Abstract
Background
Catastrophic thinking and fear-avoidance belief are negatively influencing severe acute pain following surgery causing delayed ambulation and discharge. We aimed to examine if a preoperative intervention of cognitive-behavioural therapy (CBT) could influence the early postsurgical outcome following lumbar spinal fusion surgery (LSF).
Methods
Ninety patients undergoing LSF due to degenerative spinal disorders were randomly allocated to either the CBT group or the control group. Both groups received surgery and postoperative rehabilitation. In addition, the CBT group received a preoperative intervention focussed on pain coping using a CBT approach. Primary outcome was back pain during the first week (0–10 scale). Secondary outcomes were mobility, analgesic consumption, and length of hospitalisation. Data were retrieved using self-report questionnaires, assessments made by physical therapists and from medical records.
Results
No difference between the groups’ self-reported back pain (p = 0.76) was detected. Independent mobility was reached by a significantly larger number of patients in the CBT group than the control group during the first three postoperative days. Analgesic consumption tended to be lower in the CBT group, whereas length of hospitalisation was unaffected by the CBT intervention.
Conclusion
Participation in a preoperative CBT intervention appeared to facilitate mobility in the acute postoperative phase, despite equally high levels of self-reported acute postsurgical pain in the two groups, and a slightly lower intake of rescue analgesics in the CBT group. This may reflect an overall improved ability to cope with pain following participation in the preoperative CBT intervention.
Trial registration
The study was approved by the Danish Protection Agency (2011-41-5899) and the Ethics Committee of the Central Denmark Region (M-20110047). The trial was registered in Current Controlled Trials (ISRCTN42281022).
Keywords: Lumbar spinal fusion, Low back pain, Cognitive-behavioural therapy, Acute postsurgical pain, Mobility, Randomised controlled trial
Background
A high level of acute pain following surgery, may adversely affect short-term physical and psychological recovery, thereby delaying mobilisation and discharge from hospital [1, 2]. Acute pain is furthermore a risk factor for the development of chronic postsurgical pain, which has a negative long-term impact on the patient’s life, and potentially imposes a significant burden on the healthcare sector and society [1, 3, 4]. The available knowledge about acute postsurgical pain in patients undergoing lumbar spinal fusion surgery (LSF) is limited. To our knowledge, only three studies have reported on acute postsurgical pain following LSF. One Danish observational study measured pain on a 0–10 visual analogue scale (VAS) during the first 24 h after LSF, and found patients to report an average VAS score of 5 [5]. Two other studies, one comparing different analgesic methods and one comparing different surgical techniques, found patients to report pain levels below 3 on a VAS scale. One of these studies measured pain on the first three postoperative days [6], and the other on the third postoperative day and on the day of discharge, respectively [7].
The experience of postsurgical pain is reinforced by psychological characteristics like fear-avoidance belief and catastrophic thinking [8, 9]. These negative characteristics seem to be susceptible to change through cognitive-behavioural therapy (CBT) with subsequent improvements in pain and function [10]. In the case of LSF, two studies have examined the effect of using CBT in the postoperative rehabilitation, overall reporting a positive effect of CBT in the long run [11, 12]. However, as the CBT intervention was offered several weeks after surgery in both studies, the ability of CBT to influence the acute postoperative phase is unclear. The effect of a preoperative rehabilitation intervention on early postoperative outcomes after LSF was examined in a study published by Nielsen et al. in 2010 [13]. In their study, a prehabilitation intervention with presurgical training and information, but not CBT, was found to be more effective than standard care in terms of improving the patients’ mobility (e.g. walking, stair climbing, daily function on ward) and decreasing length of hospitalisation [13]. Additionally, acute postsurgical pain was measured on a VAS scale (0–100) on the day of discharge, where no difference between groups was found. In 2015, the authors of this article published an RCT investigating the effect of a preoperative CBT intervention on LSF patients [14]. This RCT revealed that the CBT intervention was superior to usual care in terms of improvement in disability and quality of life three months after surgery. We therefore found it relevant to explore whether the CBT intervention could also have an effect on the patient’s pain and mobility already in the early postoperative phase. Thus, the aim of the present study was to examine whether a preoperative CBT intervention could influence acute postsurgical pain, mobility, analgesic intake and length of hospitalisation in patients undergoing LSF. This aim is in accordance with the previously published study protocol (ISRCTN42281022) [15].
