How does cancer immunotherapy work?
We think that cancer immunotherapy works by generating an antigen-specific immune response against a target antigen. The first therapeutic cancer vaccine to be approved by the US Food and Drug Administration was sipuleucel-T (Provenge, Dendreon). Sipuleucel-T is a personalized, cell-based vaccine generated from a patient’s own peripheral blood monocytes. It works by targeting the antigen prostatic acid phosphatase (PAP), which is expressed on prostate cancer cells—Dr Philip Kantoff showed this in a 2010 article in the New England Journal of Medicine. PAP is an excellent vaccine target because it is highly specific to prostate cancer, and approximately 90% to 95% of late-stage prostate tumors express it.
What exactly is antigen spread?
Antigen spread was recognized quite some time ago, and it has been examined in both animal models and in patients. When an immune response begins, it generally focuses on a single target. For example, in an autoimmune disease such as rheumatoid arthritis, the body may start by attacking a specific protein in the joint. What happens next is that as joint tissue breaks down in this proinflammatory environment, additional proteins become exposed. The immune system then recognizes and attacks these additional antigens, which may cause even more proteins to become exposed. As the response continues and broadens, it becomes increasingly difficult to halt. Although this broadening of the body’s immune response can be devastating in autoimmune diseases, it is exactly what we would like to see in cancer immunotherapy.
The presence of antigen spread after immunotherapy has been examined in only a handful of studies. One important study involves a vaccine against prostate-specific antigen called Prostvac, which is in development at the National Institutes of Health. In a small group of patients, Dr James Gulley and his colleagues showed that using the vaccine in combination with radiation therapy caused an immune response to a number of prostate antigens (the article appeared in Clinical Cancer Research with Nesslinger as the first author). This same vaccine, which is now being tested in a phase 3 trial, also showed some evidence for improved survival in an earlier phase 2 trial published in the Journal of Clinical Oncology, with Kantoff as the lead author.
Could you talk a little bit more about antigen spread and how it applies to sipuleucel-T?
Sipuleucel-T targets PAP, which, as mentioned earlier, is an excellent target for a prostate cancer vaccine. To get more immune pressure against the tumor, however, we would like to see the immune system recognize additional tumor-associated proteins as antigens. It would be useful if the breakdown of certain tumor cells would lead to the recognition of other proteins by the immune system. The question is, does the immune system make new antibodies against anything else in response to sipuleucel-T?
We are able to look at far more antibodies than ever before—approximately 9000 different types at once—thanks to new technology that allows us to identify and validate serum immunoglobulin G responses to secondary antigens after treatment.
Based on data from the phase 3 IMPACT (Immunotherapy for Prostate Adenocarcinoma Treatment Study) trial that was conducted by a group of coinvestigators, we evaluated humoral antigen spread after sipuleucel-T treatment in patients with metastatic castration-resistant prostate cancer. In addition, we validated a subset of these serum immunoglobulin G responses in patients from the ProACT (Prostate Active Cellular Therapy) study. We presented our results at the 2014 American Society of Clinical Oncology Genitourinary Cancers Symposium. We found that 38% of the patients given sipuleucel-T made antibodies to ERAS, 27% made antibodies to KLK2, and 27% made antibodies to KRAS. It was very clear that this antigen spread occurred only in the patients who got vaccinated—it did not occur in any of the control patients.
Could you talk more about this study, including the tests you used to look for antigen spread?
We used a 2-step process to test for antibodies. The first step employed a chip called a high-content protein microarray platform (ProtoArray, Life Technologies Corporation) that contains 9000 kinds of proteins. In basic terms, we placed a small amount of the patient’s serum onto the chip, washed it, and observed whether any areas of the chip were bound by antibodies in the patient’s serum. Each patient’s serum was tested before treatment, and again at week 6, week 14, and week 26. The 10 proteins we found were KRAS, ERAS, KLK2, LGALS8, TSPAN13, LGALS3, ECE1, ANPEP, CACNG1, and FBXO6.
After we knew which proteins each patient had an antibody response to, we confirmed our results using an enzyme-linked immunosorbent assay (ELISA) via the Luminex xMAP technology (Luminex Corporation). We wound up with data on 93 patients who were treated with sipuleucel-T and 40 placebo patients, which was a fair number of patients. The data are overall quite consistent with the notion that antigen spread does occur with sipuleucel-T.
Finally, we wanted to know whether antibody response had a correlation with survival—that was an especially interesting part of the study. We were surprised to learn that although sipuleucel-T is a vaccine against PAP, the presence of antibodies to PAP did not have a statistically significant correlation with survival.
