Abstract
Pneumonia caused by Mycoplasma pneumoniae (M. pneumoniae pneumonia) is a major cause of community-acquired pneumonia worldwide. The surveillance of M. pneumoniae pneumonia is important for etiological and epidemiological studies of acute respiratory infections. In Japan, nation-wide surveillance of M. pneumoniae pneumonia has been conducted as a part of the National Epidemiological Surveillance of Infectious Diseases (NESID) program. This surveillance started in 1981, and significant increases in the numbers of M. pneumoniae pneumonia patients were noted in 1984, 1988, 2006, 2010, 2011, 2012, and 2015. The epidemics in 2011 and 2012 were particularly widespread and motivated researchers to conduct detailed epidemiological studies, including genotyping and drug resistance analyses of M. pneumoniae isolates. The genotyping studies based on the p1 gene sequence suggested that the p1 gene type 1 lineage has been dominant in Japan since 2003, including the epidemic period during 2011–2012. However, more detailed p1 typing analysis is required to determine whether the type 2 lineages become more relevant after the dominance of the type 1 lineage. There has been extensive research interest in implications of the p1 gene types on the epidemiology of M. pneumoniae infections. Serological characterizations of sera from patients have provided a glimpse into these associations, showing the presence of type specific antibody in the patient sera. Another important epidemiological issue of M. pneumoniae pneumonia is the emergence of macrolide-resistant M. pneumoniae (MRMP). MRMPs were noted among clinical isolates in Japan after 2000. At present, the isolation rate of MRMPs from pediatric patients is estimated at 50–90% in Japan, depending on the specific location. In view of the situation, Japanese societies have issued guiding principles for treating M. pneumoniae pneumonia. In these guiding principles, macrolides are still recommended as the first-line drug, however, if the fever does not subside in 48–72 h from first-line drug administration, a change of antibiotics to second-line drugs is recommended.
Keywords: Mycoplasma pneumoniae, community-acquired pneumonia, infectious diseases surveillance, periodic epidemics, P1 cytadhesin, P1 typing, hemadsorption, macrolide resistance
Surveillance of M. pneumoniae Pneumonia in Japan
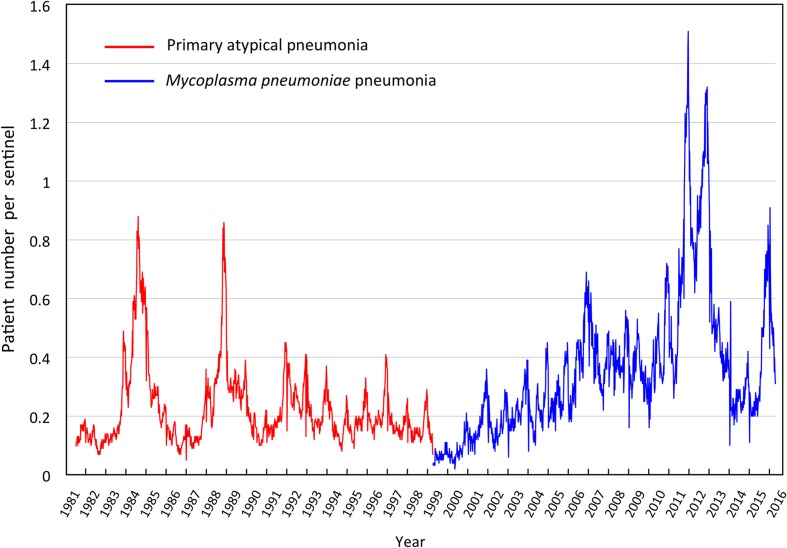
In Japan, the National Epidemiological Surveillance of Infectious Diseases (NESID) program is conducted under the Infectious Diseases Control Law (Law Concerning the Prevention of Infectious Diseases and Medical Care for Patients of Infections), which includes nationwide surveillance of pneumonia cases caused by Mycoplasma pneumoniae. M. pneumoniae pneumonia is classified as a category V infectious disease in the NESID, and the numbers of affected patients (total of outpatients and inpatients) are reported weekly from sentinel hospitals. Approximately 500 hospitals across Japan that have departments of pediatrics and internal medicine and more than 300 beds are currently selected as the sentinels for surveillance of M. pneumoniae pneumonia in Japan. For notification of each new M. pneumoniae pneumonia patient, confirmation is required using one of the tests listed in Table 1 in addition to clinical symptoms observed by a clinician. Previously, culture isolation of M. pneumoniae and detection of serum antibodies against M. pneumoniae were employed as the tests for notification. However, detection of M. pneumoniae genomic DNA by polymerase chain reaction (PCR) or loop-mediated isothermal amplification (LAMP) and detection of M. pneumoniae antigens by immuno-chromatographic methods have been recently included in the tests for notification1. The data from sentinels are integrated at the Infectious Disease Surveillance Center (IDSC), National Institute of Infectious Diseases (NIID) and published weekly2. Since the NESID program was initiated in July 1981, the surveillance of primary atypical pneumonia (PAP) was continuously performed until March 1999. The criteria of PAP include pneumonia other than M. pneumoniae pneumonia, such as that caused by Chlamydophila pneumoniae, Legionella pneumophila, or several viruses. However, as the major cause of PAP is M. pneumoniae, this surveillance largely represented the general trend of mycoplasma epidemics. As of April 1999, M. pneumoniae pneumonia-specific surveillance was initiated by NESID under the revised Infectious Diseases Control Law. Figure 1 shows the most recent M. pneumoniae pneumonia surveillance data collected by the NESID. In the early period of data collection, there were large increases of PAP patients observed in 1984 and 1988. Before the NESID surveillance was started in Japan, an extensive epidemiological study of M. pneumoniae pneumonia in school children was performed in the 1960s and 1970s in Sendai city (Niitu, 1984). In this study, an increase of M. pneumoniae pneumonia patients was observed every 4 years (i.e., 1964, 1968, 1972, and 1976), suggesting periodicity in the epidemics of this disease. Epidemics observed by the NESID in 1984 and 1988 (Figure 1) are compatible with this 4-year periodicity pattern observed in Sendai city. Given that these 4-year-cycle epidemics occurred in Olympic years, M. pneumoniae pneumonia has often been referred to as “Olympic disease” in Japan. However, after this period, 4-year-cycle epidemics were no longer observed in the NESID surveillance, although slight increases in the number of patients were observed in 1992 and 1996. The reason for disappearance of periodic epidemic is unknown, however, it is noteworthy that clarithromycin has been introduced for treatment of PAP since 1991. After 2000, M. pneumoniae pneumonia epidemics were observed in 2006, 2010, 2011, and 2012. The epidemics in 2011 and 2012 were particularly widespread and attracted public attention. Although the reason for these large epidemics in 2011 and 2012 is unknown, large increases in the numbers of M. pneumoniae pneumonia patients were also reported in Europe and other countries during this period (Chalker et al., 2011; Blystad et al., 2012; Nir-Paz et al., 2012; Pereyre et al., 2013; Kim et al., 2015). After these large epidemics in 2011 and 2012, the number of M. pneumoniae pneumonia patients decreased rapidly, and was quite low in 2014. However, the number of patients increased again since the summer of 2015 and reached a higher level during the winter (Figures 1 and 2). An increase of patient number was also reported in China in 2015 (Yan et al., 2016).
Table 1.
Tests required for notification of Mycoplasma pneumoniae pneumonia from sentinel clinics.
| Test (Method) | Specimen |
|---|---|
| Isolation of M. pneumoniae (Culture method) | Specimens derived from the patient’s respiratory tract |
| Detection of M. pneumoniae antigen (Immuno-chromatographic method)a | |
| Detection of M. pneumoniae DNA (PCR, LAMP, etc.)b | |
| Detection of antibody (serological diagnosis) | Serum |
aFour commercial immuno-chromatographic diagnosis kits for M. pneumoniae have been approved and used in Japan since 2013: Prime check MycoplasmaTM (Alfresa Parma), Ribotest MycoplasmaTM (Asahi Kasei), Prorast MycoTM (LSI Medience), and Immuno Ace MycoplasmaTM (Tauns Laboratories). The detection targets of these four kits are P1 adhesin, ribosomal L7/L12, DnaK and P30 proteins, respectively. bGenomic DNA detection tests have been introduced to the surveillance since 2011.
FIGURE 1.
Weekly cases of primary atypical pneumonia (from April 1981 to March 1999, red line) and Mycoplasma pneumoniae pneumonia (from April 1999 to present, blue line) in Japan reported by The National Epidemiological Surveillance of Infectious Diseases (NESID).
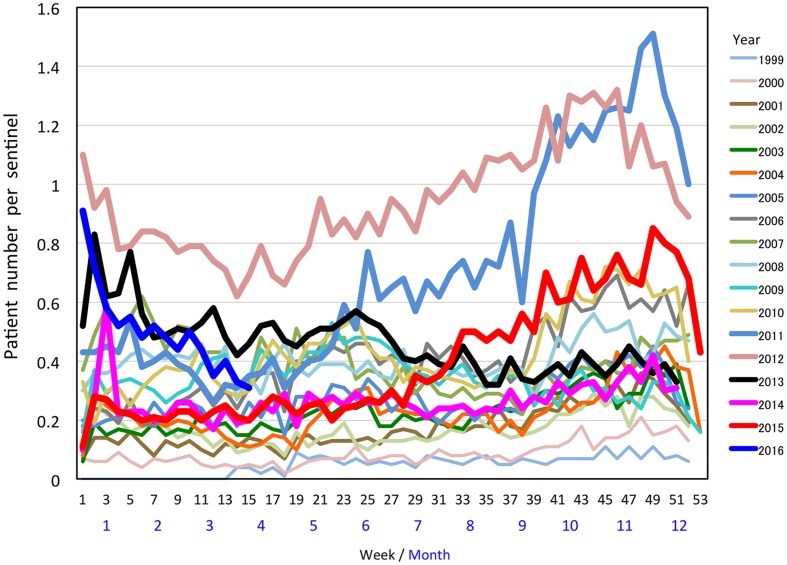
FIGURE 2.
