Abstract
Purpose
The purpose of this study was to determine the association of insurance status with disease stage at presentation, treatment, and survival among the top 10 most deadly cancers using the SEER database.
Patients and Methods
A total of 473,722 patients age 18 to 64 years who were diagnosed with one of the 10 most deadly cancers in the SEER database from 2007 to 2010 were analyzed. A Cox proportional hazards model was used for multivariable analyses to assess the effect of patient and tumor characteristics on cause-specific death.
Results
Overall, patients with non-Medicaid insurance were less likely to present with distant disease (16.9%) than those with Medicaid coverage (29.1%) or without insurance coverage (34.7%; P < .001). Patients with non-Medicaid insurance were more likely to receive cancer-directed surgery and/or radiation therapy (79.6%) compared with those with Medicaid coverage (67.9%) or without insurance coverage (62.1%; P < .001). In a Cox regression that adjusted for age, race, sex, marital status, residence, percent of county below federal poverty level, site, stage, and receipt of cancer-directed surgery and/or radiation therapy, patients were more likely to die as a result of their disease if they had Medicaid coverage (hazard ratio [HR], 1.44; 95% CI, 1.41 to 1.47; P < .001) or no insurance (HR, 1.47; 95% CI, 1.42 to 1.51; P < .001) compared with non-Medicaid insurance.
Conclusion
Among patients with the 10 most deadly cancers, those with Medicaid coverage or without insurance were more likely to present with advanced disease, were less likely to receive cancer-directed surgery and/or radiation therapy, and experienced worse survival.
INTRODUCTION
It is estimated that 15.4% of the US population, representing 48 million individuals, does not have health insurance.1 The Patient Protection and Affordable Care Act (ACA)2 was signed into law in March 2010 and aims to expand access to public and private health insurance.3
Cancer is currently the second leading cause of death in the United States and is responsible for approximately one in four deaths.4 Previous studies have shown that uninsured patients with cancer are more likely to present with advanced disease,5,6 do not receive the same treatment,7–9 and display worse survival7,10–12 compared with those with insurance. However, these studies have generally been limited to certain populations with select cancers. Estimates of the impact of insurance status on the presentation, treatment, and survival of patients with cancer on a larger scale are lacking.
The SEER program of the National Cancer Institute assembles information on cancer incidence, local treatment, and survival in the United States. SEER program registries collect data on patient demographics, including primary tumor site, tumor morphology and stage at diagnosis, first course of treatment, and follow-up for survival. In addition, this past year, the SEER program released information regarding individual patient insurance status. Registries participating in the SEER program capture approximately 97% of incident cases,13 and the population residing within the areas served by SEER cancer registries is comparable to the general US population, because the catchments for the 18 SEER registries comprise approximately 28% of the US population.14
The purpose of this study was to determine the association of insurance status with disease stage at presentation, treatment, and survival among non-Medicare–age adult patients diagnosed with one of the 10 most deadly cancers using the SEER public-use database.
PATIENTS AND METHODS
Description of Study Cohort
A total of 1,069,590 patients who were diagnosed with one of the 10 most deadly cancers (ie, breast, prostate, lung, colorectal, head and neck, liver, pancreatic, ovarian, and esophageal cancers and non-Hodgkin lymphoma [NHL]) between January 1, 2007, and December 31, 2010, were identified in the public-use SEER database using SEER*Stat software (version 8.1.2).15 SEER began collecting information on insurance status in 2007. Patients were excluded if age at diagnosis was < 18 years (n = 1,786) or if they did not undergo active follow-up (ie, death certificates or autopsy results only; n = 2,103). Patients age > 64 years (n = 591,979) were excluded, because this is the age at which most patients become eligible for Medicare, and per the SEER program, designation of insurance status is unreliable for these patients. Because this data set is in the public domain, it was deemed institutional review board exempt.
Key Covariates
Patient characteristics included age, race, sex, marital status, and urban versus rural residence. Married status, as defined by the SEER database, includes common-law marriages. Urban was defined as big metropolitan, metropolitan, or urban, and rural was defined as less urban or rural, using SEER definitions. Insurance status was defined as non-Medicaid insurance (insured or insured/no specifics), Medicaid coverage (any Medicaid), or uninsured. The SEER definition for insured includes those with private insurance (managed care, health maintenance organization, or preferred-provider organization), Medicare, and coverage from the military or Veterans Affairs at the time of initial diagnosis and/or treatment. Patients with unknown insurance status were excluded from further analysis. Robustness of the multivariable Cox proportional hazards model (Statistical Analysis) was tested using sensitivity analysis by categorizing patients with unknown insurance status as all having non-Medicaid insurance, Medicaid insurance, or uninsured, with similar results. Percent below federal poverty level was obtained from linked county-level data.16 Stage was based on the American Joint Committee on Cancer staging atlas (sixth edition).17 Extent of disease was based on TNM staging and categorized as localized (no nodal or metastatic disease), regional (nodal disease), or distant (any metastatic disease). The exception was NHL, for which Ann Arbor staging was used: local (stage I), regional (stage II to III), and distant (stage IV).
Treatment Course and Outcomes
Patients who received external-beam radiation therapy (RT) and surgery were identified based on SEER variables. Receipt of RT was defined as beam radiation (SEER codes: beam radiation or combination of beam with implants or isotopes). For prostate cancer, RT receipt also included brachytherapy (SEER code: radioactive implants). Surgery was defined as definitive in nature using SEER surgical codes, excluding those who underwent biopsy only. Site-specific cancer-directed surgery and/or RT was defined as surgery (breast, colorectal, liver, ovarian, and pancreatic cancers), surgery and/or RT (esophageal, head and neck, lung, and prostate cancers), or RT (NHL). SEER does not include information on receipt of chemotherapy, which can be definitive treatment for some disease sites (eg, NHL). Cause-specific survival was defined as the time between diagnosis and death resulting from the primary cancer through December 31, 2010.
