Abstract
Background and Aims:
High utilization and inappropriate usage of antimicrobial agents (AMAs) in an Intensive Care Unit (ICU) increases resistant organisms, morbidity, mortality, and treatment cost. Prescription audit and active feedback are a proven method to check the irrational prescription. Measuring drug utilization in DDD/100 bed-days is proposed by the WHO to analyze and compare the utilization of drugs. Data of AMAs utilization are required for planning an antibiotic policy and for follow-up of intervention strategies. Hence, in this study, we proposed to evaluate the utilization pattern and cost analysis of AMA used in the ICU.
Methodology:
A prospective observational study was conducted for 1 year from January 1, 2014, to December 31, 2014, and the data were obtained from the ICU of a tertiary care hospital. The demographic data, disease data, relevant investigation, the utilization of different classes of AMAs (WHO-ATC classification) as well as individual drugs and their costs were recorded.
Results:
One thousand eight hundred and sixty-two prescriptions of AMAs were recorded during the study period with an average of 1.73 ± 0.04 prescriptions/patient. About 80.4% patients were prescribed AMAs during admission. Ceftriaxone (22.77%) was the most commonly prescribed AMA followed by piperacillin/tazobactam (15.79%), metronidazole (12%), amoxicillin/clavulanic acid (6.44%), and azithromycin (4.34%). Ceftriaxone, piperacillin/tazobactam, metronidazole, and linezolid were the five maximally utilized AMAs with 38.52, 19.22, 14.34, 8.76, and 8.16 DDD/100 bed-days respectively. An average cost of AMAs used per patient was 2213 Indian rupees (INR).
Conclusion:
A high utilization of AMAs and a high cost of treatment were noticed which was comparable to other published data, though an increased use of newer AMAs such as linezolid, clindamycin, meropenem, colistin was noticed.
Keywords: Antimicrobial agents, cost analysis, DDD/ATC, drug utilization study, Intensive Care Unit
Introduction
Till date, about 5000 antimicrobial agents (AMAs) have been discovered, out of which only around 100 are used clinically for treating infection.[1] Unfortunately, as the need for new AMA has grown over time, development of novel drugs has been slow in the recent years. It seems likely that in coming decade we will have to depend on the currently available class of drugs. In view of continuing emergence of resistant pathogens, considerable effort will be needed to contain resistance development so as to maintain the effectiveness of available AMAs.
Critically ill patients admitted in Intensive Care Units (ICUs) are found to have a frequent infection and are more prone for developing new infections. AMAs are the most frequently prescribed drugs in the ICU.[2] Due to this, the total AMA consumption in ICU is approximately ten times higher than the general hospital wards.[3] As a result, AMAs used in ICU constitute a major part of the total hospital AMA consumption and cost.[4]
We can draw a plan for most effective empiric antibiotic treatment strategy by knowing of ICUs most common bacterial isolates with their antibiotic susceptibility patterns. It can also guide us to restrict the clinical availability of certain AMAs to maintain their effectiveness.[5] Every institution should have an antibiotic policy and guideline in place which should be based on local susceptibility pattern of pathogens. Guidelines could be unit specific or institutional-based and should be updated annually. Guidelines will help physicians to prescribe rationally and to choose the best effective, most appropriate empiric antibiotic for the patient. To form a guideline or for timely updation of guidelines and to check adherence to it, an audit of prescription or drug utilization studies are needed to be done.
In view of this, it was proposed to study the drug utilization patterns of AMAs and rationality of their use in the ICU of our institution that would help us to (a) determine the most commonly prescribed AMAs in the ICU of our institute (b) calculate average costs of AMAs prescribed.
Methodology
A prospective study was carried out in the general ICU of a Tertiary Care Hospital.
All patients admitted to the general ICU during the study period and who have given consent were included as the study population. Patients who were transferred to other specialty ICUs/wards from general ICU or discharged/death within 24 h of admission were excluded from the study.
Data were collected from patient's records. The following parameters were recorded:
Patient demographic profile
Mean length of stay (LOS) in ICU
Distribution of pattern of illness based on diagnosis
Associated comorbidities (other illness)
Percentage of oral/parenteral route of administration
-
Prescription frequency of individual AMAs:
- “Antimicrobial prescription”[6] means initiation of one AMA. For example, if a physician writes an order for gentamycin and amoxicillin-clavulanate, the patient will be considered to have received two prescriptions
Prescription frequency of class of AMAs (WHO-ATC classification)[7]
-
Utilization of AMAs in ICU presented as DDD/100 bed-days (WHO/DDD):[7]
- Formula for calculating DDD per 100 bed-days is:[8]
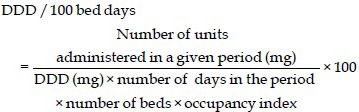
Number of beds in ICU = 14
Occupancy index for that period in our ICU was 0.85
The cost of AMAs utilized in ICU.