Weekly cases of M. pneumoniae pneumonia in Japan between 1999 and 2015 reported by the NESID. http://www.nih.go.jp/niid/ja/10/2096-weeklygraph/1659-18myco.html.
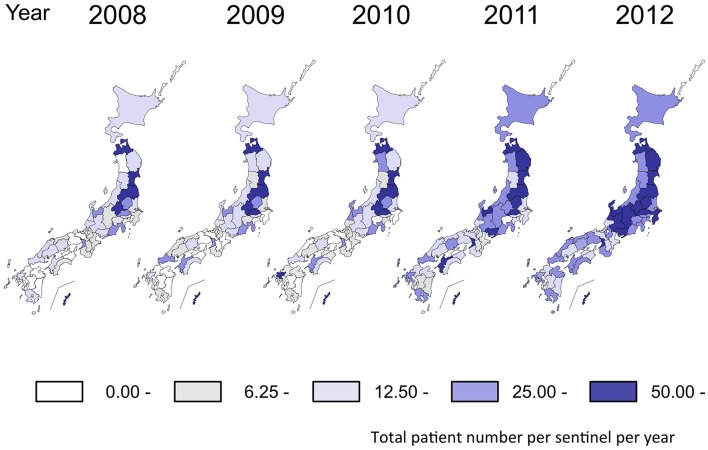
Such period occurrences of M. pneumoniae pneumonia epidemics in 3–7-year intervals has been observed in surveillances of M. pneumoniae pneumonia in many areas of the world (Lind and Bentzon, 1976; Foy et al., 1979; Lind et al., 1997; Rastawicki et al., 1998; Ito et al., 2001; Eun et al., 2008; Chalker et al., 2011; Blystad et al., 2012; Youn and Lee, 2012; Kim et al., 2015). This phenomenon is considered to be one of the characteristic features of this disease. One potential reason for the pattern of periodic epidemics of M. pneumoniae pneumonia may be related to interactions between the pathogen and the immunological status of the human population (Fernald and Clyde, 1970; Mogabgab et al., 1975; Hayatsu et al., 1981; Leith et al., 1983; Barile et al., 1994). Once M. pneumoniae pneumonia epidemics occur, protective immunity may arise in the human population. However, this protective immunity may not last long, and the next generation will be dominated by younger individuals who had not been exposed, and thus do not have the protective immunity. In this situation, M. pneumoniae become active and may cause the next epidemic. A mathematical model of this process was recently reported (Omori et al., 2015). There are also reports of weather factors that might affect M. pneumoniae infections (Onozuka et al., 2009; Onozuka and Chaves, 2014). Examination of the NESID data from a seasonal perspective shows that the number of M. pneumoniae pneumonia patients generally increases in autumn and winter every year. However, depending on the year, small increases are sometimes also observed in early summer (Figure 2). From a regional view, the number of patients varies according to prefectures in Japan. In the 2011 and 2012 epidemic period, the numbers of patients increased in most of the prefectures compared to those in previous years (Figure 3). Approximately 80% of M. pneumoniae pneumonia patients in Japan are in the 1–14-year-old age group, although M. pneumoniae pneumonia occurs in all age groups.
FIGURE 3.
Incidence of M. pneumoniae pneumonia in Japan by prefecture reported by the NESID. The ranges of the number of cases in each prefecture (annual cases per sentinel) are shown in different colors. The figure is adapted from Infectious Agents Surveillance Report (IASR), 33 (10), 2012. http://www.nih.go.jp/niid/en/iasr-vol33-e/865-iasr/2738-tpc392.html.
The national surveillance of M. pneumoniae pneumonia in the NESID program is based on reports from sentinel hospitals, and is thus not a survey of the total number of patients with this disease. Since the sentinels are large hospitals, information of M. pneumoniae pneumonia patients who are diagnosed and treated in small outpatient clinics is not included in the NESID data. The NESID also does not provide molecular epidemiological data or drug resistance information of M. pneumoniae clinical isolates. Although these issues need to be addressed, the weekly surveillance data provided by the NESID is nevertheless useful and functions as an alert for public health workers, medical institutions, and researchers. The NESID data allow for researchers to conduct detailed epidemiological studies to grasp the actual situation of M. pneumoniae infections, including molecular epidemiological and drug resistance aspects of this infectious disease, especially when the signs of epidemics are observed in the surveillance data.
Molecular Epidemiology
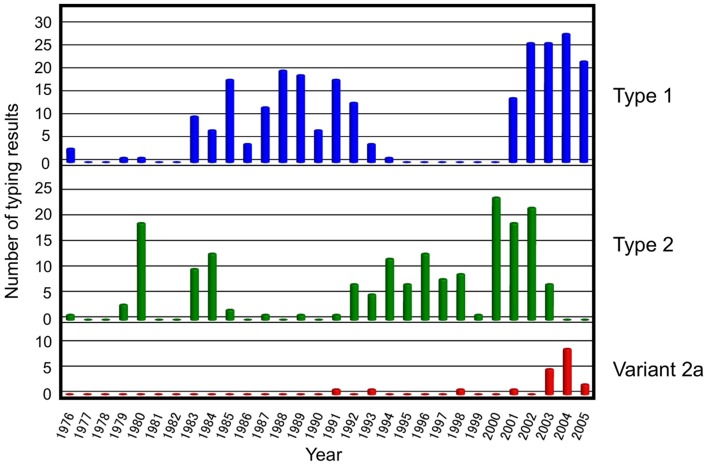
In general, M. pneumoniae clinical isolates can be classified into two distinct genetic lineages (type 1 and 2 lineages) based on their genomic background (Simmons et al., 2013; Brown et al., 2015; Lluch-Senar et al., 2015; Touati et al., 2015; Xiao et al., 2015). The p1 gene, which encodes the major cytadhesin P1 protein, exhibits sequence polymorphism between the type 1 and 2 lineages (Su et al., 1990; Kenri et al., 1999; Spuesens et al., 2010; Zhao et al., 2011; Dumke et al., 2015). The p1 types were also referred as the p1 subtypes or groups in previous studies. A number of typing analyses of M. pneumoniae isolates based on p1 gene polymorphism have been reported to date (Jacobs et al., 1996; Sasaki et al., 1996; Cousin-Allery et al., 2000; Kenri et al., 2008; Dumke et al., 2010b; Liu et al., 2010; Martinez et al., 2010). In our previous study, we genotyped M. pneumoniae isolated mainly in Kanagawa prefecture, Japan, and found that the rate of p1 types 1 and 2 detection was not constant but rather varied year by year (Figure 4) (Sasaki et al., 1996; Kenri et al., 2008). In brief, type 2 was dominant in the early 1980s, 1990s, and at the beginning of the 2000s, while type 1 was dominant in the late 1980s and after 2003. This study demonstrated an alternative type-shift phenomenon of M. pneumoniae p1 types with intervals of about 10 years. The time dependency of the rate of types 1 and 2 of the p1 gene on the study period has also been observed in isolates from other parts of the world; however, no reports have shown a clear type-shift pattern similar to that observed in Kanagawa prefecture (Cousin-Allery et al., 2000; Pereyre et al., 2007; Martinez et al., 2010; Spuesens et al., 2012; Diaz et al., 2015; Kogoj et al., 2015). In typing analyses of isolates in Germany, the rate of types 1 and 2 detection was found to be relatively constant during the research period of about 10 years including the epidemics in 2011–2013 (Dumke et al., 2010b, 2015; Jacobs et al., 2015). The relationship between M. pneumoniae pneumonia epidemics and two type lineages of M. pneumoniae remains unclear (Jacobs et al., 1996, 2015; Kenri et al., 2008).
FIGURE 4.
Typing analysis of the M. pneumoniae p1 gene from isolates detected in Japan between 1976 and 2005. The majority of M. pneumoniae strains and clinical specimens included in this analysis were collected in the Kanagawa prefecture. Figure adapted from Kenri et al. (2008).
According to several p1 typing studies, the dominant M. pneumoniae in Japan has been considered to be type 1 strains since 2003 (Fujii et al., 2012; Horino, 2012; Ohya et al., 2012; Ishiguro et al., 2015; Kubota et al., 2015; Suzuki et al., 2015). Apparent p1 type shift of M. pneumoniae clinical strains was not observed during the large epidemic period in 2011 and 2012. For example, 126 M. pneumoniae strains were isolated at the Kanagawa Prefectural Institute of Public Health between 2003 and 2011. Of these, 101 (80%) were type 1, 7 (6%) were type 2, and 18 (14%) were type 2 variants (Ohya et al., 2012). At the Yamagata Prefectural Institute of Public Health, 358 isolates were genotyped between 2004 and 2013. Of these, 278 (77.7%) were type 1, 10 (2.8%) were variant 2a, 5 (1.4%) were variant 2b, and 65 (18.2%) were variant 2c. No type 2 strain was detected in Yamagata. In the case of Yamagata, type 1 accounted for 85–100% of the annual isolates recorded between 2004 and 2011. However, the isolation rate of type 1 reduced to 73.5% (83/113) and 33.9% (21/62) in 2012 and 2013, respectively. The proportion of variant 2c isolates increased in 2012 and 2013, as a counterpart of type 1 (Suzuki et al., 2015). At this point, it is not clear whether this is the sign of p1 type change in this area. Although type 1 is considered to be dominant across a wide area of Japan at present, there is a report of a local area where type 2 is prevalent (Ishiguro et al., 2015). Most of type 2 lineage strains isolated in Japan in recent years are variants 2a and 2c while variant 2b and type 2 strains are rare. Type 2 was frequently found among the clinical isolates before 2000 (Figure 4), but type 2 was replaced by its variants (2a and 2c) almost completely during the last decade. The dominance of type 1 was also reported in recent clinical isolates in China and France (Liu et al., 2010; Wang et al., 2012; Pereyre et al., 2013; Tian et al., 2013; Zhao et al., 2013a; Xiao et al., 2014; Xue et al., 2014; Zhou et al., 2015). The results of a recent study conducted in Beijing, China indicate an increasing trend of type 2 lineage (Zhao et al., 2015), although it is not yet clear whether the type-shift phenomenon from type 1 to 2 is occurring. Further p1 typing analysis is needed to explore whether type 2 lineage strains might become prevalent in the future in areas where type 1 are currently dominant.
