Abstract
Objective
To examine the impacts of job insecurity during the recession of 2007–2009 on health care utilization among a panel of U.S. employees.
Data Sources/Study Setting
Linked administrative and claims datasets on a panel of continuously employed, continuously insured individuals at a large multisite manufacturing firm that experienced widespread layoffs (N = 9,486).
Study Design
We employed segmented regressions to examine temporal discontinuities in utilization during 2006–2012. To assess the effects of job insecurity, we compared individuals at high‐ and low‐layoff plants. Because the dataset includes multiple observations for each individual, we included individual‐level fixed effects.
Principal Findings
We found discontinuous increases in outpatient (3.5 visits/month/10,000 individuals, p = .002) and emergency (0.4 visits/month/10,000 individuals, p = .05) utilization in the panel of all employees. Compared with individuals at low‐layoff plants, individuals at high‐layoff plants decreased outpatient utilization (−4.0 visits/month/10,000 individuals, p = .008), suggesting foregone preventive care, with a marginally significant increase in emergency utilization (0.4 visits/month/10,000 individuals, p = .08).
Conclusions
These results suggest changes in health care utilization and potentially adverse impacts on employee health in response to job insecurity during the latest recession. This study contributes to our understanding of the impacts of economic crises on the health of the U.S. working population.
Keywords: Health care utilization, job insecurity, mass layoffs, panel study, workplace
Job insecurity refers to an individual's perception of a threat to his or her employment and the anticipation of job loss (Sverke and Hellgren 2002). Prior research has demonstrated that subjective job insecurity brings about worsened physical and mental health among affected individuals (Ferrie et al. 2002; Sverke, Hellgren, and Naswall 2002). Objective measures of job insecurity, such as the occurrence of downsizing or local mass layoffs, have also been associated with higher work‐related stress (Dragano, Verde, and Siegrist 2005), decreased job satisfaction (Heaney, Israel, and House 1994), and worsened health among surviving employees (Kivimäki et al. 2003; Vahtera et al. 2004; Martikainen, Maki, and Jantti 2008; Modrek and Cullen 2013b).
A related literature addresses the health effects of recessions and economic downturns. Several comprehensive reviews of this literature exist (Catalano et al. 2011; Modrek et al. 2013). Studies on the effects of recessions often focus on the effects among unemployed individuals or at the population level, with fewer studies examining outcomes specifically among employed individuals; job insecurity may be more pronounced among surviving employees if the economy is in recession, as labor markets are weaker and other employment opportunities may be limited (Modrek et al. 2013). A study by the American Life Panel Survey during 2008–2010 found that employees consistently overestimated their likelihood of unemployment (Hurd and Rohwedder 2010). Therefore, it is important to specifically examine the health impacts of job insecurity during economic downturns. For example, during the “Great Recession” of 2007–2009, studies have shown increased incidence of hypertension and diabetes among surviving employees at high‐layoff firms (Modrek and Cullen 2013a), as well as increased use of mental health treatments (Modrek, Hamad, and Cullen 2015).
Notably absent from this literature is an examination of the impacts of mass layoffs and job insecurity on health care utilization, although prior work has examined utilization during recessions more generally. For the purposes of this literature review, we include studies that employ both objective and subjective measures of job insecurity. Studies of health care utilization provide insight into health‐seeking behavior in response to financial and psychological threats (actual or anticipated). For example, Roehrig et al. (2012) identified a decrease in the U.S. national expenditure on health during the Great Recession. This may suggest a possible decline in the need for services, as some studies have reported improved health during recessions (Miller et al. 2009). Supporting this hypothesis, studies found decreased health care utilization during the Great Recession based on reports from insurers and health care providers (American Academy of Family Physicians 2009; American Hospital Association 2009; Johnson, Rockoff, and Mathews 2010). Yet it is possible that lower expenditures are due to patients foregoing care, as prior work has found decreased cancer screening during economic downturns (Catalano, Satariano, and Ciemins 2003; Dorn et al. 2012). Other studies have documented greater utilization of outpatient and emergency room (ER) visits among those whose homes were recently foreclosed upon and increased hospitalizations among the elderly during the Great Recession, as well as increased outpatient utilization more generally, suggesting that utilization changes may reflect worsening health in response to economic downturns (Pollack et al. 2011; McInerney and Mellor 2012; Du and Yagihashi 2015). These conflicting findings may be due to limitations in methodologies; for example, surveys of insurers likely suffer from survivorship bias as laid‐off workers lose their private insurance. Alternatively, it may be that population‐level studies mask the presence of heterogeneous effects on different subgroups due to differences in the degree of job insecurity. Almost without exception, these studies have examined the effects on utilization of macroeconomic changes, rather than the impacts of an individual's more immediate environment.
In this study, we examined health care utilization trends among a panel of continuously employed, continuously insured workers at a large U.S. manufacturing firm in the hopes of clarifying the impacts of job insecurity on health and health‐seeking behavior during recessions. We used mass layoffs at an individual's place of work as an objective measure of his or her job insecurity, as mass layoffs have been associated in prior work with increased subjective job insecurity among surviving employees (Kivimäki et al. 2000). We hypothesized that job insecurity at the firm brought about changes in health care utilization among employees, especially those with heightened job insecurity (i.e., those working in plants with relatively more layoffs). The direction of this change was a priori unclear: economic forces such as reduced household income or fear or unemployment may lead to decreased utilization in the context of avoidance of absenteeism; meanwhile, worsening health due to increased job demands or physiological stress might lead to increased utilization (Catalano 2009). To test this hypothesis, we explored patterns in outpatient, ER, and inpatient utilization. Furthermore, we investigated pathways through which health may be impacted. That is, we examined the impacts of job insecurity on medication adherence and foregone preventive care, to test the hypothesis that economic hardship led to an inappropriate decrease in utilization. We also examined whether there were changes in utilization specifically among those with preexisting poor health, to evaluate whether the trends we observed were driven by this high‐risk subgroup.
Methods
Dataset
Our sample was constructed using administrative and claims datasets from a multisite U.S. manufacturing firm that experienced widespread layoffs during the Great Recession. These data are available to researchers through an ongoing collaboration between the investigators and the firm under study, and they have been described in detail in previous publications (Cullen et al. 2006). Our panel included 9,486 employees who were continuously employed from January 2006 to December 2012 at the 26 largest plants in 15 states nationwide (Table 1). These plants were those for which reliable administrative data were available during the study period. In this sample, all were continuously covered by similar insurance plans with comprehensive health care benefits. Insurance plans underwent only minor design changes during the study period. Approximately 97 percent of employees at this firm selected this insurance coverage, with the remaining 3 percent electing coverage from a separate health maintenance organization (HMO) plan; the latter data were not available to us. All variables were derived from these linked datasets, and there were no missing data.