Statistical Analysis
Pearson's χ2 statistic was used to assess significance of the difference between proportions in assessment of univariable associations. Unadjusted associations between insurance groups and outcomes were displayed using Kaplan-Meier curves and compared using the log-rank test.
A multivariable logistic regression model was used to determine the association between insurance status and receipt of cancer-directed surgery and/or RT among patients with nonmetastatic disease. Patients with metastatic disease were not included in this analysis, because chemotherapy (not available in SEER) is generally the primary treatment for these patients. All sites were adjusted for age, race, sex, marital status, urban versus rural residence, and percent of county below federal poverty level. The estimated odds ratio (OR) is reported.
The Cox proportional hazards model was used for both univariable and multivariable analyses to assess the effect of patient and tumor characteristics on the end point of cause-specific death stratified by insurance status. All sites were controlled for age, race, sex, marital status, urban versus rural residence, percent of county below federal poverty level, disease stage (local, regional, or distant), and receipt of cancer-directed surgery and/or RT. In addition, breast and prostate sites were controlled for other factors: estrogen receptor and prostate-specific antigen and Gleason score, respectively. The estimated hazard ratio (HR) is reported.
A P value ≤ .05 was considered to be statistically significant. Statistical tests were based on a two-sided significance level. Data analysis was performed using STATA/IC statistical software (version 12.1; STATA, College Station, TX).
RESULTS
A total of 473,722 patients met the inclusion criteria. Patient demographics and tumor characteristics of the 473,722 eligible patients are listed in Table 1. Median follow-up was 17 months (range, 0 to 47 months). A total of 371,628 (78.4%) had non-Medicaid insurance, 55,135 (11.6%) had Medicaid coverage, 22,442 (4.7%) did not have insurance, and 24,517 (5.2%) had unknown insurance status. On univariable analysis, the following demographic factors were associated with lack of insurance: younger age, male sex, nonwhite race, being unmarried, rural residence, and higher county poverty level (all P < .001). A total of 55.6% of the uninsured were men. Although nonwhite individuals represented 32.9% of the cohort, they represented 46.3% of uninsured and 50.9% of those with Medicaid coverage (P < .001). Patients who were single represented 34.3% of the cohort, but they comprised 57.8% of the uninsured and 64.3% of those with Medicaid coverage (P < .001).
Table 1.
Patient Demographics and Clinical Characteristics
| Characteristic | All Patients |
Non-Medicaid Insurance |
Uninsured |
Medicaid Coverage |
Unknown |
P | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | No. | % | ||
| All patients | 473,722 | 100.0 | 371,628 | 78.4 | 22,442 | 4.7 | 55,135 | 11.6 | 24,517 | 5.2 | |
| Age, years | < .001 | ||||||||||
| Median | 56 | 56 | 55 | 55 | |||||||
| Range | 18-64 | 18-64 | 18-64 | 18-64 | |||||||
| 18-29 | 5,288 | 1.1 | 3,553 | 1.0 | 437 | 1.9 | 1,040 | 1.9 | 258 | 1.1 | |
| 30-39 | 20,321 | 4.3 | 15,113 | 4.1 | 1,245 | 5.5 | 3,085 | 5.6 | 878 | 3.6 | |
| 40-49 | 85,957 | 18.1 | 65,893 | 17.7 | 4,596 | 20.5 | 11,833 | 21.5 | 3,635 | 14.8 | |
| 50-59 | 213,497 | 45.1 | 167,395 | 45.0 | 10,173 | 45.3 | 24,802 | 45.0 | 11,127 | 45.4 | |
| ≥ 60 | 148,659 | 31.4 | 119,674 | 32.2 | 5,991 | 26.7 | 14,375 | 26.1 | 8,619 | 35.2 | |
| Percent of county below poverty | < .001 | ||||||||||
| < 10 | 111,857 | 23.6 | 94,353 | 25.4 | 3,643 | 16.2 | 7,343 | 13.3 | 6,518 | 26.6 | |
| 10-12.99 | 111,520 | 23.5 | 91,443 | 24.6 | 3,985 | 17.8 | 10,482 | 19.0 | 5,610 | 22.9 | |
| 13-16.49 | 141,156 | 29.8 | 107,197 | 28.8 | 7,850 | 35.0 | 19,327 | 35.1 | 6,782 | 27.7 | |
| ≥ 16.5 | 109,041 | 23.0 | 78,591 | 21.1 | 6,960 | 31.0 | 17,980 | 32.6 | 5,510 | 22.5 | |
| Unknown | 148 | 0.0 | 44 | 0.0 | 4 | 0.0 | 3 | 0.0 | 97 | 0.4 | |
| Sex | < .001 | ||||||||||
| Female | 235,238 | 49.7 | 185,171 | 49.8 | 9,972 | 44.4 | 31,676 | 57.5 | 8,419 | 34.3 | |