Multilocus variable-number tandem-repeat analysis (MLVA)-based typing is a newly developed strategy for molecular epidemiological analyses of M. pneumoniae (Degrange et al., 2009; Chalker et al., 2015). Several reports demonstrated that Japanese clinical isolates can be also separated into multiple MLVA types as same as the clinical strains isolated in the other areas (Degrange et al., 2009; Kubota et al., 2015; Touati et al., 2015). However, more MLVA typing studies are needed to discuss the characteristic profiles of Japanese strains in terms of this typing method.
Serological Characterization of M. pneumoniae Pneumonia Patient Sera Against Type 1 and 2 P1 Proteins
P1 cytadhesin is one of the major antigens of M. pneumoniae that induce antibody production. Indeed, the anti-P1 antibody is frequently detected in the sera of M. pneumoniae pneumonia patients (Hirschberg et al., 1991; Razin and Jacobs, 1992; Rastawicki et al., 1996; Tuuminen et al., 2001). Since the P1 protein exhibits amino acid sequence polymorphism between the type 1 and 2 lineages, there was a possibility that P1 proteins of types 1 and 2 have different immunogenicity and induce specific antibodies during infection. In support of this idea, there are reports of the production of a monoclonal antibody that specifically recognizes type 1 P1 protein (Gerstenecker and Jacobs, 1990; Jacobs et al., 1996), and induction of type-specific immunity was achieved with P1 fragment antigens in guinea pigs (Dumke et al., 2008). To obtain more evidence for specific immunological responses to the two P1 types, we engineered and produced three recombinant P1 protein fragments, shown in Figure 5A. The amino acid sequences of the rP1-N1 and rP1-N2 regions are derived from P1 protein of the strains M129 (type 1) and FH (type 2), respectively (Kenri et al., 2006a,b). These regions exhibit the highest differences between type 1 and 2 P1 proteins, whereas the amino acid sequence of rP1-8 region is identical between type 1 and 2 P1 proteins. Using these three P1 fragments as antigens, we performed a western blotting analysis of the sera of nine M. pneumoniae pneumonia patients to detect anti-P1 IgG (Figure 5B). The patient sera chosen for this western blot were those that exhibited high antibody titers in the serological diagnosis for M. pneumoniae pneumonia (see Table 2). Furthermore, p1 genes were detected from sputum samples of the same patients and were genotyped by PCR (Figure 5B and Table 2). This information indicates the most probable type of M. pneumoniae that infected the patients. The western blot result is shown in Figure 5B. All of the patient sera exhibited similar reactivity against the rP1-8 fragment, whereas the reactivity against rP1-N1 and rP1-N2 varied depending on the serum sample (Figure 5B). The sera from patients whose sputa were type 1 p1-positive in PCR showed stronger reactivity against rP1-N1 (Figure 5B, lanes 1–4, 8, and 10). On the other hand, the sera from patients with type 2 p1-positive sputa exhibited stronger reactivity against rP1-N2 (Figure 5B, lanes 5, 6, and 9) except for one serum (Figure 5B, lane 7). One of the serum samples from a healthy subject, used as a negative control, also showed weak reactivity against rP1-8 and rP1-N2 (Figure 5B, lane 11). This individual most likely had a previous, and perhaps unnoticed, infection with type 2 M. pneumoniae. These results demonstrated that induction of type-specific anti-P1 antibodies occurs in humans during M. pneumoniae infection (Kenri et al., 2006a,b).
FIGURE 5.
Western blotting of the sera from M. pneumoniae pneumonia patients against recombinant P1 antigens. (A) Schematic illustration of the P1 protein structure. P1 is a 170-kDa membrane protein consisting of about 1,630 amino acids (aa) depending on the strains. The first 59 aa of this protein (hatched box) is a leader peptide, which is removed during maturation. The two gray boxes indicate polymorphic regions of P1 protein that exhibit amino acid sequence variation between type 1 and 2 strains. RepMP4 and RepMP2/3 indicate repetitive regions of the p1 gene. Multiple copies of DNA sequences similar to the RepMP4 and RepMP2/3 regions are present throughout the M. pneumoniae genome. The three filled boxes indicate the positions of recombinant P1 protein fragments produced in E. coli. The rP1-N1 region corresponds to aa 218 to 352 of the P1 protein of M129 strain (type 1). The rP1-N2 region corresponds to aa 218 to 357 of the P1 protein of FH strain (type 2). The rP1-8 region corresponds to aa 1160 to 1518 of M129 P1 (Kenri et al., 2006b). (B) Western blotting of patient sera against rP1-N1, rP1-N2, and rP1-8 recombinant proteins. Purified rP1-N1, rP1-N2, and rP1-8 proteins were separated by 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis and were blotted on a nitrocellulose membrane. Diluted (100-fold) serum samples from nine patients and two healthy subjects were reacted with the membrane. IgGs bound to the membrane were detected by alkaline phosphatase-conjugated anti-human IgG secondary antibody. The positions of recombinant P1 protein fragments are shown on the left. Lane M: Coomassie Brilliant Blue stain of the blotted membrane; lanes 1–10: patient sera (serum samples of lanes 5 and 9 were obtained from the same patient in an interval of 1 week); lanes 11 and 12: serum from healthy subjects. Types of p1 genes detected by the nested PCR method (Kenri et al., 2008) from the sputum of same patient are shown on the bottom. The analyses of serum and sputum samples were performed as a part of previous studies (Yamazaki et al., 2006; Kenri et al., 2008).
Table 2.
Hemadsorption inhibitory activity of patient and non-patient sera.
| Serum No.a | Antibody titerb | p1 gene types detected from patient sputac | Hemadsorption (HA) inhibitory activityd |
|||
|---|---|---|---|---|---|---|
| M129 (Type 1) |
FH (Type 2) |
|||||
| 1/5 | 1/10 | 1/5 | 1/10 | |||
| 1 | 1280 | 1 | + | ± | – | – |
| 2 | 2560 | 1 | + | ± | ± | – |
| 3 | 1280 | 1 | + | + | + | ± |
| 4 | >2560 | 1 | + | + | – | – |
| 5 | >2560 | 2 | ± | – | + | ± |
| 6 | >2560 | 2 | ± | – | + | ± |
| 7 | 1280 | 2 | ± | – | ± | – |
| 8 | >2560 | 1 | + | + | – | – |
| 9 | 1280 | 2 | ± | – | + | ± |
| 10 | >2560 | 1 | + | – | – | – |
| 11 | ND | NT | – | – | – | – |
| 12 | ND | NT | – | – | – | – |
aSerum number corresponds to the lane number of Figure 5B. bAntibody titer was measured with Serodia Myco II kit (Fujirebio, Tokyo, Japan); ND, not determined. cDetection and typing of the p1 gene was performed by the nested PCR method as a part of previous study (Kenri et al., 2008); NT, not tested. dFive to ten colonies of M. pneumoniae M129 (type 1) or FH (type 2) strains were formed on PPLO agar cast in a 24-well microplate (1.5 ml PPLO agar per well). Colony-forming wells were soaked with 1 ml of phosphate-buffered saline (PBS) for 5 min at room temperature. After removal of PBS, 0.1 ml of diluted patient serum (fivefold or 10-fold dilution by PBS) was added to the well and incubated for 20 min at 37°C. After removal of the patient serum, 0.5 ml of a diluted sheep red blood cell (RBC) suspension (100-fold dilution by PBS) was added to the well and incubated for 20 min at 37°C. After incubation, excess RBCs were removed by washing with 1 ml of PBS three times. The state of hemadsorption of M. pneumoniae colonies was evaluated by microscopic observation. +: complete hemadsorption inhibition (no adsorption of RBCs was observed); ±: partial inhibition (partial adsorption of RBCs was observed); –: no inhibition (colonies were fully covered by RBCs; Kenri et al., 2006b).
Hemadsorption (HA) Inhibitory Activity of M. pneumoniae Pneumonia Patient Sera
It has been reported that M. pneumoniae pneumonia patient sera exhibit inhibitory activity toward the adsorption of red blood cells to M. pneumoniae colonies [i.e., hemadsorption (HA) inhibitory activity; Hirschberg et al., 1991; Razin and Jacobs, 1992; Rastawicki et al., 1996; Tuuminen et al., 2001; Schurwanz et al., 2009]. Thus, we examined the HA inhibitory activity of the patient sera analyzed by western blotting in Figure 5B, and the results are shown in Table 2. The sera from type 1-infected patients (No. 1–4, 8, and 10) tended to show stronger HA inhibitory activity against M129 strain (type 1). On the other hand, the sera from type 2-infected patients (No. 5, 6, and 9) exhibited stronger HA inhibitory activity against FH strain (type 2) compared to M129. This result indicated that M. pneumoniae pneumonia patient sera with a high antibody titer possessed type-specific HA inhibitory activities (Kenri et al., 2006a,b). Indeed, some anti-P1 antibodies have been reported to show HA inhibitory activity (Krause and Baseman, 1983; Jacobs et al., 1989; Gerstenecker and Jacobs, 1990); however, it is not clear whether the type-specific anti-P1 antibodies detected in the western blotting in Figure 5B play a role in determining the type-specific HA inhibitory activity. It is possible that antibodies against another type-specific antigen are responsible for the observed type-specific HA inhibitory activity. If these type-specific HA inhibitory activities of patient sera serve as protective immunity for M. pneumoniae infection, this might explain the type shift phenomenon of M. pneumoniae isolates.