Methods
The patients were recruited consecutively from the orthopaedic departments at two Danish hospitals in the period October 2011 to June 2013. Patients who fulfilled the inclusion criteria were informed about the study by the nurses in the ambulatory. The inclusion criteria were 1) a primary diagnosis of degenerative disc disease, stenosis or spondylolisthesis grade 1–2 (assessed by the operating surgeon); 2) fusion of maximum three levels, 3) age between 18 and 64 years, and 4) competence in the Danish language. Patients were excluded if the waiting time for surgery was less than 4 weeks, a driving distance of more than 80 km from the hospital, or in case of psychiatric, inflammatory or malignant disease. Eligible patients consenting to participation were assigned by computer-generated block randomisation (by hospital) on a 1:2 ratio to receive either standard treatment (surgery and postoperative rehabilitation) or standard treatment plus a preoperative CBT intervention. The 1:2 ratio was applied to enable group sessions in the intervention group. Due to the nature of the intervention, the patients could not be blinded to treatment allocation. The trial was registered in Current Controlled Trials (ISRCTN42281022, please see http://www.isrctn.com/search?q=ISRCTN42281022).
Interventions
The full details of the interventions are described in a previous publication [15]. Briefly, the interventions were as follows:
-
Control group
Patients in the control group received the standard course of treatment, which includes preoperative information about the upcoming operation, the anaesthetic procedure, medication, the postoperative rehabilitation and physical restrictions following surgery. Information was given by the operating surgeon, nurses and therapists. The surgical technique used was at the discretion of the surgeon.
-
Cognitive-behavioural group
In addition to the standard course of treatment, the patients were to participate in four 3-h group-sessions. The main topics covered were the interaction of cognition and pain perception, coping strategies, pacing principles, ergonomic directions, return to work, and details about the surgical procedure. The intervention was managed by a multidisciplinary team consisting of a psychologist, an occupational therapist, a physical therapist, a spine surgeon, a social worker and a previously operated patient. Each treatment session was standardised although some flexibility was allowed to meet the participants’ needs. To ensure uniformity of the sessions during the project period a staff manual was handed out to supplement the treatment sessions, and furthermore the primary investigator met with the staff at regular intervals. Compliance with the intervention was defined a priori as attendance at half of the sessions as a minimum.
-
Outcomes
The patients’ demographic characteristics were collected from the hospitals’ medical records system and from self-report questionnaires.
The primary outcome was the severity of back pain during the first postoperative week. The patients reported their average daily pain in a diary using a numeric rating scale (NRS) of 0–10 [16], and the median of postoperative days 1–7 was calculated, in accordance with the recommendations from the International Association for the Study of Pain (IASP) [1].
Secondary outcomes included postoperative mobility, consumption of rescue analgesics (i.e., analgesic consumption beyond the standardised analgesic protocol), and length of hospitalisation. Mobility was measured on the first three postoperative days using the Cumulated Ambulation Score (CAS) [17]. The CAS measures the level of mobility in the three activities getting in and out of bed, sit-to-stand from a chair, and walking. Each activity was assessed daily on a three-point scale from 0–2 (0 = Not able to, 1 = Able to, with assistance, 2 = Able to safely, without assistance). The assessment was performed by the physical therapist attending the patient at the ward.
The information on analgesic consumption was retrieved from the medical records system. Due to great variability in analgesic medications and dosages, we converted these data into daily morphine-equivalent doses to enable comparison between the groups [18].
Data on number of days of hospitalisation were retrieved from the medical records system.
-
Statistical methods
The analysis was based on intention-to-treat. All data were entered twice into EpiData version 3.1, and any divergence was corrected according to original data. STATA version 13.0 (Stata Corp, College Station, TX) was used for statistical evaluation. Due to the non-parametrical nature of the primary outcome, postsurgical back pain (0–10 scale) the difference between group medians (with 25th and 75th percentiles) was compared using the Wilcoxon rank sum test. A difference of two NRS-points was considered a clinically relevant difference between groups. Our sample size calculation was, however, based on the Oswestry Disability Index (ODI), and not the numeric pain rating scale, as the power was set to show an effect on functional disability at the one-year follow-up. These data have been presented in a previous publication, in accordance with the published study protocol for this trial [15]. For comparison of secondary outcomes (mobility, medication and hospitalisation), which were all of a non-parametrical nature, the Wilcoxon rank sum test or the chi squared statistic were used as appropriate.
