Abstract
Emerging data suggest that type 1 diabetes is a more aggressive disease in children than in adults, with important differences in pathophysiology and clinical course. Therefore, the efficacy of disease-modifying therapies may be different in the two populations. Understanding the developmental and regulatory pathways for type 1 diabetes–modifying therapies in children will enable industry, academia, funders, advocacy groups, and regulators to translate new science to clinical care. This consensus report characterizes the fundamental differences in type 1 diabetes between children and adults and proposes a thoughtful approach to better understand the development and regulatory pathways for type 1 diabetes therapies.
Introduction
Despite advances in the treatment of type 1 diabetes, the disease remains a significant burden for individuals, especially for children and their families. Preventing or halting β-cell destruction—that is, using disease-modifying therapy, instead of just managing symptoms of hyperglycemia—could alleviate this burden. In recent years, potential treatments to alter the course of the disease via targeting the immune response or directly impacting β-cell health have multiplied. The challenge remains to bring such disease-modifying therapies into clinical use, particularly in children.
For diseases that occur in both children and adults, the pathway of pediatric drug development often relies on the concept that the impact of the disease, disease pathophysiology, clinical course, and response to therapy are essentially the same in the adult and pediatric populations. Under this assumption, clinical trials are usually conducted in adults first, with the intent of protecting children from the risks of new therapies. This approach could lead to delays in getting these therapies to children. In addition, if the outcome of such trials successfully leads to approval in the adult population, clinical use in children may occur prior to definitive studies demonstrating safety and efficacy in the pediatric population. Conversely, if the outcome of such trials in the adult population is negative, a therapy that could be efficacious in the pediatric population may never be tested.
Emerging data have increasingly highlighted the differences between type 1 diabetes diagnosed in children as compared with those in adults. Such differences imply that the requirement to first demonstrate efficacy and safety in adults may not be appropriate for type 1 diabetes, indicating that a different pathway should be considered when developing disease-modifying therapies in children with type 1 diabetes.
The American Diabetes Association (ADA), in conjunction with JDRF, the T1D Exchange, and the Benaroya Research Institute, convened a consensus conference in January 2015 entitled “Defining Pathways for Development of Disease-Modifying Therapies in Children With Type 1 Diabetes” to consider how differences in pediatric- and adult-onset disease should be incorporated when weighing the risks and benefits of each potential clinical trial and therapy. Speakers described the current understanding of the burden of the disease, its clinical course, and responses to therapy in the context of differences in pediatric- and adult-onset type 1 diabetes. Additional speakers discussed the ethical and regulatory framework for conducting studies and developing therapies in children. The meeting concluded with an open session in which all participants discussed pathways to engage children in clinical research as well as unmet research needs. This discussion resulted in a series of recommendations for future research directions.
Clinical Burden of Type 1 Diabetes
Epidemiology
Continued increases in the global incidence and prevalence of type 1 diabetes indicate that the disease is an expanding problem. As defined by the U.S. population-based SEARCH for Diabetes in Youth (SEARCH) study, approximately 22 out of every 100,000 children aged <20 years develop type 1 diabetes annually in the U.S. (1). Incidence rates in most countries are steadily rising, particularly in the youngest children (2,3); data from the U.S. suggest that this increase is ∼2.7% per year (4). The prevalence of type 1 diabetes in U.S. children aged <20 years is approximately 1 per 526 children (4), translating to just less than 200,000 affected youth (5). Modeling suggests that the number of children with type 1 diabetes will nearly triple between 2010 and 2050 (6).
Data on type 1 diabetes incidence in adults are less clear due to difficulties in defining and recognizing type 1 diabetes in adults. It has been estimated that 5% of all cases of diabetes diagnosed in adults may be type 1 diabetes (7). As is true for incidence data, precise prevalence estimates in adults are lacking. According to survival data and estimates of incident cases, when both children and adults are considered, 900,000 to 1.25 million Americans live with type 1 diabetes (7,8).
Glycemic Control
Glycemic control is the foundation of type 1 diabetes care due to its role in prevention of acute and long-term complications.
