Abstract
Background:
In Indiana, high school football coaches are required to complete a coaching education course with material related to concussion awareness, equipment fitting, heat emergency preparedness, and proper technique. Some high schools have also opted to implement a player safety coach (PSC). The PSC, an integral component of USA Football’s Heads Up Football (HUF) program, is a coach whose primary responsibility is to ensure that other coaches are implementing proper tackling and blocking techniques alongside other components of the HUF program.
Purpose:
To compare injury rates in Indiana high school football teams by their usage of a PSC or online coaching education only.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
Athletic trainers (ATs) evaluated and tracked injuries at each practice and game during the 2015 high school football season. Players were drawn from 6 teams in Indiana. The PSC group, which used the PSC component, was comprised of 204 players from 3 teams. The “education only” group (EDU), which utilized coaching education only, was composed of 186 players from 3 teams. Injury rates and injury rate ratios (IRRs) were reported with 95% confidence intervals (CIs).
Results:
During 25,938 athlete-exposures (AEs), a total of 149 injuries were reported, of which 54 (36.2%) and 95 (63.8%) originated from the PSC and EDU groups, respectively. The practice injury rate was lower in the PSC group than the EDU group (2.99 vs 4.83/1000 AEs; IRR, 0.62; 95% CI, 0.40-0.95). The game injury rate was also lower in the PSC group than the EDU group (11.37 vs 26.37/1000 AEs; IRR, 0.43; 95% CI, 0.25-0.74). When restricted to concussions only, the rate was lower in the PSC group (0.09 vs 0.73/1000 AEs; IRR, 0.12; 95% CI, 0.01-0.94), although only 1 concussion was reported in the PSC group. No differences were found in game concussion rates (0.60 vs 4.39/1000 AEs; IRR, 0.14; 95% CI, 0.02-1.11).
Conclusion:
Findings support the PSC as an effective method of injury mitigation in high school football. Future research should seek to replicate this study using larger samples from additional states.
Keywords: epidemiology, pediatrics, prevention
Over 1 million high school students play tackle football annually in the United States.16 Because of the high rates of injury and concussion in football,5,11,15,20,23 there is concern regarding the health and safety of this large population of high school athletes. The Institute of Medicine (IOM) has called for research examining the incidence of concussion in young athletes as well as the effectiveness of interventions aiming to reduce the incidence of concussion and other injuries.9
In 2014, the Indiana General Assembly passed the Senate Enrolled Act Number 222 (SEA222), which required all “football coaches and assistant football coaches who are coaching individuals less than 20 years of age to complete a course concerning player safety and concussions at least once during a 2-year period.”8 The statute requires that the course include education regarding concussion awareness, equipment fitting, heat emergency preparedness, and proper football technique and be approved by the Indiana Department of Education (IDOE). The IDOE found that the HUF Certification Course satisfies all the requirements of SEA222.21
The HUF Certification Course, however, is just one component of USA Football’s Heads Up Football (HUF) program.22 The other integral piece of the program is the in-person training and implementation of the player safety coach (PSC). The PSC is a coach whose primary responsibility is to ensure other coaches are adhering to proper safety protocols, including instructing proper tackling and blocking techniques and ensuring proper equipment fitting. The PSC is generally a long-standing member of the coaching staff who receives additional in-person HUF training from a USA Football Master Trainer. Using the socioecological model as a frame of reference, Kerr et al12 posited that factors across multiple levels of influence (eg, individual, interpersonal, environmental, policy/law) affect concussion incidence and reporting and that interventions should consider attending to these multiple levels. Thus, the addition of a PSC may target multiple levels across the socioecological model.12
Neither the effectiveness of the HUF program at the high school level nor the added benefit of the PSC at the high school level has yet been examined. However, promising findings regarding the effectiveness of the HUF program have been reported in the Fairfax County (Virginia) Public School District.6 Previous research examining the HUF program including the PSC has found its implementation in youth football to be associated with lower injury rates and a smaller number of head impacts sustained in practices.13,14 Examination of interventions to reduce the incidence and severity of injury are important for high school football given that high school football injury rates exceed those reported in youth football.4,5 Because Indiana high school football coaches are required to complete a football-specific coaching education course with material related to concussion awareness, equipment fitting, heat emergency preparedness, and proper technique (all components of the HUF program)8 but are not required to have a PSC, an opportunity to examine the effect of the PSC exists. Therefore, the purpose of the current study was to examine the effect of the usage of a PSC on the incidence of injuries, particularly concussions, within Indiana high school football players during the 2015 season.