Results
Patient recruitment and flow
During the inclusion period from 1 October 2011 to 1 July 2013 a total of 221 patients fulfilled the inclusion criteria. After applying the exclusion criteria 157 patients remained, and of these 96 agreed to participate (Fig. 1). Most patients declined participation due to severe pain making them unable to drive to and from the hospital in case of allocation to the CBT group, and some declined because they could not take time off work. The majority of the patients (81 of 96) were recruited from one of the two hospitals (the regional hospital). Sixty-three patients were allocated to the intervention group, and 33 to the control group. Six patients were excluded (4 in the CBT group) at the time of surgery due to change of surgical technique or cancellation of surgery. The median number of days from baseline measurement to surgery was 42.5 days (range 26–210 days) for the group as a whole. Table 1 shows the patients’ baseline characteristics.
Fig. 1.
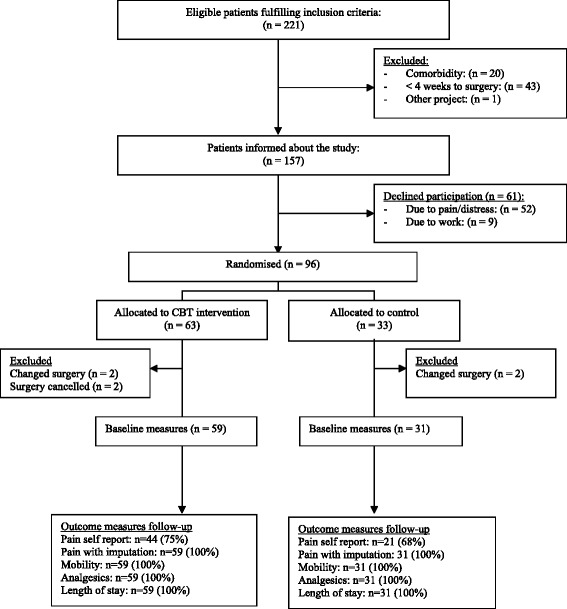
Patient recruitment, allocation and follow-up
Table 1.
Baseline patient data
| Patient characteristics | CBT group | Control group |
|---|---|---|
| (n = 59) | (n = 31) | |
| Male gender | 23 (39) | 16 (52) |
| Age (year ± SD) | 51.4 (9.2) | 47.7 (8.9) |
| Smoking n (%) | 20 (32) | 10 (30) |
| Working status | ||
| Employed Unemployed Disability pension Early retirement |
32 (54) 11 (19) 9 (15) 7 (12) |
15 (48) 11 (36) 5 (16) 0 (0) |
| Diagnosis | ||
| Spondylolisthesis | 16 (27) | 7 (23) |
| Degenerative disc disease | 43 (73) | 24 (77) |
| Surgical procedures | ||
| PLF | 41 (69) | 12 (39) |
| TLIF | 17 (29) | 19 (61) |
| Uninstrumented | 1 (2) | 0 (0) |
| Previous spine surgery | ||
| Spondylodesis | 2 (3) | 1 (3) |
| Decompression | 7 (11) | 1 (3) |
| Fusion levels | ||
| One | 36 (62) | 20 (69) |
| Two | 19 (32) | 8 (27) |
| Three | 4 (7) | 3 (10) |
| Disability (ODI) | ||
| Mean (SD) | 40.7 (13.2) | 40.8 (15) |
| Pain (LBPRS) | ||
| Back,median (25;75 percentile) | 7.0 (5.3;8.0) | 7.2 (6.0;8.0) |
| Leg, median (25;75 percentile) | 6.3 (4.3;7.7) | 6.3 (3.7;8.3) |
| Quality of life (EQ-5D) | 0.655 (0.389;0.723) | 0.627 (0.356;0.723) |
Numbers are presented as n (%) unless otherwise stated
EQ-5D EuroQol 5 Dimensions, LBPRS low back pain rating scale, ODI oswestry disability index, PLF posterolateral fusion, TLIF transforaminal lumbar interbody fusion
Clinical outcomes
The results for all outcome measures are presented in Table 2.
Table 2.
