Abstract
Background
The aim of this observational study was to determine whether subthreshold bipolarity affects treatment response and remission in patients with major depressive disorder receiving antidepressant (AD) monotherapy over a 6-month follow-up period.
Methods
Seventy-eight patients with major depressive disorder were stratified into two subgroups according to the presence of subthreshold bipolarity, identified using the Korean version of the Mood Disorder Questionnaire (K-MDQ), which classifies patients as positive for a screening of bipolarity based on the cutoff for the total K-MDQ score (ie, 7 points). They received AD monotherapy such as escitalopram, sertraline, paroxetine, or tianeptine for 6 months. The Beck Depression Inventory (BDI), Hamilton Depression Rating Scale (HAMD), Hamilton Anxiety Scale, and Beck Scale for Suicide Ideation were applied at baseline, 1 week, 3 weeks, 2 months, 3 months, and 6 months.
Results
The mean HAMD, BDI, and Beck Scale for Suicide Ideation scores were higher in the bipolarity group than in the nonbipolarity group at 3 weeks. The mean BDI score was also higher in the bipolarity group than in the nonbipolarity group at 6 months. Evaluation of the ratio of improvement for each scale revealed different patterns of percentage changes between the two groups over the 6-month follow-up period. Furthermore, the response and remission rates (as assessed using BDI and HAMD scores) were higher in the nonbipolarity group than in the bipolarity group, with the exception of HAMD scores at the 3-week follow-up time point.
Conclusion
The findings of this study showed that depressed patients with bipolarity had a worse response to AD monotherapy than did those without bipolarity.
Keywords: subthreshold bipolarity, antidepressant, major depressive disorder, treatment response, remission
Introduction
Patients with major depressive episodes (MDEs) of bipolar disorder (BD) types I or II (BD I or BD II, respectively) generally exhibit weak responses to antidepressant (AD) therapy.1,2 In addition, most recent findings indicate that this high rate of resistance to ADs is not limited to BD I or II. Eighty percent of patients with AD-resistant unipolar depression were BD I, II, and not otherwise specified, and bipolar spectrum disorder (BSD) at 1-year follow-up.3 In an analysis of treatment-resistant depression, AD was associated with a poor outcome in both BD and BSD patients.4 Another study reported that patients with subthreshold bipolarity exhibited a poor prognosis over a 5-year follow-up period.5 Thus, the diagnosis of BD or BSD is underestimated, and the most common reason for treatment resistance appears to be masked BD. Furthermore, some investigators claimed that patients with Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV)-defined unipolar major depressive disorder (MDD) with subthreshold bipolar features should be excluded from drug trials.6
However, a recent meta-analysis found no significant difference in short-term AD response rates between patients with unipolar depression and BD.7 In addition, some investigators reported that fluoxetine monotherapy may be an effective short-term treatment for a BD II MDE with a relatively low rate of syndromal hypomanic episodes.8 These investigators also reported similar results in patients with rapid cycling BD II.9 In addition, some other investigators evaluated Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study data, and reported that recent hypomanic- or manic-like symptoms, family history of BD, and early illness onset were not associated with treatment resistance to AD, although irritability, psychic agitation, increased appetite, and psychotic-like symptoms were significantly associated with a worse treatment response to AD.10 Together these findings indicate that the effectiveness of ADs in patients with BD or BSD remains a matter of controversy.
The aim of this observational study was to determine whether subthreshold bipolarity affects treatment response and remission in patients with MDD – defined according to criteria in DSM-IV – receiving AD monotherapy over a 6-month follow-up period.
