Abstract
Virtually all efforts to generate an effective protection against the life-long, recurrent genital infections caused by Herpes simplex virus-2 (HSV-2) have failed. Apart from sexual transmission, the virus can also be transmitted from mothers to neonates, and is a key facilitator of HIV co-acquisition. Here, we uncover a nanoimmunotherapy using specially designed Zinc Oxide Tetrapod Nanoparticles (ZOTEN) with engineered oxygen vacancies. We demonstrate that ZOTEN, when used intravaginally as a microbicide, is an effective suppressor of HSV-2 genital infection in female BALB/c mice. The strong HSV-2 trapping ability of ZOTEN significantly reduced the clinical signs of vaginal infection and effectively decreased animal mortality. In parallel, ZOTEN promoted the presentation of bound HSV-2 virions to mucosal antigen presenting cells, enhancing T cell- mediated and antibody-mediated responses to the infection, and thereby, suppressing a re-infection. We also found that ZOTEN exhibits strong adjuvant-like properties, which is highly comparable to alum, a commonly used adjuvant. Overall, our study provides very first evidence for the protective efficacy of an intravaginal microbicide/vaccine or microbivac platform against primary and secondary female genital herpes infections.
Introduction
HSV-2 is an enveloped double-stranded DNA virus. Globally, it is one of the most common human pathogens. HSV-2 has been found to cause mucosal and neurological infections, however, it typically causes genital infections (genital herpes) manifesting as severe lesions in and around the genitalia, accompanied by inflammation of infected and nearby tissues (1,2). In addition, disease recurrence and associated morbidity are very common, despite therapy (1). Genital herpes is thus a top-priority healthcare concern (1, 2). However, virtually all the attempts to develop an effective vaccine have failed and current HSV-2 antivirals are inefficient, due essentially to the development of drug-resistance and failure to prevent recurrence (1,3). Highly innovative strategies are needed to develop an effective prophylaxis against HSV-2 infection and associated diseases.
Rapid emergence of nanotechnology, and nanoparticle use in medicine, has led to numerous novel discoveries in the field of drug development (4). Using nanoparticles as an alternative to traditional therapies has unprecedented advantages such as enhanced efficacy, reduced side effects and more targeted localization in disease sites (4–6). Previous studies suggested that uniquely synthesized zinc oxide nanoparticles suppress viral infection in vitro by binding to HSV-2 virions and rendering them ineffective for a productive infection (7).
Here, we provide evidence for the in vivo efficacy of specially designed and synthesized zinc oxide (ZnO) tetrapod-form nanoparticles (ZOTEN) that prevent HSV-2 infection and disease. Additionally, ZOTEN therapy creates a platform for viral antigen presentation, provides adjuvant benefits and enhances cell-mediated and humoral anti-HSV-2 immunity. This work presents proof for a novel microbivac concept (8), which has the potential to prevent infection to sero-negative individuals. ZOTEN provides a platform for virus capture and presentation of neutralized virions to mucosal antigen presenting cells for initiating and boosting adaptive immunity. Our study also demonstrates the feasibility that intravaginal route can be used for vaccine delivery.
Materials and Methods
Cell Culture
Human vaginal epithelial (VK2/E6E7) cells were obtained from ATCC. VK2/E6E7 cells were passaged in Karatinocyte serum free medium (SFM) (Gibco/BRL, Carlsbad, CA, USA) supplemented with epidermal growth factor (EGF) and bovine pituitary extract (BPE). African green monkey kidney (Vero) cells were provided by Dr. P.G. Spear (Northwestern University, Chicago, IL). Human cervical (HeLa) cells were provided by Dr. B.S. Prabhakar (University of Illinois at Chicago). Vero cells and HeLa cells were maintained in Dulbecco’s modified Eagle’s medium (DMEM; Life Technologies, Grand Island, NY) supplemented with 10% FBS and 1% penicillin-streptomycin.
Viruses
Two strains of HSV-2 were used: wild type HSV-2(333) and β-galactosidase-expressing HSV-2(333) gJ- (23). High-titred stocks of the virus strains were propagated by infecting Vero cells at a low MOI of 0.01 and harvesting cells when cytopathic effect was 90 to 100%. Cell associated virus particles were released by sonication. Both virus strains were titred on Vero cells, and stored at −80 °C.
Mouse Vaginal Swabs and Vaginal Wash
Female Balb/c mice of 6–8 weeks age were used for experiments. All animal studies were performed in compliance with the U.S. Department of Health and Human Services Guide for the Care and Use of Laboratory Animals and also adhered to the guidelines of the World Medical Association’s Declaration of Helsinki. Seven days prior to infection, animals were injected with progesterone. Vaginal swabs were collected according to protocol mentioned earlier with slight modifications (10). Briefly, vaginal swabs were collected by gently inserting presoaked calcium Alginate fiber tipped applicator swabs (Fisherbrand) into the vagina and gently brushing the side walls of the vagina, three times. The swabs were then placed in 1 mL of DMEM containing 5% (vol/vol) FBS, 1% gentamicin and stored at −80 °C until titred. Before titring, the swabs were thawed and vigorously vortexed for 30 s. Serial dilutions of the washes were used to generate the plaques on Vero cells.
HSV-2(333)gJ- Replication and Spread
Virus replication and spread was assessed by sacrificing mice as specified on days post viral inoculation. The vaginas were removed and split open longitudinally. Vaginal tissue was then fixed in 2% paraformaldehyde 0.02% Nonidet-P40 in PBS for 6 hours. Following fixation the organs were stained overnight with X-gal (1 mg.ml 6-bromo-4-chloro-3-indolyl-b-D-galactopyranisude, 3mM potassium ferrous cyanide, 3mM ferric cyanide, 2mM magnesium chloride 0,1mM EGTA, 0.01 sodium deoxycholate, and 0.02 Nonidet-P40). The staining of the vaginal tissue was scored on a scale from 0–5, 0 = no blue staining; 1 = 10% – 20% of surface covered in blue lesions; 2 = 30% of the surface covered in blue lesions; 3 = 40%-50% of surface covered in blue lesions; 4 = 60% – 70% of surface covered in blue lesions 5 = 80% −100% covered in blue lesions. All examiners who have done scoring were masked regarding the treatment condition of each mouse.
HSV inflammation
Extracted vaginas were semi-quantatively assessed for inflammation. The inflammation of vaginal tissue was scored on a scale from 0–4; 0 = no inflammation; 1 = mild inflammation; 2 = moderate inflammation; 3 = severe inflammation and mild tissue damage; 4 = severe inflammation, severe tissue damage/ necrosis of tissue. All examiners who have done scoring were masked regarding the treatment condition of each mouse.
Immunohistochemistry
14 days post infection mice were sacrificed and dorsal root ganglion were removed for fixation, embedding in paraffin, and sectioning as described earlier (11). Sections were stained with H&E and a semi-quantative scale was made to determine the level of inflammation within, spinal cord, meninges, dorsal root ganglion, and nerve root.
Mouse model of genital herpes
BALB/c female mice were injected with 0.1 ml of Depo-Provera (Medroxyprogesterone acetate) at a concentration of 25 mg/ml to allow mice to get on the same menstrual cycle. Seven days after injection, mice were inoculated with HSV-2 (333) (or HSV-2 (333) gJ-) with or without ZOTEN. A viral dose of 5×105 pfu was used for all infections. Following challenge, mice were monitored for 21 days to evaluate clinical signs of disease and system tolerance of various different treatments. Also, infected mice were monitored for death or severe morbidity requiring euthanasia. The day of death or sacrifice was recorded for each animal.
HSV-2 serum entry Inhibition Assay
The presence of antibodies against HSV-2 in mouse sera was detected according to a protocol mentioned earlier with slight modifications (12). Virus neutralization was measured by evaluating the level of inhibition that sera had on the entry of β-galactosidase reporter virus HSV-2(333)gJ−. Serum was incubated with virus for 30 minutes before addition to cells. 2 hours post infection, virus and sera inoculum was removed, and infection continued for additional 4 hours. ONPG substrate solution was added to cells for 30 minutes to 1 hour at 37°C. Tecan plate reader was used to for the collection of optical density values.