Table 1.
Panel Characteristics* (2006–2012)
| Employees (N = 9,486) | |
|---|---|
| Female (%) | 18.9 |
| Age in 2006, mean (SD) | 45.3 (8.0) |
| Race (%) | |
| White | 82.5 |
| Black | 8.6 |
| Hispanic | 6.0 |
| Other | 2.9 |
| Employed at high‐layoff plant† (%) | 55.6 |
| Risk score‡ (%) | |
| 0–1 | 67.6 |
| 1–2 | 24.5 |
| 2–4 | 7.9 |
*Inclusion criteria: continuous employment and continuous insurance coverage during study period.
†High‐layoff plants are those in which at least 40 individuals were terminated in a single day.
‡A score of 1 indicates that the individual's health expenditures are likely to fall at the mean in the following year, with each unit increase predicting a one‐fold increase in expenditures above the mean.
Measures
Utilization data included detailed information from each medical encounter and prescription drug claims. The latter included prescriptions that were filled by the individual, but not those that were prescribed and never filled. Using current procedural terminology (CPT) codes, we enumerated how many encounters an individual had in each month in three domains: outpatient physician clinic visits, ER visits, and inpatient hospitalizations. Thus, our primary outcome variables measured the number of visits per person per month in a given domain. Outcomes were reported per 10,000 individuals to facilitate interpretation of the magnitude of the observed relationships.
To examine the effects of job insecurity more locally, we used the personnel dataset to determine the presence of mass layoffs at each site, defined as 40 or more individuals terminated on a given day. This represented a natural break in the data and is similar to definitions used in prior studies and by the Bureau of Labor Statistics (Bureau of Labor Statistics 2013b; Modrek and Cullen 2013a). Eight of the 26 plants experienced mass layoffs, with the first in January 2009 and the last in March 2010. Surviving employees at these plants were assumed to experience greater job insecurity compared to those at other plants. While this approach does not capture employees’ perceived or subjective job insecurity, it has been used in prior studies as an objective measure (Vahtera et al. 2004; Martikainen, Maki, and Jantti 2008). As it captures changes in the employee's immediate environment, it may more accurately represent perceived job insecurity, as compared to state‐level unemployment rates used in other studies.
Using prescription claims data, we calculated medication adherence for each individual. We considered four categories of medications: (1) beta‐blockers and (2) angiotensin‐converting enzyme (ACE) inhibitors and angiotensin‐receptor blockers (ARBs) for hypertension, (3) statins for high cholesterol, and (4) controller medications for asthma and chronic obstructive pulmonary disease (COPD). We chose these medications because the drugs in these categories are seldom used to treat other conditions, and because adherence is important in the treatment of chronic disease. For each category, we calculated the medication possession ratio (MPR), dividing the number of days’ supply of the medication the individual filled in that year by 360. This measure denotes the percentage of the medication that an individual filled in a given year, a method employed to measure adherence in prior studies (Hill et al. 2013).
We also examined whether changes in utilization were more pronounced among those who were more ill at baseline. To classify individuals by health status, we used a third‐party algorithm (DxCG Software; Verisk Health Inc, Jersey City, New Jersey, USA) to compute a health risk stratification score for each individual at baseline in 2006. This score was computed using an individual's historical CPT and International Classification of Diseases codes and use of health care services. A score of 1 indicates that the individual's health expenditures are likely to fall at the mean in the following year. Each unit increase predicts a one‐fold increase in expenditures above the mean. This score predicts a variety of health outcomes (Handel 2011; Modrek and Cullen 2012, 2013a; Kubo et al. 2013), including mortality in higher quintiles (Hamad et al. 2015). We created a categorical variable to classify individuals’ underlying health into three groups: 0–1 (reference group), 1–2 (slightly above the mean), and 2–4 (more than double the mean) (Table 1). We excluded individuals with scores greater than 4 (1.4 percent of the sample) as they likely have severe preexisting conditions.
Data Analysis
The primary outcome variables included the number of monthly outpatient, ER, and inpatient visits. To examine changes in these outcomes over time, we employed segmented (piecewise) linear regression, a method used to compare trends in an outcome variable before and after a defined discontinuity or “knot.” This method has been used previously to examine health care utilization during the Great Recession (Dorn et al. 2012; Modrek, Hamad, and Cullen 2015). We modeled the knot in January 2009, the month in which major layoffs began at the firm, with a press release in January 2009 announcing plans for a workforce reduction of 13 percent, citing “extraordinary times requiring extraordinary actions” (Alcoa 2009). The press release did not specify which plants would be affected, so we assumed that individuals at all plants experienced some degree of job insecurity after the announcement in anticipation of the layoffs. Later announcements also indicated that multiple rounds of layoffs would occur, contributing to a sense of chronic job insecurity, particularly at high‐layoff plants (DeWitt 2009).
After conducting a graphical analysis of the data using kernel‐weighted local polynomial regressions, we found that this knot corresponded to a natural break in the data. The piecewise model allowed for differences in slope and intercept in two linear segments. Identifying a change in the intercept would reflect a difference in the baseline level of utilization in this population, which might occur abruptly as a result of a major shock such as the firm's announcements of mass layoffs. Meanwhile, a shift in slope would capture any sustained variation in the rate of change of utilization that might result from chronic job insecurity. We allowed the post‐2009 segment to extend until 2012, as prior studies have demonstrated that the effects of job insecurity on health status can linger for several years, even after job security is restored (Ferrie et al. 2002). Others have shown that the effects of chronic job insecurity are more persistent (Heaney, Israel, and House 1994), which was probable at this firm given that layoffs continued into 2010. More specifically, studies at this firm have found that increased work stress and use of mental health treatments persisted until 2012 (Modrek and Cullen 2013b; Modrek, Hamad, and Cullen 2015).
To examine the effects of job insecurity even more locally, we conducted two additional analyses. In the first, we included an interaction term between time and an indicator variable for whether an individual's plant experienced a mass termination event in the models described above, thereby comparing utilization trends among employees at high‐ and low‐layoff plants. In the second, we narrowed our sample to examine utilization trends at only high‐layoff plants. In this second set of models, we again conducted segmented regressions, but in this case we measured time relative to the occurrence of the first mass termination event at a given plant. Plants without mass termination events were not included in this second set of models. In these analyses, we assumed that the occurrence of mass layoffs at an individual's own plant was likely to make the threat of job loss more salient and led to a heightened sense of subjective job insecurity compared to employees at plants without mass layoffs. This has been empirically shown in the prior studies of layoffs and job insecurity, and conceptually it is likely related to both an increased likelihood of job loss as well as fear of job loss (Kivimäki et al. 2000; Sverke and Hellgren 2002).
