Abstract
Schwannomas are benign nerve sheath tumours arising from Schwann cells. Presacral schwannomas are rare with only case report and short case series being reported in literature. Complete surgical resection is the treatment of choice for these rare tumours. Approach to surgical resection depends on the type of the tumour. Type 3 tumours have conventionally been treated with open intra or extra peritoneal approach. With improvement in the laparoscopic surgical skills, more and more complex surgical procedures have been attempted via this approach. We are presenting a case of presacral schwannoma in an overweight lady treated by laparoscopic resection.
Keywords: Presacral schwannoma, laparoscopic surgery, minimally invasive approach
Introduction
Presacral tumours in adults are quite rare accounting for 1 of 40,000 hospital admissions (1). Neurogenic tumours in the presacral area are even rarer accounting for 10–15% of tumours arising from the presacral region (2). Although many of these are incidental findings on imaging for abdominal symptoms, some of them can present with vague lower abdominal pain as well as constipation because of the mass effect. These tumours offer significant surgical challenge because of the narrow working space available as well as abundant vascularity of the presacral plexus of vessels. Although various approaches have been documented in literature, laparoscopic resection has been considered complex with high rates of conversion to open surgery. We are presenting a case of presacral schwannoma resected via laparoscopic approach in an overweight female.
Case snippet
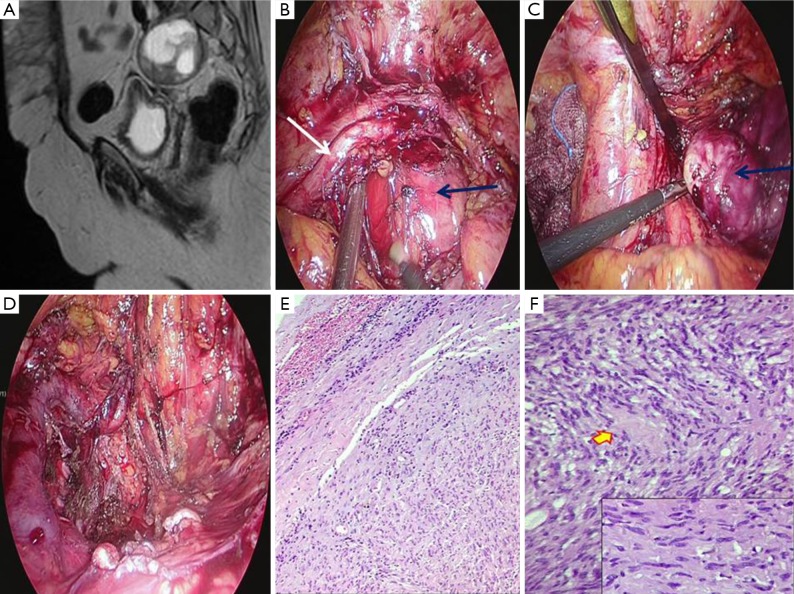
A 57-year-old lady presented with pain in the lower abdomen of 6 months duration. On evaluation with contrast enhanced computed tomography of abdomen (CECT), a lobulated soft tissue mass of size 55×68×55 mm3 was detected in the presacral area. A magnetic resonance imaging (MRI) of the pelvis confirmed it as dumb-bell shaped tumor with extension into widened left first sacral foramen representing a nerve sheath tumour (Figure 1A). As the body mass index (BMI) of the patient was 33, a laparoscopic resection was planned. Intra operatively, rectum was mobilized first and left ureter as well as the iliac vessels were demonstrated (Figure 1B). The tumor was dissected from all the surrounding structures. Resection was completed by dividing the left hypogastric nerve as well as anterior division of the first sacral nerve root (Figure 1C,D). Sacrificing both of these was essential to achieve complete resection of the tumor. Duration of the surgery was 300 minutes and there was 200 mL of blood loss. Post operative course was uneventful and she was discharged on seventh postoperative day. Histopathological examination of the resected tumor confirmed it as a benign schwannoma (Figure 1E,F). Patient has been followed up for more than a year and is asymptomatic, disease free and without any permanent neurological deficit.
Figure 1.
Figure depicting radiological, intra operative and histopathological characteristics of the presacral schwannoma. (A) Coronal MRI images showing the presacral schwannoma; (B) intra operative picture of the tumor (blue arrow—tumor; white arrow—ureter); (C) dissection of the tumor from the presacral area (blue arrow); (D) complete resection of the tumor; (E) Low magnification micropicture showing circumscribed spindle cell tumor with lymphoid cells in the capsule (Hematoxylin and Eosin staining, ×40); (F) spindle cell tumor with doubly indented wavy nuclei revealing focal palisade (marked) with no significant atypia or mitosis (magnification, ×100). Inset: higher magnification showing wavy nuclei and interspersed lymphocytes, reminiscent of a nerve sheath tumor (magnification, ×400). MRI, magnetic resonance imaging.