Synthesis and characterization of ZOTEN (tetrapod-form ZnO Micro-nanoparticles)
ZOTEN structures were synthesized by a recently developed flame transport synthesis (FTS) approach (9, 13). The preparation of ZOTEN starts from spherical zinc micro particles obtained commercially. Synthesis involves Zn particles, PVB powder, and Ethanol. A mixture is prepared and burned together in the furnace at 900°C. The flame (generated due to the burning of sacrificial polymer PVB) carries the Zn microparticles upward, where they are subsequently transformed into the vapor state in the form of individual Zn atoms, Zn dimers, Zn trimers, etc. The highly unstable atomic variants in the Zn vapor immediately start participating in nucleation and growth processes with the help of available native oxygen molecules in the environment. First Zn and O combine to form a primary cluster and once the stable nucleus has been formed, further available Zn and O atoms contribute to conventional 1D spike growth. Homogeneous nucleation results in growth of tetrapod-type structures. PVB (polyvinyl Butyrol) decomposes completely into CO2 and O2 and tetrapods growth occurs in normal ambient conditions. This highly efficient process gives a ZOTEN actual yield of 99.9%. Mishra et. al. show that this process creates uniform ZnO tetrapods (ZOTEN) by electron microscopy (13). The shape and size of the synthesized structures were investigated using scanning electron microscopy (SEM) at 10 kV electron beam acceleration voltage and 18 µA filament (LaB6) current. The SEM results confirmed the tetrapod shape of the ZnO structures with arm diameters in the range of 200 nm to 1 µm and arm lengths in the range of 5 µm to 30 µm. Identical ZOTENs were used for all experiments demonstrated here.
Assessment of Clinical and Neurological Signs of Disease
Following vaginal challenge with HSV-2(333), mice were observed for the development of clinical signs of disease for 21 days or until death/sacrifice. Mice were examined for the development of external lesions, hair loss, inflammation, and skin lesions around the vaginal opening, rectum, tail base, and hind legs. Mice were also monitored for the development of neurological signs of disease such as fecal/urine retention, hind-limb paralysis, hunched posture, lethargy, dehydration, and ruffled fur. Any animal exhibiting severe morbidity was sacrificed. Each mouse was given a infection severity score from 0 to 5 (0= no lesions; 1= slight hair loss and inflammation; 2= hair loss, inflammation, and small lesion < 0.5 cm; 3= significant hair loss broken skin, scabbing, multiple pustules, bleeding; 4= large lesions on vaginal opening, rectum and hind leg, significant hair loss, broken skin >1 cm; 5= serve scabbing and bleeding, multiple lesions, lesions on tail base, pustules, serve inflammation/bleeding). All examiners who have done scoring were masked regarding the treatment status of each mouse.
T- Cell Proliferation Assay
After BALB/c mice were injected with Depo-Provera, 1 of 5 treatment conditions was used to prime the immune system. 1- Uninfected and untreated; 2-UV inactivated virus alone; 3- ZOTEN and UV inactivated virus; 3- Alum and UV inactivated virus; 4- Alum, ZOTEN, and UV inactivated virus. Mice were sacrificed 21 days post inoculation. Spleens were removed and single cell suspensions were made. Isolated splenocytes were treated with ACK lysis buffer for 5 minutes at room temperature to lyse red blood cells. Following incubation, equal numbers of cells were seeded in a round bottom 96- well plate for 24 hours. Cells were then challenged with HSV-2 for 2 days before being labeled with BrdU (Invitrogen). Following BrdU labeling, stimulated splenocytes were stained with Anti-Mouse CD4-PE and Anti-Mouse CD8. FACS analysis was performed to determine the level of T-cell proliferation. Results are shown as the percentage of lymphocytes that have incorporated BrdU into newly formed cells.
Cytotoxicity of T-Lymphocyte Killing Assay
To measure the cytotoxicity of T-lymphocytes against VK2/E6E7 target cells, cytotoxic-T lymphocyte (CTL) killing assays were performed as previously described (14,15). Briefly, target cells were labeled with Vybrant Dil Cell-Labeling Solution (life technologies) and then incubated with T-lymphocytes at the indicated effector/target ratios. After 4 hours, cells were harvested; TO-PRO-3-iodide, a membrane impermeable DNA stain was added to each culture (0.5µM final concentration), and cells were finally analyzed by flow cytometry. Background and maximum TO-PRO-3 iodide staining were obtained by incubating target cells with medium and detergent, respectively. The percentage specific lysis was calculated as [(%TO-PRO-3-iodide+PKH26+ cells in effector/target cell co-culture -% TO-PRO-3-iodide+PKH26+ cells in medium)/(% TO-PRO-3-iodide+PKH26+ cells in detergent - % TO-PRO-3-iodide+PKH26+ cells in medium] × 100%.
Imaging
Dendritic cells were isolated according to a protocol mentioned earlier (16). Cells were isolated, counted and cultured in glass bottom dishes (MatTek Corporation, Ashland, MA). ZOTEN (0.1mg/mL) and 1 × 106 pfu of GFP HSV-2 (333) were added to the dish and incubated for 1 hour in 37°C before being imaged under the microscope (Zeiss Confocal 710, Germany using a 63 oil objective lens).
Statistics
The following statistical tests were used for various experiments. Appropriate statistical tests are mentioned in the figure legends for every respective experiment. Statistical significance was calculated by one-way analysis of variance (ANOVA) followed by Tukey’s post hoc t-test, student t test, Mantel-Cox log rank test, 2way ANOVA, Kaplan-Meier survival analysis using graphpad *P≤0.5, **P≤0.01, ***P≤0.001.
Study Approval
The Animal Care and Use Committee at the University of Illinois has approved all animal studies, and the experimental protocols used in this study.
