubMed] [Google Scholar]
- 22.Morrison C, Fichorova RN, Mauck C, et al. Cervical inflammation and immunity associated with hormonal contraception, pregnancy, and HIV-1 seroconversion. J Acquir Immune Defic Syndr. 2014;66:109–117. doi: 10.1097/QAI.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 23.Fleming DC, King AE, Williams AR, et al. Hormonal contraception can suppress natural antimicrobial gene transcription in human endometrium. Fertility and sterility. 2003;79:856–863. doi: 10.1016/s0015-0282(02)04930-0. [DOI] [PubMed] [Google Scholar]
- 24.Baeten JM, Nyange PM, Richardson BA, et al. Hormonal contraception and risk of sexually transmitted disease acquisition: results from a prospective study. Am.J Obstet.Gynecol. 2001;185:380–385. doi: 10.1067/mob.2001.115862. [DOI] [PubMed] [Google Scholar]
- 25.Hancock EB, Manhart LE, Nelson SJ, et al. Comprehensive assessment of sociodemographic and behavioral risk factors for Mycoplasma genitalium infection in women. Sexually transmitted diseases. 2010;37:777–783. doi: 10.1097/OLQ.0b013e3181e8087e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lavreys L, Chohan V, Overbaugh J, et al. Hormonal contraception and risk of cervical infections among HIV-1-seropositive Kenyan women. AIDS. 2004;18:2179–2184. doi: 10.1097/00002030-200411050-00010. [DOI] [PubMed] [Google Scholar]
- 27.Morrison CS, Bright P, Wong EL, et al. Hormonal contraceptive use, cervical ectopy, and the acquisition of cervical infections. Sex Transm.Dis. 2004;31:561–567. doi: 10.1097/01.olq.0000137904.56037.70. [DOI] [PubMed] [Google Scholar]
- 28.Huijbregts RP, Helton ES, Michel KG, et al. Hormonal contraception and HIV-1 infection: medroxyprogesterone acetate suppresses innate and adaptive immune mechanisms. Endocrinology. 2013;154:1282–1295. doi: 10.1210/en.2012-1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hughes GC, Thomas S, Li C, et al. Cutting edge: progesterone regulates IFN-alpha production by plasmacytoid dendritic cells. J Immunol. 2008;180:2029–2033. doi: 10.4049/jimmunol.180.4.2029. [DOI] [PubMed] [Google Scholar]
- 30.Huijbregts RP, Michel KG, Hel Z. Effect of progestins on immunity: medroxyprogesterone but not norethisterone or levonorgestrel suppresses the function of T cells and pDCs. Contraception. 2014 doi: 10.1016/j.contraception.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kleynhans L, Du Plessis N, Black GF, et al. Medroxyprogesterone acetate alters Mycobacterium bovis BCG-induced cytokine production in peripheral blood mononuclear cells of contraceptive users. PLoS One. 2011;6:e24639. doi: 10.1371/journal.pone.0024639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hapgood JP, Ray RM, Govender Y, et al. Differential glucocorticoid receptor-mediated effects on immunomodulatory gene expression by progestin contraceptives: implications for HIV-1 pathogenesis. American journal of reproductive immunology. 2014;71:505–512. doi: 10.1111/aji.12214. [DOI] [PubMed] [Google Scholar]
- 33.Erickson QL, Clark T, Larson K, et al. Flash freezing of Mohs micrographic surgery tissue can minimize freeze artifact and speed slide preparation. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.] 2011;37:503–509. doi: 10.1111/j.1524-4725.2011.01926.x. [DOI] [PubMed] [Google Scholar]
- 34.Li Q, Estes JD, Schlievert PM, et al. Glycerol monolaurate prevents mucosal SIV transmission. Nature. 2009;458:1034–1038. doi: 10.1038/nature07831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hladik F, McElrath MJ. Setting the stage: host invasion by HIV. Nat.Rev.Immunol. 2008;8:447–457. doi: 10.1038/nri2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khokha R, Murthy A, Weiss A. Metalloproteinases and their natural inhibitors in inflammation and immunity. Nature reviews. Immunology. 2013;13:649–665. doi: 10.1038/nri3499. [DOI] [PubMed] [Google Scholar]
- 37.Curry TE, Jr., Osteen KG. The matrix metalloproteinase system: changes, regulation, and impact throughout the ovarian and uterine reproductive cycle. Endocrine reviews. 2003;24:428–465. doi: 10.1210/er.2002-0005. [DOI] [PubMed] [Google Scholar]
- 38.Murphy G. Tissue inhibitors of metalloproteinases. Genome biology. 2011;12:233. doi: 10.1186/gb-2011-12-11-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miller CJ, McChesney M, Moore PF. Langerhans cells, macrophages and lymphocyte subsets in the cervix and vagina of rhesus macaques. Lab Invest. 1992;67:628–634. [PubMed] [Google Scholar]
- 40.Ballweber L, Robinson B, Kreger A, et al. Vaginal langerhans cells nonproductively transporting HIV-1 mediate infection of T cells. J Virol. 2011;85:13443–13447. doi: 10.1128/JVI.05615-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bahamondes L, Trevisan M, Andrade L, et al. The effect upon the human vaginal histology of the long-term use of the injectable contraceptive Depo-Provera. Contraception. 2000;62:23–27. doi: 10.1016/s0010-7824(00)00132-3. [DOI] [PubMed] [Google Scholar]
- 42.Gilliet M, Cao W, Liu YJ. Plasmacytoid dendritic cells: sensing nucleic acids in viral infection and autoimmune diseases. Nature reviews. Immunology. 2008;8:594–606. doi: 10.1038/nri2358. [DOI] [PubMed] [Google Scholar]
- 43.Siegal FP, Kadowaki N, Shodell M, et al. The nature of the principal type 1 interferon-producing cells in human blood. Science. 1999;284:1835–1837. doi: 10.1126/science.284.5421.1835. [DOI] [PubMed] [Google Scholar]
- 44.Africander D, Verhoog N, Hapgood JP. Molecular mechanisms of steroid receptor-mediated actions by synthetic progestins used in HRT and contraception. Steroids. 2011;76:636–652. doi: 10.1016/j.steroids.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 45.Stanczyk FZ, Hapgood JP, Winer S, et al. Progestogens used in postmenopausal hormone therapy: differences in their pharmacological properties, intracellular actions, and clinical effects. Endocrine reviews. 2013;34:171–208. doi: 10.1210/er.2012-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koubovec D, Ronacher K, Stubsrud E, et al. Synthetic progestins used in HRT have different glucocorticoid agonist properties. Mol.Cell Endocrinol. 2005;242:23–32. doi: 10.1016/j.mce.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 47.Fahey JV, Schaefer TM, Channon JY, et al. Secretion of cytokines and chemokines by polarized human epithelial cells from the female reproductive tract. Human reproduction. 2005;20:1439–1446. doi: 10.1093/humrep/deh806. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.