Methods
Design and Participants
This study employed a single-season observational cohort design. We utilized a convenience sample of 6 high schools that were followed over the 2015 high school football season. Three high schools were in the PSC group, which utilized the HUF program’s PSC component. The remaining 3 were in the “education only” group (EDU), which utilized online coaching education only.
We recruited high schools based on criteria that they were located in Indiana, had a high school football program, and utilized 1 full-time athletic trainer (AT) for football, as previous research suggested that high schools with full-time versus outreach ATs varied in the reporting of football injury rates.10 High schools that were interested were provided with training for data collection. As we recruited high schools, we ensured that equitable demographics existed between groups. Thus, within both the PSC and EDU groups, 2 of the 3 high schools were located in rural settings, and 1 of the 3 high schools had student populations over 1000 students. The 3 high schools in the PSC group had a total of 204 players, while the 3 high schools in the EDU group had a total of 186 players.
Coach Education Programming
As mandated by SEA222, all 6 high schools in this study were required to have their football coaches complete a football-specific coaching education course with material related to concussion awareness, equipment fitting, heat emergency preparedness, and proper technique.8 All 6 high schools completed the HUF Certification Course, which was hosted on the National Federation of State High School Associations (NFHS) website.17 This coursework is comprised of 4 modules: (1) concussion, (2) heat and hydration, (3) cardiac arrest, and (4) proper tackling, blocking, and equipment fit. After each module, participants completed a test to gauge their understanding of the concepts. The first 3 modules were provided by NFHS, whereas the fourth module was developed by USA Football.
The presence of the PSC component served as the independent variable. The EDU schools were selected if the team self-identified as not utilizing a PSC. The PSC schools were selected if the team had an identified PSC that was confirmed by USA Football as having participated in an in-person training program with a Master Trainer. Because both PSC and EDU high schools completed the HUF Certification Course, the primary difference between study arms is the presence of a PSC, which allows for the closest proxy of examining the direct effect of the PSC.
Data Collection
Data were collected as part of the National Athletic Treatment, Injury, and Outcomes Network (NATION), an independent injury surveillance program operated by the Datalys Center for Sports Injury Research and Prevention.5 The methodology of NATION has been previously described.5 Definitions related to data collected are provided in Table 1.
TABLE 1.
Definitions Related to Data Collected in the Study
| Injury | Injury or illness occurring during a school-sanctioned game or practice and requiring examination from an athletic trainer (AT) or team physician. |
| Time-loss injury | Injury or illness that requires restricted participation at least 24 hours beyond the day of injury. |
| Concussion | Did not provide a working definition of concussion and relied on the expertise and knowledge of ATs and the medical staff with whom they work to properly detect and diagnose concussions. As required by SEA222, players were required to obtain physician approval to return to sport after concussion. |
| Athlete-exposure | One player participating in 1 game or 1 practice. |
| Injury rate | Estimate of injury incidence that includes player time of exposure, calculated as the sum of all injuries (numerator) divided by the sum of athlete-exposures (denominator). Injury rates were expressed per 1000 athlete-exposures and reported with 95% confidence intervals. |
| Injury rate ratio | Quotient of dividing 1 injury rate by another injury rate (eg, RateA/RateB); a common rate ratio is one that compares the game injury rate to the practice injury rate (ie, Rategame/Ratepractice). |
ATs reported all injury data in real-time from all games and practices that occurred during the 2015 season. Reporting was done through the electronic health record application used by medical staff throughout the academic year as part of their daily clinical practice. In addition, ATs also provided the number of student-athletes participating in each game and practice. Common data elements that included injury and exposure information were de-identified, recoded, and exported to an aggregate database. This process eliminates the burden of double data entry by extracting the de-identified common data elements directly from the application rather than asking ATs to document injuries twice (once for their own records and once for the study). All ATs received standardized training in the use of their electronic medical records in the context of NATION. Injury and exposure information were exported through an automated export process and reviewed by quality control staff weekly. If range and consistency checks identified questionable values, the quality control staff would contact the AT to help correct any errors.