Methods
Subjects and study design
In total, 102 outpatients aged between 18 and 65 years who met the DSM-IV Text Revision criteria for MDD were recruited at Ilsan Paik Hospital for Korean MDD cohort for suicide prevention (KOMDD study). The following inclusion criteria of this cohort were applied: 1) having total Beck Depression Inventory (BDI) or Hamilton Depression Rating Scale (HAMD) scores exceeding 19 or 17, respectively, prior to the treatment and 2) no history of AD treatment within 12 weeks before first visit to our hospital. The exclusion criteria were the presence of 1) previous hypomanic/manic episode, 2) a high suicide risk, 3) history of brain trauma or organic brain disease, or 4) neurological disease. Depression severity was assessed using HAMD and BDI scores at baseline, 1 week, 3 weeks, 2 months, 3 months, and 6 months. Furthermore, the Hamilton Anxiety Scale, Beck Scale for Suicidal Ideation (BSS), and DSM-IV manic or hypomanic criteria for switch were applied at baseline, 1 week, 3 weeks, 2 months, 3 months, and 6 months. In addition, bipolarity screening was performed at baseline using the Korean version of the Mood Disorder Questionnaire (MDQ; K-MDQ), which classifies patients as positive for a screening of bipolarity based on a cutoff total K-MDQ score of 7 points.
Current data are a part of this KOMDD cohort. In addition, a post hoc analysis after a 6-month follow-up period was performed. Among initial 102 subjects, 78 subjects participated in MDD treatment course, which is similar to real-world setting for MDD pharmacotherapy (initially AD monotherapy). Based on clinical impression, subjects who need to receive augmentation or combination treatment afterward for analyzing the influence of bipolarity to AD monotherapy were excluded in the current analysis. After a 6-month follow-up period, 78 subjects were stratified into two groups according to the presence of subthreshold bipolarity, which was established using the K-MDQ, which classifies patients as positive for a screening of bipolarity based on a cutoff total K-MDQ score of 7 points, and history taking (nonbipolarity group [n=48] vs bipolarity group [n=30]). The patients received AD monotherapy such as escitalopram, sertraline, paroxetine, or tianeptine for 6 months. Treatment response was defined as ≥50% improvement in mean HAMD or BDI scores from baseline. In addition, remission was defined as ≤7 points of HAMD or ≤10 points of BDI.
The study protocol was approved by the Ethics Committee of Ilsan Paik Hospital, and written informed consent to participate was obtained from all patients before beginning the investigation.
Statistical analysis
An observed case analysis was used to assess the efficacy during the 6-month follow-up period. Student’s t-test and χ2 test were used to compare clinical variables between depressed patients with and without bipolarity. Repeated-measures analysis of variance was also conducted to analyze the differences in each scale between the two groups throughout the 6 months. In addition, Student’s t-test was used to analyze the difference between the two groups in each scale at each visit.
Results
A total of 78 patients were enrolled; the completion rate of this study is 37.5% (18/48) in the nonbipolarity group and 26.6% (8/30) in the bipolarity group for 6 months. Table 1 compares the baseline clinical variables between the bipolarity and nonbipolarity groups. The mean baseline total BSS and K-MDQ scores differed significantly between the bipolarity and nonbipolarity groups, as did the frequency of a history of suicide attempt. In contrast, the mean baseline total BDI, HAMD, and Hamilton Anxiety Scale scores did not differ significantly between the two groups. In addition, only one of the patients among the entire cohort experienced hypomanic conversion.
Table 1.
Comparison of baseline clinical variables between groups with (+) and without (−) subthreshold bipolarity, defined according to a predefined cutoff (7 points) score on K-MDQ
| Variable | Bipolarity (−) (n=48) |
Bipolarity (+) (n=30) |
P-value |
|---|---|---|---|
| Age (years) | 38.90±12.78 | 39.13±15.31 | 0.94 |
| Sex (male/female) | 11/37 | 6/24 | 0.76 |
| Suicide attempt history (no/yes) | 33/15 | 13/17 | 0.026* |
| Baseline BDI score | 25.75±9.52 | 29.6±9.72 | 0.089 |
| Baseline HAMD score | 19.21±4.73 | 18.5±5.39 | 0.54 |
| Baseline HAMA score | 20.31±6.05 | 22.07±6.31 | 0.22 |
| Baseline BSS score | 9.44±7.71 | 16.67±9.97 | <0.01** |
| K-MDQ score | 3.85±1.57 | 9.63±2.01 | <0.01** |
Notes:
P<0.05,
P<0.01. Except where indicated otherwise, the data are mean ± SD.