Results
Synthesis and characterization of ZOTEN
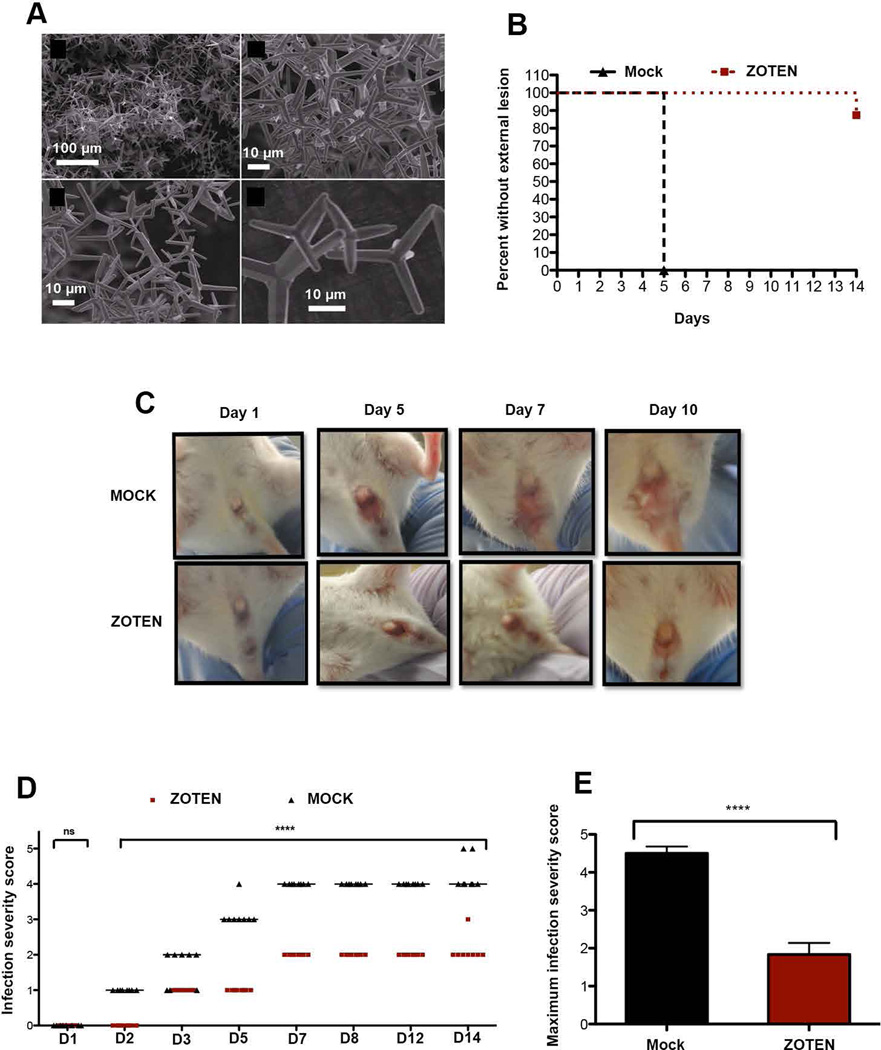
The ZnO tetrapod micro-nanoparticles (ZOTEN) used in this study were synthesized by the recently introduced flame transport synthesis (FTS) approach (9). In FTS process, Zn microparticles and polyvinyl butyral (PVB) powders are used as precursor material. Zn microparticles are mixed in PVB powder in the ratio of 1:2 and then the mixture (in a ceramic crucible) is heated inside a muffle type furnace up to 900°C for 30 minutes in normal air environment. During the synthesis process, sacrificial PVB polymer maintains the necessary separation between Zn microparticles which are transported and simultaneously converted into nano-microscale ZnO tetrapods by the generated flame inside the furnace. After this process ZnO tetrapods are harvested from the ceramic crucible (9,17,18). The microstructural evolutions of the synthesized ZOTEN were characterized using scanning electron microscope (20 keV Philips-FEI XL30 equipped with LaB6 filament). ZOTEN consisted of spike like structures, which meet at central point (Fig. 1A). The process of ZOTEN formation is highly efficient and the actual yield is 99.9% (19)
Figure 1. ZOTEN treatment significantly diminishes lesions when challenged with HSV-2.
A. Scanning electron microscopy (SEM) images of ZnO tetrapod nanoparticles (ZOTEN) synthesized by flame transport synthesis. Top left: Low magnification SEM image showing the overview structure from ZOTEN powder. Top right: Slightly higher magnification SEM image demonstrating interconnected network from ZOTEN. Bottom images demonstrate high magnification SEM images of tetrapod-form geometry of ZOTEN, used in this study.
B. Mice were challenged intravaginally with HSV-2 333 with or without ZOTEN. Mice were examined daily after for external lesions, for 14 days. The day on which the external lesion was first noted was recorded for each animal (n=6–12 mice for each experimental group). As the experiment progressed the n value changed due to death of mice in certain groups. Mantel-Cox log rank test was used to determine the statistical significance of lesion appearance in Control and ZOTEN treated mice. P <0.001. Representative data are from one of three independent experiments is shown.
C. To monitor progression of infection, mice were observed daily for the development of lesions around the vaginal opening, and base of the tail. Representative images from three independent experiments are shown.
D. Infection severity score was noted based on the progression of acute infection. The severity of infection was scored on a scale of 0–5, 5 being the most severe. All examiners who have done scoring were masked regarding the treatment status of each mouse. Error bars represent the standard error of the mean. (S.E.M). Asterisks represent a significant difference calculated using a 2way ANOVA; ****P<0.0001. (n=6 mice for each group). Representative data from one of three independent experiments is shown.
E. Maximum infection severity score among ZOTEN-treated and mock-treated mice. ZOTEN treated mice overall show reduced infection severity score when compared to mock. Representative data from one of three independent experiments is shown.
ZOTEN diminishes the development of Acute Signs of HSV-2 infection
To assess the virucidal potential of ZOTEN therapy in vivo, we utilized a mouse vaginal HSV-2 infection model (19). Female Balb/c mice were made susceptible to intravaginal infection by inducing the diestrus stage (uncornified vaginal epithelium) of the estrous cycle by injecting Depo-Provera (progesterone) (20). Mice were inoculated with HSV-2 (333), in the presence and absence of ZOTEN, to allow the assessment of viral entry and spread within various organs and tissues. All mice were infected with 5 × 105 plaque forming units. Mice were examined daily for clinical symptoms of infection such as hair loss, inflammation, and lesion development on the vagina, rectal opening, tail base and legs. While all infected mock-treated mice displayed external lesions by 5 days post challenge, ZOTEN-treated mice showed significantly reduced lesion development, as less than 20% of ZOTEN-treated animals developed external lesions on day 14 post infection and beyond (Fig. 1B). Thus it appeared that ZOTEN decreases the rate and extent of lesion formation after HSV-2 infection.
Mock-treated mice began to lose hair and developed small lesions around the vaginal opening at 5 days post infection, which continuously increased in number and size as infection progressed, eventually leading to the formation of pustules and bleeding at the base of the tail (Fig. 1C). On the other hand, less than 20% of ZOTEN-treated mice showed slight inflammation at the vaginal opening with minor hair loss at day 5, crusting at the proximal region of the back leg by day 10 (Fig. 1D). The remaining (greater than 80%) of ZOTEN-treated mice were comparable to uninfected mice, displaying no hair loss or lesion development. To further assess the effect of ZOTEN on lesion development after infection, infected mice were given daily infection severity scores based on the progression of infection and related disease symptoms. Extent and severity of lesion development were significantly reduced by ZOTEN treatment (Fig. 1E). Together, these results confirmed that ZOTEN treatment as a microbicide significantly suppresses the acute symptoms of HSV-2 infection.
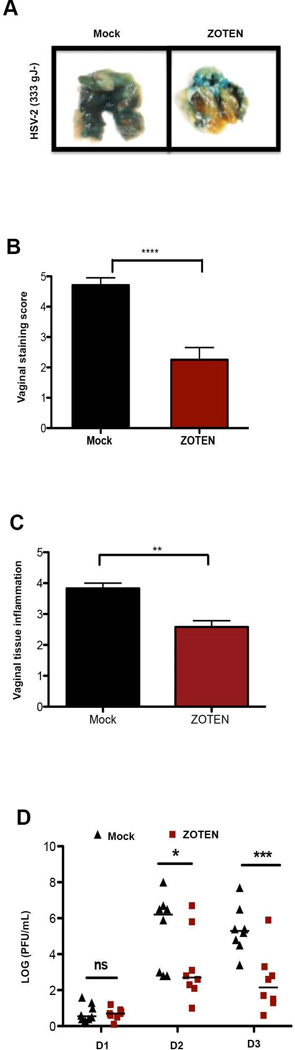
ZOTEN reduces viral loads in the vaginas of infected mice
Having observed the strong ability of ZOTEN to suppress acute HSV-2 genital disease, we then sought to determine the effect of ZOTEN on viral loads in the infected mice vaginas. BALB/c mice infected with β-galactosidase-expressing HSV-2 gJ- were sacrificed 5 days post challenge. The vaginas were extracted and stained with X-gal to assess the level of viral entry that occurred within the vaginal epithelium. Stained tissue sections were scored on a scale of 0–5, where 0 signifies no X-gal staining while 5 signifies extensive X-gal staining on the epithelium. We found that ZOTEN treatment decreased X-gal staining, suggesting significantly lowered viral loads by the treatment (Fig. 2A). Average staining score of ZOTEN-treated mice was ~2.1 contrary to a score of ~4.4 for mock group (Fig. 2B). Additionally, by measuring inflammation in extracted vaginas according to criteria mentioned in materials and methods, we found that ZOTEN-treated mice had vaginas with less inflammation and tissue damage (Fig. 2C), consistent with decreased viral loads in the tissues.