| Male | 238,484 | 50.3 | 186,457 | 50.2 | 12,470 | 55.6 | 23,459 | 42.5 | 16,098 | 65.7 | |
| Race | < .001 | ||||||||||
| White | 317,903 | 67.1 | 263,124 | 70.8 | 12,060 | 53.7 | 27,056 | 49.1 | 15,663 | 63.9 | |
| Black | 65,961 | 13.9 | 45,350 | 12.2 | 5,092 | 22.7 | 12,596 | 22.8 | 2,923 | 11.9 | |
| Hispanic | 49,344 | 10.4 | 32,930 | 8.9 | 3,718 | 16.6 | 10,314 | 18.7 | 2,382 | 9.7 | |
| Asian or Pacific Islander | 31,852 | 6.7 | 25,419 | 6.8 | 1,364 | 6.1 | 4,002 | 7.3 | 1,067 | 4.4 | |
| American Indian/Alaska native | 2,639 | 0.6 | 1,444 | 0.4 | 75 | 0.3 | 979 | 1.8 | 141 | 0.6 | |
| Unknown | 6,023 | 1.3 | 3,361 | 0.9 | 133 | 0.6 | 188 | 0.3 | 2,341 | 9.5 | |
| Marital status | < .001 | ||||||||||
| Single | 162,265 | 34.3 | 108,626 | 29.2 | 12,965 | 57.8 | 35,439 | 64.3 | 5,235 | 21.4 | |
| Married | 280,578 | 59.2 | 245,813 | 66.1 | 8,430 | 37.6 | 17,367 | 31.5 | 8,968 | 36.6 | |
| Unknown | 30,879 | 6.5 | 17,189 | 4.6 | 1,047 | 4.7 | 2,329 | 4.2 | 10,314 | 42.1 | |
| Residence | < .001 | ||||||||||
| Rural | 416,346 | 88.0 | 331,564 | 89.3 | 18,561 | 82.7 | 45,618 | 83.3 | 20,603 | 84.2 | |
| Urban | 56,638 | 12.0 | 39,861 | 10.7 | 3,872 | 17.3 | 9,129 | 16.7 | 3,776 | 15.4 | |
| Unknown | 148 | 0.0 | 44 | 0.0 | 4 | 0.0 | 3 | 0.0 | 97 | 0.4 | |
| Tumor stage* | < .001 | ||||||||||
| 0 | 3,389 | 0.8 | 2,617 | 0.7 | 157 | 0.8 | 379 | 0.7 | 236 | 1.0 | |
| 1 | 147,049 | 33.1 | 123,125 | 35.3 | 4,307 | 20.8 | 13,296 | 25.6 | 6,321 | 28.0 | |
| 2 | 135,706 | 30.6 | 111,140 | 31.9 | 4,637 | 22.4 | 13,176 | 25.3 | 6,753 | 30.0 | |
| 3 | 68,029 | 15.3 | 53,031 | 15.2 | 4,259 | 20.6 | 8,909 | 17.1 | 1,830 | 8.1 | |
| 4 | 48,065 | 10.8 | 32,373 | 9.3 | 4,433 | 21.4 | 9,901 | 19.0 | 1,358 | 6.0 | |
| Unknown | 41,945 | 9.4 | 26,662 | 7.6 | 2,907 | 14.0 | 6,329 | 12.2 | 6,047 | 26.8 | |
| Nodal stage* | < .001 | ||||||||||
| 0 | 271,920 | 61.2 | 223,777 | 64.1 | 9,867 | 47.7 | 24,982 | 48.1 | 13,294 | 59.0 | |
| 1 | 72,889 | 16.4 | 57,140 | 16.4 | 3,764 | 18.2 | 10,094 | 19.4 | 1,891 | 8.4 | |
| 2 | 50,455 | 11.4 | 36,542 | 10.5 | 3,650 | 17.6 | 8,961 | 17.2 | 1,302 | 5.8 | |
| 3 | 15,339 | 3.5 | 10,854 | 3.1 | 1,088 | 5.3 | 3,003 | 5.8 | 394 | 1.7 | |
| Unknown | 33,580 | 7.6 | 20,635 | 5.9 | 2,331 | 11.3 | 4,950 | 9.5 | 5,664 | 25.1 | |
| Metastasis* | |||||||||||
| No | 349,453 | 78.7 | 285,654 | 81.9 | 13,019 | 62.9 | 35,576 | 68.4 | 15,204 | 67.4 | |
| Yes | 70,947 | 16.0 | 49,030 | 14.1 | 6,293 | 30.4 | 13,346 | 25.7 | 2,278 | 10.1 | |
| Unknown | 23,783 | 5.4 | 14,264 | 4.1 | 1,388 | 6.7 | 3,068 | 5.9 | 5,063 | 22.5 | |
| Ann Arbor lymphoma staging* | < .001 | ||||||||||
| 1 | 8,441 | 28.6 | 6,684 | 29.5 | 390 | 22.4 | 761 | 24.2 | 606 | 31.1 | |
| 2 | 4,454 | 15.1 | 3,564 | 15.7 | 275 | 15.8 | 474 | 15.1 | 141 | 7.2 | |
| 3 | 4,562 | 15.5 | 3,613 | 16.0 | 323 | 18.6 | 492 | 15.7 | 134 | 6.9 | |
| 4 | 9,897 | 33.6 | 7,531 | 33.3 | 670 | 38.5 | 1,244 | 39.6 | 452 | 23.2 | |
| Unknown | 2,125 | 7.2 | 1,253 | 5.5 | 83 | 4.8 | 171 | 5.4 | 618 | 31.7 | |
| Cancer-directed surgery and/or radiation therapy | < .001 | ||||||||||
| No | 114,473 | 24.2 | 75,809 | 20.4 | 8,506 | 37.9 | 17,698 | 32.1 | 12,460 | 50.8 | |
| Yes | 359,249 | 75.8 | 295,819 | 79.6 | 13,936 | 62.1 | 37,437 | 67.9 | 12,057 | 49.2 | |
| Malignancy | NA | ||||||||||
| Breast | 135,736 | 28.7 | 111,948 | 30.1 | 3,458 | 15.4 | 16,317 | 29.6 | 4,013 | 16.4 | |
| Prostate | 101,899 | 21.5 | 86,477 | 23.3 | 2,515 | 11.2 | 3,718 | 6.7 | 9,189 | 37.5 | |
| Lung | 66,918 | 14.1 | 47,326 | 12.7 | 5,036 | 22.4 | 12,036 | 21.8 | 2,520 | 10.3 | |
| Colorectal | 61,116 | 12.9 | 46,971 | 12.6 | 4,088 | 18.2 | 7,046 | 12.8 | 3,011 | 12.3 | |
| Head and neck | 29,691 | 6.3 | 21,335 | 5.7 | 2,125 | 9.5 | 4,501 | 8.2 | 1,730 | 7.1 | |
| NHL | 29,539 | 6.2 | 22,680 | 6.1 | 1,742 | 7.8 | 3,145 | 5.7 | 1,972 | 8.0 | |
| Liver | 16,541 | 3.5 | 10,659 | 2.9 | 1,247 | 5.6 | 3,788 | 6.9 | 847 | 3.5 | |
| Pancreas | 13,687 | 2.9 | 10,168 | 2.7 | 917 | 4.1 | 1,996 | 3.6 | 606 | 2.5 | |
| Ovary | 12,340 | 2.6 | 9,561 | 2.6 | 858 | 3.8 | 1,570 | 2.8 | 351 | 1.4 | |
| Esophagus | 6,255 | 1.3 | 4,503 | 1.2 | 456 | 2.0 | 1,018 | 1.8 | 278 | 1.1 | |
Abbreviations: NA, not available; NHL, non-Hodgkin lymphoma.