Abbreviations: BDI, Beck Depression Inventory; HAMD, Hamilton Depression Rating Scale; HAMA, Hamilton Anxiety Rating Scale; BSS, Beck Scale for Suicide Ideation; K-MDQ, Korean version of the Mood Disorder Questionnaire; SD, standard deviation.
The mean HAMD, BDI, and BSS scores were higher in the bipolarity group than in the nonbipolarity group at 3 weeks (Figures 1–3). The mean BDI score was also higher in the bipolarity group than in the nonbipolarity group at 6 months (Figure 2). In particular, the mean BDI score in the bipolarity group at the final visit (at 6 months) was more than 20 points. In addition, none of the scores on all scales differed significantly between the two groups at the 6-month follow-up on repeated analysis of variance. However, when the ratio of the change compared to scores attained at previous visits for each scale was evaluated (eg, visit 1 BDI - visit 2 BDI/visit 1 BDI ×100%), different patterns emerged between the two groups over the 6-month follow-up period (Figures 4–7).
Figure 1.
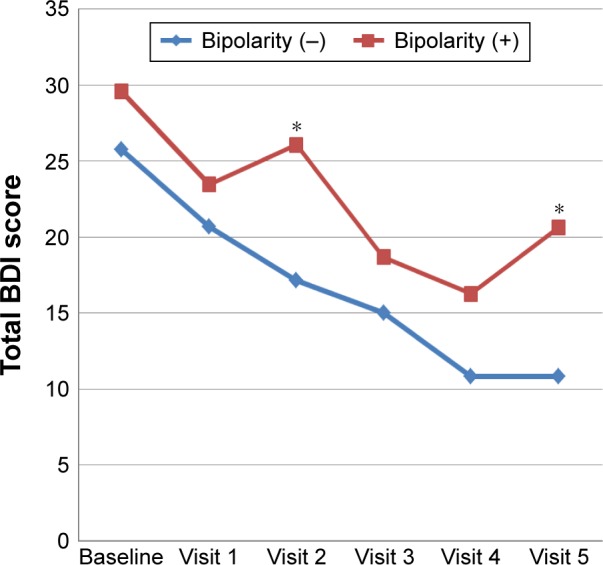
Comparison of mean BDI scores over a 6-month follow-up period between depressed patients with and without bipolarity.
Note: *P<0.05.
Abbreviation: BDI, Beck Depression Inventory.
Figure 2.
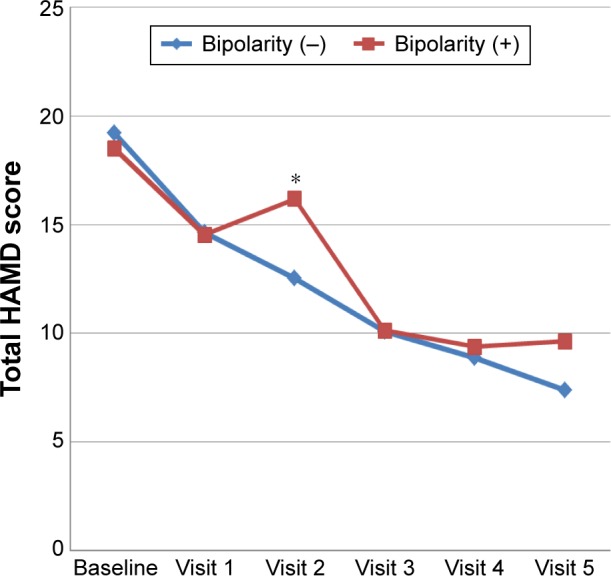
Comparison of mean HAMD scores over a 6-month follow-up period between depressed patients with and without bipolarity.
Note: *P<0.05.
Abbreviation: HAMD, Hamilton Depression Rating Scale.
Figure 3.