Pain, mobility, analgesic use, and length of stay after fusion in CBT and control group
| Outcome Reported as median (25th; 75th percentiles) unless stated otherwise | CBT group | N | Control group | N | P-value |
|---|---|---|---|---|---|
| Back paina | 5.4 (4.0;6.5) | 44 | 5.3 (4.0;6.1) | 21 | 0.74 |
| Mobility on day 3, n (%)b | 59 | 31 | |||
| Walk | 43 (73) | 15 (48) | 0.02 | ||
| Rise and sit from a chair | 58 (98) | 26 (84) | 0.017 | ||
| Get in and out of bed | 58 (98) | 26 (84) | 0.017 | ||
| Analgesic use | 59 | 31 | |||
| Morphine equivalents | 142.5 (70;275) | 196.8 (145;345) | 0.23 | ||
| Hospitalisation | 59 | 31 | |||
| Number of days | 5 (4;6) | 4 (4;6) | 0.46 |
aPain: measured using numeric rating scale (0-10/best-worst)
bThe numbers indicate the number (%) of patients being able to carry out the activity without support on the third postoperative day
For the primary outcome the CBT group reported a median back pain severity of 5.6 (range 1.7–10.0), which was no different from that of the control group of 5.3 (range 1.1–7.7) (P = 0.73). Due to a non-response rate of 28 % on the pain diaries, we chose to perform a sensitivity analysis where missing data on back pain were imputed with data retrieved from the medical records. This reduced the median scores slightly, although non-significantly, with a median score of 4.9 (range 1.7–10) and 4.9 (range 1.1–7.8) for the CBT group and the control group, respectively.
With regards to postoperative mobility patients in the CBT group performed superiorly on the measured activities during the first 3 postoperative days (Fig. 2). Thus, independent walking ability was achieved by 39 % (n = 23) versus 16 % (n = 5) (P < 0.026) on day 2, and by 73 % (n = 43) versus 48 % (n = 15) of patients on day 3 (P < 0.02). For the activities getting in and out of bed and getting up from a chair the CBT group correspondingly performed better on all three days of assessment, with the difference being significant on day 3 (Fig. 2).
Fig. 2.
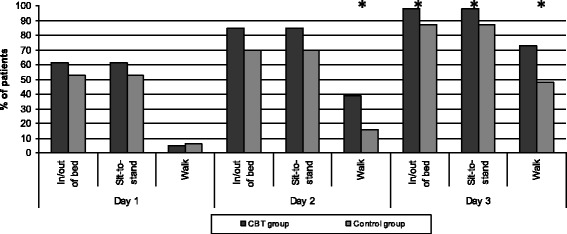
Independent mobility the first 3 days after lumbar fusion surgery. Columns represent the percentage of patients in each group who are able to manage the given activity without any assistance from a person or an aid. CBT = cognitive-behavioural therapy. * = P < 0.05
In terms of analgesic consumption, a lower consumption was observed in the CBT group, although the difference between groups was only significant on postoperative day 2 (Fig. 3).
Fig. 3.

Use of analgesics during the first 5 postoperative days following lumbar spinal fusion surgery. Units in morphine equivalent dose. Graph illustrating median values. Day 0 = the day of surgery; CBT = cognitive behavioural therapy group. *P < 0.05
The length of stay was comparable between the groups with a median number of days of five (range 3–9) in the CBT group and four (range 3–10) in the control group.
Compliance with intervention
Of the 49 patients who complied with the intervention 15 patients attended all 4 sessions, 21 attended 3 sessions and 13 attended 2 sessions. For the ten patients that did not comply (i.e., attended only 1 or no sessions) various reasons for non-compliance were given, e.g., could not take time off as expected (n = 3), driving to and from hospital caused too much pain (n = 2), on maternity leave prior to surgery (n = 1), serious illness of close relative (n = 1) and other personal reasons (n = 3). All patients remained in the analysis, regardless of their compliance with the intervention.
Discussion
The purpose of our study was to investigate whether a preoperative CBT intervention had a positive effect on acute postsurgical pain, mobility, use of analgesics, and length of hospitalisation. We did not find CBT to be superior in terms of pain reduction. In fact, both groups reported a moderate to severe level of back pain (>5 NRS points) postoperatively, which is comparable to the findings of the Danish observational study previously described [5]. These pain levels are high compared with the results of the other studies, generally reporting postoperative pain levels below 3 points [6, 7, 13]. These differences may be due to different methods for reporting acute postsurgical pain, as these studies reported pain using VAS scales where we used the NRS scale. However, there seems to be little difference between the two scales, as the literature finds VAS and NRS scores to correspond well and also finds them equally responsive [16, 19]. Also, the differences could be due to variability in the diagnosis of the study populations, as two of the studies included only patients with spondylolisthesis grade I and II [6, 7]. The third study did not report specifically on the patients' diagnosis (“degenerative disease”) [13].
