Abstract
Background:
Pediatric Intensive Care Unit (PICU) patients are often prescribed antibiotics with a low threshold in comparison to patients elsewhere. Irrational antibiotics use can lead to rapid emergence of drug resistance, so surveillance of their use is important.
Objectives:
To evaluate the use of antibiotics in relation to bacteriological findings in PICU of a Tertiary Hospital.
Methods:
Retrospective review of medical records of all children (age 1 month–16 years) admitted in our closed multidisciplinary-cardiothoracic PICU from January to June 2013 was performed, after approval from Ethical Review Committee. For each antibiotic, indication (prophylactic, empiric, therapeutic) and duration of use were recorded. All diagnoses of infections were recorded according to diagnostic criteria of IPSCC 2005. Results are presented as frequency and percentages and median with inter quartile range using SPSS version 19.
Results:
All of the total 240 patients admitted in PICU during the study period received antibiotics: 43% (n = 104) prophylactically, 42% (n = 102) empirically, and 15% (n = 15) therapeutically. Median number of antibiotic use per patient in PICU was 3, with range of 1–7. 25% received 1 antibiotic, 23% received 2 antibiotics, 29% received 3 antibiotics, and rest received ≥4 antibiotics. Most commonly used antibiotics were cefazolin, meropenem, vancomycin and ceftriaxone, and most frequently used combination was meropenem and vancomycin. In majority of the cases, (70%) empiric antibiotic combinations were stopped in 72 h.
Conclusion:
This is the first report of antibiotics use in PICU from our country, which shows that antibiotics are prescribed universally in our PICU. Strategies to assess the need for antibiotic use are needed.
Keywords: Antibiotic use, developing country, infection, Pediatric Intensive Care Unit
Introduction
Children admitted to Pediatric Intensive Care Unit (PICU) have life threatening illnesses. They either already have infection when admitted or are at high-risk of acquiring infections because of different procedures, use of invasive devices, and extended length of stay.[1] These are the known risk factors for acquiring health care associated infections (HAIs) which can be quite difficult to treat but are preventable to an extent.[2] HAIs have been reported to be in 16–23% of patients admitted in PICUs.[3,4] Antibiotics are the most commonly used medicines in the Intensive Care Units (ICUs).[5] The critical nature of the illness of patients admitted to PICU and the high-risk of developing HAIs often leads to the prescription of multiple and prolonged antibiotics. The use of antibiotics may be helpful in preventing HAIs, but their unnecessary and irrational use has a few serious disadvantages. Prolonged and inappropriate use of antibiotics has resulted in emergence of antibiotic resistance which is an important clinical, economic, and public health problem.[6] Several papers have been published regarding the use of antibiotics both in adult and pediatric critically ill patients from developed countries.[1,2,6,7] They showed that they were able to identify reasons for not using antibiotics in many patients. This kind of surveillance leads to antibiotic stewardship program and proper use. However, availability of such data is limited from PICU of developing country specially ours. The objective of this study is to evaluate the use of antibiotic in relation to diagnosis and bacteriological findings in the PICU of a tertiary hospital. This would help in instituting strategies to prevent inappropriate use hence improving the outcome and reduce cost.
Methods
We reviewed medical records of all children (age -1 month–16 years) admitted in our closed multidisciplinary-cardiothoracic PICU from January to June 2013 after Ethical Review Committee approval. Data collected included demographic variables (age, gender), clinical, laboratory, microbiological data, and use of antibiotics on a structured data collection sheet. For each patient the cumulative number of antibiotics prescribed during the length of stay in PICU was recorded. All diagnosis of infections was recorded according to the diagnostic criteria of IPSCC 2005. The indications of antibiotics were categorized as prophylaxis, empirical, and therapeutics. Prophylactic antibiotic treatment was defined as administration of antibiotics without any evidence of infection to prevent infection in patients at risk of developing infection mainly in postoperative patients. Empiric antibiotic treatment was labeled to be present when antibiotics were prescribed for systemic signs of infection without identifying a specific source of infection. Therapeutic antibiotic treatment was defined as treatment based on culture and sensitivity report. For each antimicrobial, the indication and duration of antibiotics were recorded. The indication for use of each antibiotic prescribed during the PICU stay was documented using above criteria. Descriptive statistics were applied using SPSS (Statistical Package for Social Sciences) version 19. Data are present as frequency with percentage and median with inter quartile range (IQR).