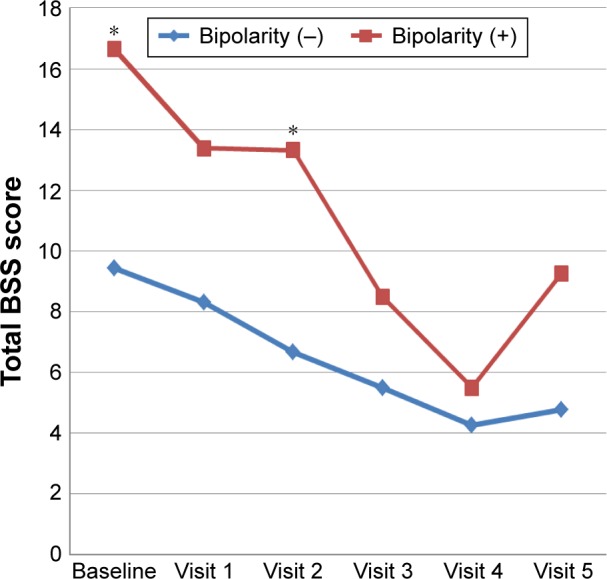
Comparison of mean BSS scores over a 6-month follow-up period between depressed patients with and without bipolarity.
Note: *P<0.05.
Abbreviation: BSS, Beck Scale for Suicide Ideation.
Figure 4.
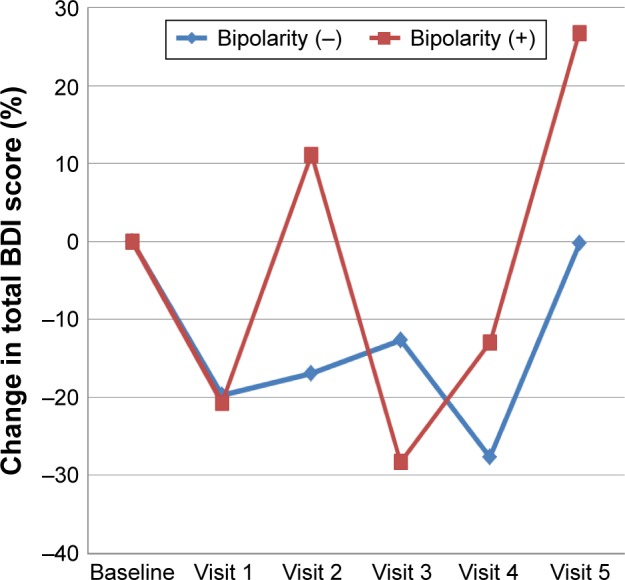
Comparison of the ratio of the change in mean BDI score relative to the score attained at the previous visit over the 6-month follow-up period between depressed patients with and without bipolarity.
Abbreviation: BDI, Beck Depression Inventory.
Figure 5.
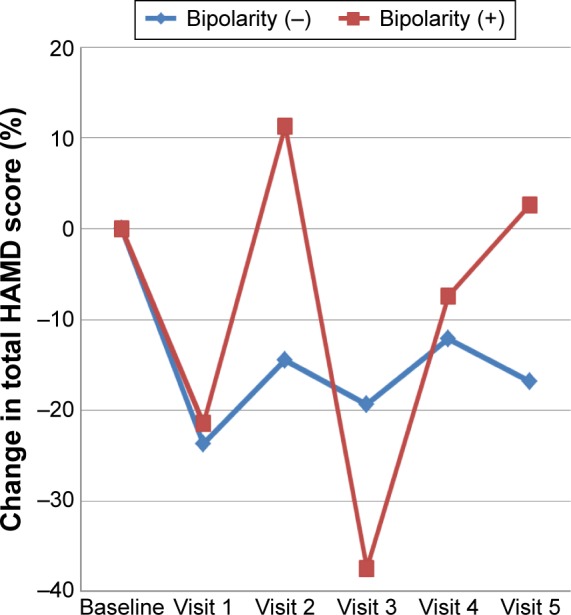
Comparison of the ratio of the change in mean HAMD score relative to the score attained at the previous visit over the 6-month follow-up period between depressed patients with and without bipolarity.