Statistical Analyses
Data were analyzed using SAS-Enterprise Guide software (version 5.1; SAS Institute Inc). Frequencies were calculated by event type (eg, practices, competitions), type of injury (eg, concussion, contusion, fracture, sprain, strain, other), and mechanism of injury (eg, player contact, surface contact, noncontact, overuse, other). Injury rates were calculated by event type. Injury rate ratios (IRRs) with 95% CIs compared the incidence of injury across groups (Table 1). IRRs with 95% CIs not including 1.00 were considered statistically significant. To compare injury rates between the PSC and EDU groups, we used an intent-to-treat analysis. The intent-to-treat analysis maintains classifications for players as being within PSC and EDU groups regardless of whether the teams adhered to those principles. Analyses were performed in 3 subgroups: the first included all reported injuries; second, only TL injuries were included; third, only concussions were included. The study protocol was reviewed and approved by the Western Institutional Review Board (Puyallup, Washington).
Results
Injury Counts
In total, 149 injuries were reported by ATs, of which 54 (36.2%) and 95 (63.8%) originated from the PSC and EDU groups, respectively (Table 2). Most injuries were reported during practices: overall, 59.1% (n = 88/149); within the PSC group, 64.8% (n = 35/54); and within the EDU group, 55.8% (n = 53/95). Most injuries were TL injuries: overall, 53.7% (n = 80/149); in the PSC group, 57.4% (n = 31/54); and in the EDU group, 51.6% (n = 49/95).
TABLE 2.
Injury Rates in Indiana High School Football Teams Implementing the Heads Up Football Educational Program With the PSC Component Versus EDU by Event Type and Type of Injury, 2015 Seasona
| PSC (n = 3) | EDU (n = 3) | Rate Ratio (95% CI), PSC vs EDU | |||
|---|---|---|---|---|---|
| Injuries in Sample, n | Rate (95% CI) per 1000 AEs | Injuries in Sample, n | Rate (95% CI) per 1000 AEs | ||
| All injuries | |||||
| Game | 19 | 11.37 (6.26-16.48) | 42 | 26.37 (18.39-34.34) | 0.43 (0.25-0.74)b |
| Practice | 35 | 2.99 (2.00-3.98) | 53 | 4.83 (3.53-6.13) | 0.62 (0.40-0.95)b |
| TL injuries only | |||||
| Game | 10 | 5.98 (2.28-9.69) | 15 | 9.42 (4.65-14.18) | 0.64 (0.29-1.41) |
| Practice | 21 | 1.79 (1.03-2.56) | 34 | 3.10 (2.06-4.14) | 0.57 (0.34-1.00)b |
| Concussions only | |||||
| Game | 1 | 0.60 (0.00-1.77) | 7 | 4.39 (1.14, 7.65) | 0.14 (0.02-1.11) |
| Practice | 1 | 0.09 (0.00-0.25) | 8 | 0.73 (0.22, 1.23) | 0.12 (0.01-0.94)b |
aAE, athlete-exposure; EDU, education only group; PSC, player safety coach; TL, time loss (resulting in time loss of at least 24 hours).
bSignificant (rate ratio 95% CI does not include 1.00).
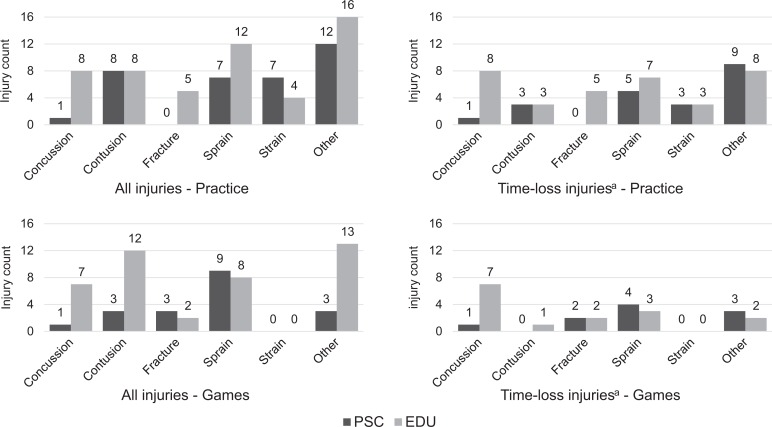
Type of Injury
A total of 17 concussions were reported overall, comprising 11.4% of all injuries. Most concussions were reported in the EDU group (88.2%, n = 15/17) as compared with the PSC group (11.8%, n = 2/17). Other common injuries overall included sprains (24.2%, n = 36/149), contusions (20.8%, n = 31/149), strains (7.4%, n = 11/149), and fractures (6.7%, n = 10/149). In practices and games, injury counts for specific types of injury were lower in the PSC group than the EDU group for all mechanisms except contusions and strains in practices and sprains in games (Figure 1). These findings were mostly similar when restricted to TL injuries.