An important finding of the present study was the significantly superior achievements on mobility, seen in the CBT group. Despite the fact that patients in the two groups experienced the same severity of acute postsurgical pain, the patients in the CBT group performed better on the assessed activities, even with a lower requirement for rescue analgesics. These results correspond well with the previously published findings on disability for this study, where the CBT group reported a significantly larger reduction on the Oswestry Disability Index (P = 0.003) already 3 months after LSF surgery, even though self-reported back pain was similar to that of the control group [14].
In terms of length of hospitalisation, patients in the CBT group were not discharged from hospital earlier than patients in the control group. As suggested by Kehlet et al. [20] this may indicate that factors like established ward routines and the staff and the patient’s expectations have a greater say for when patients are discharged than the patient’s actual condition itself. Similarly, in the prehabilitation study by Nielsen et al., routines in discharge procedures caused a delay between the achievement of recovery milestones and the time of discharge [13].
Our sample size calculation was based on the Oswestry Disability Index (ODI) and not the NRS, as the power was set to show an effect on functional disability at the 1-year follow-up. These data have been presented in a previous publication in accordance with the published study protocol for this trial [15]. We therefore cannot rule out that our study was insufficiently powered to demonstrate differences in pain. However, even with the low response of patients ( 44 from the CBT group and 21 from the control group) it allows for the detection of a difference between the groups of 2.0 NRS units (SD 2.0) at a significance level of 0.05 with a power of 80 %. Hence, a more powerful design would probably not have affected the overall conclusions regarding pain.
We included both spondylolisthesis and disc degeneration patients in the study to mimic daily clinical practice and to increase the external validity of the study. By random, the two posterior surgery procedures (PLF and TLIF) were unevenly distributed in the two groups. As the TLIF is a procedure with longer surgery time than the PLF, a difference could perhaps have been expected in this early recovery phase. However, in the present study this was not the case, as patients undergoing TLIF reported lower pain levels during hospitalisation in both the CBT group and the control group.
A limitation to our study was the moderate response rate of 72 % for the pain diaries. However, a non-responder analysis revealed no significant differences between non-responders and responders regarding their baseline characteristics, e.g. gender (P = 0.69), age (P = 0.25), ODI score (P = 0.97) and pain severity (P = 0.83).
Another limitation study pertains to the issue of blinding, an almost unavoidable limitation of studies investigating complex interventions. Thus, although the physiotherapists assessing mobility (CAS score) were not informed about the patients’ group assignment, a few of the patients accidentally revealed this. This may of course have had an influence in favour of the CBT group for those patients whose group assignment was known.
Conclusion
We believe that this study adds important knowledge about the early postoperative period following LSF. Although the preoperative CBT intervention did not influence acute postsurgical pain, the intervention had a positive effect on the patients’ ability to cope with pain as evidenced by earlier achievement of independent mobility and less use of analgesics in the intervention group. With reference to the previously published results from this trial, showing an overall positive effect of the CBT intervention, we therefore recommend that a CBT intervention is offered prior to LSF surgery. We further find it relevant to investigate whether a change in ward procedures would enable a faster discharge for those with independent mobility already on postoperative day two or three.
Acknowledgments
We would like to thank the staff at the orthopaedic departments at Regional Hospital Silkeborg and Aarhus University Hospital, especially the nurses for helping with patient recruitment, and the physical therapists for performing mobility assessments of all the patients during their hospitalisation.
Funding
The study was supported by the Danish Council for Strategic Research, the Health Research Fund of Central Denmark Region, the Danish Rheumatism Association and the Health Foundation. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. The funding bodies played no role in the design, collection, analysis and interpretation of the data, in writing the manuscript, or the decision to submit for publication.
Availability of data and materials
The dataset supporting the conclusions of this article is available from the corresponding author.
Authors’ contributions
NR participated in the design, planning and coordination of the study, and in the development and planning of the CBT intervention. NR performed the data analysis and drafted and revised the manuscript. LGO conceived of the study and participated in its design. LGO also helped develop the CBT intervention and revised the manuscript. CVN has participated in the design of the study and has revised the manuscript. FBC and LGO have participated in data analysis and interpretation. FBC, RH and CB have furthermore revised the manuscript. All authors have read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was conducted in agreement with the Helsinki Declaration, and was approved by the Ethics Committee of Central Denmark Region (M-20110047). All patients signed a consent form upon inclusion into the study.