Emergence of Macrolide-Resistant M. pneumoniae (MRMP)
It has been known at least since the 1970s that M. pneumoniae can acquire resistance against macrolides relatively easily in laboratory culture (Niitu et al., 1970; Nitu et al., 1974; Lucier et al., 1995; Pereyre et al., 2004). There are also some early reports of MRMP clinical isolates (Stopler et al., 1980; Clara et al., 1989). However, MRMPs rapidly and broadly spread after 2000, especially in eastern Asian countries such as China, Korea, and Japan (Okazaki et al., 2001; Matsuoka et al., 2004; Morozumi et al., 2005, 2008; Cao et al., 2010; Bebear et al., 2011; Hong et al., 2013; Zhao et al., 2013b, 2014). The frequencies of MRMP detection are now increasing in other areas of the world (Pereyre et al., 2007; Li et al., 2009; Peuchant et al., 2009; Dumke et al., 2010a; Averbuch et al., 2011; Chironna et al., 2011; Yamada et al., 2012; Eshaghi et al., 2013; Tsai et al., 2013; Wu et al., 2013; Caballero Jde et al., 2014; Saraya et al., 2014; Diaz et al., 2015; Zheng et al., 2015). MRMPs are isolated more frequently from adolescent and pediatric patients than from adults, which is likely related to the frequent use of macrolides for treatments of mycoplasmal infections at younger ages. However, isolation of MRMPs from adult patients is also on the rise (Isozumi et al., 2009; Miyashita et al., 2012; Yoo et al., 2012; Hanada et al., 2014; Zhou et al., 2015). Most of the MRMPs isolated in Japan carry the A2063G mutation in domain V of the 23S rRNA gene that confers strong resistance to 14- and 15-membered macrolides and lincosamides. However, there is a report of a local outbreak caused by MRMPs carrying the A2063T mutation, which exhibits only moderate resistance to macrolides (Suzuki et al., 2013). The most recent estimate of the isolation rate of MRMPs from adolescent and pediatric patients in Japan is 50–90%, depending on the area (Morozumi et al., 2008; Akaike et al., 2012; Miyashita et al., 2012; Kawai et al., 2013b; Ishiguro et al., 2015). Given this situation, the Japan Pediatric Society3 and The Japanese Society for Mycoplasmology4 have issued guiding principles for treating M. pneumoniae pneumonia (The committee on the guiding principle for treatment of Mycoplasma pneumoniae pneumonia, 2014).
Therapeutic Strategies for M. pneumoniae Pneumonia
Mycoplasma pneumoniae is generally susceptible to macrolides, tetracyclines, and the new quinolone antibiotics. However, as stated above, the emergence of MRMP since 2000 has made the treatment of M. pneumoniae pneumonia challenging. Although MRMP strains have been reported in European countries and in the United States, the detection rates from these countries are lower than those in East Asia, including Japan. Caution in monitoring and treating MRMP strains and the necessity of continuous surveillance for these strains are partially described in the guidelines of the Infectious Diseases Society of America (IDSA), American Thoracic Society (ATS; Mandell et al., 2007), European Respiratory Society, European Society for Clinical Microbiology and Infectious Diseases for adults (Woodhead et al., 2011), and in the Pediatric Infectious Diseases Society (PIDS) and IDSA for children (Bradley et al., 2011). However, the necessity and strategies of alternative antibiotic treatment for MRMP strains have not been described in detail. The detection rates of MRNPs are associated with age (Miyashita et al., 2013): detection rates are higher in children aged ≤15 years than in adults. In addition, the detection rates among adults are higher in adolescents aged 16–19 years than in those aged ≥20 years.
The guidelines of the IDSA and ATS recommend macrolides or tetracyclines as the first-line drugs for M. pneumoniae pneumonia, and fluoroquinolones as the second-line drugs in adults. The guidelines of the PIDS and IDSA for children recommend azithromycin as the first-line oral drug, and clarithromycin, erythromycin, or doxycycline (for patients aged ≥8 years) along with levofloxacin or moxifloxacin (for adolescent patients) as the second-line oral drugs, for mild cases. For treatment via injection, azithromycin is recommended as the first-line drug (although this is not indicated for children in Japan), and erythromycin and levofloxacin (also not indicated for children in Japan) are recommended as the second-line drugs.
Thus, the applicability of antibiotics differs between adults and children; in addition, the indication for antibiotics for children is different between Japan and other countries. In view of these points, the therapeutic guiding principles3,4 for M. pneumoniae pneumonia issued in Japan are reviewed in the following sections.
Treatment in Adults: Recommendations by the Japanese Society of Mycoplasmology
The first-line drugs for M. pneumoniae pneumonia in adults are macrolide antibiotics. Oral administration of clarithromycin (400 mg/day administered in two divided doses) or erythromycin (800–1,200 mg/day administered in 4–6 divided doses for 7–10 days) is recommended for patients on an outpatient basis. Oral azithromycin administered at 500 mg once a day for 3 days or at 2 g once a day for 1 day is also indicated (Table 3). The minimum inhibitory concentration (MIC) values of macrolides for M. pneumoniae without macrolide resistance genes are extremely low, while those of fluoroquinolones and tetracyclines are higher (Akaike et al., 2012). Minocycline, levofloxacin, garenoxacin, moxifloxacin, sitafloxacin, and tosufloxacin are recommended as second-line drugs (Table 3). Intravenous administration is indicated for inpatients: minocycline, azithromycin, and erythromycin are recommended as first-line drugs, and levofloxacin, ciprofloxacin, and pazufloxacin are recommended as the second-line drugs (Table 4).
Table 3.
Recommended treatments for adult outpatients of M. pneumoniae pneumonia.
| Drug | Route of administration | mg/dose | Dose/day | |
|---|---|---|---|---|
| First-line drug | Clarithromycin (CAM) | Oral | 200 | 2 |
| Azithromycin (AZM) (Slow-release formulation) | Oral | 2000 | 1 (1 day) | |
| Azithromycin (AZM) | Oral | 500 | 1 (3 days) | |
| Erythromycin (EM) | Oral | 200 | 4–6 | |
| Second-line drug | Minocycline (MINO) | Oral | 100 | 2 |
| Levofloxacin (LVFX) | Oral | 500 | 1 | |
| Garenoxacin (GRNX) | Oral | 400 | 1 | |
| Moxifloxacin (MFLX) | Oral | 400 | 1 | |
| Sitafloxacin (STFX) | Oral | 100 | 2 | |
| Oral | 200 | 1 | ||
| Tosufloxacin (TFLX) | Oral | 150 | 2–3 |
The table is adapted from the guiding principle (Chiryo–Shishin) issued by the Japanese Society of Mycoplasmology (JSM). http://square.umin.ac.jp/jsm/shisin.pdf.
Table 4.
Recommended treatments for adult inpatients of M. pneumoniae pneumonia.
| Drug | Route of administration | mg/dose | Dose/day | |
|---|---|---|---|---|
| First-line drug | Minocycline (MINO) | Intravenous (drip infusion) | 100 | 2 |
| Azithromycin (AZM) | Intravenous (drip infusion) | 500 | 1 | |
| Erythromycin (EM) | Intravenous (drip infusion) | 300–500 | 2–3 | |
| Second-line drug | Levofloxacin (LVFX) | Intravenous (drip infusion) | 500 | 1 |
| Ciprofloxacin (CPFX) | Intravenous (drip infusion) | 300 | 2 | |
| Pazufloxacin (PZFX) | Intravenous (drip infusion) | 500–1000 | 2 |
The table is adapted from the guiding principle of JSM (http://square.umin.ac.jp/jsm/shisin.pdf).
There is concern surrounding the emergence of quinolone resistance in Streptococcus pneumoniae and other respiratory pathogenic bacteria owing to the use of quinolones as the initial treatment for pneumonia. Quinolones have been shown capable of inducing resistance in M. pneumoniae strains in vitro (Gruson et al., 2005). Therefore, quinolones should be avoided during the initial treatment in young patients with suspected M. pneumoniae pneumonia. M. pneumoniae pneumonia is less common in the elderly than in the younger generation. Quinolones are prescribed for elderly patients with pneumonia, because microorganisms other than M. pneumoniae are typically involved. On the other hand, tetracyclines are not likely to induce resistance in M. pneumoniae. Intravenous administration of tetracycline is recommended as the first-line treatment for hospitalized patients (Table 4). Although there is no sufficient evidence regarding the duration of antibiotic administration for the treatment of M. pneumoniae pneumonia in adults, the Japanese Society of Mycoplasmology recommends a duration of 7–10 days.
When the fever does not subside within 48–72 h after the administration of macrolides, the antibiotics should be changed considering the possibility of MRMP involvement. At present, MRMP is susceptible to both tetracyclines and fluoroquinolones. A study of the treatment for infection with MRMP in children demonstrated that minocycline showed a higher rate of bacterial elimination than tosufloxacin, and the fever subsided faster upon treatment with minocycline than with tosufloxacin (Kawai et al., 2013a).
Considering the emergence of quinolone resistance, the first-line drug recommended for MRMP pneumonia is minocycline (Table 5). Oral minocycline administered at 200 mg/day in two divided doses on an outpatient basis, and intravenous minocycline administered at 100 mg twice a day for inpatients is recommended. Quinolones are recommended as second-line drugs for both outpatients and inpatients (Tables 5 and 6). For outpatient treatment, levofloxacin, garenoxacin, moxifloxacin, sitafloxacin, or tosufloxacin is orally administered (Tables 3 and 5). For inpatient treatment, levofloxacin, ciprofloxacin, or pazufloxacin is intravenously administered (Tables 4 and 6). The duration of antibiotic treatment is 7–10 days, similar to that for infection with macrolide-sensitive M. pneumoniae.
Table 5.
Recommended treatments for adult outpatients of macrolide-resistant M. pneumoniae pneumonia.
| Drug | Route of administration | mg/dose | Dose/day | |
|---|---|---|---|---|
| First-line drug | Minocycline (MINO) | Oral | 100 | 2 |
| Second-line drug | Levofloxacin (LVFX) | Oral | 500 | 1 |
| Garenoxacin (GRNX) | Oral | 400 | 1 | |
| Moxifloxacin (MFLX) | Oral | 400 | 1 | |
| Sitafloxacin (STFX) | Oral | 100 | 2 | |
| 200 | 1 | |||
| Tosufloxacin (TFLX) | Oral | 150 | 2–3 |
The table is adapted from the guiding principle of JSM (http://square.umin.ac.jp/jsm/shisin.pdf).
Table 6.