Abbreviation: HAMD, Hamilton Depression Rating Scale.
Figure 6.
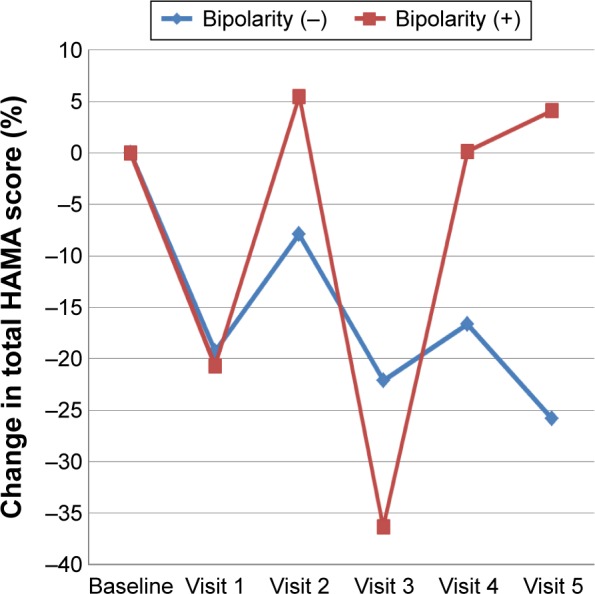
Comparison of the ratio of the change in mean HAMA score relative to the score attained at the previous visit over the 6-month follow-up period between depressed patients with and without bipolarity.
Abbreviation: HAMA, Hamilton Anxiety Rating Scale.
Figure 7.
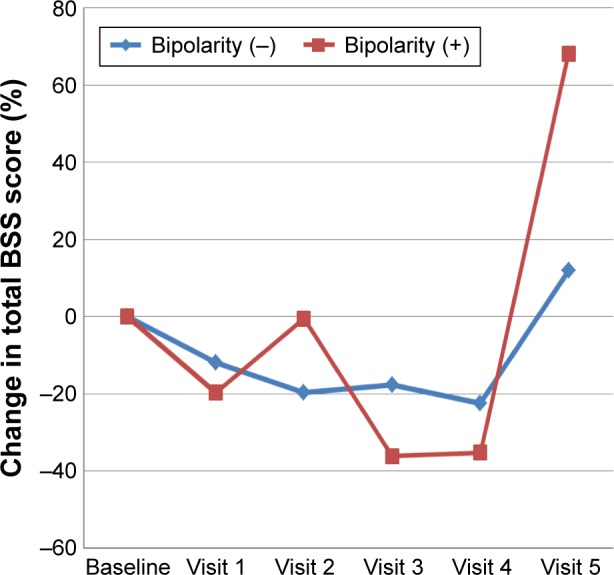
Comparison of the ratio of the change in mean BSS score relative to the score attained at the previous visit over the 6-month follow-up period between depressed patients with and without bipolarity.
Abbreviation: BSS, Beck Scale for Suicide Ideation.
The response and remission rates of the nonbipolarity group, as assessed using BDI and HAMD scores, were higher than those of the bipolarity group, with the exception of those at the 3-week follow-up for HAMD (eg, the number needed to treat was typically three or four using either BDI or HAMD at 6 months; Table 2).
Table 2.
Comparison of response and remission rates (as reflected by BDI and HAMD scores) between patients with and without bipolarity
| Follow-up visit | BDI
|
HAMD
|
||
|---|---|---|---|---|
| Bipolarity (−) | Bipolarity (+) | Bipolarity (−) | Bipolarity (+) | |
| 1 week (partial response rate) | 45.8% | 36.4% | 45.0% | 32.0% |
| 3 weeks (response rate) | 30.6% | 16.0% | 31.6% | 7.7% |
| 2 months (remission rate) | 40.0% | 31.3% | 30.0% | 37.5% |
| 3 months (remission rate) | 50.0% | 27.3% | 53.8% | 38.5% |
| 6 months (remission rate) | 50.0% | 25.0% | 66.7% | 37.5% |
Abbreviations: BDI, Beck Depression Inventory; HAMD, Hamilton Depression Rating Scale.