We also assessed heterogeneity in employees’ responses to the recession by including an interaction term between time and a categorical variable for risk score.
In all models, we accounted for the possibility that changes in utilization may be due to aging of the sample by including a third‐degree polynomial for age. We also included year to account for secular trends. In analyses of trends in medication adherence, which is an annual rather than a monthly measure, we did not control for year or age due to the small number of time periods and subsequent collinearity, although we did include age‐squared and age‐cubed. As the dataset includes multiple observations for each individual, we included individual‐level fixed effects and robust standard errors clustered at the individual level in all models.
To evaluate the robustness of our findings, we conducted sensitivity analyses. To determine whether the placement of our knot at January 2009 is an appropriate model of the discontinuity in utilization trends, we tested alternative specifications. We examined models in which the knot is placed instead in January 2007, 2008, 2010, and 2011. If discontinuities in utilization trends are present at other knots, it may complicate the interpretation of our findings. Then, to isolate the effects of local job insecurity from possible effects of the recession more generally, we included a time‐varying variable representing monthly state‐level unemployment rates in the model of the overall employee sample.
Results
Utilization Trends
Segmented regressions in the overall sample (Figure 1, Table S1) revealed increased outpatient utilization among all employees after January 2009. Increases in the intercept (99.8 visits/10,000 individuals, p = .002) and slope (3.5 visits/month/10,000 individuals, p = .02) were apparent. ER visits also rose, with a marginally significant increase in the intercept of 10.0 visits/10,000 individuals (p = .06), and an increase in the slope of 0.4 visits/month/10,000 individuals (p = .05). There was no change for inpatient hospitalizations.
Figure 1.
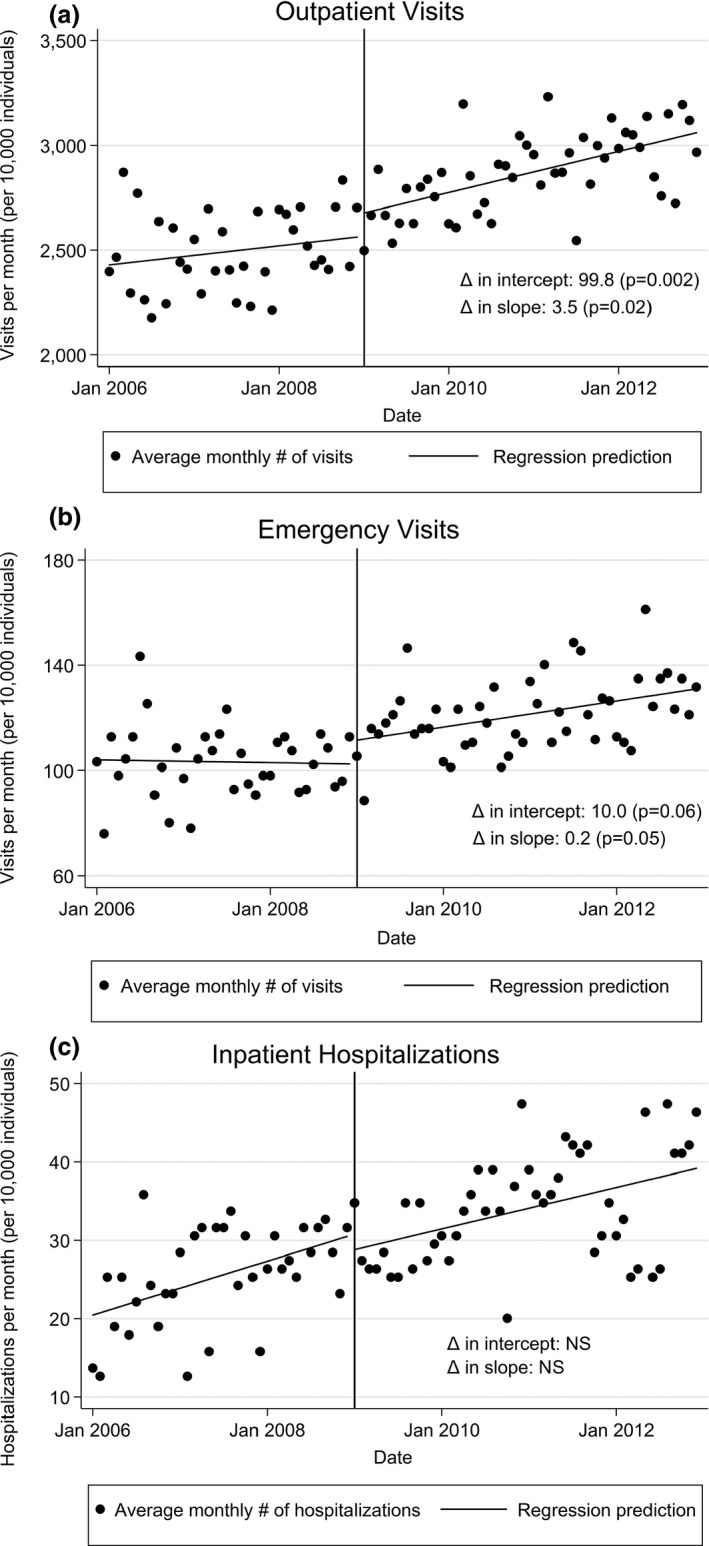
Health Care Utilization among All Employees before and after January 2009, by Type of Visit. (Analyses were conducted using segmented regressions with fixed effects at the individual level. Standard errors clustered at individual level. Covariates include year, age‐squared, and age‐cubed. NS = not significant)
Utilization by Degree of Job Insecurity
To examine the effects of job insecurity more locally, we first included an interaction term between time and an indicator variable for whether an employee worked at a high‐layoff plant (Table 2). Employees at high‐layoff plants experienced decreased outpatient utilization relative to employees at other plants (−4.0 visits/month/10,000 individuals, p = .008), although the overall trend was still positive, and marginally significantly increased ER utilization (0.4 visits/month/10,000 individuals, p = .08).
Table 2.