Figure 2. ZOTEN treatment as a vaccine significantly diminishes HSV-2 inflammation and genital infection.
A. Mice were inoculated with HSV-2 (333), in the presence or absence of ZOTEN. Five days after infection, mice were euthanized. The extent of vaginal infection was analyzed by the expression of β-galactosidase from the reporter virus. The tissue staining and virus infection were scored on a scale of 0–5, 5 being the most severe. Representative images of the vaginas from three independent experiments are shown.
B. The tissue staining, indicative of virus loads, was scored on a scale of 0–5. Vaginal staining score was assigned after tissue staining. All examiners who have done scoring were masked regarding the treatment status of each mouse. Error bars represent the S.E.M. Asterisks represent a significant difference calculated using a 2way ANOVA; ****P<0.0001. (n=6 mice for each group). Representative data from one of three independent experiments is shown.
C. Five days after virus inoculation with HSV-2 (333), female mice were euthanized. Tissue inflammation score was assigned after the extraction of the vagina. Inflammation was scored on a scale of 0–5, 5 being the most severe. All examiners who have done scoring were masked regarding the treatment status of each mouse. Six mice were used for each group (n=6). Error bars represent the S.E,M. . Asterisks represent a significant difference calculated using a 2way ANOVA; **P<0.01. Representative data from one of three independent experiments is shown.
D. Mice were intravaginally inoculated with HSV-2 and vaginal swabs were collected for the first three days of infection (n= 8–10). Each symbol represents the PFU per individual mouse, while horizontal lines indicate the mean value. Asterisks represent a significant difference calculated using a 2way ANOVA. *P≤0.05, **P≤0.01, ***P≤0.001. Representative data from one of three independent experiments is shown.
To further confirm the effect of ZOTEN treatment on virus levels in infected mice, the mice vaginas were swabbed for 5 consecutive days following intravaginal challenge, to measure the levels of virus within the vaginal lumen. Viral titres recovered from vaginal swabs revealed that ZOTEN-treated mice produced significantly lower viral titres at all points of infection tested (Fig. 2D). These results indicate the strong ability of ZOTEN to suppress HSV-2 vaginal infection in mice. Reduced redness, inflammation, hair loss and lesion development, along with decreased viral replication levels by ZOTEN treatment strongly support its potential as an intravaginal microbicide against HSV-2 infection.
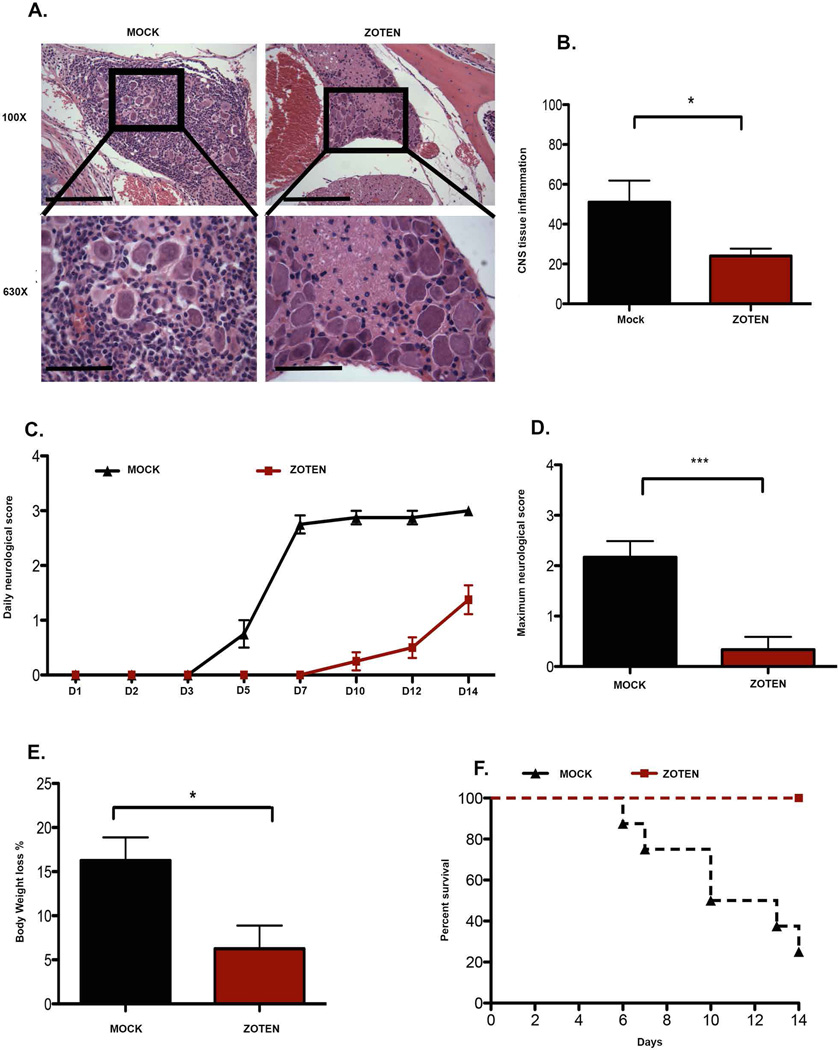
ZOTEN reduces the development of chronic infection and animal mortality
A hallmark of the establishment of a chronic HSV-2 infection is virus dissemination within the body, leading to tissue inflammation (1). Since HSV-2 spreads predominantly to tissues of the peripheral and central nervous systems (1, 2, 21), we assessed these tissues for signs of inflammation or tissue damage, suggestive of HSV-2 spread. Therefore, dorsal root ganglia (DRG) and spinal cords (SC) of mock- or ZOTEN-treated mice were removed, fixed, sectioned and stained with H&E, to determine inflammation levels (Fig. 3A) and scored on a semi-quantitative scale according to criteria mentioned in materials and methods (Fig. 3B). Hence, ZOTEN-treated mice showed significantly less inflammation in the spinal cords than mock treated group, reflecting less viral dissemination into neuronal tissues.
Figure 3. ZOTEN vaccine reduces the development of chronic infection, and abolishes mortality.
A. Fourteen days post infection with HSV-2, the spinal column was dissected, fixed, paraffin embedded and stained with H&E. H&E staining of the spinal cord and dorsal root ganglion revealed the presence of inflammation within the CNS 14 days post infection. Images were captured using a 100× magnification. Representative images from three independent experiments are shown.
B. Average percentage of tissue inflammation noted in each group (n=15). All examiners who have done scoring were masked regarding the treatment status of each mouse. Error bars represent the S.E.M. from the mean. Asterisks represent a significant difference calculated using a 2way ANOVA; *P≤0.05. Representative data from one of three independent experiments is shown.
C. Mice were monitored for the development of neurological symptoms and scored on a scale of 0–5, 5 being the most severe. (n=6 mice for each group). All examiners who have done scoring were masked regarding the treatment status of each mouse. Error bars represent the S.E.M. from the mean. Asterisks represents significant difference calculated using 2way ANOVA; * P≤0.05, **P≤0.01, ***P≤0.001, ****P≤0.0001. Representative data from one of three independent experiments is shown.
D. The average maximum neurological score achieved by day 14. Error bars represent the S.E.M. Asterisks represent a significant difference calculated using a 2way ANOVA. Representative data from one of three independent experiments is shown.
E. The average percentage of weight loss occurring by day 14 post infection. Error bars represent the S.E.M. Asterisks represent a significant difference calculated using a 2way ANOVA; *P≤0.05. (n=6 mice for each group). Representative data from one of three independent experiments is shown.
F. Survival analysis of infected mice Kaplan-Meier survival analysis was used to determine the statistical difference between each treatment group. (n=6 mice for each group). The P= 0.002. Representative data from one of three independent experiments is shown.