Data were collected in Microsoft Excel software and interpreted by applying descriptive analysis using IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.
Results
A total of 1076 patients were admitted in the ICU during the period under review, who met all the criteria to be included in the study. Of the total, 717 (66.6%) were males and 359 (33.4%) were females. The age of the patients in this study ranged from 18 to 98 years [Table 1]. The mean age of all the patients was 52.9 ± 16.9. The mean age of males and females was found to be 52.2 ± 16.5 and 54.4 ± 17.6, respectively. Patients were in ICU for days ranging from 2 to 26 days with an average of 4.0 ± 3 days. Five hundred and twenty-four patients admitted in ICU had comorbidities which were 48.9% of total admission [Tables 2 and 3]. Total and average number of AMAs prescribed, their frequency, and utilization are in Tables 4 and 5.
Table 1.
Distribution of patients according to age
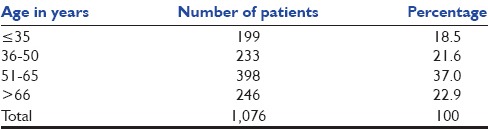
Table 2.
Frequency of comorbidity found in patients
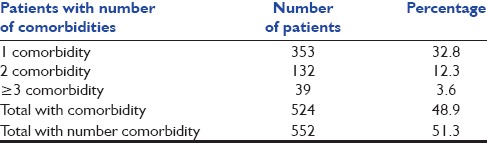
Table 3.
Number of patients with comorbidity
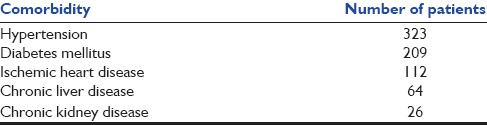
Table 4.
Number of antimicrobial agents prescribed per patient
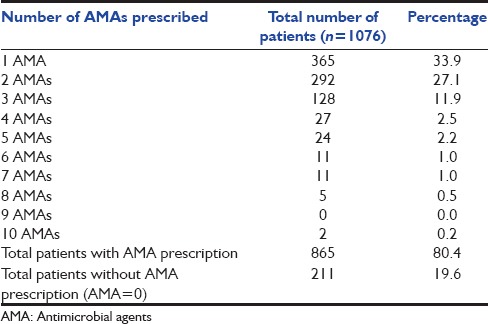
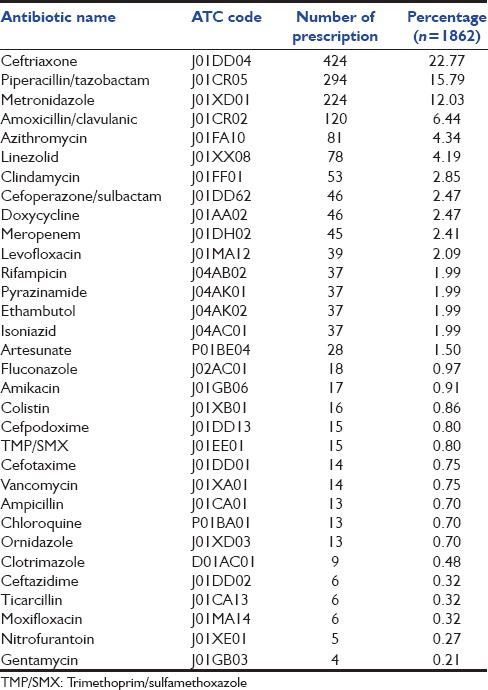
Table 5.