Moderating Factors of Monthly Health Care Utilization (per 10,000 Individuals) among All Employees (2006–2012)
| By Job Security | By Risk Score | |||||
|---|---|---|---|---|---|---|
| Visits per 10,000 Individuals per Month [95% CI] | Visits per 10,000 Individuals per Month [95% CI] | |||||
| Outpatient | Emergency | Inpatient | Outpatient | Emergency | Inpatient | |
| Time pre‐Jan 2009 | −0.15 [−5.05, 4.76] | 0.39 [−0.41, 1.19] | 0.43* [0.033, 0.83] | 11.5** [7.01, 15.9] | 0.97* [0.22, 1.73] | 0.76** [0.38, 1.13] |
| Time post‐Jan 2009 | 6.45** [1.85, 11.0] | 0.43 [−0.36, 1.22] | 0.42 [−0.0064, 0.85] | 3.28 [−1.02, 7.59] | 0.52 [−0.23, 1.27] | 0.31 [−0.089, 0.71] |
| Interaction terms: Job security† | ||||||
| Pre‐2009 × High‐layoff | 1.67 [−2.05, 5.39] | −0.33 [−0.89, 0.23] | 0.045 [−0.23, 0.32] | |||
| Post‐2009 × High‐layoff | −3.98** [−6.94, −1.02] | 0.40 [−0.053, 0.85] | −0.074 [−0.33, 0.18] | |||
| Interaction terms: Risk score‡ | ||||||
| Pre‐2009 × Risk score 1–2 | −25.9** [−30.9, −21.0] | −1.65** [−2.35. −0.96] | −0.33 [−0.67, 0.0071] | |||
| Pre‐2009 × Risk score 2–4 | −49.5** [−59.2, −39.9] | −4.18** [−5.70, −2.66] | −2.62** [−3.54, −1.71] | |||
| Post‐2009 × Risk score 1–2 | 0.61 [−3.32, 4.53] | −0.058 [−0.61, 0.49] | 0.063 [−0.27, 0.40] | |||
| Post‐2009 × Risk score 2–4 | 6.30 [−1.17, 13.8] | 1.69** [0.42, 2.96] | 0.62 [−0.028, 1.26] | |||
| Year | 78.4 [−162, 318] | −29.8 [−62.3, 2.82] | −7.57 [−24.4, 9.26] | 53.3 [−187, 294] | −33.9* [−66.5, −1.29] | −7.68 [−24.5, 9.11] |
| Age‐squared | −2.16 [−7.47, 3.15] | 0.52 [−0.19, 1.22] | 0.077 [−0.31, 0.46] | −3.07 [−8.41, 2.27] | 0.52 [−0.19, 1.23] | 0.046 [−0.34, 0.43] |
| Age‐cubed | 0.025 [−0.015, 0.064] | −0.0033 [−0.0084, 0.0019] | −0.00027 [−0.0032, 0.0026] | 0.041* [0.00095, 0.080] | −0.0027 [−0.0080, 0.0025] | 0.00016 [−0.002, 0.0031] |
| Number of observations | 796,824 | 796,824 | 796,824 | 796,824 | 796,824 | 796,824 |
| Number of individuals | 9,486 | 9,486 | 9,486 | 9,486 | 9,486 | 9,486 |
Analyses involved segmented regression with a discontinuity in January 2009, with fixed effects at the individual level. Time‐invariant characteristics, such as an individual's gender, risk score, or degree of job insecurity, were therefore not included in the model. Standard errors clustered at the individual level. Age was not included in these models as it is perfectly collinear with year.
†A high‐layoff plant was one in which 40 or more employees were laid off in a single day. Reference group = low‐layoff plants.
‡Higher risk scores indicate higher predicted health expenditures in the following year. Reference group = risk score 0–1.
*p < .05, **p < .01.
We then examined changes in utilization relative to the timing of the first mass termination event at high‐layoff plants to evaluate the effects of local job insecurity, rather than modeling the discontinuity at January 2009 (Figure 2). There was an increase in the intercept for outpatient visits of 182 visits/10,000 individuals (p < .001), although there was no increase in slope as we found in the overall employee panel. There was also an increase in the slope for ER visits of 0.9 visits/month/10,000 individuals (p = .004). There was no change for inpatient hospitalizations.
Figure 2.
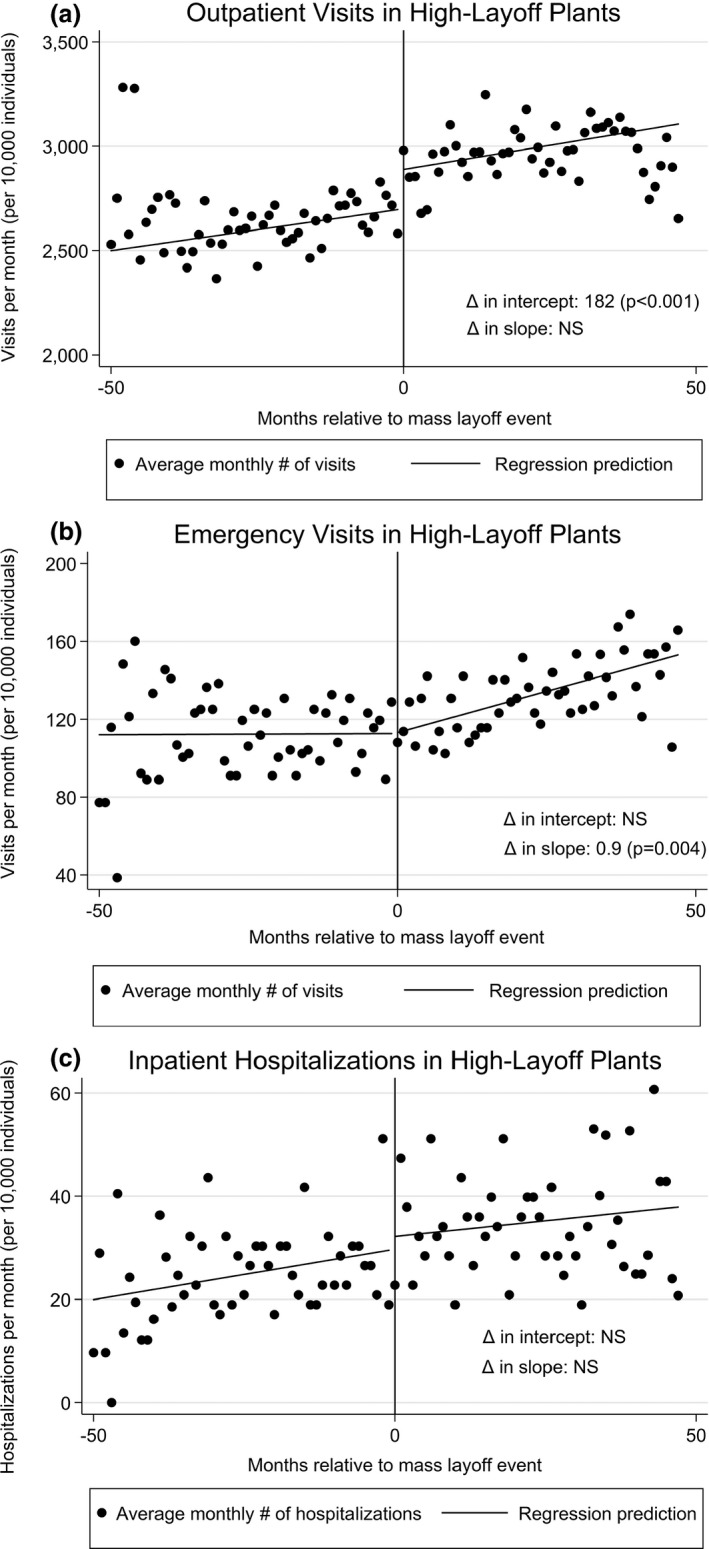
Health Care Utilization among Employees at High‐Layoff Plants Relative to Mass Layoff Event, by Type of Visit. (Analyses were conducted using segmented regressions with fixed effects at the individual level. Standard errors clustered at individual level. Covariates include year, age‐squared, and age‐cubed. NS = not significant)
Medication Adherence
We found an increase in the annual percentage filled of beta‐blockers, ACE inhibitors/ARBs, and statins after 2009, and decreased use of asthma/COPD controllers (Table 3A). Individuals at high‐layoff plants exhibited similar behavior, although the decrease in asthma/COPD controllers was no longer statistically significant (Table 3B).