Recommended treatments for adult inpatients of macrolide-resistant M. pneumoniae pneumonia.
| Drug | Route of administration | mg/dose | Dose/day | |
|---|---|---|---|---|
| First-line drug | Minocycline (MINO) | Intravenous (drip infusion) | 100 | 2 |
| Second-line drug | Levofloxacin (LVFX) | Intravenous (drip infusion) | 500 | 1 |
| Ciprofloxacin (CPFX) | Intravenous (drip infusion) | 300 | 2 | |
| Pazufloxacin (PZFX) | Intravenous (drip infusion) | 500–1000 | 2 |
The table is adapted from the guiding principle of JSM (http://square.umin.ac.jp/jsm/shisin.pdf).
In severe cases of M. pneumoniae pneumonia involving respiratory failure, methylprednisolone is administered at 500–1,000 mg/day for 3–5 days concomitantly with an appropriate antimycoplasmal drug. It should be noted that the relationship between MRMP and severe M. pneumoniae infection remains unclear.
Treatment in Children: Recommendations by the Japanese Society of Pediatric Pulmonology, Japanese Society for Pediatric Infectious Diseases, Japan Pediatric Society, and Japanese Society of Mycoplasmology
Macrolides are also recommended as the first-line drugs for M. pneumoniae pneumonia in children. The incidence of MRMP isolates from pediatric cases varies both regionally and epidemically in Japan, ranging from <50% in patients without a history of macrolide treatment to >90% in patients that were treated by macrolides without clinical effectiveness. The MIC values of macrolides for macrolide-sensitive M. pneumoniae are extremely low, and the rates of bacterial elimination are high. The MIC values of tetracyclines and tosufloxacin for macrolide-sensitive M. pneumoniae are relatively higher than those of macrolides. In addition, M. pneumoniae may not be eliminated after treatment with these drugs. Tosufloxacin is the only fluoroquinolone approved for children in Japan (Table 7).
Table 7.
Recommended treatments for pediatric patients of M. pneumoniae pneumonia.
| Drug | Route of administration | Drug dose (mg/kg/day) | Divided dose/day | Treatment period (days) |
|---|---|---|---|---|
| Erythromycin (EM) | Oral | 25–50 | 4–6 | 14 |
| Clarithromycin (CAM) | Oral | 10–15 | 2–3 | 10 |
| Azithromycin (AZM) | Oral | 10 | 1 | 3 |
| Tosufloxacin (TFLX) | Oral | 12 | 2 | 7–14 |
| Minocycline (MINO) | Oral or intravenous drip infusion | 2–4 | 2 | 7–14 |
The table is adapted from the guiding principle of JSM (http://square.umin.ac.jp/jsm/shisin.pdf).
In children with pneumonia caused by macrolide-sensitive M. pneumoniae, treatment with macrolides has been shown to alleviate the fever within 48 h in more than 80% of cases. On the other hand, fever persists in approximately 70% of children with MRMP infection. These data indicate that the clinical effectiveness of macrolides should be evaluated on the basis of the presence of fever at 48–72 h after treatment. Persistent fever suggests the possibility of infection with macrolide-resistant strains or mixed infection with microorganisms other than M. pneumoniae. For cases of M. pneumoniae pneumonia with failure of macrolide treatment, either tosufloxacin or tetracyclines are applicable. Quinolones might induce drug resistance in the microflora other than M. pneumoniae, and should be administered with caution. Tetracyclines may cause side effects such as transient anostosis, staining of the teeth, and enamel hypoplasia. Tetracyclines are contraindicated in children aged under 8 years. The recommended duration of treatment for M. pneumoniae pneumonia caused by macrolide-sensitive strains is 14 days with erythromycin, 10 days with clarithromycin, and 3 days with azithromycin. Treatment with tosufloxacin or tetracyclines for pneumonia caused by MRMPs should be administered for 7–14 days. Systemic administration of steroids for severe pneumonia should be considered; however, the indications of systemic steroid use are not yet determined. One study showed that steroid therapy is effective in patients with fever lasting >7 days, with a serum lactate dehydrogenase level of ≥480 IU/L (Oishi et al., 2011).
Conclusion
The nationwide surveillance of M. pneumoniae pneumonia in Japan is based on reports collected from approximately 500 sentinel hospitals, and is thus not reflective of the total number of patients. However, this weekly monitoring can detect previous epidemics and patterns, and has played a significant role as an alert system for medical and public health workers as well as researchers. Therefore, the effort for this surveillance program should be continued.
There are two distinct genetic lineages of M. pneumoniae that exhibit polymorphism in the cytadhesin P1 protein sequence. However, the involvements of these two lineages in pneumonia epidemics and differences in their pathogenicity are not yet fully understood. Nevertheless, cytadhesin P1 is an important factor that plays a critical role in the infection mechanism of this pathogen and in the interactions with host cells. We believe that p1 gene typing is an important aspect for molecular epidemiological studies of M. pneumoniae and should be performed by combining modern genotyping methods based on MLVA, multi-locus sequence typing, and/or whole-genome SNP strategies.
Emergence of MRMP is serious problem for the treatment of M. pneumoniae pneumonia. Given this situation, several Japanese academic and medical societies have issued specific guiding principles for treatment of M. pneumoniae pneumonia. Macrolides are still recommended as the first-line drug in children and adults. However, if the fever does not subside in 48–72 h from first-line drug administration, a change of antibiotics to second-line drugs (i.e., fluoroquinolones and tetracyclines) is recommended.
Author Contributions
TY wrote the therapeutic strategy section of the paper. TK wrote the surveillance and epidemiology sections of the paper.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors are grateful to Dr. Mitsuo Narita of Sapporo Tokushukai Hospital for reading the manuscript and helpful suggestions.
Funding. This work was supported by a grant (H26-Kokui-Shitei-001) from the Ministry of Health, Labor, and Welfare of Japan and a Grant-in Aid for Scientific Research on Innovative Areas (grant 25117530 and 15H01337) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan.
References
- Akaike H., Miyashita N., Kubo M., Kawai Y., Tanaka T., Ogita S., et al. (2012). In vitro activities of 11 antimicrobial agents against macrolide-resistant Mycoplasma pneumoniae isolates from pediatric patients: results from a multicenter surveillance study. Jpn. J. Infect. Dis. 65 535–538. 10.7883/yoken.65.535 [DOI] [PubMed] [Google Scholar]
- Averbuch D., Hidalgo-Grass C., Moses A. E., Engelhard D., Nir-Paz R. (2011). Macrolide resistance in Mycoplasma pneumoniae, Israel, 2010. Emerg. Infect. Dis. 17 1079–1082. 10.3201/eid/1706.101558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barile M. F., Grabowski M. W., Kapatais-Zoumbois K., Brown B., Hu P. C., Chandler D. K. (1994). Protection of immunized and previously infected chimpanzees challenged with Mycoplasma pneumoniae. Vaccine 12 707–714. 10.1016/0264-410X(94)90220-8 [DOI] [PubMed] [Google Scholar]
- Bebear C., Pereyre S., Peuchant O. (2011). Mycoplasma pneumoniae: susceptibility and resistance to antibiotics. Future Microbiol. 6 423–431. 10.2217/fmb.11.18 [DOI] [PubMed] [Google Scholar]
- Blystad H., Anestad G., Vestrheim D. F., Madsen S., Ronning K. (2012). Increased incidence of Mycoplasma pneumoniae infection in Norway 2011. Euro. Surveill. 17:20074. [DOI] [PubMed] [Google Scholar]
- Bradley J. S., Byington C. L., Shah S. S., Alverson B., Carter E. R., Harrison C., et al. (2011). The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin. Infect. Dis. 53 e25–e76. 10.1093/cid/cir531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R. J., Holden M. T., Spiller O. B., Chalker V. J. (2015). Development of a multilocus sequence typing scheme for molecular typing of Mycoplasma pneumoniae. J. Clin. Microbiol. 53 3195–3203. 10.1128/JCM.01301-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caballero Jde D., del Campo R., Mafe Mdel C., Galvez M., Rodriguez-Dominguez M., Canton R., et al. (2014). First report of macrolide resistance in a Mycoplasma pneumoniae isolate causing community-acquired pneumonia in Spain. Antimicrob. Agents Chemother. 58 1265–1266. 10.1128/AAC.02325-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao B., Zhao C. J., Yin Y. D., Zhao F., Song S. F., Bai L., et al. (2010). High prevalence of macrolide resistance in Mycoplasma pneumoniae isolates from adult and adolescent patients with respiratory tract infection in China. Clin. Infect. Dis, 51 189–194. 10.1086/653535 [DOI] [PubMed] [Google Scholar]
- Chalker V., Stocki T., Mentasti M., Fleming D., Harrison T. (2011). Increased incidence of Mycoplasma pneumoniae infection in England and Wales in 2010: multiocus variable number tandem repeat analysis typing and macrolide susceptibility. Euro. Surveill, 16:19865. [PubMed] [Google Scholar]