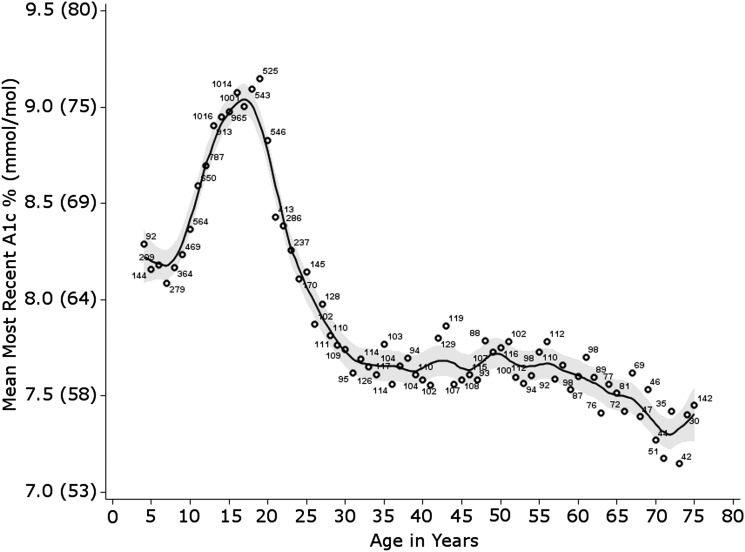
The ADA recommends an HbA1c target of <7.5% (<58 mmol/mol) for youth aged <18 years and an HbA1c target of <7.0% (<53 mmol/mol) for adults (9). Unfortunately, these targets are infrequently met. Data from the T1D Exchange clinic registry, which includes ∼26,000 participants with type 1 diabetes seen at ∼70 adult and pediatric diabetes specialty centers in the U.S., show mean HbA1c levels well above targets at all ages, particularly in teenagers (Fig. 1) (10). Population-based data from the SEARCH study also reflect significant hyperglycemia; nearly 17% of youth with type 1 diabetes have HbA1c >9.5% (>80 mmol/mol), with higher HbA1c levels observed in children from ethnic minority populations (4). Data from other countries indicate suboptimal glycemic control as well (11). These rates persist despite the availability of comprehensive care recommendations and advanced technology.
Figure 1.
Mean HbA1c levels by age. Circles represent mean HbA1c values for each year of age from 16,057 T1D Exchange registry participants. Participants aged <4 years were grouped as age 4 and those aged ≥75 years were grouped as age 75. Shaded area represents the 95% CI around smoothed line. Numbers next to circles are the N for each year of age. Reprinted with permission from Miller et al. (10).
In addition to the failure to meet glycemic targets, current care also fails to prevent severe hypoglycemic episodes. In 2015, the T1D Exchange found that up to 6% of individuals had reported a seizure or loss of consciousness attributable to hypoglycemia in the previous 3 months (10). The previously well-recognized relationship between better glucose control and higher rates of hypoglycemia was not seen in the T1D Exchange clinic registry data; similar rates of severe hypoglycemia were seen across all HbA1c values (Supplementary Table 1) (10). These data indicate that factors beyond glycemic control, such as endogenous insulin secretion, may be important in preventing severe hypoglycemia.
Diabetic ketoacidosis (DKA) also remains a common acute complication. In the U.S., the SEARCH study reported that ∼30% of participants younger than 20 years of age with type 1 diabetes presented with DKA (12). Recent data noted that 46% of newly diagnosed children had DKA at onset in 2012 (13). Outside of diabetes onset, 3% of the T1D Exchange participants reported experiencing at least one episode of DKA requiring a visit to a hospital or other medical facility within the prior 3 months. DKA rates were generally highest in children (10).
Neurocognitive Effects
Studies have shown that both children and adults with type 1 diabetes may have evidence of cognitive dysfunction and structural changes within the central nervous system. Differences between people with and without diabetes are most apparent on measures of psychomotor speed, cognitive flexibility, intelligence, attention, and visual perceptual ability, whereas learning, memory, and language skills are usually unaffected. Effect sizes are moderate (14) and are somewhat lower in children (15), with one important exception. Some children who developed type 1 diabetes early in life, before the age of 6 or 7 years, not only perform more poorly on virtually all cognitive tests—including measures of learning and memory—but also are more likely to meet diagnostic criteria for clinically significant impairment (16).