Table 3.
Changes in Annual Adherence to Medications (2006–2012)
| Pre‐2009 | Post‐2009 | p‐Value for Pre–Post Δ in Trend | |
|---|---|---|---|
| % Δ in MPR†/year [95% CI] | % Δ in MPR/year [95% CI] | ||
| Panel A: Overall employee sample† | |||
| Beta‐blockers | 0.20* [0.014, 0.39] | 0.22* [0.030, 0.41] | .08 |
| ACEIs/ARBs | 0.12* [0.0071, 0.23] | 0.15** [0.037, 0.26] | <.001 |
| Statins | 0.070 [−0.053, 0.19] | 0.095 [−0.028, 0.22] | <.001 |
| Asthma/COPD controllers | 0.14 [−0.12, 0.40] | 0.10 [−0.15, 0.36] | .03 |
| Panel B: Employees at high‐layoff plants‡ | |||
| Beta‐blockers | 0.31* [0.029, 0.59] | 0.34* [0.055, 0.62] | .02 |
| ACEIs/ARBs | 0.11 [−0.034, 0.26] | 0.15* [0.0079, 0.30] | <.001 |
| Statins | 0.10 [−0.064, 0.27] | 0.14 [−0.029, 0.30] | <.001 |
| Asthma/COPD controllers | 0.16 [−0.19, 0.51] | 0.13 [−0.22, 0.47] | .13 |
†Analyses were conducted using segmented regression with a discontinuity in 2009, with fixed effects at the individual level. Control variables included age‐squared and age‐cubed. Standard errors clustered at the individual level.
‡Analyses were conducted using segmented regression with a discontinuity in the year of each plant's first mass layoff event, with fixed effects at the individual level. Control variables included age‐squared and age‐cubed. Standard errors clustered at the individual level.
*p < .05, **p < .01.
ACEI, angiotensin‐converting enzyme inhibitors; ARB,angiotensin‐receptor blockers; COPD, chronic obstructive pulmonary disease; MPR, medication possession ratio.
Utilization by Health Risk Score
Prior to the onset of the recession, employees with initially high‐risk scores demonstrated relative declines in utilization in all domains, likely indicative of mean reversion, as would be expected among high‐risk individuals who have experienced an earlier health crisis (e.g., a myocardial infarction or motor vehicle accident) (Table 2). After January 2009, however, individuals with the highest baseline risk scores experienced significant increases in ER utilization (1.7 visits/month/10,000 individuals, p = .009) and marginally significant increases in outpatient (6.3 visits/month/10,000 individuals, p = .09) and inpatient (0.6 hospitalizations/month/10,000 individuals, p = .06) utilization relative to employees with lower risk scores.
Sensitivity Analyses
When testing alternative placements of the knot, in 2008 we noted an increased slope and intercept for outpatient visits, and an increased slope for ER visits (Table S2). In 2007, the increase in the slope for outpatient utilization was significant; and in 2010, the increase in intercept was significant. To summarize, the discontinuous changes that we find in January 2009 are similar in January 2008, before the occurrence of mass layoffs at the firm, but squarely within the time period of the recession.
Including a time‐varying variable representing monthly unemployment rates resulted in similar coefficients and significance levels as in the primary models, although the increase in intercepts for outpatient and emergency utilization was no longer significant (Table S1).
Discussion
Our study examined the impacts on health care utilization of job insecurity in a continuously employed, continuously insured panel of U.S. workers in response to local mass layoffs during the Great Recession. It adds to the existing literature on the effects of job insecurity on health by demonstrating heterogeneous effects on health care utilization. We found a discontinuous increase in outpatient and ER visits in the overall sample after January 2009, when layoffs began at the firm. This included changes in the baseline level of utilization (intercept) and the rate of growth (slope), consistent with findings from previous studies in which job insecurity leads to both immediate and persistent effects on health status (Heaney, Israel, and House 1994; Ferrie et al. 2002; Modrek and Cullen 2013b; Modrek, Hamad, and Cullen 2015). We noted a greater relative increase in outpatient, ER, and inpatient utilization among individuals with higher baseline health risk scores, suggesting greater vulnerability in those with poor baseline health. We included controls for age and year, suggesting that our findings are not due to aging or secular trends.