Prescription frequency of individual antimicrobial agents
Discussion
The demographic parameters of the patients revealed the number of males admitted in the ICU was almost double to that of female, and the mean age of patients was around 53 years which was nearly equal for both males and females. Studies done previously in Bengaluru in 2006,[9] Dehradun in 2012[10] and Pokhara, Nepal, in 2002[8] had shown a similar mean age of patients of around 50 years with minimal difference in the mean age of males and females. Male:female ratio was also found to be similar to that of the present study.[8,9,10,11] In contrast, a study done by Smythe et al. in Detroit showed an equal proportion of male and female admitted to the ICU with a mean age of 65 years.[12] These findings suggest that in Indian settings more males are admitted to the ICU. The most likely reason for this finding could be that in India male population has more access to medical facility compared to females, who even in critical illnesses are reluctant to utilize health care facilities, especially in those of lower socioeconomic strata. A maximum number of patients belonged to age group of 51–65 years which constitutes 37%. Sixty percent of patients were more than 50 years of age [Table 1]. This finding is similar to the results of studies done in Pokhara and Nagpur.[8,13]
Average LOS in ICU was found to be 4 ± 3 days in our study. In other studies done in ICUs of North India, South India, Nepal, and USA, average LOS in ICU was 5.75, 6.22, 4.0, and 5.2 days, respectively.[9,10,11] The difference found in the mean LOS could be due to the difference in illness pattern among the population.
Patients with a wide spectrum of clinical conditions were admitted, multiple, and complex diagnosis often observed. Respiratory infections, cerebrovascular accidents, septicemia, cardiovascular diseases, and febrile illnesses were among most commonly encountered medical conditions. About 50% of patients had comorbidity. Among them, 32% had more than one comorbidity [Table 2]. Hypertension was the most commonly found comorbidity followed by diabetes mellitus and ischemic heart disease [Table 3]. These findings were similar to the previous study done in Bengaluru.[9]
The ICU mortality rate was found to be 12%, whereas 4.9% discharged against medical advice. Our results are similar to the study done in Pokhara[8] where ICU mortality rate was 15.4% and in another study 3.8% patients were DAMA.[10] However, many Indian studies reported ICU mortality rate as high as around 35%.[9,10,14]
Prescription of antimicrobial agent (frequency)
In the prescription audit, the average number (mean) of drugs per prescription is a key indicator. It is recommended that for minimizing the risk of drug interactions, number of drugs per prescription should be kept low. It will also reduce hospital cost and development of bacterial resistance.[15] In our study, out of total 1076 patients, 211 (19.6%) patients did not receive AMA, whereas remaining 865 (80.4%) patients received one or more AMAs during their ICU admission period. A total 1862 AMAs prescribed during the whole study period, by taking average (mean) it comes to 1.73 AMAs per patient [Table 4]. In a similar study done in Dehradun, the average number of AMA per prescription was found to be 1.74.[10] Other studies support our finding with an average of 2.09 AMA per patient prescription.[14] Similar to our result, the Qatar study done in a medical ICU[16] reported 74% of admitted patients were treated with AMA and the Bengaluru study[9] reported 83% patients received AMA. However, our AMAs use frequency was inconsistent with some earlier studies done in Turkey[17] and Nepal[8] which reported 57.5% and 30% AMAs use, respectively. These variations were probably due to different geographic region of study and a different patient population. Out of all the patients who received AMAs in our study, 57.8% received more than one AMA. Bengaluru studyreported 69% of patients were prescribed more than one AMA.[9]
The most common AMA prescribed was ceftriaxone (22.77%). This is in accordance with the similar study by John et al. in Bengaluru[9] where ceftriaxone was prescribed in 23.8% patients. Five most common AMAs prescribed were piperacillin/tazobactam (15.79%), metronidazole (12.03%), amoxicillin/clavulanic acid (6.44%), and azithromycin (4.34%) beside ceftriaxone, all together they constitute 61% of total AMA prescriptions [Table 5]. In a study at CMC, Ludhiana,[14] the most commonly prescribed antibiotics in ICU were the 3rd generation cephalosporins, levofloxacin, and meropenem. Whereas, another study done at PGIMER Chandigarh,[11] cefotaxime, amoxicillin/clavulanic acid, cefepime, and ciprofloxacin were most commonly prescribed. On reviewing literature on more similar studies done in India, the most commonly prescribed AMAs in the ICU were amikacin, cefoperazone/sulbactam, cefuroxime, amoxicillin/clavulanic acid, and piperacillin/tazobactam.[9] Similarly, beta-lactams and fluoroquinolones were the most commonly prescribed antibiotics in ICU in a study done at Manipal, Karnataka,[18] whereas a study in Maharashtra,[19] the most commonly prescribed antibiotics in ICU were found to be tobramycin, cefuroxime, amikacin, cefoperazone/sulbactam, amoxicillin/clavulanic, and ceftriaxone. On reviewing similar studies around the world, we found a study done in ICU of Khyber Teaching Hospital, Peshawar, Pakistan,[20] the most commonly prescribed antibiotics were penicillin, 1st generation cephalosporins, and quinolones, whereas in a Brazilian study[21] cephalosporins, aminoglycosides, and fluoroquinolones were found to be most commonly prescribed in ICU.