Dysfunction may appear soon after the diagnosis. For example, young children who had diabetes for less than 2 or 3 years, were diagnosed early in life, and had elevated HbA1c values performed poorly on multiple cognitive tests and manifested widely distributed microstructural white matter changes (17,18). A recent report demonstrated that older children and adolescents studied within 3 days of the diagnosis performed significantly below average on tests of psychomotor speed, and those scores predicted HbA1c values 1 year later (19).
Longitudinal studies have demonstrated that cognitive function may decline somewhat over time when children with type 1 diabetes are followed from childhood into early adulthood (20). Over a 12-year period, children followed since diagnosis showed only a 1-point decrease in intelligence quotient scores compared with demographically similar subjects without diabetes. However, when patients with an earlier onset of diabetes were compared with those with a later onset, a greater decline over time was observed (∼4 points), and when those who experienced severe hypoglycemia at any age were compared with those who never experienced hypoglycemia, an even greater decline was seen (∼6 points) (21).
The pathophysiological basis for neurocognitive changes in children with type 1 diabetes remains poorly understood, but it appears that the development of diabetes early in life is an important risk factor, as is a history of chronically elevated hyperglycemia and/or severe hypoglycemia. Interventions that can delay the onset of diabetes (for example, shift its onset beyond the first 6–7 years of life) or that can reduce the occurrence of glycemic extremes may lead to marked reductions in the risk of cognitive dysfunction in children and adolescents.
Long-term Consequences
The long-term prognosis for those with childhood-onset type 1 diabetes has greatly improved over the last 30 years (22). Advanced chronic complications are now rarely seen in the U.S. during childhood or adolescence, although early signs of complications can still be detected (4).
Indeed, recent data from the Pittsburgh Epidemiology of Diabetes Complications (EDC) study suggest that for those who were diagnosed with type 1 diabetes in childhood between 1965 and 1980 life expectancy is now only 3.8 years less than what might be expected (23). Furthermore, as suggested by the Finnish Diabetic Nephropathy Study (FinnDiane) (24) and confirmed in the EDC over a 20-year follow-up (25), there appears to be no excess mortality in those who avoid increased albuminuria. Although rare, when death does occur in children with diabetes, it is usually (∼80% in one recent analysis [26]) due to acute complications (hypoglycemia or DKA).
In contrast, two national databases in Scotland (27) and Sweden (28) showed that mortality rates still appear to be greatly increased in adults with type 1 diabetes relative to individuals without diabetes. Interestingly, both of these studies included those with adult-onset type 1 diabetes. This raises the issue as to whether the natural history differs in childhood- versus adult-onset cases. It has long been thought by some that the prepubertal years of type 1 diabetes are less “damaging” than the years after the onset of puberty. A recent study from Sweden supports this concept (29), but the tenet remains controversial. Death due to DKA or hypoglycemia among adults with type 1 diabetes is less common, proportionately, than in children and accounts for between 10% (26) and 18% (30) of all deaths.
The 30-year cumulative incidence of complications in the Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) conventional treatment group and in the DCCT “eligible” participants from the EDC study showed similar rates (31). In the DCCT conventional treatment group, 50% developed proliferative retinopathy, 14% had cardiovascular disease, and 25% had nephropathy. Despite significant changes in clinical care, among the major complications, only end-stage renal disease showed a major fall in the EDC after 30 years’ duration (22). As shown by the DCCT, improved glycemic control is likely the most critical risk factor in terms of reducing complication rates in type 1 diabetes; the inability to achieve glycemic targets as outlined above is therefore one explanation for the persistence of complications in type 1 diabetes. However, even with improved glucose control and potential reductions in other factors, such as smoking, insulin resistance (32), hypertension (33), and hyperlipidemia (33,34), the increasing incidence of type 1 diabetes combined with the increased survival of those diagnosed in childhood noted above portends an increasing burden on society with respect to care of adults with long-standing type 1 diabetes.
Data from the DCCT highlight the important role of residual endogenous insulin secretion in microvascular complications and hypoglycemia. For patients receiving exogenous insulin therapy, measurement of C-peptide reflects endogenous β-cell secretion. Patients with a stimulated C-peptide >0.2 nmol/L had a 62% lower risk for severe hypoglycemia and a 79% lower risk for progression of retinopathy (35) (Supplementary Fig. 1), indicating that C-peptide >0.2 nmol/L is a clinically significant threshold. Even lower, but measurable, amounts of C-peptide were recently reported to confer protection from long-term complications (36). The value of small amounts of endogenous β-cell function is also highlighted in islet transplantation literature. Most patients undergoing islet transplantation have recurrent severe hypoglycemia as a result of hypoglycemic unawareness—a severely debilitating consequence of type 1 diabetes. Although only 44% of patients remain insulin independent 3 years after transplant, almost all subjects with modest C-peptide production after transplant have complete resolution or significant reduction in severe hypoglycemia (37).