We explored the moderating effects of job insecurity, which has been associated with increased chronic disease, worsened mental health, and decreased outpatient utilization (Sverke, Hellgren, and Naswall 2002; Modrek and Cullen 2013a; Reichert, Augurzky, and Tauchmann 2015). The increased intercept for outpatient visits among employees may represent an abrupt increase in utilization—or “hoarding”—due to fears of loss of insurance, while the subsequent decreased slope among employees at high‐layoff plants relative to those at low‐layoff plants may represent foregone care due to fears of reprisal for absenteeism or economic hardship (International Foundation of Employee Benefit Plans 2009). This is supported by previous studies, which found decreased cancer screening during economic downturns (Catalano, Satariano, and Ciemins 2003; Dorn et al. 2012), although these studies did not utilize a panel population and therefore may suffer from selection bias. Another study found that high community‐level unemployment was associated with a decrease in preventive dental visits among an insured population, also suggesting foregone preventive care (Quinn, Catalano, and Felber 2009). While the decreased outpatient visits in this subsample may be because less healthy individuals were laid off and not included in our panel, as shown in prior work on this population during the recession (Modrek and Cullen 2013a; Modrek, Hamad, and Cullen 2015), this is less likely to be the explanation given the increased ER use. The growth in ER utilization may represent exacerbation of chronic disease or increased workloads among survivors leading to deteriorating health, or substitution of ER visits for outpatient visits to avoid absenteeism (Davidson 1978). This finding is consistent with other studies finding increased ER use during the Great Recession (Chen et al. 2014).
Supplemental analyses to explore the pathways through which these changes may have occurred demonstrate no consistent drop in medication usage during the study period. This may be due to the robustness of the insurance coverage enjoyed by this workforce and the low costs of medications under this plan. The only drugs that demonstrate a decreased MPR are asthma/COPD controllers, whose out‐of‐pocket costs are at least double those of the other medications (i.e., roughly $25 per month compared to $5–12 per month). This may also be due to employees “stocking up” on medications due to fear of job and insurance loss (International Foundation of Employee Benefit Plans 2009).
Another potential pathway involves the impacts of financial stressors on stress physiology (Cohen, Janicki‐Deverts, and Miller 2007). A separate study of this population showed increased utilization of mental health treatments in response to the recession (Modrek, Hamad, and Cullen 2015). Future studies could consider measurements of allostatic load and biomarkers of chronic stress to explore this hypothesis.
Sensitivity analyses demonstrate that the discontinuous changes that we find in January 2009 are also present in January 2008, before the occurrence of mass layoffs at the firm, but squarely within the time period of the recession. We do not observe similar discontinuous changes at other time points. While this suggests that our findings may be driven by macroeconomic conditions more generally, including a time‐varying state‐level unemployment variable left our results unchanged with the exception of a loss of significance for the intercepts for outpatient and emergency utilization.
Implications for Policies and Interventions
The magnitude of these changes makes our findings relevant to health care spending. While the increase in outpatient and ER expenditures among employees was a few cents per member per month (data not shown), this represents an increase of over 60 percent. Compared to diabetes care management programs, in which a decrease in expenditure of 1–2 percent is considered noteworthy (Milliman Inc. 2012), this represents significant growth in health care spending. If these findings are replicated in other studies, they suggest that employers, insurers, and providers should be attentive to shifts in health care utilization in response to job insecurity, and intervene to either accommodate these shifts or work to counter them.
The results are also suggestive of the toll that job insecurity takes on employee physical and mental health. It has been shown that addressing employee perceptions around fairness and control can mitigate the negative effects of job insecurity (Sverke and Hellgren 2002). These perceptions could be addressed through workplace wellness or employee assistance programs. One study that also found decreased primary care use and increased ER use among the uninsured segment of the U.S. population suggested that this might be remedied by expansions in Medicaid coverage (Chen et al. 2014); our study, however, suggests that insurance coverage in and of itself may not be a sufficient factor in assisting individuals to seek preventive services. Others have suggested actively encouraging surviving employees to continue to use preventive services (Quinn, Catalano, and Felber 2009). Overall, however, there is little research on specific remedies of job insecurity, and future research could address this gap in knowledge.
Strengths and Limitations
Our study contributes new knowledge to our understanding of the impacts of job insecurity on health care utilization. While this sample is not representative of the U.S. population in terms of demographics, it is among the first to observe a large stable panel of individuals using objective measures (i.e., claims data) for a period of several years. With the exception of Medicare data, which include only older individuals, U.S. datasets provide few opportunities to examine populations in such detail, which is an advantage of this study sample. While some studies have relied on subjective reports by health providers, our study uses a robust dataset of claims and personnel data. Unlike studies of macroeconomic effects, it enables the study of more local effects of job insecurity by using linked administrative datasets. Population‐level data from insurers or providers may suffer from survivorship bias, leading to a perception of decreased utilization (American Academy of Family Physicians 2009; American Hospital Association 2009; Johnson, Rockoff, and Mathews 2010), while our sample consists of a panel of employees. Research conducted in high‐income countries with universal health insurance echoes our findings of increased outpatient utilization (Carr‐Hill, Rice, and Roland 1996; Kraut et al. 2000).
This study has several limitations. First, we are unable to make definitive causal conclusions based on the types of models employed in this study. Also, while our population provides evidence of the effects of job insecurity on health care utilization among a geographically and demographically diverse segment of the U.S. workforce, it is nevertheless not generalizable to the entire U.S. population: roughly 60 percent of the U.S. population was employed at any given point during the Great Recession (Bureau of Labor Statistics 2013a), and about 55 percent were covered by employer‐based insurance plans that were likely not as robust as those enjoyed by this sample (DeNavas‐Walt, Proctor, and Smith 2010). Moreover, the manufacturing industry experienced greater declines in employment than other industries during the Great Recession (Bureau of Labor Statistics 2012). Future research could examine workers in other sectors. This study also does not reflect utilization trends among those not in the workforce, such as the elderly. Our study may be limited in its use of mass layoffs as an objective proxy for job insecurity, which may contribute to measurement error. A subjective individual‐level measure of job insecurity might enhance the ability to detect more subtle associations between job insecurity and health care utilization. Future research should consider inclusion of alternative measures of job insecurity. Similarly, our measure of drug adherence is based on prescriptions filled, and it does not capture actual consumption of medications that were prescribed. Given the specific characteristics of health care access and insurance coverage in the United States, this study has limited generalizability to international settings. Finally, this study examines the effects of job insecurity during a recession, which may differ from job insecurity due to other factors, such as industrial restructuring or technological change.