Additional signs of HSV-2 infection spread include development of neurological disease, weight loss, and finally animal death (1, 2, 21). Consistent with decreased inflammation by ZOTEN treatment, reduced neurological disease symptoms were also observed upon treatment (Fig. 3C and 3D). Furthermore, infection-induced weight loss was much less remarkable among ZOTEN-treated mice (Fig. 3E). To further confirm the impact of ZOTEN treatment on overall animal health and vitality, we assessed mortality rates of ZOTEN- or mock-treated mice. ZOTEN-treated mice had a significantly lower mortality rate than mock-treated mice, as 100% of the mice within the ZOTEN-treated group survived the 21 day period of evaluation. Conversely, 50% of the mock-treated mice died by day 10 post-infection, reaching 80% mortality by day 14 (Fig. 3F). Collectively, this data indicates the ability of ZOTEN to reduce chronic disease development associated with inflamed tissues, neurological disease symptoms, weight loss and mortality.
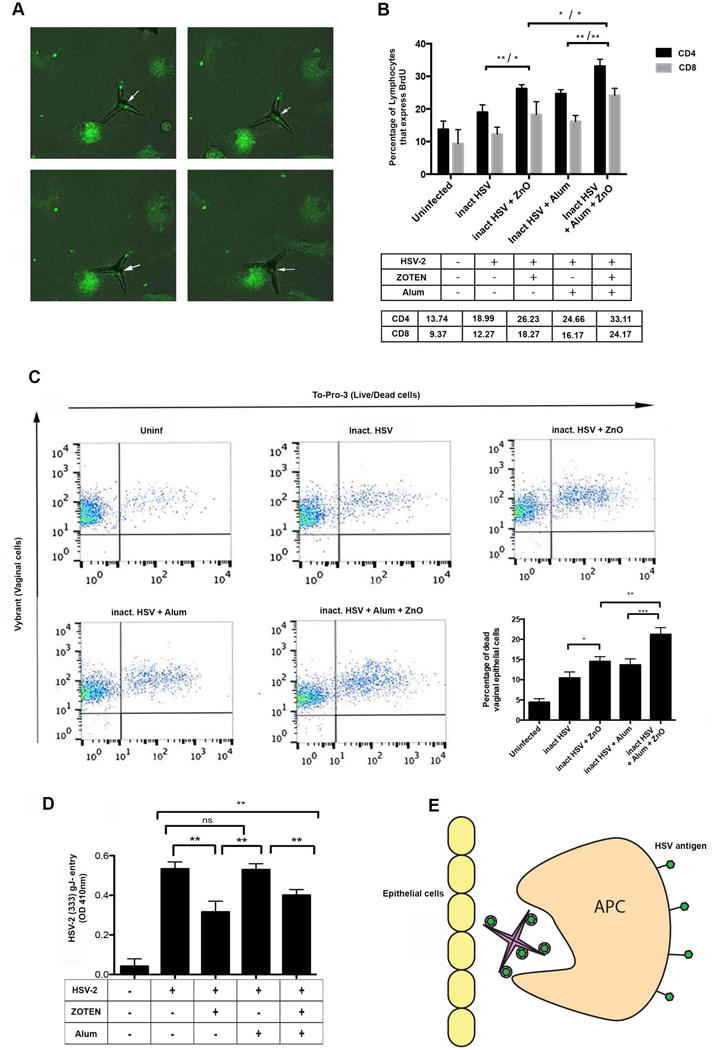
ZOTEN stimulates adaptive immune responses to HSV-2 infection
We have noticed that ZOTEN has a tendency to bind HSV-2 viral particles (7), and thus we reasoned if this interaction may enhance viral antigen accessibility to, and engulfment by, antigen-presenting cells such as dendritic cells. Dendritic cells were isolated from spleens of mice and were infected with HSV-2 in the presence of ZOTEN (HSV-2−ZOTEN combination) for 2 hours, and clearance of viral antigens by dendritic cells was monitored microscopically. We observed gradual removal of ZOTEN-bound viral particles (Fig. 4A) suggesting that ZOTEN may facilitate virus uptake by dendritic cells in the mucosal layer of the vaginal tract.
Figure 4. ZOTEN enhances anti-HSV-2 immunity and T cell responses.
A. ZOTEN-sequestered virus particles are rapidly taken up by dendritic cells. In presence of dendritic cells, the removal of distinctive GFP virus particles located at the apex and center of ZOTEN was observed. GFP virus is highlighted with white arrows. The direct interaction between ZOTEN and GFP virus is also visualized. Representative data from one of three independent experiments is shown.
B. ZOTEN stimulates CD4 and CD8 cell response. Animals were inoculated intravaginally with different treatments as mentioned in the table. Spleens of mice (n=3 each group) were extracted on day 21 post infection and equal numbers of splenocytes were incubated with HSV-2 and BrdU for 48 hrs. Y-axis represents the percentage of indicated lymphocytes that are positive for BrdU. Table shows the specific numbers for the percentage of indicated lymphocytes corresponding to the graph. Representative data from one of two independent experiments is shown.
C. Splenocytes from ZOTEN-treated mice showed higher cytotoxicity when compared to that of mock-treated mice (Cytotoxic T-lymphocyte Killing Assay). Infected Vaginal epithelial cells were stained with Vybrant dye as a cell tracer and co-cultured with extracted splenocytes at a ratio of 1:25. After 4 hours of incubation, TO-PRO-3 dye was added to each culture and analyzed by flow cytometry. Loss of membrane integrity of cells as a measure of cytotoxicity was assessed by To-Pro-3 iodide staining of DNA, which is blocked by intact cell membranes. Cytotoxicity is expressed as percentage of cell death within the entire Vybrant cell population [dead vybrant cells/ (dead + live vybrant cells)] *100. Three animals were used per mouse group. Percentage target cell death was corrected for spontaneous background death by subtracting the percentage of dead cells in control samples from dead cells within the test samples. Error bars represent S.E.M with *P≤0.05, **P≤0.01, ***P≤0.001. Representative data from one of two independent experiments is shown.
D. Sera from ZOTEN treated mice reduced HSV-2 (333) gJ- entry in Human vaginal epithelial cells (Vk2/E6). To evaluate the development of immunity against HSV-2, the virus was pretreated with sera from ZOTEN-treated, or mock-treated infected mice, and then added to Vk2/E6 cells (MOI 10) for 6 hours to assess entry. Infection was then assayed (β-galactosidase assay). HSV-2 (333) gJ- mutant virus has a gene encoding beta galactosidase. Its substrate o-nitrophenyl- β-Dgalactopyranoside (ONPG) was added to the culture. Infected cells producing virally encoded beta galactosidase enzymatically act on ONPG, which was quantified by using a spectrophotometer with optical density of 410nm. Error bars represent S.E.M from an average of 3 mice per group. Asterisks signify *P≤0.05, **P≤0.01, ***P≤0.001. Representative data from one of two independent experiments is shown.
E. Shown in the schematic is an APC cell engulfing a virus bound by ZOTEN. HSV-2 particles infecting the vaginal epithelial cells are trapped by ZOTEN near vaginal walls. After internalization, proteins from viral particles are presented on the surface of APC.
Adaptive immune responses (both cell-mediated and humoral) are key lines of defense against viral infections, such as HSV-2 genital herpes (21–26). Thus, having noticed the enhanced antigen uptake by antigen presenting cells upon ZOTEN treatment, we sought to determine the adaptive immune response profile as a function of HSV-2 genital infection in vivo, in presence or absence of ZOTEN treatment. First, we investigated whether ZOTEN can exert adjuvant properties to support development of adaptive immune responses to viral antigens. Using UV-inactivated HSV-2 virus as a source of viral antigens, we determined levels of infection-induced CD8 and CD4 T lymphocytes as a function of ZOTEN treatment. Mice were sacrificed and splenocytes were isolated 14 days post inoculation. We found that a combination of inactivated HSV-2 and ZOTEN increased T cell numbers to a greater extent than inactivated HSV-2 treatment alone (Fig. 4B). Also, the combination of alum and HSV-2 increased T cell proliferation just as much as the combination of HSV-2 and ZOTEN. This data suggests that ZOTEN can serve as an efficient adjuvant.