Quality of Life
Quality of life (QOL) is recognized as a central outcome for health care and health care policy and is increasingly considered as an important outcome measure in clinical trials evaluating interventions to improve diabetes management. The construct includes both general well-being and health-related QOL, encompassing the disease state and physical symptoms, functional status, psychological and social functioning, and neurocognitive functioning.
Factors related to the QOL of individuals with type 1 diabetes include medical, demographic, and psychosocial components. In addition, the QOL of parents and other family members is also affected, particularly for those with childhood type 1 diabetes, because many parents experience increased psychological distress as well as the burden of caregiving related to diabetes management.
There are a number of reliable and valid measures of both child self-reported and parent proxy-reported generic and diabetes-specific QOL for children and adolescents with type 1 diabetes (38–40). These measures typically provide an overall score and scale scores for the domains of QOL, and because they are fairly brief, they have good utility for use in clinical trials. Comparisons of QOL cannot be made between adults and children in the same study because there are no standardized QOL measures that are appropriate for both populations.
Although some individual studies showed small to moderate effect sizes based on several standardized measures, weighted effect sizes across studies suggest that scores are more similar than different across QOL domains between children with type 1 diabetes and healthy peers. Interestingly, however, parents tend to rate their children’s QOL as lower compared with healthy peers (41). Numerous studies have documented that many parents report significant distress after their child’s diagnosis of diabetes, with significant symptoms of depression and posttraumatic stress disorder evident in up to one-third and with ∼20% reporting distress up to 4 years later (42). Fear of hypoglycemia is also common among parents of children with type 1 diabetes and is related to their own increased emotional distress as well as poor glycemic control in their children (43,44). Thus, it is clear that the QOL of parents and caregivers is affected by type 1 diabetes in their children.
There is conflicting literature about the relationship of QOL with factors such as age of onset or duration of the disease in childhood (45). One study was unique in examining diabetes-specific QOL in a sample of 59 adults with type 1 diabetes, including 16 diagnosed before the age of 5 years (46). Those diagnosed very early in life reported better QOL than those with later diagnoses; however, these results are limited by the small study sample size. Similarly, there appears to be a limited effect of treatment regimens or use of glucose-sensing technology on QOL in both children and adults (41,47,48).
Multiple studies have demonstrated that lower HbA1c is associated with better QOL (48–50). A recent prospective study showed that poor QOL predicted later poor glycemic control (51). Both pediatric and adult studies reveal a reduced QOL with respect to the consequences of the disease. SEARCH results reveal that in children reduced QOL is associated with the presence of comorbidities and early health complications, greater frequency of serious hypoglycemic episodes and emergency department visits, and hospitalizations for poor metabolic control (48,49). Similarly, studies in adults with type 1 diabetes find that QOL is adversely impacted by lower socioeconomic status, longer duration of diabetes, presence of health complications, comorbid psychiatric disorders, less social support, decreased physical activity, obesity, more hypoglycemic episodes, and perceived sense of burden related to diabetes self-management (52–54).
Clinical Course
Type 1 diabetes starts long before the clinical onset of hyperglycemia, progressing through multiple stages of the disease (55). In relatives of individuals with type 1 diabetes and those without relatives tested due to high genetic risk, islet autoantibodies can be identified, signaling that the immune system is inappropriately sensing and damaging β-cells. Those confirmed to have multiple antibodies are considered to have “islet autoimmunity”; the vast majority of these individuals will develop diabetes over time (56,57). Prior to clinical diagnosis, impaired insulin secretion and eventual abnormal glucose tolerance are evidence of β-cell injury and death. After clinical diagnosis, β-cell destruction continues, with the majority of individuals eventually having minimal or no detectable endogenous insulin secretion. Although this overall picture of the disease course has been confirmed in multiple studies over the past decades, there are now considerable data highlighting significant differences in the clinical course of the disease and rate of the disease progression in children compared with adults.