Results
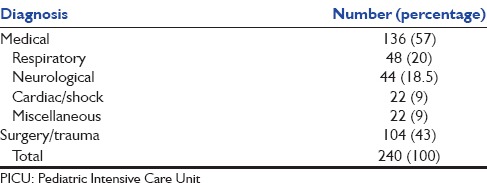
During the study period, 240 patients were admitted to PICU. Baseline characteristics of enrolled patients are described in Table 1. The median age of our sample was 26 months with IQR of 93 and 150 (62.5%) were male. The most common diagnostic categories were postoperative congenital heart diseases (35%), acute neurological disorders including central nervous system infections (26.6%) followed by respiratory problems (14.6%) [Table 2].
Table 1.
Basic characteristics of patients admitted in PICU who received Antibiotics
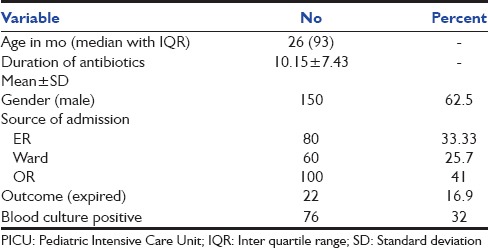
Table 2.
Diagnostic categories of patients who received antibiotics in PICU
Antibiotics surveillance data
All patients (100%) admitted to our ICU received antibiotics. Prophylactic therapy (three doses as per our hospital policy) was used in 103/240 cases (43%) prior to surgical procedures. Empirical therapy was used in 42% (101/240) while 15% (36/240) received antibiotics therapeutically.
The median number of antibiotics received per patient in our PICU was 3 with a range of 1–7 (IQR 2), 25% (n = 60) received one antibiotic, 23% (n = 56) received two antibiotics, 29% (n = 70) received three antibiotics, rest received ≥4 antibiotics in our cohort [Figure 1]. >1 antibiotic either as a combination or sequential therapy was prescribed in 76% of the patients.
Figure 1.
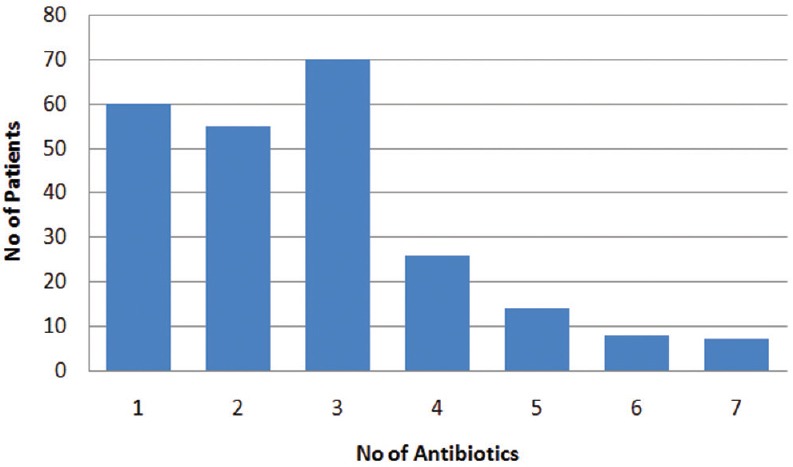
No of antibiotics per patient
The most commonly used drugs were cefazolin, meropenem, vancomycin, and ceftriaxone, [Figure 2]. The most frequently used combinations included meropenem and vancomycin (24%, n = 58/240) and meropenem, vancomycin, and colistin (12%; 28/240). Of those who received empiric therapy, 33% of patients received combination antibiotics. Combination therapy with meropenem and vancomycin as prophylaxis after surgical repair or replacement of cardiac valves was prescribed to three patients. The median duration of antibiotic use was 4 days with IQR of 2 days, and median PICU length of stay was 4 days with IQR of 3 days. The median duration of antibiotics use for prophylactic therapy was 1 day with IQR of 2. The median duration of empirical therapy was 1 day with IQR of 4 days. The empirical therapy was deescalated after 72 h in 70% (n = 72). Failure to discontinue accounted for 15% of all cases in whom culture report was negative; prolonged empiric treatment was continued (5–7 days) as therapeutic in 15% (n = 15) as the culture sensitivity report showed that organism is sensitive to the drug prescribed empirically. Therapeutic use of antibiotics was 15%.