When we look at the class of AMA prescribed cephalosporins and other beta-lactams (J01D) was maximally prescribed (30.13%) followed by penicillins (23.25%). Our finding is also supported by a study in done in Turkey,[17] which reported cephalosporin as the most commonly prescribed class contrary to a Nepal study,[8] which reported penicillins as the most common AMA drug class prescribed. Cephalosporins are frequently used due to a broader spectrum of activity and relatively lesser toxicity.
In our study, a fair number of utilization of newer AMAs were noticed such as linezolid (oxazolidinones) (4.19%), clindamycin (lincosamides) (2.85%), meropenem and imipenem (carbapenems) (2.57%), doxycycline (tetracycline) levofloxacin (quinolones) (2.09%), and vancomycin (glycopeptides) (0.75%) (2.47%). Similarly, utilization of newer AMAs was reported in the Bengaluru study.[9] It is observed that the patterns of the use of AMAs are different in private hospitals and the government hospitals. The factors for such differences are the time period in which the AMAs were used as well as the cost.
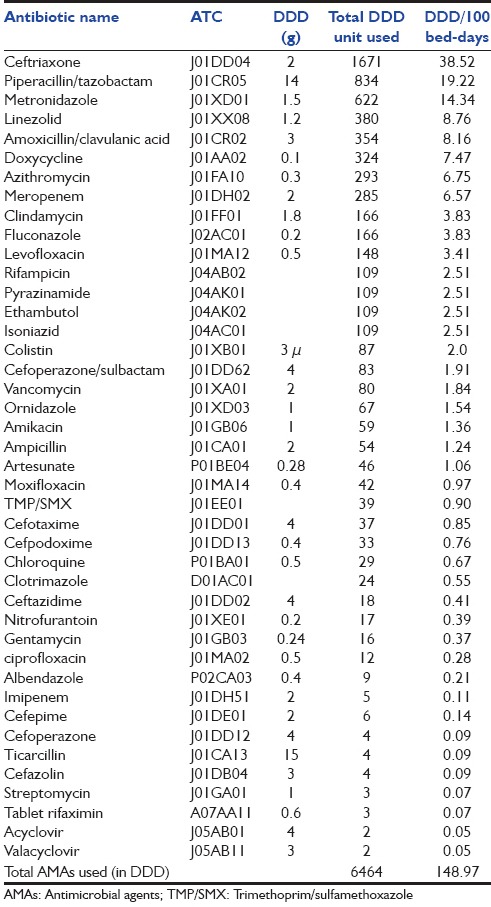
Utilization of antimicrobial agent (quantitatively in DDD)
The concept of ATC/DDD and drug utilization study based on DDD was brought by WHO.[7] Studies based on ATC/DDD are superior for comparing the use of drugs between hospitals or on regional levels. In our study, we analyzed AMA use pattern in DDD/100 bed-days [Table 5]. The utilization of AMAs in total was 148.97 DDD/100 bed-days. Our result is higher than a study done in Pokhara where utilization was 118.2/100 bed-days.[8] Higher utilization could be because Pokhara's study is 13-year-old. The same finding was observed in a Brazilian study where utilization of antibiotics had increased from 83.8 DDDs/100 bed-days in 1990 to 124.6 DDDs/100 bed-days in 1996.[22] In a study from Germany, antibiotic usage was calculated from 35 ICUs was found to be 133.7 DDD/100 bed-days.[23]
Five highly utilized (quantitatively) AMAs in our study were ceftriaxone, piperacillin/tazobactam, metronidazole, linezolid, and amoxicillin/clavulanic acid whose utilization were 38.52, 19.22, 14.34, 8.76, and 8.16 DDD/100 bed-days, respectively. On reviewing similar studies from India, we found five most utilized AMAs as the 3rd generation cephalosporins (18.48), meropenem (16.47), metronidazole (14.65), levofloxacin (15.97), and ceftriaxone (13.42).[14] In the Pokhara study use of penicillins, fluoroquinolones, 2nd and 3rd generation cephalosporins were 55.1, 5.34, 0.82, and 13.74 DDD/100 bed-days, respectively.[8]
Studies from Europe had reported a significant reduction in antibiotic utilization from 162.9 to 101.2 DDD/100 patient-days after introducing hospital antibiotic policy.[24] This observation highlights the importance of the antibiotic policy and also points out the need for regular scrutiny and modification of the policy.