Figure 1.
Injury counts in Indiana high school football teams implementing the Heads Up Football educational program with the player safety coach component (PSC) versus coaching education only (EDU) by event type and type of injury, 2015 season. aTime-loss injuries are those injuries that restrict participation for at least 24 hours.
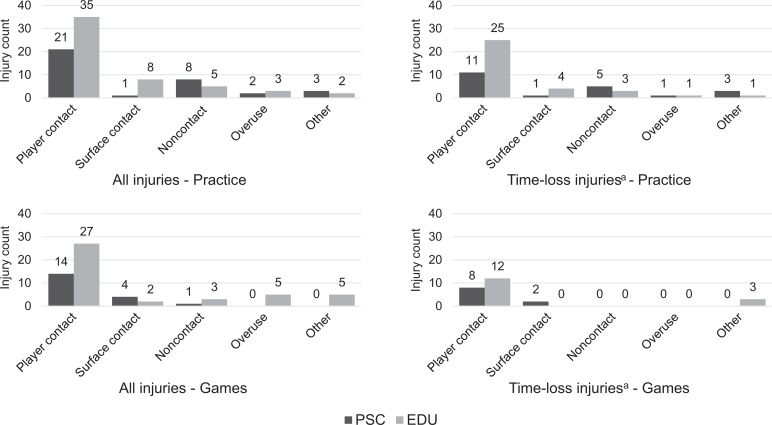
Mechanism of Injury
Most injuries overall were due to player contact (65.1%, n = 97/149), followed by noncontact (11.4%, n = 17/149), and surface contact (10.1%, n = 15/149). In practices and games, injury counts for specific types of injury were lower in the PSC group than the EDU group for all mechanisms except surface contact in practices and noncontact in games (Figure 2). These findings were similar when restricted to TL injuries.
Figure 2.
Injury counts in Indiana high school football teams implementing the Heads Up Football educational program with the player safety coach component (PSC) versus coaching education only (EDU) by event type and mechanism of injury, 2015 season. aTime-loss injuries are those injuries that restrict participation for at least 24 hours.
Injury Rates
The 149 reported injuries were sustained during 25,938 AEs, leading to an overall injury rate of 5.74 per 1000 AEs (Table 2). The overall injury rate was lower in the PSC group than the EDU group (4.04 vs 7.56/1000 AEs; IRR, 0.53; 95% CI, 0.38-0.75).
Practice Rates
The 88 reported injuries during practices were sustained during 22,674 AEs in 372 practices (72 in the preseason), of which 179 (39 in the preseason) were in the PSC group and 193 (33 in the preseason) were in the EDU group. This led to a practice injury rate of 3.88 per 1000 AEs (Table 2). The practice injury rate was lower in the PSC group than the EDU group (2.99 vs 4.83/1000 AEs; IRR, 0.62; 95% CI, 0.40-0.95). When restricted to TL injuries only, the injury rate was still significantly lower in the PSC group (1.79 vs 3.10/1000 AEs; IRR, 0.58; 95% CI, 0.34-1.00). In addition, when restricted to concussions only, the IRR was also lower in the PSC group (0.09 vs 0.73/1000 AEs; IRR, 0.12; 95% CI, 0.01-0.94), although only 1 concussion was reported in the referent PSC group during practice.
Game Rates
The 61 reported injuries during games were sustained during 3264 AEs in 69 games, of which 30 were in the PSC group and 39 were in the EDU group. This led to a game injury rate of 18.69 per 1000 AEs (Table 2). The game injury rate was lower in the PSC group than in the EDU group (11.37 vs 26.37/1000 AEs; IRR, 0.43; 95% CI, 0.25-0.74). No statistically significant differences were found when restricted to TL injuries only (5.98 vs 9.42/1000 AEs; IRR, 0.64; 95% CI, 0.29-1.41) or concussions only (0.60 vs 4.39/1000 AEs; IRR, 0.14; 95% CI, 0.02-1.11).