Having found that ZOTEN can act as an adjuvant, we further assessed the cytotoxic T-lymphocyte (CTL) cell memory responses to infection, an important adaptive immune response against viral infections (23, 24). Splenocytes from different groups of mice were assessed for developing a memory response to re-infection by HSV-2. Vaginal epithelial cells (VK2/E6E7) were infected with HSV-2 (333) at a MOI of 0.1, stained with Vybrant dye, and incubated for 24 hrs prior to co-culture with the splenocytes. The splenocytes were incubated with infected cells for 4 hours and TO-PRO-3 dye was added to culture. Cytotoxic T cell-mediated VK2/E6E7 cell lysis gives rise to a Vybrant−TO-PRO-3 double positive population of cells. We found that splenocytes of mice infected and treated with ZOTEN and inactivated HSV-2 showed significantly higher cytotoxicity towards HSV-2-infected cells, compared to those from inactivated HSV-2 alone (Fig. 4C). ZOTEN-alum combination showed a higher enhanced cytotoxic T cell response, indicating a strong immunogenicity-enhancing property of ZOTEN, which may be used in combination with existing adjuvants to achieve synergism.
Since HSV-2 genital disease is characterized by a high recurrence rate, we wanted to further explore the abilities of ZOTEN to protect against re-infection. We have found that ZOTEN stimulates memory T cell-mediated immune responses (Fig. 4C), and wanted to assess humoral immunity in response to infection in vivo upon treatment with ZOTEN, especially considering that HSV-2 suppresses humoral immunity via various mechanisms to enable uninterrupted infection (27). Sera were evaluated for their ability to inhibit entry of HSV-2 and suppress infection of cells. We found that sera from ZOTEN-treated mice significantly reduced the ability of the virus to infect cells (Fig. 4D). Interestingly, despite the fact that ZOTEN adjuvant properties were comparable to alum (Figure 4B), induction of virus-neutralizing antibody production in mice was a unique property of ZOTEN (Fig. 4D). Altogether, data suggest that ZOTEN enhances adaptive immune responses to HSV-2 infection, including memory response to re-infection, and to prevent genital disease recurrence (Fig. 4), in addition to its abilities to suppress acute (Fig. 1) and chronic (Fig. 2) disease.
Discussion
The global wide-spread nature of HSV-2, its high recurrence rate, the high susceptibility of the female reproductive tract to plethora of sexually transmitted diseases including HSV-2 (28), highlight the need for new ways to prevent or control this debilitating infection. Previously failed vaccine studies against genital herpes in humans have focused mostly on intramuscular immunization formulated in the oil-in-water emulsion with alum-based adjuvants. To obtain higher efficacy of protection there is a lot of interest to examine alternate adjuvants and routes of immunization to elicit strong protective immunity to genital herpes. The new vaccine designs or treatments need to aim to prevent disease transmission and spread to uninfected individuals. Current therapies provide little effect against disease, due to drug resistance, toxicities, and disease recurrence, and to date no vaccine is currently available for prevention or treatment of genital herpes (29). Thus the present study reports the very first evidence for the novel Microbivac concept (8), which is expected to guide future microbicide and vaccine development strategies against persistent infections. The microbivac concept uses a virus trapping agent which provides immediate protection by trapping virus particles and then presents them for mucosal immunity development. ZOTEN prevents cell entry by inhibiting the interaction between virus and cellular receptors. HSV bound to ZOTEN are taken up by APCs in the mucosal surface and are presented to prime the immune system. Given its potential use as a microbicide, ZOTEN is expected to provide immunity boost every time the virions are trapped by it. This manuscript also represents a report of a potential intravaginal vaccine, which we found to be effective in mice. While most nanoparticles have been administered intraperitoneally, intranasally or orally, we show that intravaginal inoculation can be utilized to provide microbial protection.
Demonstrating the virucidal potential of ZOTEN therapy in vivo, ZOTEN-treated mice showed significantly reduced lesion development, as less than 20% of ZOTEN-treated animals developed external lesions or detectable inflammation (Fig. 1A–E). We found that ZOTEN treatment decreased viral loads and that ZOTEN-treated mice produced significantly lower viral titres at all points of infection tested (Fig. 2A–D). Average staining score of ZOTEN-treated mice was ~2.1 contrary to a score of ~4.4 for mock group (Fig. 2B). We also found that ZOTEN-treated mice had less inflammation in the spinal cords than mock treated group, reflecting less viral dissemination into neuronal tissues, reduced neurological disease symptoms or weight loss (Fig. 3C and 3D). As an overall assessment of animal health and vitality, ZOTEN-treated mice had 100% survival rate compared to the 50%-80% mortality rates seen with the mock-treated mice at day 10 and day 17 respectively (Fig. 3F).
ZOTEN traps HSV-2 virions (7), but given its relatively large size, it cannot enter epithelial cells. We used high resolution fluorescence microscopy to demonstrate its partial engulfment of virions by dendritic cells. Gradual removal of ZOTEN-bound GFP viral particles was observed via live cell imaging (Fig. 4A), suggesting that ZOTEN may facilitate virus uptake by dendritic cells, which may facilitate a rapid clearance of trapped virions from the vaginal tract and process the virions for antigen presentation. Interestingly, a combination of inactivated HSV-2 and ZOTEN increased T cell numbers significantly to greater extent than inactivated HSV-2 treatment alone (Fig. 4B). The initial differences in CD4 and CD8 responses (Fig. 4B) generated by the ZOTEN approach may appear relatively small but they are statistically significant. It is also worth noting that the responses are expected to keep growing over time, especially given the unique advantages generated by the microbivac approach. ZOTEN is expected to be used repeatedly as a microbicide, and its virus trapping abilities and adjuvant-like properties will boost adaptive immunity, including CD4/CD8 responses, every time HSV-2 virions are trapped by this microbicide. An additional advantage is that the immunity will develop against the whole virus as antigens. While subunit vaccine studies in the past that used just adjuvanted HSV-2 gD were unable to elicit strong protective immunity against HSV-2 in clinical trials, the polyantigenic response has been alluded to be more beneficial in a HSV vaccine that uses a mutant virus by deleting gD to prevent cell entry and cell-to-cell spread (30–35).
The combination of alum and HSV-2 increased T cell proliferation just as much as the combination of HSV-2 and ZOTEN. This data suggests that ZOTEN can provide an additional benefit as an efficient adjuvant. We found that splenocytes of mice primed with ZOTEN showed significantly higher cytotoxicity towards HSV-2-infected cells, compared to those from control infected-untreated mice (Fig. 4C). ZOTEN-alum combination showed a higher enhanced cytotoxic T cell response, indicating a strong immunogenicity-enhancing property of ZOTEN, which may be used in combination with existing adjuvants to achieve synergism. We also found that sera from ZOTEN-treated mice significantly reduced the ability of the HSV to infect and enter cells, which was a unique property of ZOTEN (Fig. 4D). Another interesting observation was that HSV-2 serum entry inhibition was unique to ZOTEN. Alum enhances a general endogenous CD4 T cell responses, antibody production and CD8 T cell priming with the help of macrophages, mast cells, and eosinophils (36). The induction of cytotoxic response through generation of antibodies in alum is non-specific when compared to ZOTEN+HSV-2 complex. According to figure 4B, alum and ZOTEN have both separately shown to increase CD4 and CD8 cell populations. However in figure 4D, serum entry inhibition studies have shown that blocking entry of HSV-2 is specific to ZOTEN but not alum, which suggests that antibodies against HSV-2 are specifically produced in ZOTEN treated mice. This could be attributed to the specific B cell response due to priming the immune system against HSV-2 in HSV-2/ZOTEN treated mice. Altogether, these data suggest that ZOTEN enhances adaptive immune responses to HSV-2 infection, including memory response to re-infection, suggesting the powerful properties of ZOTEN to prevent genital disease recurrence (Fig. 4), in addition to its abilities to suppress acute (Fig. 1) and chronic (Fig. 2) diseases.