Here, it can be noted that the frequency of prescriptions is the number of times the name of a drug is written, and utilization refers to the quantity of drug consumed.
Route of administration
In our study, 77% of prescribed AMAs were given parenterally and 23% by orally. This is comparatively similar to other studies.[8] Parenteral route of administration is preferred over oral because of better drug monitoring, quicker onset of action, and better bioavailability with the former.
Cost of antimicrobial agent
Increasing cost of medicines is causing a huge economic burden on patients who bear the cost of treatment in India. In view of this, we tried to calculate the average cost of AMAs per patient as well of individual AMAs used in our ICU setup. The total cost of all AMAs used throughout the study period was 238,145 Indian rupees (INR) which comes to 2213 INR per patient [Table 6]. Piperacillin/tazobactam constitute the major portion of the total cost of all AMAs used (30%). Top five AMAs utilized constitute 74% of total AMA cost. The next four most expensive AMAs utilized were meropenem (16%), linezolid (11%), ceftriaxone (9%), and colistin (8%). On reviewing other studies from India, we found total AMA cost per patient varied from 4364 to 1995 INR.[10] Meropenem with 34.7% of total AMA cost was the most expensive AMA utilized. The study in Pokhara reported 1958 INR per patient cost of AMA in ICU.[8]
Table 6.
Utilization of antimicrobial agents in Intensive Care Unit presented as DDD/100 bed-days
Comparisons of AMA utilization cost globally could be misleading because of the huge variations in the pricing of drugs. However, on reviewing data on cost analysis from developed countries, it is found that ICU AMAs costs per patient-day varied from $208 to $312.[25] A study from Turkey reported AMA cost per patient-day in ICU as $89.64 and meropenem as the most costly drug used.[17]
Recommendations
First, to improve judicious use of AMAs, institution-specific AMA policy, and protocols should be made. To increase adherence with protocol, training of prescriber, regular audit with active feedback should be implemented. Through longitudinal surveillance of AMAs use, a database can be created to compare the trends in the utilization of AMAs.
Antibiotic stewardship program could be implemented to reduce the AMA use; under this, some easy to use strategies are antibiotic restriction and antibiotic cycling. Finally, the inclusion of clinical pharmacologist and microbiologist in the management team could prove helpful inappropriate prescription of AMAs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Khardori N. Antibiotics – Past, present, and future. Med Clin North Am. 2006;90:1049–76. doi: 10.1016/j.mcna.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Krivoy N, El-Ahal WA, Bar-Lavie Y, Haddad S. Antibiotic prescription and cost patterns in a general intensive care unit. Pharm Pract (Granada) 2007;5:67–73. doi: 10.4321/s1886-36552007000200003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Røder BL, Nielsen SL, Magnussen P, Engquist A, Frimodt-Møller N. Antibiotic usage in an intensive care unit in a Danish University Hospital. J Antimicrob Chemother. 1993;32:633–42. doi: 10.1093/jac/32.4.633. [DOI] [PubMed] [Google Scholar]
- 4.Marschner JP, Thürmann P, Harder S, Rietbrock N. Drug utilization review on a surgical intensive care unit. Int J Clin Pharmacol Ther. 1994;32:447–51. [PubMed] [Google Scholar]
- 5.Dukes MN. Drug utilization studies. Methods and uses. Introduction. WHO Reg Publ Eur Ser. 1993;45:1–4. [PubMed] [Google Scholar]
- 6.Bergmans DC, Bonten MJ, Gaillard CA, van Tiel FH, van der Geest S, de Leeuw PW, et al. Indications for antibiotic use in ICU patients: A one-year prospective surveillance. J Antimicrob Chemother. 1997;39:527–35. doi: 10.1093/jac/39.4.527. [DOI] [PubMed] [Google Scholar]
- 7.WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC Classification and DDD Assignment. 2013. [Last accessed 2015 Sep 11]. pp. 1–284. Available from: http://www.whocc.no/filearchive/publications/1_2013guidelines.pdf .