TNM staging applies to all tumors except NHL.
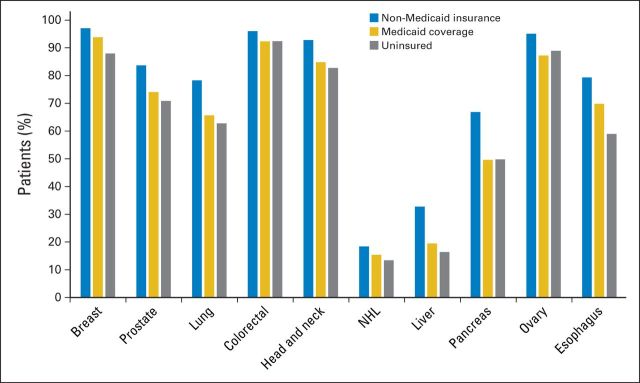
Stage at Diagnosis
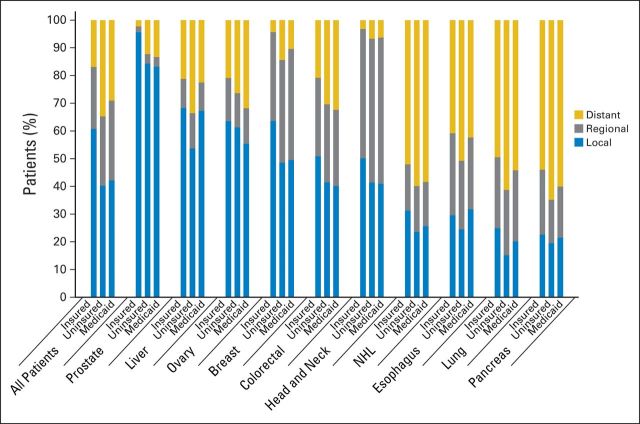
Overall, patients with non-Medicaid insurance were less likely to present with distant disease (16.9%) than those without any insurance coverage (34.7%). Correspondingly, patients with non-Medicaid insurance were more likely to present with localized disease (60.8%) compared with those without insurance coverage (40.3%; P < .001). Of patients with Medicaid coverage, an intermediate proportion presented with distant (29.1%) and localized (42.2%) disease. Proportions of patients presenting with distant, regional, and localized disease for all patients and by cancer site are summarized in Figure 1.
Fig 1.
Proportion of patients presenting with localized, regional, or distant disease by insurance status. All P < .001. For non-Hodgkin lymphoma (NHL), Ann Arbor stage I disease was considered localized, stage II to III disease was considered regional, and stage IV disease was considered distant.
Cancer-Directed Treatment
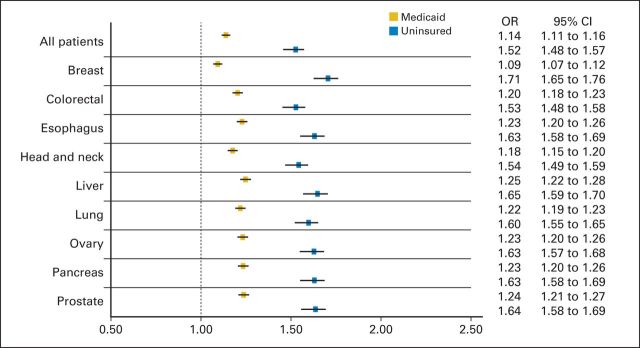
Among those with nonmetastatic disease, 50.5% underwent surgery alone, 13.8% received RT alone, and 22.4% both underwent surgery and received RT. Patients with non-Medicaid insurance were more likely to undergo cancer-directed surgery and/or receive RT (79.6%) as compared with those without insurance coverage (62.1%; P < .001). Again, patients with Medicaid coverage had an intermediate proportion who received definitive treatment (67.9%; Appendix Fig A1, online only). In a logistic regression that adjusted for demographics, patients with nonmetastatic disease were more likely to not undergo cancer-directed surgery and/or receive RT if they lacked insurance (OR, 1.52; 95% CI, 1.48 to 1.57; P < .001) or had Medicaid coverage (OR, 1.14; 95% CI, 1.11 to 1.16; P < .001; Fig 2).