Discussion
Effective strategies are needed to mitigate injury risk in football given that these injury rates are typically higher than most other sports.3,5,7,11 Reductions in injury rates and head impacts in practices have been found in youth football settings utilizing the HUF program.13,14 However, little research has been done at other levels of competition such as high school, where injury rates may be higher.4 In Indiana, SEA222 mandates that high school football coaches complete a football-specific coaching education course with material related to concussion awareness, equipment fitting, heat emergency preparedness, and proper technique.8 In response, some schools have implemented the HUF program, which satisfies all requirements and in addition includes the presence of a PSC. Our findings suggest that in the 2015 season, the use of the PSC was associated with lower injury rates than coaching education alone. As posited in the socioecological model,12 greater reductions in injury incidence may occur when addressing multiple levels of influence, as seen in those schools utilizing a PSC alongside coaching education.
Given that the HUF program focuses on practice settings where coaches instruct and enforce proper tackling and blocking skills, findings of lower practice injury rates among high schools utilizing the PSC component are promising. Furthermore, reductions were also found when restricted to TL injuries only. This, coupled with similar findings at the youth football level,13 suggests that the HUF program with the inclusion of the PSC component may be effective in reducing not just minor injuries in practices but also those with greater severity (eg, TL injuries that require athletes to miss at least 24 hours of participation). Nevertheless, given that only 3 high school football programs were utilized per group, it is essential for further research with larger samples to verify our findings. In addition, other states may not have such legislation requiring coaching education as seen in Indiana. Thus, such states may have varying “baseline” concussion education and implementation of injury prevention programming. Still, the value of such research allows for further examination of the potential added value of the HUF program, alone or with the inclusion of a PSC, in conjunction with already enacted policy.
Because the HUF program was primarily targeted at modifying practice activities, it was suspected that there would not be a difference in game injury rates between the PSC and EDU groups. However, the all-injury game injury rate was also lower in the PSC group than the EDU group. Players in the PSC group may have better form during tackling and blocking in games as well or may enter games in a healthier state because of a lower cumulative exposure to contact in practices, thus preventing more injuries. In youth football, players in leagues utilizing the HUF program including the PSC component sustained a lower number of head impacts in practices than players in leagues without the HUF program.13,14 However, the current study did not acquire head impact data. In addition, when restricted to TL injuries only, no differences were found in games between the PSC and EDU groups. This was probably due to the large proportion of game injuries being relatively minor (eg, contusions) and potentially not allowing for sufficient statistical power to detect differences among TL injuries only. At the same time, high schools in the EDU group played an average 3 more games in the 2015 season than those in the PSC group; however, injury incidence in later games was not higher than earlier games. Still, the effects of an intervention specific to 1 setting (eg, practices) on outcomes in another setting (eg, competitions) and cumulative injury risk have been seldom examined. Additional prospective research is warranted in the context of how policy and programming in practices may affect injury incidence in games and how injury risk varied within a season.
The concussion rate reported in the PSC group was lower than that in the EDU group, although this finding was only significant within practices. Because only 2 concussions were reported in the PSC group, the resulting concussion rates and rate ratios are imprecise. Thus, caution must be taken when interpreting findings. Interestingly, high school concussion rates from our study (4.39 and 0.73/1000 AEs in games and practices, respectively) were larger than those previously reported. Data from previous seasons (ranging from 2008-2014) reported rates ranging from 2.01 to 3.05 per 1000 AEs in games and 0.31 to 0.66 per 1000 AEs in practices.2,4,15 As posited by previous research,19 the increase in concussion is likely not due to increased incidence but rather an increase in reporting. The higher concussion rates in the EDU group may be the result of Indiana’s SEA222, which required coaching education regarding concussion recognition and management.8 Thus, it is possible that with such legislation, Indiana high schools may be currently identifying a larger proportion of the concussions that occur, and the HUF program is consequently reducing concussion risk. However, follow-up research is needed as our findings may not be generalizable to other Indiana high schools. Variations in our findings compared with previous research may also be attributable to differences such as location, contact guidelines, and reporting standards. Continued surveillance of concussions in high school athletes, as recommended by the IOM,9 will help to better estimate concussion incidence and the effects of policy and programming to reduce its incidence. In particular, such longitudinal examinations are needed to differentiate true reductions in concussion incidence from increased reporting.