Discussion
This is the first study to evaluate whether subthreshold bipolarity affects treatment response and remission in patients with MDD receiving AD monotherapy over a 6-month follow-up period. The mean baseline total BSS and K-MDQ scores differed significantly between the bipolarity and nonbipolarity groups, as did the frequency of a history of suicide attempt. Thus, these patients with bipolarity seem to be vulnerable to suicide.
MDD patients with subthreshold bipolarity had a higher total BDI score than those without subthreshold bipolarity at both 3 weeks and 6 months. In particular, the mean BDI score of the bipolarity group was more than 20 points at 6 months, which indicates relapse of depression with moderate severity. In addition, the response and remission rates in the nonbipolarity group, as assessed using BDI and HAMD scores, were higher than in the bipolarity group, with the exception of the 3-week follow-up score for HAMD. Thus, the bipolarity group appeared to respond worse to AD monotherapy than the nonbipolarity group. These results corresponded with previous studies,11–13 which found that underlying bipolarity was an important contributor to AD nonresponse. Furthermore, Correa et al reviewed 196 articles and found a high rate of conversion of treatment-resistant depression into BD.4 Maalouf et al also found that depressed patients with subsyndromal manic symptoms responded less to AD than those without the same symptoms, although that study only involved adolescents.14
In addition to manic-like symptoms, O’Donovan et al found that patients with bipolarity including family history of BD or suicide, early onset, mixed symptoms, and agitation exhibited a lower rate of response to AD monotherapy compared to patients without bipolarity, although that study was retrospective.15 Recently, BD I differed from MDD in terms of greater rates of psychomotor retardation and psychotic features.16 In addition, BD II was distinguished from MDD by the greater likelihood of mixed features.16 However, a previous (STAR*D) post hoc analysis revealed that while psychosis and depression severity were associated with treatment resistance, a family history of BD and manic-like symptoms were not.10 In addition, the BSD criteria suggested by Ghaemi et al17 did not predict treatment resistance, and some investigators found that fluoxetine monotherapy may be a more effective and tolerable treatment in patients with BD II than lithium.8 Thus, the relationship between treatment resistance and BD or bipolarity remains unclear.
Intriguingly, the changes in the four scales in the bipolarity group exhibited a wax-and-wane pattern with a “W” shape, which was not seen in the nonbipolarity group (Figures 3–7). This reflects an alternation of improvement and aggravation in the bipolarity group when they were evaluated over a short-term period; for example, there was a 10% aggravation of HAMD score from visit 2 to visit 3, but an approximate 40% improvement on the same scale from visit 3 to visit 4 in that patient group (Figure 5). Thus, clinicians must identify the presence of subthreshold bipolarity in patients with MDD and will then know to expect this waxing and waning pattern in their treatment response to AD monotherapy and a low remission rate in that patient group.
The findings regarding manic or hypomanic switch with AD use in BD are also controversial. Some investigators have found that AD can cause (hypo)manic switch in BD during acute depressive and maintenance phase.18,19 However, hypomanic switch occurred in only one patient with subthreshold bipolarity in the present study. Bond et al found that the risk of (hypo)manic switch with AD use in BD II is intermediate between that in BD I and MDD.20 Thus, it is possible that the risk of (hypo)manic switch depends on the subtype of BD. However, in the large, randomized, controlled Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) study, there was no difference in the rate of (hypo)manic switch or in the efficacy between mood stabilizer plus AD (eg, sertraline or bupropion) and mood stabilizer plus placebo in patients with BDs I and II.2 However, the patients in both the groups of that study were allowed to use other drugs with an AD effect, such as quetiapine, olanzapine, and lamotrigine, as well as mood stabilizers.21 Many clinicians still prefer to prescribe a combination treatment of mood stablilizer and AD to depressed patients with BD. In addition, in one meta-analysis, the pooled relative risk of (hypo)manic switch indicated a lack of significant difference in responses of unipolar and BD patients in acute MDEs.7 Thus, the available evidence is not sufficient to draw the conclusion that ADs such as selective serotonin-reuptake inhibitors should not be used in patients with BD or bipolarity due to manic or hypomanic switch. However, the findings of the present study suggest that the reason that care should be taken when prescribing ADs (and especially selective serotonin-reuptake inhibitors) in patients with bipolarity is not AD tolerability (eg, manic switch), but rather efficacy.