Fig 2.
Forest plot depicting odds ratios (ORs) and 95% CIs for not undergoing cancer-directed surgery and/or receiving radiation therapy for patients with nonmetastatic disease with Medicaid coverage and those with no insurance as compared with patients with non-Medicaid insurance. All sites controlled for age, race, sex, marital status, residence (urban v rural), and percent of county below federal poverty level.
Cause-Specific Survival
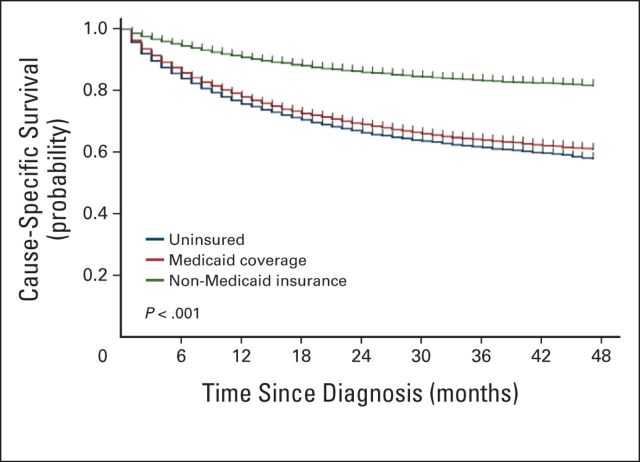
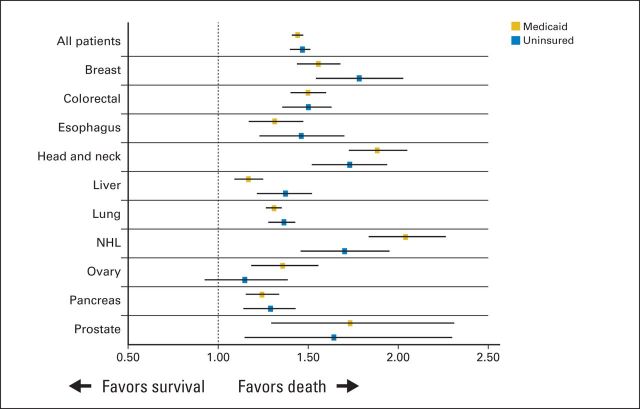
Unadjusted 2-year cause-specific survival among those with non-Medicaid insurance was 86.2%, compared with 69.1% among those with Medicaid coverage and 66.5% among those without insurance coverage (P < .001; Fig 3). In a Cox regression that adjusted for demographics, site, stage (local, regional, or distant), and undergoing cancer-directed surgery and/or receiving RT, patients were more likely to die as a result of their disease if they had Medicaid coverage (HR, 1.44; 95% CI, 1.41 to 1.47; P < .001) or did not have insurance (HR, 1.47; 95% CI, 1.42 to 1.51; P < .001) compared with those with non-Medicaid insurance (Fig 4). Among all patients, the following were associated with increased risk of death: Medicaid coverage or no insurance, older age, male sex, black race, single marital status, advanced disease stage, rural residence, increased county poverty level, and lack of cancer-directed surgery and/or RT (Table 2). Moreover, there was variability in risk of death according to disease site.
Fig 3.
Unadjusted Kaplan-Meier curve illustrating cause-specific survival by insurance status for patients with one of 10 most deadly cancers. P < .001.
Fig 4.
Forest plot depicting hazard ratios and 95% CIs for cancer-specific death for patients with Medicaid coverage and those with no insurance as compared with patients with non-Medicaid insurance. All sites controlled for age, race, sex, marital status, stage (local, regional, or distant), residence (urban v rural), percent of county below federal poverty level, and undergoing cancer-directed surgery and/or receiving radiation therapy. Breast and prostate sites also controlled for estrogen receptor and prostate-specific antigen and Gleason score, respectively. NHL, non-Hodgkin lymphoma.
Table 2.
Results of Multivariable Analysis to Determine Predictors of Cancer-Specific Mortality
| Variable | HR | 95% CI | P |
|---|---|---|---|
| Insurance status | |||
| Non-Medicaid insurance | 1 | ||
| Medicaid coverage | 1.44 | 1.41 to 1.47 | < .001 |
| Uninsured | 1.47 | 1.42 to 1.51 | < .001 |
| Age | |||
| Continuous | 1.01 | 1.01 to 1.01 | < .001 |
| Sex | |||
| Female | 1 | ||
| Male | 1.26 | 1.24 to 1.29 | < .001 |
| Race | |||
| White | 1 | ||
| Black | 1.15 | 1.12 to 1.17 | < .001 |
| Hispanic | 1.00 | 0.97 to 1.03 | .83 |
| Asian or Pacific Islander | 0.89 | 0.86 to 0.92 | < .001 |
| American Indian/Alaska native | 1.08 | 0.96 to 1.21 | .20 |
| Unknown | 0.54 | 0.44 to 0.67 | < .001 |
| Marital status | |||
| Married | 1 | ||
| Single | 1.23 | 1.21 to 1.25 | < .001 |
| Disease site | |||
| Breast | 1 | ||
| Prostate | 0.42 | 0.39 to 0.45 | < .001 |
| Lung | 8.05 | 7.76 to 8.36 | < .001 |
| Colorectal | 2.63 | 2.52 to 2.74 | < .001 |
| Head and neck | 3.44 | 3.28 to 3.61 | < .001 |
| NHL | 0.83 | 0.79 to 0.88 | < .001 |
| Liver | 13.18 | 12.59 to 13.79 | < .001 |
| Pancreas | 11.74 | 11.24 to 12.26 | < .001 |
| Ovary | 4.01 | 3.78 to 4.24 | < .001 |
| Esophagus | 9.01 | 8.53 to 9.51 | < .001 |
| Disease stage | |||
| Local | 1 | ||
| Regional | 2.59 | 2.52 to 2.67 | < .001 |
| Distant | 7.32 | 7.13 to 7.51 | < .001 |
| Residence | |||
| Urban | 1 | ||
| Rural | 1.06 | 1.04 to 1.09 | < .001 |
| Percent of county below federal poverty level | |||
| Continuous | 1.01 | 1.01 to 1.02 | < .001 |
| Cancer-directed surgery and/or radiation therapy | |||
| Yes | 1 | ||
| No | 1.63 | 1.60 to 1.67 | < .001 |
Abbreviations: HR, hazard ratio; NHL, non-Hodgkin lymphoma.