Effect of Age on Progression From Risk to Onset of Clinical Disease
Prior to diagnosis, important information about the age at which β-cell autoimmunity first appears has been gleaned from genetically at-risk cohorts followed from birth. These include the Diabetes Autoimmunity Study in the Young (DAISY) in Colorado, the Finnish Type 1 Diabetes Prediction and Prevention (DIPP) study, the BABYDIAB studies in Germany, and the international The Environmental Determinants of Diabetes in the Young (TEDDY) study. Data from the National Institutes of Health (NIH)-sponsored Diabetes Prevention Trial–Type 1 (DPT-1) (58,59) and the Type 1 Diabetes TrialNet Pathway to Prevention Study (60) (www.diabetestrialnet.org) also provide evidence on the effect of age on progression from autoimmunity to clinical disease.
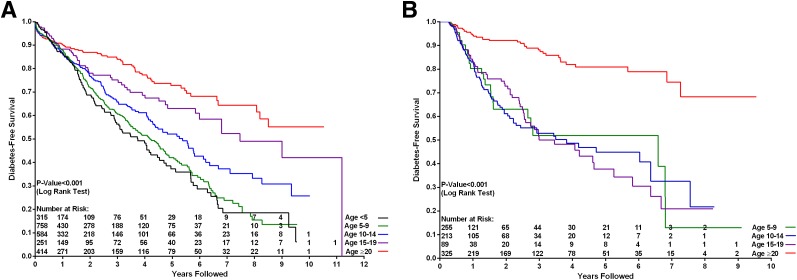
Children with high genetic risk based on HLA haplotype have been followed from birth for the development of autoantibodies and type 1 diabetes. Combined data from DAISY, DIPP, and BABYDIAB suggest that nearly all children who develop multiple autoantibodies go on to eventually develop childhood type 1 diabetes (>85% risk at 15 years) (61). Developing multiple autoantibodies prior to age 3 years further increased the rate of progression compared with children who developed antibodies at older ages. These cohort studies in children followed from birth indicate that the disease process starts very early in life. The DIPP study found that 65% of those who developed clinical disease before puberty had antibodies before age 2 years and 95% before age 5 years (62). The DPT-1 and the TrialNet Pathway to Prevention Study screened first- and second-degree family members (1–45 years of age) of probands with type 1 diabetes for the presence of autoantibodies. Data from these studies also suggest that the vast majority of relatives with two or more antibodies eventually develop clinical disease at a rate of ∼10–12% per year (57). TrialNet found that the most important factor associated with a more rapid rate of progression is age; children with multiple antibodies progress to clinical disease much more rapidly than adults (P < 0.0001). These dramatic differences are illustrated in Fig. 2A. The path from islet immunity to clinical disease includes an interim stage of metabolic decompensation manifested as impaired glucose tolerance. Overall, more than 85% of antibody-positive relatives with impaired glucose tolerance will have clinical disease within 5 years. Strikingly, even at this stage of the disease progression, younger age markedly increases the rate of the disease development compared with older age (Fig. 2B).
Figure 2.
Impact of age on risk for disease progression in antibody-positive relatives participating in TrialNet Pathway to Prevention Study. A: Life table of progression to diabetes according to age in double antibody–positive relatives. B: Life table of progression to diabetes according to age in double antibody–positive subjects from time of abnormal glucose tolerance.
Effect of Age on Residual Insulin Secretion After Clinical Diagnosis
Similar data are now available regarding the rate of decline of endogenous insulin secretion, measured by C-peptide, after the onset of clinical disease. A series of recent studies provide new insights; detectable C-peptide secretion persists longer after the type 1 diabetes diagnosis than is commonly appreciated, and age is the most important factor impacting the rate of decline of C-peptide post diagnosis.