Figure 2.
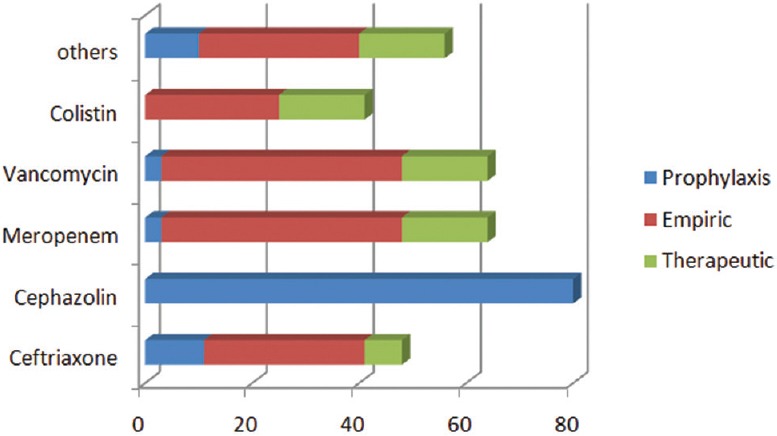
Most commonly used antibiotics and their indication
A total of 280 blood cultures, 50 tracheal aspirates sample, and 32 urine samples were sent for analysis during study period and 55 micro-organisms were isolated from 362 specimens of 140 patients who had one or more specimens cultured during study period. The blood cultures were positive in 14%, and tracheal aspirates were positive in 24%. Most common isolates in blood were Acinetobacter, Staphylococcus and Klebsiella pneumonia (KP). Tracheal cultures most commonly yielded Acinetobacter and KP. Rate of MDR was 7% in our cohort, and the most common isolates were Acinetobacter and KP. Overall, 22/240 (9%) patients died during the study period.
Discussion
Good antibiotics prescribing practice means using most effective, least toxic, and least costly antibiotic for a precise duration.[8] Our study highlights some very important points. The entire patient population (100%) received antibiotics as prophylaxis or empirical therapy mostly without always having evidence of any infection as compared to other studies that reported antibiotic usage of 50–94% in their PICUs.[1,2,9] In our study, 76% patients received combination or multiple antibiotics therapy (2 or more drugs). These findings are concerning since our MDRO rate, and mortality is high and all of our patients receive antibiotics whether indicated or not. Our study shows that empirical therapy was prescribed to the majority (42%) of the patients without any microbiologic evidence of infection. This might have been due to the reason of limited microbiologic yield and the critical condition of the patients admitted to PICU. A similar study of antibiotic use in PICU of Canada showed 27–40% usage of empiric antibiotic treatment[2] while another study by Ding et al. from China showed that 71% of their patients in PICU received empiric antibiotic treatment.[1] Failure to stop empirical therapy was found in 15% of the patients with no micro-organisms isolated which is similar to a study in Canada.[2]
In our study, 76% patients received more than two antibiotics simultaneously which is much higher than reported by Ding et al., Blinova et al. and Grohskopf et al.[1,2,10] They reported use of two or more antibiotics in 47%, 55–69%, and 40% of their patients, respectively. These variations can be due to difference in prescribing practices, differences in rates and types of infections and antibiotic guidelines among countries but such a high rate of combination therapy cannot be justified except in certain conditions, like in very critical patients, with the purpose of providing broad coverage against micro-organisms or when more than one organism is isolated.
Prophylaxis was given in 43% of patients for 1 day which was prescribed for the postoperative patient, the majority (35%) of whom were postoperative congenital heart diseases. Most common prophylactic antibiotic prescribed was cephazolin which is the standard prophylactic antibiotic being used in these patient.