- 8.Shankar PR, Partha P, Dubey AK, Mishra P, Deshpande VY. Intensive care unit drug utilization in a teaching Hospital in Nepal. Kathmandu Univ Med J (KUMJ) 2005;3:130–7. [PubMed] [Google Scholar]
- 9.John LJ, Devi P, John J, Guido S. Drug utilization study of antimicrobial agents in medical intensive care unit of a tertuart care hospital. Asian J Pharm Clin Res. 2011;4:81–4. [Google Scholar]
- 10.Amit GS. Drug use evaluation study in a tertiary care corporate hospital with special reference to use of antibiotics in ICU department. Int J Adv Pharm Biol Chem. 2013;2:179–89. [Google Scholar]
- 11.Biswal S, Mishra P, Malhotra S, Puri GD, Pandhi P. Drug utilization pattern in the intensive care unit of a tertiary care hospital. J Clin Pharmacol. 2006;46:945–51. doi: 10.1177/0091270006289845. [DOI] [PubMed] [Google Scholar]
- 12.Smythe MA, Melendy S, Jahns B, Dmuchowski C. An exploratory analysis of medication utilization in a medical intensive care unit. Crit Care Med. 1993;21:1319–23. doi: 10.1097/00003246-199309000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Badar VA, Navale SB. Study of prescribing pattern of antimicrobial agents in medicine intensive care unit of a teaching hospital in Central India. J Assoc Physicians India. 2012;60:20–3. [PubMed] [Google Scholar]
- 14.Williams A, Mathai AS, Phillips AS. Antibiotic prescription patterns at admission into a tertiary level intensive care unit in Northern India. J Pharm Bioallied Sci. 2011;3:531–6. doi: 10.4103/0975-7406.90108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stratton CW, 4th, Ratner H, Johnston PE, Schaffner W. Focused microbiologic surveillance by specific hospital unit: Practical application and clinical utility. Clin Ther. 1993;15(Suppl A):12–20. [PubMed] [Google Scholar]
- 16.Hanssens Y, Ismaeil BB, Kamha AA, Elshafie SS, Adheir FS, Saleh TM, et al. Antibiotic prescribing pattern in a medical intensive care unit in Qatar. Saudi Med J. 2005;26:1269–76. [PubMed] [Google Scholar]
- 17.Usluer G, Ozgunes I, Leblebicioglu H Turkish Antibiotic Utilization Study Group. A multicenter point-prevalence study: Antimicrobial prescription frequencies in hospitalized patients in Turkey. Ann Clin Microbiol Antimicrob. 2005;4:16. doi: 10.1186/1476-0711-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adiga MN, Alwar MC, Pai MR, Adiga US. Pattern of antimicrobial agents use in hospital deliveries: A prospective comparative study. [Last accessed 2015 Oct 12];Online J Health Allied Sci. 2009 8:10. Available from: http://www.ojhas.org/issue32/2009-4-10.htm . [Google Scholar]
- 19.Patil PH, Kuchake VG, Ajay K, Pitambar D, Surana S. Evaluation of drug utilization especially antimicrobial agent pattern in tertiary care unit hospital. Int J Community Pharm. 2009;2:13–23. [Google Scholar]
- 20.Farooqi R, Afridi M, Farooqi J. Use of antibiotics in hospitalized adult patients: An experience from NWFP. Rawal Med J. 2005;30:16–8. [Google Scholar]
- 21.Fonseca LG, de Oliveira Conterno L. Audit of antibiotic use in a Brazilian University Hospital. Braz J Infect Dis. 2004;8:272–80. doi: 10.1590/s1413-86702004000400002. [DOI] [PubMed] [Google Scholar]
- 22.de Castro MS, Pilger D, Ferreira MB, Kopittke L. Trends in antimicrobial utilization in a University Hospital, 1990-1996. Rev Saude Publica. 2002;36:553–8. doi: 10.1590/s0034-89102002000600003. [DOI] [PubMed] [Google Scholar]
- 23.Meyer E, Jonas D, Schwab F, Rueden H, Gastmeier P, Daschner FD. Design of a surveillance system of antibiotic use and bacterial resistance in German intensive care units (SARI) Infection. 2003;31:208–15. doi: 10.1007/s15010-003-3201-7. [DOI] [PubMed] [Google Scholar]
- 24.Peto Z, Benko R, Matuz M, Csullog E, Molnar A, Hajdu E. Results of a local antibiotic management program on antibiotic use in a tertiary intensive care unit in Hungary. Infection. 2008;36:560–4. doi: 10.1007/s15010-008-7377-8. [DOI] [PubMed] [Google Scholar]
- 25.Weber RJ, Kane SL, Oriolo VA, Saul M, Skledar SJ, Dasta JF. Impact of intensive care unit (ICU) drug use on hospital costs: A descriptive analysis, with recommendations for optimizing ICU pharmacotherapy. Crit Care Med. 2003;31(1 Suppl):S17–24. doi: 10.1097/00003246-200301001-00003. [DOI] [PubMed] [Google Scholar]