This study was subject to several limitations. K-MDQ played an important role in dividing the patients into two groups. However, scores on that scale are not specific to BD; Zimmerman et al found that while MDQ mainly identifies mood instability, as opposed to distinct episodes of abnormal mood, many patients who score positive on the screen meet the criteria for borderline personality disorder.22 However, even if it is accepted that MDQ positivity does not necessarily reflect the presence of BD, in this (MDQ-positive) subgroup, the finding that the AD response was lower has clinical significance. In addition, patients with borderline personality disorder were excluded in our study. Second, the sample was small and the study did not have a randomized design. Third, the number of comparisons probably can affect type I error. Notwithstanding these limitations, the present study was performed in a real clinical setting. Randomized and controlled studies with large samples are needed to confirm the present findings.
Acknowledgments
This study was supported by a grant from the National Research Foundation of Korea (NRF), funded by the Ministry of Education (NRF-2014R1A1A2A10059345). The authors would like to thank Jo BW for her assistance with data collection.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Pacchiarotti I, Bond DJ, Baldessarini RJ, et al. The International Society for Bipolar Disorders (ISBD) task force report on antidepressant use in bipolar disorders. Am J Psychiatry. 2013;170(11):1249–1262. doi: 10.1176/appi.ajp.2013.13020185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356(17):1711–1722. doi: 10.1056/NEJMoa064135. [DOI] [PubMed] [Google Scholar]
- 3.Sharma V, Khan M, Smith A. A closer look at treatment resistant depression: is it due to a bipolar diathesis? J Affect Disord. 2005;84(2–3):251–257. doi: 10.1016/j.jad.2004.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Correa R, Akiskal H, Gilmer W, Nierenberg AA, Trivedi M, Zisook S. Is unrecognized bipolar disorder a frequent contributor to apparent treatment resistant depression? J Affect Disord. 2010;127(1–3):10–18. doi: 10.1016/j.jad.2010.06.036. [DOI] [PubMed] [Google Scholar]
- 5.Maj M, Pirozzi R, Magliano L, Fiorillo A, Bartoli L. Agitated “unipolar” major depression: prevalence, phenomenology, and outcome. J Clin Psychiatry. 2006;67(5):712–719. doi: 10.4088/jcp.v67n0504. [DOI] [PubMed] [Google Scholar]
- 6.Rihmer Z, Dome P, Gonda X. Antidepressant response and subthreshold bipolarity in “unipolar” major depressive disorder: implications for practice and drug research. J Clin Psychopharmacol. 2013;33(4):449–452. doi: 10.1097/JCP.0b013e318299d2d5. [DOI] [PubMed] [Google Scholar]
- 7.Vazquez GH, Tondo L, Undurraga J, Baldessarini RJ. Overview of antidepressant treatment of bipolar depression. Int J Neuropsychopharmacol. 2013;16(7):1673–1685. doi: 10.1017/S1461145713000023. [DOI] [PubMed] [Google Scholar]
- 8.Amsterdam JD, Shults J. Efficacy and mood conversion rate of short-term fluoxetine monotherapy of bipolar II major depressive episode. J Clin Psychopharmacol. 2010;30(3):306–311. doi: 10.1097/JCP.0b013e3181da5300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amsterdam JD, Luo L, Shults J. Effectiveness and mood conversion rate of short-term fluoxetine monotherapy in patients with rapid cycling bipolar II depression versus patients with nonrapid cycling bipolar II depression. J Clin Psychopharmacol. 2013;33(3):420–424. doi: 10.1097/JCP.0b013e31828ea89e. [DOI] [PubMed] [Google Scholar]