Conclusion
Our study demonstrates discontinuous changes in health care utilization among a panel of continuously employed, continuously insured U.S. workers in response to heightened job insecurity. The results add to the literature on the impacts of job insecurity on health care utilization, suggesting differential effects among subgroups based on the degree of job insecurity. In particular, it suggests an increase in overall utilization concerning for “hoarding” of health care or worsening health, but a relative decrease in outpatient care and increase in emergency care among those at high‐layoff plants. The latter results confirm findings from the previous literature that suggest foregone preventive care among employed individuals during economic downturns with potentially negative long‐term health consequences. This study suggests that the health and social impacts of increased job insecurity experienced by workers during the recent recession may still emerge even as the economy improves.
Data Sharing
As an alternative to providing a deidentified dataset to the public domain, we allow access for reanalyses or appropriate follow‐on analyses by any qualified investigator willing to sign a contractual covenant with the host institution limiting the use of data to a specific agreed‐upon purpose and observing the same restrictions as are limited in our contract with the firm, such as 60‐day manuscript review for compliance purposes.
Supporting information
Appendix SA1: Author Matrix.
Table S1. Health Care Utilization among Employees before and after January 2009, by Type of Visit.
Table S2. Changes in Knot Placement for Overall Employee Health Care Utilization, 2006–2012.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by the National Institute on Aging (1R01AG026291) and by a grant from Alcoa. Dr. Hamad is supported by a KL2 Mentored Career Development Award of the Stanford Clinical and Translational Science Award to Spectrum (NIH KL2 TR 001083). Dr. Cullen serves as a senior medical advisor to Alcoa, under the terms of a research contract between Stanford University and Alcoa. All other authors receive some percentage of their salary support from a grant from Alcoa. The funders had no role in study design or conduct; the collection, management, analysis, or interpretation of the data; preparation or approval of the manuscript; or the decision to submit the paper for publication.
Disclosures: None.
Disclaimers: None.
References
- Alcoa . 2009. Alcoa Taking Decisive Action to Address Economic Downturn. Pittsburgh, PA: Alcoa. [Google Scholar]
- American Academy of Family Physicians . 2009. Patient Care during the 2008–2009 Recession. Leawood, KS: American Academy of Family Physicians. [Google Scholar]
- American Hospital Association . 2009. The Economic Crisis: The Toll on the Patients and Communities Hospitals Serve. Washington, D.C: American Hospital Association. [Google Scholar]
- Bureau of Labor Statistics . 2012. Spotlight on Statistics: The Recession of 2007–2009. Washington, DC: Bureau of Labor Statistics. [Google Scholar]
- Bureau of Labor Statistics . 2013a. News Release: Mass Layoffs—May 2013. Washington, DC: U.S. Department of Labor. [Google Scholar]
- Bureau of Labor Statistics . 2013b. “Labor Force Statistics from the Current Population Survey” [accessed on December 16, 2013]. Available at http://data.bls.gov/timeseries/LNS12300000
- Carr‐Hill, R. A. , Rice N., and Roland M.. 1996. “Socioeconomic Determinants of Rates of Consultation in General Practice Based on Fourth National Morbidity Survey of General Practices.” British Medical Journal 312: 1008–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano, R. A. 2009. “Health, Medical Care, and Economic Crisis.” New England Journal of Medicine 360 (8): 749–51. [DOI] [PubMed] [Google Scholar]
- Catalano, R. A. , Satariano W. A., and Ciemins E. L.. 2003. “Unemployment and the Detection of Early Stage Breast Tumors among African Americans and Non‐Hispanic Whites.” Annals of Epidemiology 13: 8–15. [DOI] [PubMed] [Google Scholar]
- Catalano, R. , Goldman‐Mellor S., Saxton K., Margerison‐Zilko C., Subbaraman M., LeWinn K., and Anderson E.. 2011. “The Health Effects of Economic Decline.” Annual Review of Public Health 32: 431–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, J. , Vargas‐Bustamante A., Mortensen K., and Thomas S. B.. 2014. “Using Quantile Regression to Examine Health Care Expenditures during the Great Recession.” Health Services Research 49 (2): 705–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, S. , Janicki‐Deverts D., and Miller G. E.. 2007. “Psychological Stress and Disease.” Journal of the American Medical Association 298 (14): 1685–7. [DOI] [PubMed] [Google Scholar]
- Cullen, M. R. , Vegso S., Cantley L., Galusha D., Rabinowitz P., Taiwo O., Fiellin M., Wennberg D., Iennaco J., Slade M. D., and Sircar K.. 2006. “Use of Medical Insurance Claims Data for Occupational Health Research.” Journal of Occupational and Environmental Medicine 48 (10): 1054–61. [DOI] [PubMed] [Google Scholar]
- Davidson, S. M. 1978. “Understanding the Growth of Emergency Department Utilization.” Medical Care 16 (2): 122–32. [DOI] [PubMed] [Google Scholar]
- DeNavas‐Walt, C. , Proctor B. D., and Smith J. C.. 2010. Income, Poverty, and Health Insurance Coverage in the United States: 2009. Washington, DC: U.S. Census Bureau. [Google Scholar]
- DeWitt, J. 2009. Alcoa to Expand Layoffs at Davenport Works. Davenport, IA: Quad‐City Times. [Google Scholar]
- Dorn, S. D. , Wei D., Farley J. F., Shah N. D., Shaheen N. J., Sandler R. S., and Kappelman M. D.. 2012. “Impact of the 2008–2009 Economic Recession on Screening Colonoscopy Utilization among the Insured.” Clinical Gastroenterology and Hepatology 10: 278–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragano, N. , Verde P. E., and Siegrist J.. 2005. “Organisational Downsizing and Work Stress: Testing Synergistic Health Effects in Employed Men and Women.” Journal of Epidemiology and Community Health 59: 694–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du, J. , and Yagihashi T.. 2015. “Health Care Use, Out‐of‐Pocket Expenditure, and Macroeconomic Conditions during the Great Recession.” The BE Journal of Economic Analysis & Policy 15 (1): 119–56. [Google Scholar]