Discussion
Schwannomas are benign nerve sheath tumours arising from Schwann cells of the neural sheath. Fifth and eight cranial nerves near the cerebellopontine angle, brachial plexus, posterior mediastinum and spinal roots are the most common sites of origin of schwannomas (3). Presacral schwannomas account for only 1–5% of spinal schwannomas (4). In general they are more common in females than males. Klimo et al. classified these tumours into three categories: type 1 tumours are confined to the sacrum; type 2 tumours originate within the sacrum but erode the wall of the sacrum and extend into the adjacent spaces; type 3 tumours are located predominantly in the presacral or retro peritoneal area (5).
Preoperative diagnosis is difficult because of the rarity of the tumor as well as absence of any specific symptoms or signs. Because of their slow growing nature, they can reach very large size and even erode the sacrum (6). Most of these tumours remain asymptomatic till they reach size large enough to cause pressure symptoms. The tumours eroding the sacrum can present with lower abdominal or back pain. Rare cases of urinary disturbances, paresthesia and alteration of bowel habits have been reported in the literature. The present patient presented with lower abdominal pain and constipation in spite of the smaller size of the tumor.
A complete resection via open abdominal or sacral approach has been advocated as the preferable treatment for these tumours. In general type 1 tumours are resected best via posterior approach; type 3 tumours via anterior approach and type 2 require combined anterior and posterior approach (7,8). Anterior approach may be either transperitoneal or extra peritoneal. Majority of the previous reports have reported transperitoneal approach although extra peritoneal approach has also been reported by few authors (9,10). The present patient had truncal obesity and either an open transperitoneal or extra peritoneal approach would have been very challenging. Smaller size of the tumor as well as the magnified view provided by the laparoscopy aided in the complete resection as well as excellent hemostasis. To the best of our knowledge, this is the first reported case of presacral schwannoma resected laparoscopically.
After complete excision of the tumor, recurrence is rare. Up to 10–50% recurrence has been reported in literature after incomplete resections. Adjuvant treatment is not recommended even in incomplete resections or recurrences. The present patient has been followed up for more than a year and is disease free.
Conclusions
Laparoscopic resection is feasible for presacral schwannoma and leads to lower blood loss as well as faster recovery.
Acknowledgements
None.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Gupta S, Sikora SS, Gupta R, et al. Presacral neurilemoma (schwannoma)--report of a rare case. Jpn J Surg 1989;19:229-31. 10.1007/BF02471591 [DOI] [PubMed] [Google Scholar]
- 2.Santiago C, Lucha PA. Atypical presentation of a retrorectal ancient schwannoma: a case report and review of the literature. Mil Med 2008;173:814-6. 10.7205/MILMED.173.8.814 [DOI] [PubMed] [Google Scholar]
- 3.Kaplan ED, Rozen WM, Murugasu A, et al. The undifferentiated presacral mass: a nervous tumour. ANZ J Surg 2010;80:470. 10.1111/j.1445-2197.2010.05324.x [DOI] [PubMed] [Google Scholar]
- 4.Lin CM, Kao CC, Lin TC, et al. Giant presacral schwannoma mimicking malignancy in a man. Acta Chir Belg 2010;110:387-9. 10.1080/00015458.2010.11680641 [DOI] [PubMed] [Google Scholar]
- 5.Klimo P, Jr, Rao G, Schmidt RH, et al. Nerve sheath tumors involving the sacrum. Case report and classification scheme. Neurosurg Focus 2003;15:E12. 10.3171/foc.2003.15.2.12 [DOI] [PubMed] [Google Scholar]
- 6.Getachew MM, Whitman GJ, Chew FS. Retroperitoneal schwannoma. AJR Am J Roentgenol 1994;163:1356. 10.2214/ajr.163.6.7992727 [DOI] [PubMed] [Google Scholar]
- 7.Wolpert A, Beer-Gabel M, Lifschitz O, et al. The management of presacral masses in the adult. Tech Coloproctol 2002;6:43-9. 10.1007/s101510200008 [DOI] [PubMed] [Google Scholar]
- 8.Mazreku A, Karaj A, Avdia I, et al. The presentation and management of presacral tumors. Acta Chir Iugosl 2010;57:55-9. 10.2298/ACI1002055M [DOI] [PubMed] [Google Scholar]
- 9.Rousseau MA, Pascal-Mousselard H, Lazennec JY, et al. The mini-invasive anterior extra peritoneal approach to the pelvis. Eur J Surg Oncol 2005;31:924-6. 10.1016/j.ejso.2005.05.006 [DOI] [PubMed] [Google Scholar]
- 10.Senoglu M, Bulbuloglu E, Demirpolat G, et al. The anterior extraperitoneal approach to the rare presacral/ retroperitoneal schwannoma. Bratisl Lek Listy 2010;111:558-61. [PubMed] [Google Scholar]