- 10.Perlis RH, Uher R, Ostacher M, et al. Association between bipolar spectrum features and treatment outcomes in outpatients with major depressive disorder. Arch Gen Psychiatry. 2011;68(4):351–360. doi: 10.1001/archgenpsychiatry.2010.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Woo YS, Chae JH, Jun TY, Kim KS, Bahk WM. The bipolar diathesis of treatment-resistant major depressive disorder. Int J Psychiatry Clin Pract. 2008;12(2):142–146. doi: 10.1080/13651500701749867. [DOI] [PubMed] [Google Scholar]
- 12.Li CT, Bai YM, Huang YL, et al. Association between antidepressant resistance in unipolar depression and subsequent bipolar disorder: cohort study. Br J Psychiatry. 2012;200(1):45–51. doi: 10.1192/bjp.bp.110.086983. [DOI] [PubMed] [Google Scholar]
- 13.Dudek D, Siwek M, Zielinska D, Jaeschke R, Rybakowski J. Diagnostic conversions from major depressive disorder into bipolar disorder in an outpatient setting: results of a retrospective chart review. J Affect Disord. 2013;144(1–2):112–115. doi: 10.1016/j.jad.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 14.Maalouf FT, Porta G, Vitiello B, et al. Do sub-syndromal manic symptoms influence outcome in treatment resistant depression in adolescents? A latent class analysis from the TORDIA study. J Affect Disord. 2012;138(1–2):86–95. doi: 10.1016/j.jad.2011.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Donovan C, Garnham JS, Hajek T, Alda M. Antidepressant monotherapy in pre-bipolar depression; predictive value and inherent risk. J Affect Disord. 2008;107(1–3):293–298. doi: 10.1016/j.jad.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 16.Frankland A, Cerrillo E, Hadzi-Pavlovic D, et al. Comparing the phenomenology of depressive episodes in bipolar I and II disorder and major depressive disorder within bipolar disorder pedigrees. J Clin Psychiatry. 2015;76(1):32–38. doi: 10.4088/JCP.14m09293. quiz 39. [DOI] [PubMed] [Google Scholar]
- 17.Ghaemi SN, Ko JY, Goodwin FK. “Cade’s disease” and beyond: misdiagnosis, antidepressant use, and a proposed definition for bipolar spectrum disorder. Can J Psychiatry. 2002;47(2):125–134. doi: 10.1177/070674370204700202. [DOI] [PubMed] [Google Scholar]
- 18.Sidor MM, MacQueen GM. An update on antidepressant use in bipolar depression. Curr Psychiatry Rep. 2012;14(6):696–704. doi: 10.1007/s11920-012-0323-6. [DOI] [PubMed] [Google Scholar]
- 19.Pacchiarotti I, Valenti M, Colom F, et al. Differential outcome of bipolar patients receiving antidepressant monotherapy versus combination with an antimanic drug. J Affect Disord. 2011;129(1–3):321–326. doi: 10.1016/j.jad.2010.07.036. [DOI] [PubMed] [Google Scholar]
- 20.Bond DJ, Noronha MM, Kauer-Sant’Anna M, Lam RW, Yatham LN. Antidepressant-associated mood elevations in bipolar II disorder compared with bipolar I disorder and major depressive disorder: a systematic review and meta-analysis. J Clin Psychiatry. 2008;69(10):1589–1601. doi: 10.4088/jcp.v69n1009. [DOI] [PubMed] [Google Scholar]
- 21.Nolen WA. The continuum of unipolar depression – bipolar II depression – bipolar I depression: different treatments indicated? World Psychiatry. 2011;10(3):196–197. doi: 10.1002/j.2051-5545.2011.tb00054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zimmerman M. Would broadening the diagnostic criteria for bipolar disorder do more harm than good? Implications from longitudinal studies of subthreshold conditions. J Clin Psychiatry. 2012;73(4):437–443. doi: 10.4088/JCP.11com07288. [DOI] [PubMed] [Google Scholar]