The overall injury rate in both groups was lower than high school football injury rates previously reported across 163 team-seasons during the 2011-2012 through 2013-2014 academic years (4.04 and 7.56 vs 15.28/1000 AEs).5 These data might suggest that both coaching education such as the HUF Certification Course or the HUF program (HUF Certification Course plus the PSC component) are beneficial in reducing high school football injury rates. However, a longer period of data collection is needed to better ascertain such an association.
At the same time, additional studies estimating high school football injury rates in previous seasons1,2,18 utilized an injury definition of participation restriction of at least 24 hours, which is similar to our definition for TL injuries. Compared with our study’s EDU group, these previous investigations found greater TL injury rates in games (12.09-12.61 vs 9.42/1000 AEs) and lower TL injury rates in practices (2.18-2.54 vs 3.01/1000 AEs).1,2,18 The overall TL injury rate (games and practices combined) reported previously by NATION (3.35/1000 AEs) was lower than the overall TL injury rate for the non-HUF group (3.90/1000 AEs).5 These findings may be attributable to varying data collection methodologies or study periods. Continued surveillance will help to better estimate the incidence of and time trends related to high school football–related injuries.
Limitations
This is a single study of high school football teams, convenience-sampled from Indiana. Thus, findings may not be generalizable to other high school football teams in Indiana or the United States in general. Our study did not consider any additional policy and programming related to injury or concussion education and prevention, nor did we obtain information on additional potential covariates that may have been associated with injury reported and resulting injury rates, such as tenures, education levels, and years of experience for both coaches and ATs. In addition, although our study suggests the benefit of the PSC component, other aspects that were not addressed in the current study may contribute to the lower injury rates found. It is unclear whether the modification of any other single component alone (eg, player-to-player contact, proper equipment fitting) would result in similar findings. We also did not include a working definition of concussion, as we relied on the education and expertise of the ATs; nevertheless, it is possible that there may have been variation in concussion reporting. Last, although one of the aims of the HUF program is to reduce the incidence of injury, it is unknown how such programming may affect other factors that are important to football programs, such as win/loss records or player statistics; further examination would be beneficial to help minimize concerns of such programming affecting player and team performance. Given these limitations, we recommend that our study be replicated by other investigators using similar or improved methodologies.
Conclusion
Our findings may support the PSC as an effective mechanism of injury mitigation in high school football. This, coupled with findings at the youth level,13,14 may highlight the benefits of a comprehensive coach education program that includes a PSC, such as the HUF program. The HUF program is also feasible due to its low cost at approximately $10 per coach. However, future research should seek to replicate and improve this study using larger samples from additional states while considering additional covariates not in the current study (eg, coach and AT experience, education, and tenure at high school).
Acknowledgment
The authors thank the many youth football leagues’ organizers, parents, players, and athletic trainers, as this study would not be possible without their support.
Footnotes
One of more of the authors have declared the following potential conflict of interest or source of funding: Funding for this study was provided by USA Football. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the program sponsor.
References
- 1. Badgeley MA, McIlvain NM, Yard EE, Fields SK, Comstock RD. Epidemiology of 10,000 high school football injuries: patterns of injury by position played. J Phys Act Health. 2013;10:160–169. [DOI] [PubMed] [Google Scholar]
- 2. Comstock RD, Currie D, Pierpoint L. Convenience sample summary report: National High School Sports-Related Injury Surveillance Study: 2014-2015 school year. http://www.ucdenver.edu/academics/colleges/PublicHealth/research/ResearchProjects/piper/projects/RIO/Documents/Convenience%20Report_2014_15.pdf. Accessed February 1, 2016.