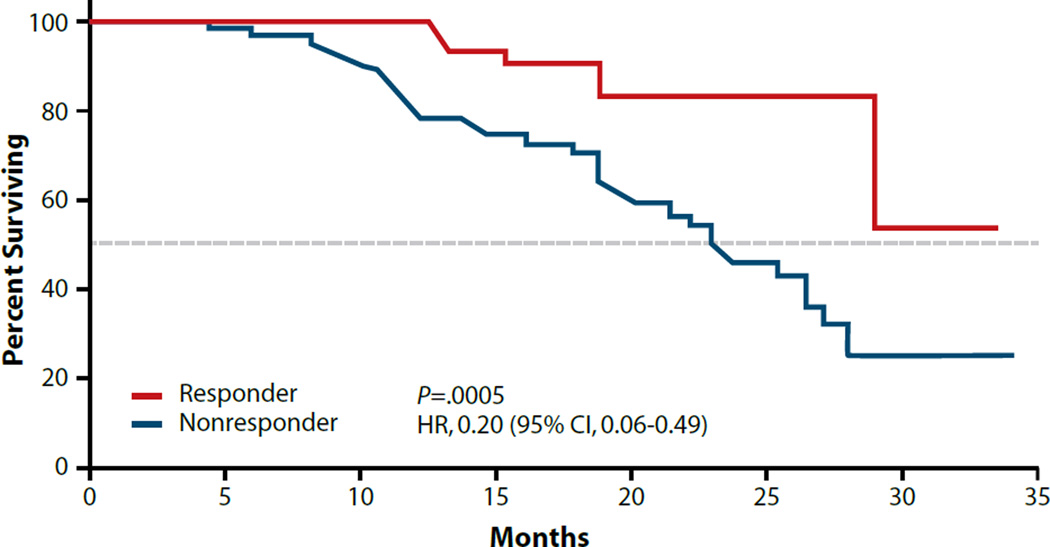
The most intriguing observation was that when patients had antibodies to PAP plus 2 other proteins, we did see a correlation with survival: the hazard ratio was a striking 0.35 and the P-value was .0058. What was even more impressive was that the patients who responded to PAP plus 3 other proteins had an even stronger correlation with survival than those who responded to PAP plus 2 other proteins—the hazard ratio was 0.20, which is impressive, and the P-value was .0005 (see the figure).
Figure.
In an analysis of data from the phase 3 IMPACT trial of sipuleucel-T, improved overall survival was seen in patients who showed an immunoglobulin G response to the primary antigen and any 3 secondary antigens.
IMPACT, Immunotherapy Prostate Adenocarcinoma Treatment.
Adapted from Drake CG et al. ASCO GU abstract 88. J Clin Oncol. 2014;32(4)(suppl).
Of course, these are retrospective data, so they can only be considered hypothesis-generating. I cannot say that enough. Prospective studies need to be conducted in which we treat patients with sipuleucel-T or standard of care and see if antigen response correlates with outcome.
What are the benefits of knowing whether antigen spread has occurred?
When we treat patients with sipuleucel-T, the PSA level usually does not decrease and we are left wondering whether the drug worked. That is the same as with many other cancer agents. For example, when we treat women with adjuvant chemotherapy after surgery for breast cancer, all we know is that we are reducing the risk of a recurrence—not whether the agent is working in that particular patient.
Having this additional information about sipuleucel-T has the potential to allow us to tell patients whether the drug is working for them. Whether that is of much value clinically is hard to say. Sipuleucel-T is not approved for retreatment, but if we were allowed to provide a second dose, I could certainly see doing that in the case of a patient who had an antibody response to 4 antigens. It would be like a booster shot. We give boosters of vaccines for tetanus and hepatitis B, so why not for cancer?
What would be of greatest value based on this type of study would be the development of immunotherapies that target some of these additional antigens: not just PAP, but perhaps KRAS, ERAS, KLK2, and others. Just like the pneumococcal vaccine contains 13 or 23 antigens, a future prostate cancer vaccine might contain multiple antigens.
Is antigen spread being studied in relation to other types of cancer besides prostate cancer?
Now that we have these high-density protein arrays, we have the ability to start doing this for other types of cancer. It is expensive, but relatively simple to do. Our group here at Johns Hopkins is looking at antigen spread related to cell-based vaccines for breast cancer and pancreatic cancer. I am also going to be doing research on a different kind of prostate cancer vaccine that is designed to work in an earlier setting. A group led by Dr Bernard Fox at the Earle A. Chiles Research Institute in Portland, Oregon, is looking at this in prostate cancer as well.
Is there anything you would like to add?
I would just like to say that these data on the sipuleucel-T product and cancer vaccines in general are quite exciting to me. These new studies appear to be giving us a nice window into how these approaches work in patients, which has the potential to help us to choose the best antigen targets for a new generation of cancer vaccines.
Biography

Suggested Readings
- Drake CG, Fan LQ, GuhaThakurta DG, et al. Antigen spread and survival with sipuleucel-T in patients with advanced prostate cancer [ASCO GU abstract 88] J Clin Oncol. 2014;32((4)(suppl)) [Google Scholar]
- Kantoff PW, Higano CS, Shore ND, et al. IMPACT Study Investigators. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363(5):411–422. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- Kantoff PW, Schuetz TJ, Blumenstein BA, et al. Overall survival analysis of a phase II randomized controlled trial of a Poxviral-based PSA-targeted immunotherapy in metastatic castration-resistant prostate cancer. J Clin Oncol. 2010;28(7):1099–1105. doi: 10.1200/JCO.2009.25.0597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nesslinger NJ, Ng A, Tsang KY, et al. A viral vaccine encoding prostate-specific antigen induces antigen spreading to a common set of self-proteins in prostate cancer patients. Clin Cancer Res. 2010;16(15):4046–4056. doi: 10.1158/1078-0432.CCR-10-0948. [DOI] [PMC free article] [PubMed] [Google Scholar]