DISCUSSION
This study analyzed the association of insurance status with disease stage at presentation, treatment, and survival among patients diagnosed with one of the 10 most deadly cancers and is the first to do so, to our knowledge, using the SEER data set. We found that those with Medicaid coverage or without insurance were more likely to present with advanced-stage disease and less likely to undergo cancer-directed surgery and/or receive RT for nonmetastatic disease. In addition, we found that patients with Medicaid coverage or without insurance had worse survival, even after controlling for demographic information, stage at diagnosis, and undergoing cancer-directed surgery and/or receiving RT.
It has been estimated that among adults age 19 to 64 years surveyed in 2010, 16% were underinsured and 28% were uninsured in the United States.18 Underinsured status is designated based on a patient's having high out-of-pocket medical costs in relation to his or her income. In total, 44% of adults age 19 to 64 years are uninsured or underinsured, amounting to 81 million individuals. As a result of the ACA, subsidies will expand access to public and private health insurance for individuals with lower incomes, and limitations to coverage resulting from preexisting conditions will be removed. In addition, dependents can retain their parents' insurance plans until their 26th birthday. It is estimated that the ACA could result in a 70% reduction in the number of underinsured individuals as well as a 60% drop in the number of uninsured individuals.18 Expanded access to insurance coverage and expanded services available through participating state Medicaid plans will likely affect cancer care.
Our study found that patients with Medicaid coverage seemed to have intermediate proportions presenting with later stages of disease and receiving local treatment as compared with the insured and uninsured cohorts; however, although there was some variability by cancer site, those with Medicaid seemed to have only marginally improved survival as compared with those who were uninsured after accounting for stage at presentation and undergoing cancer-directed surgery and/or receiving RT. Some of this survival discrepancy may be attributed to the interruptions in coverage to which Medicaid patients can be subject. That said, previous research has demonstrated that on a more global scale, the expansion of Medicaid programs is associated with improved self-reported health and reduced mortality.19 This suggests that the implementation of Medicaid may have differential effects on survival outcomes from cancer and noncancer diagnoses.
Nonetheless, as part of the ACA, enrollment in Medicaid is expected to expand. Currently, only 63% of eligible adults age 19 to 64 year enroll in Medicaid, with wide geographic differences in use.20 With the expansions under the ACA, enrollment is expected to increase from approximately 55 million to 105 million by 2019.21 The Breast and Cervical Cancer Prevention and Treatment Act of 2000 allowed states to extend Medicaid eligibility to women diagnosed with breast or cervical cancer through federally funded screening programs. Since its adoption, every state has adopted this optional Medicaid expansion, although there has been some variation in timing and implementation.22 No other patients with a particular cancer type have expanded access to Medicaid. However, despite this expanded access, we found that although patients with breast cancer with Medicaid coverage presented with earlier-stage disease and more often underwent cancer-directed surgery and/or received RT as compared with uninsured patients with breast cancer, cause-specific survival among patients with breast cancer with Medicaid was similar to that among those who were uninsured (after accounting for stage at presentation and undergoing cancer-directed surgery and/or receiving RT).
Data from the National Cancer Database (NCDB), a hospital-based cancer registry, have previously shown that uninsured patients are more likely to present with advanced-stage disease in lung,7 breast,23 prostate,24 cervical,25 head and neck,8,26 and other cancer types.5,6 Uninsured patients are less likely to receive definitive treatment in lung,7 breast,9 and bladder cancers.27 In addition, worse survival among those without insurance has been demonstrated for a variety of cancer types.10–12 However, these studies looked only at specific cancers and were not as broad in scope as our work. Moreover, the NCDB represents only patients treated in a hospital setting and does not capture patients treated exclusively as outpatients. It is possible that patients with early-stage disease are more likely to be diagnosed and treated exclusively in freestanding centers and thus would not be captured by the NCDB. In addition, a significant portion of patients without health insurance may not be treated at participating centers accredited by the Commission on Cancer of the American College of Surgeons and thus would not be included in these studies. Finally, it is not known how representative the population included in the NCDB is of the entire US population. Conversely, the SEER data set has been shown to be representative of the US population with regard to income and education, although it does tend to have a higher proportion of foreign-born individuals.28 One study from 2013 did look at the association of insurance status with outcomes in the SEER data set; however, it used county-level data to estimate insurance rates.29
Our study has certain limitations as a function of the data set used. For one, the SEER database does not report patient-level income, and therefore, we used county-level income data as a surrogate for patient socioeconomic status. Moreover, the SEER registry does not contain information on comorbid conditions or performance status, staging workup, or use of systemic therapy, which influence cause-specific survival and for which we could not adjust our analysis. Nonetheless, it is unlikely that insurance status is merely a surrogate for receipt of chemotherapy, because 52% of patients underwent surgery and 39% received RT in our cohort despite not having insurance coverage. Of note, patients who undergo definitive surgery may undergo more extensive preoperative workup as well more complete intraoperative and pathologic staging, which could have influenced the results of this analysis. In addition, the SEER insurance variable does not further subdivide those with insurance (managed care, health maintenance organization, or preferred provider organization), Medicare, and coverage from the military or Veterans Affairs. Some patients who may have enrolled in Medicaid or other insurance after their diagnosis may not have been correctly captured in this data set. This could potentially dilute the discrepancies in presentation, treatment, and survival among those who have Medicaid coverage and the uninsured. There is evidence that those who enroll in Medicaid around the time of diagnosis present with more-advanced disease30 and display worse survival31 compared with those who were previously enrolled in Medicaid. In addition, 5.2% of patients had unknown insurance status, although on sensitivity analysis, this did not influence the results of the multivariable survival model. Finally, given the lack of specificity in Medicare designation in the SEER data set, we were unable to make conclusions about patients age ≥ 65 years.