- Chalker V. J., Pereyre S., Dumke R., Winchell J., Khosla P., Sun H., et al. (2015). International Mycoplasma pneumoniae typing study: interpretation of M. pneumoniae multilocus variable-number tandem-repeat analysis. New Microbes New Infect. 7 37–40. 10.1016/j.nmni.2015.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chironna M., Sallustio A., Esposito S., Perulli M., Chinellato I., Di Bari C., et al. (2011). Emergence of macrolide-resistant strains during an outbreak of Mycoplasma pneumoniae infections in children. J. Antimicrob. Chemother. 66 734–737. 10.1093/jac/dkr003 [DOI] [PubMed] [Google Scholar]
- Clara F., Von Busch C., Goeddertz P., Novotna I. (1989). Resistance of Mycoplasma pneumoniae to erythromycin: a clinical case with severe pulmonary, cerebral and systemic complications. J. Chemother. 1 411–413. [PubMed] [Google Scholar]
- Cousin-Allery A., Charron A., de Barbeyrac B., Fremy G., Skov Jensen J., Renaudin H., et al. (2000). Molecular typing of Mycoplasma pneumoniae strains by PCR-based methods and pulsed-field gel electrophoresis. Application to French and Danish isolates. Epidemiol. Infect. 124 103–111. 10.1017/S0950268899003313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degrange S., Cazanave C., Charron A., Renaudin H., Bebear C., Bebear C. M. (2009). Development of multiple-locus variable-number tandem-repeat analysis for molecular typing of Mycoplasma pneumoniae. J. Clin. Microbiol. 47 914–923. 10.1128/JCM.01935-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz M. H., Benitez A. J., Winchell J. M. (2015). Investigations of Mycoplasma pneumoniae infections in the United States: trends in molecular typing and macrolide resistance from 2006 to 2013. J. Clin. Microbiol. 53 124–130. 10.1128/JCM.02597-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumke R., Schnee C., Pletz M. W., Rupp J., Jacobs E., Sachse K., et al. (2015). Mycoplasma pneumoniae and Chlamydia spp. infection in community-acquired pneumonia, Germany, 2011-2012. Emerg. Infect. Dis. 21 426–434. 10.3201/eid2103.140927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumke R., Schurwanz N., Jacobs E. (2008). Characterisation of subtype- and variant-specific antigen regions of the P1 adhesin of Mycoplasma pneumoniae. Int. J. Med. Microbiol. 298 483–491. 10.1016/j.ijmm.2007.06.002 [DOI] [PubMed] [Google Scholar]
- Dumke R., von Baum H., Luck P. C., Jacobs E. (2010a). Occurrence of macrolide-resistant Mycoplasma pneumoniae strains in Germany. Clin. Microbiol. Infect. 16 613–616. 10.1111/j.1469-0691.2009.02968.x [DOI] [PubMed] [Google Scholar]
- Dumke R., Von Baum H., Luck P. C., Jacobs E. (2010b). Subtypes and variants of Mycoplasma pneumoniae: local and temporal changes in Germany 2003-2006 and absence of a correlation between the genotype in the respiratory tract and the occurrence of genotype-specific antibodies in the sera of infected patients. Epidemiol. Infect. 138 1829–1837. 10.1017/S0950268810000622 [DOI] [PubMed] [Google Scholar]
- Eshaghi A., Memari N., Tang P., Olsha R., Farrell D. J., Low D. E., et al. (2013). Macrolide-resistant Mycoplasma pneumoniae in humans, Ontario, Canada, 2010-2011. Emerg. Infect. Dis 19 1525–1527. 10.3201/eid1909.121466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eun B. W., Kim N. H., Choi E. H., Lee H. J. (2008). Mycoplasma pneumoniae in Korean children: the epidemiology of pneumonia over an 18-year period. J. Infect. 56 326–331. 10.1016/j.jinf.2008.02.018 [DOI] [PubMed] [Google Scholar]
- Fernald G. W., Clyde W. A. (1970). Protective effect of vaccines in experimental Mycoplasma pneumoniae disease. Infect. Immun. 1 559–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foy H. M., Kenny G. E., Cooney M. K., Allan I. D. (1979). Long-term epidemiology of infections with Mycoplasma pneumoniae. J. Infect. Dis. 139 681–687. 10.1093/infdis/139.6.681 [DOI] [PubMed] [Google Scholar]
- Fujii H., Omori A., Nakagawa N., Hatsimoto T., KAgeoka T., Nakajima H., et al. (2012). Macrolide resistance rate and minimum inhibitory concentration of Mycoplasma pneumoniae clinical strains isolated in Kurashiki Central Hospital between 2008 and 2012. Infect. Dis. Surveil. Rep. (IASR) 33 265–266. [Google Scholar]
- Gerstenecker B., Jacobs E. (1990). Topological mapping of the P1-adhesin of Mycoplasma pneumoniae with adherence-inhibiting monoclonal antibodies. J. Gen. Microbiol. 136 471–476. 10.1099/00221287-136-3-471 [DOI] [PubMed] [Google Scholar]
- Gruson D., Pereyre S., Renaudin H., Charron A., Bebear C., Bebear C. M. (2005). In vitro development of resistance to six and four fluoroquinolones in Mycoplasma pneumoniae and Mycoplasma hominis, respectively. Antimicrob. Agents Chemother. 49 1190–1193. 10.1128/AAC.49.3.1190-1193.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanada S., Morozumi M., Takahashi Y., Mochizuki S., Sato T., Suzuki S., et al. (2014). Community-acquired pneumonia caused by macrolide-resistant Mycoplasma pneumoniae in adults. Intern. Med. 53 1675–1678. 10.2169/internalmedicine.53.1418 [DOI] [PubMed] [Google Scholar]
- Hayatsu E., Kawakubo Y., Yayoshi M., Araake M., Wakai M., Yoshida A., et al. (1981). Immunological responses of hamsters in the acquired immune state to Mycoplasma pneumoniae infection. Microbiol. Immunol. 25 1255–1263. 10.1111/j.1348-0421.1981.tb00135.x [DOI] [PubMed] [Google Scholar]
- Hirschberg L., Holme T., Krook A. (1991). Human antibody response to the major adhesin of Mycoplasma pneumoniae: increase in titers against synthetic peptides in patients with pneumonia. APMIS 99 515–520. 10.1111/j.1699-0463.1991.tb05184.x [DOI] [PubMed] [Google Scholar]
- Hong K. B., Choi E. H., Lee H. J., Lee S. Y., Cho E. Y., Choi J. H., et al. (2013). Macrolide resistance of Mycoplasma pneumoniae, South Korea, 2000-2011. Emerg. Infect. Dis. 19 1281–1284. 10.3201/eid1908.121455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horino A. (2012). The epidemic of Mycoplasma pneumonia in 2011 season. Jpn. J. Mycoplasmol. 39 71–74. [Google Scholar]
- Ishiguro N., Koseki N., Kaiho M., Kikuta H., Togashi T., Oba K., et al. (2015). Regional differences in rates of macrolide-resistant Mycoplasma pneumoniae in Hokkaido, Japan. Jpn. J. Infect. Dis. 10.7883/yoken.JJID.2015.054 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Isozumi R., Yoshimine H., Morozumi M., Ubukata K., Ariyoshi K. (2009). Adult community-acquired pneumonia caused by macrolide resistant Mycoplasma pneumoniae. Respirology 14 1206–1208. 10.1111/j.1440-1843.2009.01619.x [DOI] [PubMed] [Google Scholar]
- Ito I., Ishida T., Osawa M., Arita M., Hashimoto T., Hongo T., et al. (2001). Culturally verified Mycoplasma pneumoniae pneumonia in Japan: a long-term observation from 1979-99. Epidemiol. Infect. 127 365–367. 10.1017/S0950268801005982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs E., Ehrhardt I., Dumke R. (2015). New insights in the outbreak pattern of Mycoplasma pneumoniae. Int. J. Med. Microbiol. 305 705–708. 10.1016/j.ijmm.2015.08.021 [DOI] [PubMed] [Google Scholar]
- Jacobs E., Gerstenecker B., Mader B., Huang C. H., Hu P. C., Halter R., et al. (1989). Binding sites of attachment-inhibiting monoclonal antibodies and antibodies from patients on peptide fragments of the Mycoplasma pneumoniae adhesin. Infect. Immun. 57 685–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs E., Vonski M., Oberle K., Opitz O., Pietsch K. (1996). Are outbreaks and sporadic respiratory infections by Mycoplasma pneumoniae due to two distinct subtypes? Eur. J. Clin. Microbiol. Infect. Dis. 15 38–44. 10.1007/BF01586183 [DOI] [PubMed] [Google Scholar]
- Kawai Y., Miyashita N., Kubo M., Akaikea H., Katoa A., Nishizawaa Y., et al. (2013a). Therapeutic efficacy of macrolides, minocycline, and tosufloxacin against macrolide-resistant Mycoplasma pneumoniae pneumonia in pediatric patients. Antimicrob. Agents Chemother. 57 2252–2258. 10.1128/AAC.00048-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawai Y., Miyashita N., Kubo M., Akaike H., Kato A., Nishizawa Y., et al. (2013b). Nationwide surveillance of macrolide-resistant Mycoplasma pneumoniae infection in pediatric patients. Antimicrob. Agents Chemother. 57 4046–4049. 10.1128/AAC.00663-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenri T., Okazaki N., Yamazaki T., Narita M., Izumikawa K., Matsuoka M., et al. (2008). Genotyping analysis of Mycoplasma pneumoniae clinical strains in Japan between 1995 and 2005: type shift phenomenon of M. pneumoniae clinical strains. J. Med. Microbiol. 57 469–475. 10.1099/jmm.0.47634-0 [DOI] [PubMed] [Google Scholar]
- Kenri T., Taniguchi R., Sasaki Y., Okazaki N., Narita M., Izumikawa K., et al. (1999). Identification of a new variable sequence in the P1 cytadhesin gene of Mycoplasma pneumoniae: evidence for the generation of antigenic variation by DNA recombination between repetitive sequences. Infect. Immun. 67 4557–4562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenri T., Yamazaki T., Okazaki N., Narita M., Arakawa Y., Sasaki T. (2006a). “Differential hemadsorption inhibitory activity of sera from patients infected with two Mycoplasma pneumoniae groups,” in Proceedings of the abstract book of 16th International Congress of International Organization for Mycoplasmology (IOM). Abstract no. 120, Jul 9-14, Cambridge. [Google Scholar]
- Kenri T., Yamazaki T., Okazaki N., Narita M., Sasaki T. (2006b). Patient sera of M. pneumoniae infections exhibit differential hemadsorption inhibitory activity against two Mycoplasma pneumoniae groups. Jpn. J. Mycoplasmol. 39 10–12. [Google Scholar]