Abbreviations
- CAS
cumulated ambulation score
- CBT
cognitive-behavioural therapy
- EQ-5D
EuroQol 5 dimensions
- LSF
lumbar spinal fusion
- NRS
numeric rating scale
- ODI
oswestry disability index
- VAS
visual analogue scale
References
- 1.Schug SA, Pogatzki-Zahn EM. Chronic Pain after Surgery or Injury. Pain: Clinical Updates. 2011;19(11) pp 1-5 .
- 2.Ip HYV, Abrishami A, Peng PWH, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: A qualitative systematic review. Anesthesiology. 2009. [DOI] [PubMed]
- 3.Jones I. Bari F. Surgery (United Kingdom): Chronic pain after surgery; 2014. [Google Scholar]
- 4.Niraj G, Rowbotham DJ. Persistent postoperative pain: Where are we now? Br J Anaesth. 2011. [DOI] [PubMed] [Google Scholar]
- 5.Vibeke Nielsen R. Storm Fomsgaard J. Mathiesen O. Insufficient pain management after spine surgery. Danish Medical Journal: Dahl JB; 2014. [PubMed] [Google Scholar]
- 6.Schenk MR, Putzier M, Kügler B, Tohtz S, Voigt K, Schink T, Kox WJ, Spies C, Volk T. Postoperative analgesia after major spine surgery: Patient-controlled epidural analgesia versus patient-controlled intravenous analgesia. Anesth Analg. 2006. [DOI] [PubMed]
- 7.Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J. 2010. [DOI] [PMC free article] [PubMed]
- 8.Theunissen M, Peters ML, Bruce J, Gramke H, Marcus MA. Preoperative anxiety and catastrophizing: A systematic review and meta-analysis of the association with chronic postsurgical pain. Clin J Pain. 2012. [DOI] [PubMed]
- 9.Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective fa. Expert Rev Neurother. 2009. [DOI] [PubMed]
- 10.Sveinsdottir V, Eriksen HR. Reme SE. Journal of Pain Research: Assessing the role of cognitive behavioral therapy in the management of chronic nonspecific back pain; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abbott AD, Tyni-Lenne R, Hedlund R. Early rehabilitation targeting cognition, behavior, and motor function after lumbar fusion: A randomized controlled trial. Spine. 2010. [DOI] [PubMed]
- 12.Monticone M, Ferrante S, Teli M, Rocca B, Foti C, Lovi A, Brayda Bruno M. Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomised controlled trial. Eur Spine J. 2014. [DOI] [PMC free article] [PubMed]
- 13.Nielsen PR, Jørgensen LD, Dahl B, Pedersen T, Tønnesen H. Prehabilitation and early rehabilitation after spinal surgery: Randomized clinical trial. Clin Rehabil. 2010. [DOI] [PubMed]
- 14.Rolving N, Nielsen CV, Christensen FB, Holm R, Bünger CE, Oestergaard LG. Does a preoperative cognitive-behavioural intervention affect disability, pain behaviour, pain and return to work the first year after lumbar spinal fusion surgery? Spine. 2015. (In press). [DOI] [PubMed]
- 15.Rolving N, Oestergaard LG. Willert MV. Blumensaat F, Bunger C, Nielsen CV. Description and design considerations of a randomized clinical trial investigating the effect of a multidisciplinary cognitive-behavioural intervention for patients undergoing lumbar spinal fusion surgery. BMC Musculoskelet Disord: Christensen FB; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferreira-Valente MA, Pais-Ribeiro JL. Jensen MP. Pain: Validity of four pain intensity rating scales; 2011. [DOI] [PubMed] [Google Scholar]
- 17.Foss NB, Kristensen MT, Kehlet H. Prediction of postoperative morbidity, mortality and rehabilitation in hip fracture patients: The cumulated ambulation score. Clin Rehabil. 2006. [DOI] [PubMed]
- 18.Anonymous Washington State Agency Medical Directors Group. Web-based opioid dose calculator. 2014. http://agencymeddirectors.wa.gov/mobile.html. Accessed 29 Jan 2015.
- 19.Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, Fainsinger R, Aass N, Kaasa S, European Palliative Care Research Collaborative (EPCRC). Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011. [DOI] [PubMed]
- 20.Kehlet H. Future perspectives and research initiatives in fast-track surgery. Langenbecks Arch Surg. 2006. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is available from the corresponding author.