Despite our findings, it is unknown to what degree the expansion of private and public health insurance will improve cancer outcomes. Some patients who do not have access to health insurance or who do not actively enroll in Medicaid may be subject to other barriers (lack of transportation, poor social support, and so on) that may limit their ability to receive care. Similarly, they may have financial barriers that limit their ability to pay rising deductibles and copays, which are required to use insurance. Moreover, these patients are more likely to be disabled and suffer from psychiatric or other comorbidities.31 Such factors may contribute to more-advanced disease presentation, inadequate treatment, and ultimately worse survival. Thus, providing health insurance among some members of the population may not inherently lead to improved outcomes. Moreover, it is quite possible that different types of cancer will be differentially affected by the proposed expansions to private and public health insurance. At least among the top 10 causes of cancer death, we noted that lung cancer had the highest proportion of uninsured patients (22.4%; Table 1).
Nonetheless, further research to explore the interaction between insurance status and cancer outcomes is undoubtedly warranted. Given the poor outcomes noted among patients with cancer with Medicaid, it would be helpful to know to what degree this is a result of patient, tumor, or treatment-related factors. Such information will be key in the improvement of cancer outcomes in this cohort of patients. Similarly, given the barriers to cancer care that many patients experience, further research is needed to identify ways to improve cancer detection, increase the rate of cancer-directed therapy, and improve outcomes.
In summary, lack of insurance is associated with advanced disease stage at presentation, less use of cancer-directed surgery and/or RT, and worse survival among patients diagnosed with one of the 10 most deadly cancers in this large, population-based data set. Upcoming changes resulting in the expansion of private insurance and Medicaid will likely alter cancer care in the United States. Further research will be required to determine if and to what degree the presentation, treatment, and outcomes of cancer are affected.
Glossary Terms
- Surveillance, Epidemiology, and End Results (SEER):
a national cancer registry that collects information from all incident malignancies in multiple geographic areas of the United States.
Appendix
Fig A1.
Proportion of patients with nonmetastatic disease treated with cancer-directed surgery and/or radiation therapy by insurance status. NHL, non-Hodgkin lymphoma.
Footnotes
Supported by Training Fellowship Grant No. T15 LM007093 from the Keck Center for Interdisciplinary Bioscience Training of the Gulf Coast Consortia (G.V.W.).
Presented at the 96th Annual Meeting of the American Radium Society, St Thomas, US Virgin Islands, April 26-30, 2014.
Terms in blue are defined in the glossary, found at the end of this article and online at www.jco.org.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Although all authors completed the disclosure declaration, the following author(s) and/or an author's immediate family member(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO's conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: None Consultant or Advisory Role: None Stock Ownership: None Honoraria: None Research Funding: Benjamin D. Smith, Varian Medical Systems Expert Testimony: None Patents, Royalties, and Licenses: None Other Remuneration: None
AUTHOR CONTRIBUTIONS
Conception and design: Gary V. Walker, Stephen R. Grant, B. Ashleigh Guadagnolo, Matthew Koshy, Usama Mahmood
Collection and assembly of data: Gary V. Walker, Stephen R. Grant, Usama Mahmood
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2012. http://www.census.gov/prod/2013pubs/p60-245.pdf.
- 2. Patient Protection and Affordable Care Act. Pub Law 111-148.