- Kim E. K., Youn Y. S., Rhim J. W., Shin M. S., Kang J. H., Lee K. Y. (2015). Epidemiological comparison of three Mycoplasma pneumoniae pneumonia epidemics in a single hospital over 10 years. Korean J. Pediatr. 58 172–177. 10.3345/kjp.2015.58.5.172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogoj R., Mrvic T., Praprotnik M., Kese D. (2015). Prevalence, genotyping and macrolide resistance of Mycoplasma pneumoniae among isolates of patients with respiratory tract infections, Central Slovenia, 2006 to 2014. Euro. Surveill. 20:3 10.2807/1560-7917.ES.2015.20.37.30018 [DOI] [PubMed] [Google Scholar]
- Krause D. C., Baseman J. B. (1983). Inhibition of Mycoplasma pneumoniae hemadsorption and adherence to respiratory epithelium by antibodies to a membrane protein. Infect. Immun. 39 1180–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubota H., Okuno R., Hatakeyama K., Uchitani Y., Sadamasu K., Hirai A., et al. (2015). Molecular typing of Mycoplasma pneumoniae isolated from pediatric patients in Tokyo, Japan. Jpn. J. Infect. Dis. 68 76–78. 10.7883/yoken.JJID.2014.336 [DOI] [PubMed] [Google Scholar]
- Leith D. K., Hansen E. J., Wilson R. M., Krause D. C., Baseman J. B. (1983). Hemadsorption and virulence are separable properties of Mycoplasma pneumoniae. Infect. Immun. 39 844–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Atkinson T. P., Hagood J., Makris C., Duffy L. B., Waites K. B. (2009). Emerging macrolide resistance in Mycoplasma pneumoniae in children: detection and characterization of resistant isolates. Pediatr. Infect. Dis. J. 28 693–696. 10.1097/INF.0b013e31819e3f7a [DOI] [PubMed] [Google Scholar]
- Lind K., Bentzon M. W. (1976). Epidemics of Mycoplasma pneumoniae infection in Denmark from 1958 to 1974. Int. J. Epidemiol. 5 267–277. 10.1093/ije/5.3.267 [DOI] [PubMed] [Google Scholar]
- Lind K., Benzon M. W., Jensen J. S., Clyde W. A., Jr. (1997). A seroepidemiological study of Mycoplasma pneumoniae infections in Denmark over the 50-year period 1946-1995. Eur. J. Epidemiol. 13 581–586. 10.1023/A:1007353121693 [DOI] [PubMed] [Google Scholar]
- Liu Y., Ye X., Zhang H., Xu X., Li W., Zhu D., et al. (2010). Characterization of macrolide resistance in Mycoplasma pneumoniae isolated from children in Shanghai, China. Diagn. Microbiol. Infect. Dis. 67 355–358. 10.1016/j.diagmicrobio.2010.03.004 [DOI] [PubMed] [Google Scholar]
- Lluch-Senar M., Cozzuto L., Cano J., Delgado J., Llorens-Rico V., Pereyre S., et al. (2015). Comparative “-omics” in Mycoplasma pneumoniae clinical isolates reveals key virulence factors. PLoS ONE 10:e0137354 10.1371/journal.pone.0137354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucier T. S., Heitzman K., Liu S. K., Hu P. C. (1995). Transition mutations in the 23S rRNA of erythromycin-resistant isolates of Mycoplasma pneumoniae. Antimicrob. Agents Chemother. 39 2770–2773. 10.1128/AAC.39.12.2770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell L. A., Wunderink R. G., Anzueto A., Bartlett J. G., Campbell G. D., Dean N. C., et al. (2007). Infectious diseases society of america/american thoracic society consensus guidelines on the management of community-acquired pneumonia in adults. Clin. Infect. Dis. 44(Suppl. 2), S27–S72. 10.1086/511159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez M. A., Ruiz M., Zunino E., Luchsinger V., Aguirre R., Avendano L. F. (2010). Identification of P1 types and variants of Mycoplasma pneumoniae during an epidemic in Chile. J. Med. Microbiol. 59 925–929. 10.1099/jmm.0.018333-0 [DOI] [PubMed] [Google Scholar]
- Matsuoka M., Narita M., Okazaki N., Ohya H., Yamazaki T., Ouchi K., et al. (2004). Characterization and molecular analysis of macrolide-resistant Mycoplasma pneumoniae clinical isolates obtained in Japan. Antimicrob. Agents Chemother. 48 4624–4630. 10.1128/AAC.48.12.4624-4630.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyashita N., Akaike H., Teranishi H., Ouchi K., Okimoto N. (2013). Macrolide-resistant Mycoplasma pneumoniae pneumonia in adolescents and adults: clinical findings, drug susceptibility, and therapeutic efficacy. Antimicrob. Agents Chemother. 57 5181–5185. 10.1128/AAC.00737-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyashita N., Kawai Y., Akaike H., Ouchi K., Hayashi T., Kurihara T., et al. (2012). Macrolide-resistant Mycoplasma pneumoniae in adolescents with community-acquired pneumonia. BMC Infect. Dis. 12:126 10.1186/1471-2334-12-126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogabgab W. J., Marchand S., Mills G., Beville R. (1975). Efficacy of inactivated Mycoplasma pneumoniae vaccine in man. Dev. Biol. Stand. 28 597–608. [PubMed] [Google Scholar]
- Morozumi M., Hasegawa K., Kobayashi R., Inoue N., Iwata S., Kuroki H., et al. (2005). Emergence of macrolide-resistant Mycoplasma pneumoniae with a 23S rRNA gene mutation. Antimicrob. Agents Chemother. 49 2302–2306. 10.1128/AAC.49.6.2302-2306.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morozumi M., Iwata S., Hasegawa K., Chiba N., Takayanagi R., Matsubara K., et al. (2008). Increased macrolide resistance of Mycoplasma pneumoniae in pediatric patients with community-acquired pneumonia. Antimicrob. Agents Chemother 52 348–350. 10.1128/AAC.00779-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niitu Y. (1984). Mycoplasma pneumoniae Infections. Acta Paediatr. Jpn. 27 73–90. 10.1111/j.1442-200X.1985.tb00619.x [DOI] [PubMed] [Google Scholar]
- Niitu Y., Hasegawa S., Suetake T., Kubota H., Komatsu S., Horikawa M. (1970). Resistance of Mycoplasma pneumoniae to erythromycin and other antibiotics. J. Pediatr. 76 438–443. 10.1016/S0022-3476(70)80485-1 [DOI] [PubMed] [Google Scholar]
- Nir-Paz R., Abutbul A., Moses A. E., Block C., Hidalgo-Grass C. (2012). Ongoing epidemic of Mycoplasma pneumoniae infection in Jerusalem, Israel, 2010 to 2012. Euro. Surveill. 17:20095. [PubMed] [Google Scholar]
- Nitu Y., Hasegawa S., Kubota H. (1974). In vitro development of resistance to erythromycin, other macrolide antibiotics, and lincomycin in Mycoplasma pneumoniae. Antimicrob. Agents Chemother. 5 513–519. 10.1128/AAC.5.5.513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohya H., Oda Y., Furukawa I., Takahashi C., Narita M. (2012). Isolation of macrolide-resistant Mycoplasma pneumoniae in 2011. Jpn. J. Mycoplasmol. 39 75–79. [Google Scholar]
- Oishi T., Narita M., Matsui K., Shirai T., Matsuo M., Negishi J., et al. (2011). Clinical implications of interleukin-18 levels in pediatric patients with Mycoplasma pneumoniae pneumonia. J. Infect. Chemother. 17 803–806. 10.1007/s10156-011-0265-7 [DOI] [PubMed] [Google Scholar]
- Okazaki N., Narita M., Yamada S., Izumikawa K., Umetsu M., Kenri T. (2001). Characteristics of macrolide-resistant Mycoplasma pneumoniae strains isolated from patients and induced with erythromycin in vitro. Microbiol. Immunol. 45 617–620. 10.1111/j.1348-0421.2001.tb01293.x [DOI] [PubMed] [Google Scholar]
- Omori R., Nakata Y., Tessmer H. L., Suzuki S., Shibayama K. (2015). The determinant of periodicity in Mycoplasma pneumoniae incidence: an insight from mathematical modelling. Sci. Rep. 5:14473 10.1038/srep14473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onozuka D., Chaves L. F. (2014). Climate variability and nonstationary dynamics of Mycoplasma pneumoniae pneumonia in Japan. PLoS ONE 9:e95447 10.1371/journal.pone.0095447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onozuka D., Hashizume M., Hagihara A. (2009). Impact of weather factors on Mycoplasma pneumoniae pneumonia. Thorax 64 507–511. 10.1136/thx.2008.111237 [DOI] [PubMed] [Google Scholar]
- Pereyre S., Charron A., Renaudin H., Bebear C., Bebear C. M. (2007). First report of macrolide-resistant strains and description of a novel nucleotide sequence variation in the P1 adhesin gene in Mycoplasma pneumoniae clinical strains isolated in France over 12 years. J. Clin. Microbiol. 45 3534–3539. 10.1128/JCM.01345-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereyre S., Guyot C., Renaudin H., Charron A., Bebear C., Bebear C. M. (2004). In vitro selection and characterization of resistance to macrolides and related antibiotics in Mycoplasma pneumoniae. Antimicrob. Agents Chemother. 48 460–465. 10.1128/AAC.48.2.460-465.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereyre S., Touati A., Petitjean-Lecherbonnier J., Charron A., Vabret A., Bebear C. (2013). The increased incidence of Mycoplasma pneumoniae in France in 2011 was polyclonal, mainly involving M. pneumoniae type 1 strains. Clin. Microbiol. Infect. 19 E212–E217. 10.1111/1469-0691.12107 [DOI] [PubMed] [Google Scholar]
- Peuchant O., Menard A., Renaudin H., Morozumi M., Ubukata K., Bebear C. M., et al. (2009). Increased macrolide resistance of Mycoplasma pneumoniae in France directly detected in clinical specimens by real-time PCR and melting curve analysis. J. Antimicrob. Chemother. 64 52–58. 10.1093/jac/dkp160 [DOI] [PubMed] [Google Scholar]
- Rastawicki W., Kaluzewski S., Jagielski M. (1998). Occurrence of serologically verified Mycoplasma pneumoniae infections in Poland in 1970-1995. Eur. J. Epidemiol. 14 37–40. 10.1023/A:1007431932087 [DOI] [PubMed] [Google Scholar]
- Rastawicki W., Raty R., Kleemola M. (1996). Detection of antibodies to Mycoplasma pneumoniae adhesion P1 in serum specimens from infected and non-infected subjects by immunoblotting. Diagn. Microbiol. Infect. Dis. 26 141–143. 10.1016/S0732-8893(96)00216-7 [DOI] [PubMed] [Google Scholar]