In the animal studies presented here and other in vitro studies performed earlier, ZOTEN was chosen to develop the microbivac concept on the basis of multiple parameters. The chemical content, ZnO is very well-characterized in cosmetic and clinical studies and well-tolerated during topical applications (37). Many beauty products contain ZnO in different formats (powder, liquid, gel) and it has been tested in clinical trials for anti-HSV effects. However, for further development of ZOTEN for potential clinical usage as a microbivac against genital herpes, additional dose optimization studies and efficacy determination studies will be needed. While mouse is generally a good model of HSV-2 genital infection, additional models such as rabbits or guinea pigs, which spontaneously reactivate the virus, need to be examined for microbicide and vaccine efficacy studies (38). Likewise, toxicology and pharmacokinetic studies, and lead optimization studies need to be performed for future clinical applications. In the studies presented here, no significant adverse effects or toxicity was exhibited in the animal studies even at the highest dosage; however, long-term efficacy, off-target effects and toxicology studies will be needed. Furthermore, recent advances in topical formulations need to be combined to even further reduce any side effects of ZOTEN. Design of more specific and even higher binding ZOTEN in the future could provide some advantages over the nonselective ZOTEN. Overall, the described studies represent the very first inhibition of viral infection and protection from future infection by a Microbivac. Thus, our studies represent an approach to antivirals with extensive potential derived from studies of viral entry inhibition and the promise of Microbivac therapy.
In conclusion, this paper provides evidence on the usefulness of ZOTEN as an effective virostatic platform, which also provides adjuvant-benefits in combination with the captured virions for induction of protective immunity against genital herpes in mice. Zinc Oxide tetrapod structures could be applied to contraceptives as a means of drug delivery, which will allow the release of the drug in a localized and efficient manner. Given that ZOTEN works therapeutically in vitro (7), it is likely that existing symptoms can also be improved in infected mice as ZOTEN will inhibit the spread of newly produced HSV-2 by trapping them. Future studies investigating the direct therapeutic aspect of ZOTEN in vivo will be performed. In addition, future clinical studies are likely to provide more information on versatile use of ZOTEN to control persistent infections.
In future, our results require further understanding of ZOTEN for induction of protective immunity in the female genital tract against genital herpes. Additional studies will be needed to elucidate the relative contribution of T cells and antibody response to the observed protection in mice. Moreover, studies using rabbits or guinea pig models of recurrent genital herpes are required to evaluate the potential of robust protective immunity to primary and recurrent genital herpes. A comparative harmonized analysis of different adjuvants, including those tested previously in human trials is also required to pinpoint the relative usefulness of ZOTEN vs. other adjuvants and for optimizing the immunization regimes for induction of protective immune responses to HSV-2.
Acknowledgments
This work was supported by the National Institutes of Health grants AI103754 (D.S.) and a core grant (EY001792).
Footnotes
Disclosures
The authors declare no conflict of interest.
References
- 1.Whitley RJ, Roizman B. Herpes simplex virus infections. Lancet. 2001;357:1513–1518. doi: 10.1016/S0140-6736(00)04638-9. [DOI] [PubMed] [Google Scholar]
- 2.Shukla D, Spear PG. Herpesviruses and heparan sulfate: an intimate relationship in aid of viral entry. J. Clin. Invest. 2001;108:503–510. doi: 10.1172/JCI13799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrei G, Snoeck R. Herpes simplex virus drug-resistance: new mutations and insights. Curr. Opin. Infect. Dis. 2013;26:551–560. doi: 10.1097/QCO.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 4.Sanvicens N, Marco MP. Multifunctional nanoparticles--properties and prospects for their use in human medicine. Trends. Biotechnol. 2008;26:425–433. doi: 10.1016/j.tibtech.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Davis ME, Chen ZG, Shin DM. Nanoparticle therapeutics: an emerging treatment modality for cancer. Nat. Rev. Drug. Discov. 2008;7:771–782. doi: 10.1038/nrd2614. [DOI] [PubMed] [Google Scholar]
- 6.Hrkach J, Von Hoff D, Mukkaram Ali M, Andrianova E, Auer J, Campbell T, De Witt D, Figa M, Figueiredo M, Horhota A, Low S, McDonnell K, Peeke E, Retnarajan B, Sabnis A, Schnipper E, Song JJ, Song YH, Summa J, Tompsett D, Troiano G, Hoven TVG, Wright J, LoRusso P, Kantoff PW, Bander NH, Sweeney C, Farokzad OC, Langer R, Zale S. Preclinical development and clinical translation of a PSMA-targeted docetaxel nanoparticle with a differentiated pharmacological profile. Sci. Transl. Med. 2012;4:128–139. doi: 10.1126/scitranslmed.3003651. [DOI] [PubMed] [Google Scholar]
- 7.Antoine TE, Mishra YK, Trigilio J, Tiwari V, Adelung R, Shukla D. Prophylactic, therapeutic and neutralizing effects of zinc oxide tetrapod structures against herpes simplex virus type-2 infection. Antiviral. Res. 2012;96:363–375. doi: 10.1016/j.antiviral.2012.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coleman JL, Shukla D. Recent advances in vaccine development for herpes simplex virus types I and II. Hum. Vaccin. Immunother. 2013;9:729–735. doi: 10.4161/hv.23289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iwanaga H, Fujii M, Takeeuchi S. Growth model of tetrapod zinc oxide particles. J Cryst. Growth. 1993;134:275–280. [Google Scholar]
- 10.Docherty JJ, Fu MM, Hah JM, Sweet TJ, Faith SA, Booth T. Effect of resveratrol on herpes simplex virus vaginal infection in the mouse. Antiviral Res. 2005;67:155–162. doi: 10.1016/j.antiviral.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 11.Park PJ, Antoine TE, Farooq AV, Valyi-Nagy T, Shukla D. An investigative peptide-acyclovir combination to control herpes simplex virus type 1 ocular infection. Invest Ophthalmol Vis Sci. 2013;54:6373–6381. doi: 10.1167/iovs.13-12832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peng T, Ponce-de-Leon M, Jiang H, Dubin G, Lubinski JM, Eisenberg RJ, Cohen GH. The gH-gL complex of herpes simplex virus (HSV) stimulates neutralizing antibody and protects mice against HSV type 1 challenge. 1998;72:65–72. doi: 10.1128/jvi.72.1.65-72.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mishra YK, Modi G, Cretu V, Postica V, Lupan O, Reimer T, Paulowicz I, Hrkac V, Benecke W, Kienle L, Adelung R. Direct Growth of Freestanding ZnO Tetrapod Networks for Multifunctional Applications in Photocatalysis, UV Photodetection, and Gas Sensing. ACS Appl. Mater. Interfaces. 2015;26:14303–14316. doi: 10.1021/acsami.5b02816. [DOI] [PubMed] [Google Scholar]