Another alarming finding is increased use of carbapenems (meropenem) which was found to be the most commonly used drug after cephazolin, mostly in combination with vancomycin. In contrast, other studies by Ding et al. and Blinova et al. report use of meropenem to be 2.5–12.5% respectively.[2,6] Other commonly used drugs were ceftriaxone and cephazolin, similar to other studies.[2,7] However, our use of broad spectrum combination therapy for suspected nosocomial infections was very high as compared to other studies.[1,2] Several different strategies can be developed to reduce the antibiotic use including hospital formulary restriction, practitioners’ education and feedback activities and teaming up with an infectious disease specialist, microbiologist, and clinical pharmacist.[10]
Our study has the limitation of being a retrospective review, single center study, and PRISM score was not calculated. None the less this adds much value to the scarce data available on antibiotic use in our country especially in a dedicated PICU which can be used to guide proper antibiotic use by different interventions mentioned above.
Conclusion
This study provides valuable insight to antibiotics usage in PICU of a developing country. Our data points that overuse of antibiotics exists in our PICU. It is recommended to guide antibiotics utilization according to microbiology and discontinue empirical therapy as soon as possible. Continued surveillance and large, multicenter studies are recommended.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ding H, Yang Y, Chen Y, Wang Y, Fan S, Shen X. Antimicrobial usage in paediatric intensive care units in China. Acta Paediatr. 2008;97:100–4. doi: 10.1111/j.1651-2227.2007.00580.x. [DOI] [PubMed] [Google Scholar]
- 2.Blinova E, Lau E, Bitnun A, Cox P, Schwartz S, Atenafu E, et al. Point prevalence survey of antimicrobial utilization in the cardiac and pediatric critical care unit. Pediatr Crit Care Med. 2013;14:e280–8. doi: 10.1097/PCC.0b013e31828a846d. [DOI] [PubMed] [Google Scholar]
- 3.Joram N, de Saint Blanquat L, Stamm D, Launay E, Gras-Le Guen C. Healthcare-associated infection prevention in pediatric intensive care units: A review. Eur J Clin Microbiol Infect Dis. 2012;31:2481–90. doi: 10.1007/s10096-012-1611-0. [DOI] [PubMed] [Google Scholar]
- 4.Urrea M, Pons M, Serra M, Latorre C, Palomeque A. Prospective incidence study of nosocomial infections in a pediatric intensive care unit. Pediatr Infect Dis J. 2003;22:490–4. doi: 10.1097/01.inf.0000069758.00079.d3. [DOI] [PubMed] [Google Scholar]
- 5.van Houten MA, Luinge K, Laseur M, Kimpen JL. Antibiotic utilisation for hospitalised paediatric patients. Int J Antimicrob Agents. 1998;10:161–4. doi: 10.1016/s0924-8579(98)00022-3. [DOI] [PubMed] [Google Scholar]
- 6.Ding H, Yang Y, Lu Q, Wang Y, Chen Y, Deng L, et al. Five-year surveillance of antimicrobial use in Chinese Pediatric Intensive Care Units. J Trop Pediatr. 2008;54:238–42. doi: 10.1093/tropej/fmm118. [DOI] [PubMed] [Google Scholar]
- 7.Stocker M, Ferrao E, Banya W, Cheong J, Macrae D, Furck A. Antibiotic surveillance on a paediatric intensive care unit: Easy attainable strategy at low costs and resources. BMC Pediatr. 2012;12:196. doi: 10.1186/1471-2431-12-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ceyhan M, Yildirim I, Ecevit C, Aydogan A, Ornek A, Salman N, et al. Inappropriate antimicrobial use in Turkish pediatric hospitals: A multicenter point prevalence survey. Int J Infect Dis. 2010;14:e55–61. doi: 10.1016/j.ijid.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 9.Ding H, Yang Y, Wei J, Fan S, Yu S, Yao K, et al. Influencing the use of antibiotics in a Chinese pediatric intensive care unit. Pharm World Sci. 2008;30:787–93. doi: 10.1007/s11096-008-9220-9. [DOI] [PubMed] [Google Scholar]
- 10.Grohskopf LA, Sinkowitz-Cochran RL, Garrett DO, Sohn AH, Levine GL, Siegel JD, et al. A national point-prevalence survey of pediatric intensive care unit-acquired infections in the United States. J Pediatr. 2002;140:432–8. doi: 10.1067/mpd.2002.122499. [DOI] [PubMed] [Google Scholar]