- 3.Hutchins VA, Samuels MB, Lively AM. Analyzing the affordable care act: Essential health benefits and implications for oncology. J Oncol Pract. 2013;9:73–77. doi: 10.1200/JOP.2012.000881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoyert DL, Xu J. Deaths: Preliminary Data for 2011. http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_06.pdf. [PubMed]
- 5.Ward EM, Fedewa SA, Cokkinides V, et al. The association of insurance and stage at diagnosis among patients aged 55 to 74 years in the national cancer database. Cancer J. 2010;16:614–621. doi: 10.1097/PPO.0b013e3181ff2aec. [DOI] [PubMed] [Google Scholar]
- 6.Halpern MT, Ward EM, Pavluck AL, et al. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: A retrospective analysis. Lancet Oncol. 2008;9:222–231. doi: 10.1016/S1470-2045(08)70032-9. [DOI] [PubMed] [Google Scholar]
- 7.Slatore CG, Au DH, Gould MK, et al. An official American Thoracic Society systematic review: Insurance status and disparities in lung cancer practices and outcomes. Am J Respir Crit Care Med. 2010;182:1195–1205. doi: 10.1164/rccm.2009-038ST. [DOI] [PubMed] [Google Scholar]
- 8.Chen AY, Schrag NM, Halpern M, et al. Health insurance and stage at diagnosis of laryngeal cancer: Does insurance type predict stage at diagnosis? Arch Otolaryngol Head Neck Surg. 2007;133:784–790. doi: 10.1001/archotol.133.8.784. [DOI] [PubMed] [Google Scholar]
- 9.Freedman RA, Virgo KS, He Y, et al. The association of race/ethnicity, insurance status, and socioeconomic factors with breast cancer care. Cancer. 2011;117:180–189. doi: 10.1002/cncr.25542. [DOI] [PubMed] [Google Scholar]
- 10.Robbins AS, Pavluck AL, Fedewa SA, et al. Insurance status, comorbidity level, and survival among colorectal cancer patients age 18 to 64 years in the National Cancer Data Base from 2003 to 2005. J Clin Oncol. 2009;27:3627–3633. doi: 10.1200/JCO.2008.20.8025. [DOI] [PubMed] [Google Scholar]
- 11.Robbins AS, Chen AY, Stewart AK, et al. Insurance status and survival disparities among nonelderly rectal cancer patients in the National Cancer Data Base. Cancer. 2010;116:4178–4186. doi: 10.1002/cncr.25317. [DOI] [PubMed] [Google Scholar]
- 12.Fedewa SA, Lerro C, Chase D, et al. Insurance status and racial differences in uterine cancer survival: A study of patients in the National Cancer Database. Gynecol Oncol. 2011;122:63–68. doi: 10.1016/j.ygyno.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Zippin C, Lum D, Hankey BF. Completeness of hospital cancer case reporting from the SEER Program of the National Cancer Institute. Cancer. 1995;76:2343–2350. doi: 10.1002/1097-0142(19951201)76:11<2343::aid-cncr2820761124>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 14.Number of Persons by Race and Hispanic Ethnicity for SEER Participants (2010 Census Data) National Cancer Institute. 2013 [Google Scholar]
- 15.Surveillance, Epidemiology, and End Results Program: SEER Data, 1973-2011. http://seer.cancer.gov/data/
- 16.Surveillance Epidemiology, and End Results Program: County Attributes. http://seer.cancer.gov/seerstat/variables/countyattribs/
- 17.Greene FL, Page DL, Fleming ID, et al., editors. AJCC Cancer Staging Manual (ed 6) New York, NY: Springer-Verlag; 2002. [Google Scholar]
- 18.Schoen C, Doty MM, Robertson RH, et al. Affordable Care Act reforms could reduce the number of underinsured US adults by 70 percent. Health Aff (Millwood) 2011;30:1762–1771. doi: 10.1377/hlthaff.2011.0335. [DOI] [PubMed] [Google Scholar]
- 19.Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med. 2012;367:1025–1034. doi: 10.1056/NEJMsa1202099. [DOI] [PubMed] [Google Scholar]
- 20.Sommers BD, Tomasi MR, Swartz K, et al. Reasons for the wide variation in Medicaid participation rates among states hold lessons for coverage expansion in 2014. Health Aff (Millwood) 2012;31:909–919. doi: 10.1377/hlthaff.2011.0977. [DOI] [PubMed] [Google Scholar]
- 21.Iglehart J. Medicaid expansion offers solutions, challenges. Health Aff (Millwood) 2010;29:230–232. doi: 10.1377/hlthaff.2010.0010. [DOI] [PubMed] [Google Scholar]
- 22.Lantz PM, Soliman S. An evaluation of a Medicaid expansion for cancer care: The Breast and Cervical Cancer Prevention and Treatment Act of 2000. Womens Health Issues. 2009;19:221–231. doi: 10.1016/j.whi.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 23.DeSantis C, Jemal A, Ward E. Disparities in breast cancer prognostic factors by race, insurance status, and education. Cancer Causes Control. 2010;21:1445–1450. doi: 10.1007/s10552-010-9572-z. [DOI] [PubMed] [Google Scholar]
- 24.Fedewa SA, Etzioni R, Flanders WD, et al. Association of insurance and race/ethnicity with disease severity among men diagnosed with prostate cancer, National Cancer Database 2004-2006. Cancer Epidemiol Biomarkers Prev. 2010;19:2437–2444. doi: 10.1158/1055-9965.EPI-10-0299. [DOI] [PubMed] [Google Scholar]
- 25.Fedewa SA, Cokkinides V, Virgo KS, et al. Association of insurance status and age with cervical cancer stage at diagnosis: National Cancer Database, 2000-2007. Am J Public Health. 2012;102:1782–1790. doi: 10.2105/AJPH.2011.300532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen AY, Schrag NM, Halpern MT, et al. The impact of health insurance status on stage at diagnosis of oropharyngeal cancer. Cancer. 2007;110:395–402. doi: 10.1002/cncr.22788. [DOI] [PubMed] [Google Scholar]
- 27.Fedeli U, Fedewa SA, Ward EM. Treatment of muscle invasive bladder cancer: Evidence from the National Cancer Database, 2003 to 2007. J Urol. 2011;185:72–78. doi: 10.1016/j.juro.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 28.Surveillance Epidemiology, and End Results Program. Population Characteristics. http://seer.cancer.gov/registries/characteristics.html.
- 29.Smith JK, Ng SC, Zhou Z, et al. Does increasing insurance improve outcomes for US cancer patients? J Surg Res. 2013;185:15–20. doi: 10.1016/j.jss.2013.05.058. [DOI] [PubMed] [Google Scholar]
- 30.Bradley CJ, Given CW, Roberts C. Late stage cancers in a Medicaid-insured population. Med Care. 2003;41:722–728. doi: 10.1097/01.MLR.0000065126.73750.D1. [DOI] [PubMed] [Google Scholar]
- 31.Koroukian SM, Bakaki PM, Raghavan D. Survival disparities by Medicaid status. Cancer. 2012;118:4271–4279. doi: 10.1002/cncr.27380. [DOI] [PMC free article] [PubMed] [Google Scholar]