- Razin S., Jacobs E. (1992). Mycoplasma adhesion. J. Gen. Microbiol. 138 407–422. 10.1099/00221287-138-3-407 [DOI] [PubMed] [Google Scholar]
- Saraya T., Kurai D., Nakagaki K., Sasaki Y., Niwa S., Tsukagoshi H., et al. (2014). Novel aspects on the pathogenesis of Mycoplasma pneumoniae pneumonia and therapeutic implications. Front. Microbiol. 5:410 10.3389/fmicb.2014.00410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasaki T., Kenri T., Okazaki N., Iseki M., Yamashita R., Shintani M., et al. (1996). Epidemiological study of Mycoplasma pneumoniae infections in japan based on PCR-restriction fragment length polymorphism of the P1 cytadhesin gene. J. Clin. Microbiol. 34 447–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schurwanz N., Jacobs E., Dumke R. (2009). Strategy to create chimeric proteins derived from functional adhesin regions of Mycoplasma pneumoniae for vaccine development. Infect. Immun. 77 5007–5015. 10.1128/IAI.00268-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons W. L., Daubenspeck J. M., Osborne J. D., Balish M. F., Waites K. B., Dybvig K. (2013). Type 1 and type 2 strains of Mycoplasma pneumoniae form different biofilms. Microbiology 159 737–747. 10.1099/mic.0.064782-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spuesens E. B., Hoogenboezem T., Sluijter M., Hartwig N. G., van Rossum A. M., Vink C. (2010). Macrolide resistance determination and molecular typing of Mycoplasma pneumoniae by pyrosequencing. J. Microbiol. Methods 82 214–222. 10.1016/j.mimet.2010.06.004 [DOI] [PubMed] [Google Scholar]
- Spuesens E. B., Meijer A., Bierschenk D., Hoogenboezem T., Donker G. A., Hartwig N. G., et al. (2012). Macrolide resistance determination and molecular typing of Mycoplasma pneumoniae in respiratory specimens collected between 1997 and 2008 in The Netherlands. J. Clin. Microbiol. 50 1999–2004. 10.1128/JCM.00400-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stopler T., Gerichter C. B., Branski D. (1980). Antibiotic-resistant mutants of Mycoplasma pneumoniae. Isr J. Med. Sci. 16 169–173. [PubMed] [Google Scholar]
- Su C. J., Chavoya A., Dallo S. F., Baseman J. B. (1990). Sequence divergency of the cytadhesin gene of Mycoplasma pneumoniae. Infect. Immun. 58 2669–2674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki Y., Itagaki T., Seto J., Kaneko A., Abiko C., Mizuta K., et al. (2013). Community outbreak of macrolide-resistant Mycoplasma pneumoniae in Yamagata, Japan in 2009. Pediatr. Infect. Dis. J. 32 237–240. 10.1097/INF.0b013e31827aa7bd [DOI] [PubMed] [Google Scholar]
- Suzuki Y., Seto J., Itagaki T., Aoki T., Abiko C., Matsuzaki Y. (2015). Gene mutations ssociated with macrolide-resistance and p1 gene typing of Mycoplasma pneumoniae isolated in yamagata, japan, between 2004 and 2013. Kansenshogaku Zasshi 89 16–22. [DOI] [PubMed] [Google Scholar]
- The committee on the guiding principle for treatment of Mycoplasma pneumoniae pneumonia (2014). The Guiding Principle for Treatment of Mycoplasma Pneumoniae pneumonia (Chryo-Shishin for Mycoplasma Pneumoniae pneumonia). Hokkiado: The Japanese Society of Mycoplasmology. [Google Scholar]
- Tian X. J., Dong Y. Q., Dong X. P., Li J. Y., Li D., Jiang Y., et al. (2013). P1 gene of Mycoplasma pneumoniae in clinical isolates collected in Beijing in 2010 and relationship between genotyping and macrolide resistance. Chin. Med. J. (Engl.) 126 3944–3948. [PubMed] [Google Scholar]
- Touati A., Blouin Y., Sirand-Pugnet P., Renaudin H., Oishi T., Vergnaud G., et al. (2015). Molecular epidemiology of Mycoplasma pneumoniae: genotyping using single nucleotide polymorphisms and SNaPshot technology. J. Clin. Microbiol. 53 3182–3194. 10.1128/JCM.01156-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai V., Pritzker B. B., Diaz M. H., Winchell J. M., Hicks L. A., Petrone B., et al. (2013). Cluster of macrolide-resistant Mycoplasma pneumoniae infections in Illinois in 2012. J. Clin. Microbiol. 51 3889–3892. 10.1128/JCM.01613-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuuminen T., Suni J., Kleemola M., Jacobs E. (2001). Improved sensitivity and specificity of enzyme immunoassays with P1-adhesin enriched antigen to detect acute Mycoplasma pneumoniae infection. J. Microbiol. Methods 44 27–37. 10.1016/S0167-7012(00)00235-9 [DOI] [PubMed] [Google Scholar]
- Wang Y., Qiu S., Yang G., Song L., Su W., Xu Y., et al. (2012). An outbreak of Mycoplasma pneumoniae caused by a macrolide-resistant isolate in a nursery school in China. Antimicrob. Agents Chemother. 56 3748–3752. 10.1128/AAC.00142-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodhead M., Blasi F., Ewig S., Garau J., Huchon G., Ieven M., et al. (2011). Guidelines for the management of adult lower respiratory tract infections–summary. Clin. Microbiol. Infect. 17(Suppl. 6), 1–24. 10.1111/j.1469-0691.2011.03602.x [DOI] [PubMed] [Google Scholar]
- Wu H. M., Wong K. S., Huang Y. C., Lai S. H., Tsao K. C., Lin Y. J., et al. (2013). Macrolide-resistant Mycoplasma pneumoniae in children in Taiwan. J. Infect. Chemother. 19 782–786. 10.1007/s10156-012-0523-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao J., Liu Y., Wang M., Jiang C., You X., Zhu C. (2014). Detection of Mycoplasma pneumoniae P1 subtype variations by denaturing gradient gel electrophoresis. Diagn. Microbiol. Infect. Dis. 78 24–28. 10.1016/j.diagmicrobio.2013.08.008 [DOI] [PubMed] [Google Scholar]
- Xiao L., Ptacek T., Osborne J. D., Crabb D. M., Simmons W. L., Lefkowitz E. J., et al. (2015). Comparative genome analysis of Mycoplasma pneumoniae. BMC Genomics 16:610 10.1186/s12864-015-1801-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue G., Wang Q., Yan C., Jeoffreys N., Wang L., Li S., et al. (2014). Molecular characterizations of PCR-positive Mycoplasma pneumoniae specimens collected from Australia and China. J. Clin. Microbiol. 52 1478–1482. 10.1128/JCM.03366-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamada M., Buller R., Bledsoe S., Storch G. A. (2012). Rising rates of macrolide-resistant Mycoplasma pneumoniae in the central United States. Pediatr. Infect. Dis. J. 31 409–410. 10.1097/INF.0b013e318247f3e0 [DOI] [PubMed] [Google Scholar]
- Yamazaki T., Narita M., Sasaki N., Kenri T., Arakawa Y., Sasaki T. (2006). Comparison of PCR for sputum samples obtained by induced cough and serological tests for diagnosis of Mycoplasma pneumoniae infection in children. Clin. Vaccine Immunol. 13 708–710. 10.1128/CVI.00413-05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan C., Sun H., Zhao H. (2016). Latest surveillance data on Mycoplasma pneumoniae infections in children suggesting a new epidemic occurring in beijing. J. Clin. Microbiol. 54 1400–1401. 10.1128/JCM.00184-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo S. J., Kim H. B., Choi S. H., Lee S. O., Kim S. H., Hong S. B., et al. (2012). Differences in the frequency of 23S rRNA gene mutations in Mycoplasma pneumoniae between children and adults with community-acquired pneumonia: clinical impact of mutations conferring macrolide resistance. Antimicrob. Agents Chemother. 56 6393–6396. 10.1128/AAC.01421-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youn Y. S., Lee K. Y. (2012). Mycoplasma pneumoniae pneumonia in children. Korean J. Pediatr. 55 42–47. 10.3345/kjp.2012.55.2.42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao F., Cao B., Li J., Song S., Tao X., Yin Y., et al. (2011). Sequence analysis of the p1 adhesin gene of Mycoplasma pneumoniae in clinical isolates collected in Beijing in 2008 to 2009. J. Clin. Microbiol. 49 3000–3003. 10.1128/JCM.00105-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao F., Liu G., Cao B., Wu J., Gu Y., He L., et al. (2013a). Multiple-locus variable-number tandem-repeat analysis of 201 Mycoplasma pneumoniae isolates from Beijing, China, from 2008 to 2011. J. Clin. Microbiol. 51 636–639. 10.1128/JCM.02567-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao F., Liu G., Wu J., Cao B., Tao X., He L., et al. (2013b). Surveillance of macrolide-resistant Mycoplasma pneumoniae in beijing, china, from 2008 to 2012. Antimicrob. Agents Chemother. 57 1521–1523. 10.1128/AAC.02060-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao F., Liu L., Tao X., He L., Meng F., Zhang J. (2015). Culture-independent detection and genotyping of Mycoplasma pneumoniae in clinical specimens from beijing, China. PLoS ONE 10:e0141702 10.1371/journal.pone.0141702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H., Li S., Cao L., Yuan Y., Xue G., Feng Y., et al. (2014). Surveillance of Mycoplasma pneumoniae infection among children in Beijing from 2007 to 2012. Chin. Med. J. (Engl.) 127 1244–1248. [PubMed] [Google Scholar]
- Zheng X., Lee S., Selvarangan R., Qin X., Tang Y. W., Stiles J., et al. (2015). Macrolide-Resistant Mycoplasma pneumoniae, United States. Emerg. Infect. Dis. 21 1470–1472. 10.3201/eid2108.150273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Z., Li X., Chen X., Luo F., Pan C., Zheng X., et al. (2015). Macrolide-resistant Mycoplasma pneumoniae in adults in zhejiang, china. Antimicrob. Agents Chemother. 59 1048–1051. 10.1128/AAC.04308-14 [DOI] [PMC free article] [PubMed] [Google Scholar]