- 14.Ferlazzo G, Thomas D, Lin SL, Goodman K, Morandi B, Muller WA, Moretta A, Munz C. The abundant NK cells in human secondary lymphoid tissues require activation to express killer cell Ig-like receptors and become cytolytic. J. Immunol. 2004;172:1455–1462. doi: 10.4049/jimmunol.172.3.1455. [DOI] [PubMed] [Google Scholar]
- 15.Lee-MacAry AE, Ross EL, Davies D, Laylor R, Honeychurch J, Glennie MJ, Snary D, Wilkinson RW. Development of a novel flow cytometric cell-mediated cytotoxicity assay using the fluorophores PKH-26 and TO-PRO-3 iodide. J. Immunol. Methods. 2001;252:83–92. doi: 10.1016/s0022-1759(01)00336-2. [DOI] [PubMed] [Google Scholar]
- 16.Leenen PJ, Radosević K, Voerman JS, Salomon B, van Rooijen N, Klatzmann D, van Ewijk W. Heterogeneity of mouse spleen dendritic cells: in vivo phagocytic activity, expression of macrophage markers, and subpopulation turnover. J Immunol. 1998;160:2166–2173. [PubMed] [Google Scholar]
- 17.Adelung R, Kaps S, Mishra YK, Claus M, Presusse T, Wolpert C. German Patent. Germany: 2011. Elastic material with a pore space bridge at the particle level by nanobridges between particles. [Google Scholar]
- 18.Mishra YK, Kaps S, Claus M, Wille S, Kovalev A, Gorb SN, Adelung R. Fabrication of Macroscopically Flexible and Highly Porous 3D Semiconductor Networks from Interpenertrating Nanostructiures by a Simple Flame Transport Approach. Part. Part. Syst. Char. 2013;30:775–783. [Google Scholar]
- 19.Parr MB, Kepple L, McDermott MR, Drew MD, Bozzola JJ, Parr EL. A mouse model for studies of mucosal immunity to vaginal infection by herpes simplex virus type 2. Lab Invest. 1994;70:369–380. [PubMed] [Google Scholar]
- 20.Taylor JM, Lin E, Susmarski N, Yoon M, Zago A, Ware CF, Pfeffer K, Miyoshi J, Takai Y, Spear PG. Alternative entry receptors for herpes simplex virus and their roles in disease. Cell.Host. Microbe. 2007;2:19–28. doi: 10.1016/j.chom.2007.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koelle DM, Corey L. Herpes simplex: insights on pathogenesis and possible vaccines. Annu. Rev. Med. 2008;59:381–395. doi: 10.1146/annurev.med.59.061606.095540. [DOI] [PubMed] [Google Scholar]
- 22.Koelle DM, Chen HB, Gavin MA, Wald A, Kwok WW, Corey L. CD8 CTL from genital herpes simplex lesions: recognition of viral tegument and immediate early proteins and lysis of infected cutaneous cells. J. Immunol. 2001;166:4049–4058. doi: 10.4049/jimmunol.166.6.4049. [DOI] [PubMed] [Google Scholar]
- 23.Koelle DM, Frank JM, Johnson ML, Kwok WW. Recognition of herpes simplex virus type 2 tegument proteins by CD4 T cells infiltrating human genital herpes lesions. J. Virol. 1998;72:7476–7483. doi: 10.1128/jvi.72.9.7476-7483.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van Lint A, Ayers M, Brooks AG, Coles RM, Heath WR, Carbone FR. Herpes simplex virus-specific CD8+ T cells can clear established lytic infections from skin and nerves and can partially limit the early spread of virus after cutaneous inoculation. J. Immunol. 2004;172:392–397. doi: 10.4049/jimmunol.172.1.392. [DOI] [PubMed] [Google Scholar]
- 25.Lang A, Nikolich-Zugich J. Development and migration of protective CD8+ T cells into the nervous system following ocular herpes simplex virus-1 infection. J. Immunol. 2005;174:2919–2925. doi: 10.4049/jimmunol.174.5.2919. [DOI] [PubMed] [Google Scholar]
- 26.Chentoufi AA, Benmohamed L. Mucosal herpes immunity and immunopathology to ocular and genital herpes simplex virus infections. Clin. Dev. Immunol. 2012;2012:1–22. doi: 10.1155/2012/149135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Metzger B, Podlech J, Müller S, Falke D. Suppression of humoral immune response against herpes simplex virus induced by defective strains, ts- and TK- mutants. Arch. Virol. 1998;99:143–152. doi: 10.1007/BF01311065. [DOI] [PubMed] [Google Scholar]
- 28.Gupta R, Warren T, Wald A. Genital herpes. Lancet. 2007;370:2127–2137. doi: 10.1016/S0140-6736(07)61908-4. [DOI] [PubMed] [Google Scholar]
- 29.Awasthi S, Friedman HM. Status of prophylactic and therapeutic genital herpes vaccines. Curr. Opin. Infect. Dis. 2013;26:551–560. doi: 10.1016/j.coviro.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 30.Mertz GJ, Ashley R, Burke RL, Benedetti J, Critchlow C, Jones CC, Corey L. Double-blind, placebocontrolled trial of a herpes simplex virus type 2 glycoprotein vaccine in persons at high risk for genital herpes infection. The Journal of Infectious Diseases. 1990;161:653–660. doi: 10.1093/infdis/161.4.653. [DOI] [PubMed] [Google Scholar]
- 31.Corey L, Langenberg AG, Ashley R, Sekulovich RE, Izu AE, Douglas JM, Jr, Handsfield HH, Warren T, Marr L, Tyring S, DiCarlo R, Adimora AA, Leone P, Dekker CL, Burke RL, Leong WP, Straus SE. Recombinant glycoprotein vaccine for the prevention of genital HSV-2 infection: two randomized controlled trials. Chiron HSV Vaccine Study Group. JAMA. 1999;282:331–340. doi: 10.1001/jama.282.4.331. [DOI] [PubMed] [Google Scholar]
- 32.Kohl S, Charlebois ED, Sigouroudinia M, Goldbeck C, Hartog K, Sekulovich RE, Langenberg AG, Burke RL. Limited antibody-dependent cellular cytotoxicity antibody response induced by a herpes simplex virus type 2 subunit vaccine. The Journal of Infectious Diseases. 2000;181:335–339. doi: 10.1086/315208. [DOI] [PubMed] [Google Scholar]
- 33.Bernstein DI, Aoki FY, Tyring SK, Stanberry LR, St-Pierre C, Shafran SD, Leroux-Roels G, Van Herck K, Bollaerts A, Dubin G Glaxo Smith Kline Herpes Vaccine Study Group. Safety and immunogenicity of glycoprotein D-adjuvant genital herpes vaccine. Clinical Infectious Diseases. 2005;40:1271–1281. doi: 10.1086/429240. [DOI] [PubMed] [Google Scholar]
- 34.Belshe RB, Leone PA, Bernstein DI, Wald A, Levin MJ, Stapleton JT, Gorfinkel I, Morrow RL, Ewell MG, Stokes-Riner A, Dubin G, Heineman TC, Schulte JM, Deal CD Herpevac Trial for Women. Efficacy results of a trial of a herpes simplex vaccine. The New England Journal of Medicine. 2012;366:34–43. doi: 10.1056/NEJMoa1103151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Petro C, González PA, Cheshenko N, Jandl T, Khajoueinejad N, Bénard A, Sengupta M, Herold BC, Jacobs WR. Herpes simplex type 2 virus deleted in glycoprotein D protects against vaginal, skin and neural disease. Elife. 2015 Mar 10;4 doi: 10.7554/eLife.06054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McKee AS, Munks MW, MacLeod MK, Fleenor CJ, Van Rooijen N, Kappler JW, Marrack P. Alum induces innate immune responses through macrophage and mast cell sensors, but these sensors are not required for alum to act as an adjuvant for specific immunity. J Immunol. 2009 Oct 1;183(7):4403–4414. doi: 10.4049/jimmunol.0900164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nohynek GJ, Dufour EK, Roberts MS. Nanotechnology, cosmetics and the skin: is there a health risk? Skin. Pharmacol. Physiol. 2008;21:136–149. doi: 10.1159/000131078. [DOI] [PubMed] [Google Scholar]
- 38.Dasgupta G, BenMohamed L. Of mice and not humans: how reliable are animal models for evaluation of herpes CD8(+)-T cell-epitopes-based immunotherapeutic vaccine candidates? Vaccine. 2011;29:5824–5836. doi: 10.1016/j.vaccine.2011.06.083. [DOI] [PMC free article] [PubMed] [Google Scholar]