- 3. Comstock RD, Knox CL, Yard EE, Gilchrist J. Sports-related injuries among high school athletes—United States, 2005-06 school year. MMWR Morb Mortal Wkly Rep. 2006;55:1037–1040. [PubMed] [Google Scholar]
- 4. Dompier TP, Kerr ZY, Marshall SW, et al. Incidence of concussion during practice and games in youth, high school, and collegiate American football players. JAMA Pediatr. 2015;169:659–665. [DOI] [PubMed] [Google Scholar]
- 5. Dompier TP, Marshall SW, Kerr ZY, Hayden R. The National Athletic Treatment, Injury and Outcomes Network (NATION): methods of the surveillance program (SP), 2011-2012 through 2013-2014. J Athl Train. 2015;50:862–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fairfax County Public Schools. FCPS student concussion, injury prevention programs are producing positive results. http://commweb.fcps.edu/newsreleases/newsrelease.cfm?newsid=2838. Accessed February 1, 2016.
- 7. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42:311–319. [PMC free article] [PubMed] [Google Scholar]
- 8. Indiana General Assembly. Senate Enrolled Act No. 222. https://iga.in.gov/legislative/2014/bills/senate/222/. Accessed February 1, 2016.
- 9. Institute of Medicine. Sports-related concussions in youth: improving the science, changing the culture. http://www.iom.edu/∼/media/Files/Report%20Files/2013/Concussions/concussions-RB.pdf. Accessed February 1, 2016. [DOI] [PubMed]
- 10. Kerr ZY, Lynall RC, Mauntel TC, Dompier TP. High school football injury rates and services by athletic trainer employment status. J Athl Train. 2016;51:70–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kerr ZY, Marshall SW, Dompier TP, Corlette J, Klossner DA, Gilchrist J. College sports-related injuries—United States, 2009-10 through 2013-14 academic years. MMWR Morb Mortal Wkly Rep. 2015;64:1330–1336. [DOI] [PubMed] [Google Scholar]
- 12. Kerr ZY, Register-Mihalik JK, Marshall SW, Evenson KR, Mihalik JP, Guskiewicz KM. Disclosure and non-disclosure of concussion and concussion symptoms in athletes: review and application of the socio-ecological framework. Brain Inj. 2014;28:1009–1021. [DOI] [PubMed] [Google Scholar]
- 13. Kerr ZY, Yeargin SW, Valovich McLeod TC, et al. Comprehensive coach education and practice contact restriction guidelines result in lower injury rates in youth American football. Orthop J Sports Med. 2015;3:2325967115594578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kerr ZY, Yeargin SW, Valovich McLeod TC, Mensch J, Hayden R, Dompier TP. Comprehensive coach education reduces head impact exposure in American youth football. Orthop J Sports Med. 2015;3:2325967115610545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Marar M, McIlvain NM, Fields SK, Comstock RD. Epidemiology of concussions among United States high school athletes in 20 sports. Am J Sports Med. 2012;40:747–755. [DOI] [PubMed] [Google Scholar]
- 16. National Federation of High Schools. 2014-15 High School Athletics Participation Survey. http://www.nfhs.org/ParticipationStatistics/PDF/2014-15_Participation_Survey_Results.pdf. Accessed February 1, 2016.
- 17. National Federation of High Schools. Indiana Football SEA 222. https://nfhslearn.com/courses/35/indiana-football-sea-222. Accessed February 1, 2016.
- 18. Rechel JA, Yard EE, Comstock RD. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43:197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rosenthal JA, Foraker RE, Collins CL, Comstock RD. National high school athlete concussion rates from 2005-2006 to 2011-2012. Am J Sports Med. 2014;42:1710–1715. [DOI] [PubMed] [Google Scholar]
- 20. Shankar PR, Fields SK, Collins CL, Dick RW, Comstock RD. Epidemiology of high school and collegiate football injuries in the United States, 2005-2006. Am J Sports Med. 2007;35:1295–1303. [DOI] [PubMed] [Google Scholar]
- 21. Thackston L. Indiana first state with concussion-related law. http://fox59.com/2014/06/26/indiana-is-first-state-with-concussion-related-law/. Accessed February 1, 2016.
- 22. USA Football. Heads Up Football. http://usafootball.com/headsup. Accessed March 13, 2015.
- 23. Zuckerman SL, Kerr ZY, Yengo-Kahn A, Wasserman E, Covassin T, Solomon GS. Epidemiology of sports-related concussion in NCAA athletes from 2009-2010 to 2013-2014: incidence, recurrence, and mechanisms. Am J Sports Med. 2015;43:2654–2662. [DOI] [PubMed] [Google Scholar]