- Ferrie, J. E. , Shipley M. J., Stansfeld S. A., and Marmot M. G.. 2002. “Effects of Chronic Job Insecurity and Change in Job Security on Self Reported Health, Minor Psychiatric Morbidity, Physiological Measures, and Health Related Behaviours in British Civil Servants: The Whitehall II Study.” Journal of Epidemiology and Community Health 56: 450–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamad, R. , Modrek S., Kubo J., Goldstein B. A., and Cullen M. R.. 2015. “Using “Big Data” to Capture Overall Health Status: Properties and Predictive Value of a Claims‐Based Health Risk Score.” PLoS ONE 10 (5): e0126054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handel, B. R. 2011. Adverse Selection and Switching Costs in Health Insurance Markets: When Nudging Hurts. Working Paper 17459. Cambridge, MA: National Bureau of Economic Research. [Google Scholar]
- Heaney, C. A. , Israel B. A., and House J. S.. 1994. “Chronic Job Insecurity among Automobile Workers: Effects on Job Satisfaction and Health.” Social Science and Medicine 38 (10): 1431–7. [DOI] [PubMed] [Google Scholar]
- Hill, J. J. , Galusha D., Slade M. D., and Cullen M. R.. 2013. “Drug Adherence after Price Changes in a Previously Compliant Population.” American Journal of Managed Care 19 (3): 236–7. [PMC free article] [PubMed] [Google Scholar]
- Hurd, M. D. , and Rohwedder S.. 2010. Effects of the Financial Crisis and Great Recession on American Households. Working Paper 16407. Cambridge, MA: National Bureau of Economic Research. [Google Scholar]
- International Foundation of Employee Benefit Plans . 2009. Health Care Plans: Impact of the Financial Crisis. Brookfield, WI: International Foundation of Employee Benefit Plans. [Google Scholar]
- Johnson, A. , Rockoff J. D., and Mathews A. W.. 2010. “Americans Cut Back on Visits to Doctor.” Wall Street Journal July 29, 2010: A1. [Google Scholar]
- Kivimäki, M. , Vahtera J., Pentti J., and Ferrie J. E.. 2000. “Factors Underlying the Effect of Organisational Downsizing on Health of Employees: Longitudinal Cohort Study.” British Medical Journal 320 (7240): 971–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivimäki, M. , Vahtera J., Elovainio M., Pentti J., and Virtanen M.. 2003. “Human Costs of Organizational Downsizing: Comparing Health Trends between Leavers and Stayers.” American Journal of Community Psychology 32 (1/2): 57–67. [DOI] [PubMed] [Google Scholar]
- Kraut, A. , Mustard C., Walld R., and Tate R.. 2000. “Unemployment and Health Care Utilization.” Scandinavian Journal of Work, Environment and Health 26 (2): 169–77. [DOI] [PubMed] [Google Scholar]
- Kubo, J. , Goldstein B. A., Cantley L. F., Tessier‐Sherman B., Galusha D., Slade M. D., Chu I. M., and Cullen M. R.. 2013. “Contribution of Health Status and Prevalent Chronic Disease to Individual Risk for Workplace Injury in the Manufacturing Environment.” Occupational and Environmental Medicine 71 (3): 159–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martikainen, P. , Maki N., and Jantti M.. 2008. “The Effects of Workplace Downsizing on Cause Specific Mortality: A Register‐Based Follow‐Up Study of Finnish Men and Women Remaining in Employment.” Journal of Epidemiology and Community Health 62: 1008–13. [DOI] [PubMed] [Google Scholar]
- McInerney, M. , and Mellor J. M.. 2012. “Recessions and Seniors’ Health, Health Behaviors, and Healthcare Use: Analysis of the Medicare Current Beneficiary Survey.” Journal of Health Economics 31: 744–51. [DOI] [PubMed] [Google Scholar]
- Miller, D. L. , Page M. E., Stevens A. H., and Filipski M.. 2009. “Why Are Recessions Good for Your Health?” The American Economic Review 99 (2): 122–7. [Google Scholar]
- Milliman Inc . 2012. The Cost and Quality Gap in Diabetes Care: An Actuarial Analysis. New York: Milliman Inc. [Google Scholar]
- Modrek, S. , and Cullen M. R.. 2012. Job Demand and Early Retirement. Chestnut Hill, MA: Center for Retirement Research at Boston College. [Google Scholar]
- Modrek, S. , and Cullen M. R.. 2013a. “Health Consequences of the ‘Great Recession’ on the Employed: Evidence from an Industrial Cohort in Aluminum Manufacturing.” Social Science and Medicine 92: 105–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modrek, S. , and Cullen M. R.. 2013b. “Job Insecurity during Recessions: Effects on Survivors’ Work Stress.” BMC Public Health 13: 929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modrek, S. , Hamad R., and Cullen M. R.. 2015. “Psychological Well‐Being during the Great Recession: Changes in Mental Health Care Utilization in an Occupational Cohort.” American Journal of Public Health 105 (2): 304–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modrek, S. , Stuckler D., McKee M., Cullen M. R., and Basu S.. 2013. “A Review of Health Consequences of Recessions Internationally and a Synthesis of the US Response during the Great Recession.” Public Health Reviews 35 (1): 1–33. [Google Scholar]
- Pollack, C. E. , Kurd S. K., Livshits A., Weiner M., and Lynch J.. 2011. “A Case‐Control Study of Home Foreclosure, Health Conditions, and Health Care Utilization.” Journal of Urban Health 88 (3): 469–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn, B. C. , Catalano R. A., and Felber E.. 2009. “The Effect of Community‐Level Unemployment on Preventive Oral Health Care Utilization.” Health Services Research 44 (1): 162–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichert, A. R. , Augurzky B., and Tauchmann H.. 2015. “Self‐Perceived Job Insecurity and the Demand for Medical Rehabilitation: Does Fear of Unemployment Reduce Health Care Utilization?” Health Economics 24 (1): 8–25. [DOI] [PubMed] [Google Scholar]
- Roehrig, C. , Turner A., Hughes‐Cromwick P., and Miller G.. 2012. “When the Cost Curve Bent—Pre‐Recession Moderation in Health Care Spending.” New England Journal of Medicine 367 (7): 590–3. [DOI] [PubMed] [Google Scholar]
- Sverke, M. , and Hellgren J.. 2002. “The Nature of Job Insecurity: Understanding Employment Uncertainty on the Brink of a New Millennium.” Applied Psychology 51 (1): 23–42. [Google Scholar]
- Sverke, M. , Hellgren J., and Naswall K.. 2002. “No Security: A Meta‐Analysis and Review of Job Insecurity and Its Consequences.” Journal of Occupational Health Psychology 7 (3): 242–64. [PubMed] [Google Scholar]
- Vahtera, J. , Kivimäki M., Pentti J., Linna A., Virtanen M., Virtanen P., and Ferrie J. E.. 2004. “Organisational Downsizing, Sickness Absence, and Mortality: 10‐Town Prospective Cohort Study.” British Medical Journal 328 (7439): 555. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1. Health Care Utilization among Employees before and after January 2009, by Type of Visit.
Table S2. Changes in Knot Placement for Overall Employee Health Care Utilization, 2006–2012.