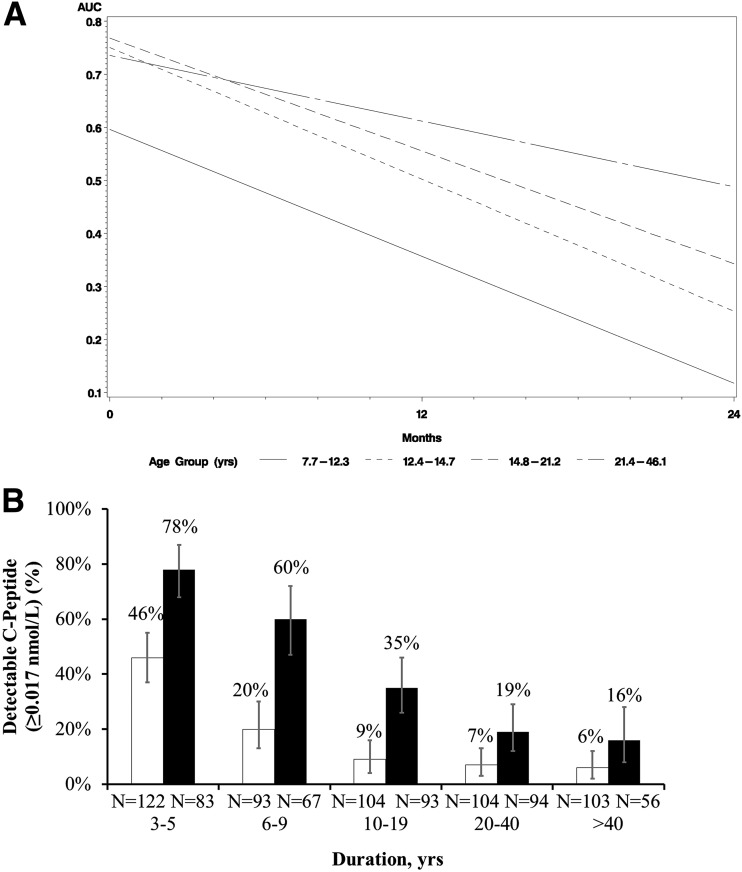
Greenbaum et al. (63) studied residual insulin secretion within 2 years of diagnosis in subjects from the TrialNet’s new-onset intervention trials. C-peptide at the start of the study was driven by age, with the youngest cohort (Fig. 3A) exhibiting the lowest C-peptide. Age was also highly correlated with loss of C-peptide over time: subjects aged 7–21 years demonstrated rates of decline in stimulated C-peptide secretion that were similar over time, whereas participants aged >21 years manifested a significantly slower rate of C-peptide decline.
Figure 3.
Impact of age on C-peptide after diagnosis. A: Model-based estimates of average slopes of C-peptide area under the curve (AUC) over time according to age quartiles (age-groups 7.7–12.3 years, 12.4–14.7 years, 14.8–21.2 years, and 21.4–46.1 years). Data from 191 TrialNet clinical trial participants. Reprinted with permission from Greenbaum et al. (63). B: Proportion of participants with detectable (≥0.017 nmol/L) nonfasting C-peptide according to age at diagnosis and duration of type 1 diabetes. White bars, those diagnosed at age ≤18 years; black bars, those diagnosed at age >18 years. Data from the T1D Exchange residual insulin study. Reprinted with permission from Davis et al. (64).
Persistence of C-peptide secretion also varies between those diagnosed as children and those diagnosed as adults, with more adults retaining C-peptide production longer after the diagnosis than is commonly appreciated. Davis et al. (64) measured C-peptide in 919 subjects characterized by the duration of the disease and whether they were diagnosed as children or as adults. Although the fraction of individuals with detectable random C-peptide diminished over time as expected, there was a dramatic difference in persistence of C-peptide according to age at diagnosis (Fig. 3B). For a given duration of the disease, the odds for having C-peptide were estimated as 6% higher for every 1-year increase in the age of diagnosis. The same difference between children and adults was observed for C-peptide ≥0.2 nmol/L.
Response to Therapy
Type 1 diabetes in children and juvenile idiopathic arthritis (JIA) have striking similarities, including similar prevalence and effect on families. Both diseases affect children and adults, and the course is notably different in the two age-groups (Table 1). Disease-modifying therapy has transformed the lives of children with JIA; instead of treatment focused on symptom management of pain or disability, treatment changing the course of the disease, although not yet curative, has markedly improved the daily lives of these families. Differences in response to therapy between pediatric and adult rheumatic disease have become apparent during the conduct of more than a dozen studies in children in recent years. As a result of these studies, many of these therapies now carry approval for use in pediatric rheumatic disease (65). As described below, a similar story is emerging with respect to the effect of age on response to disease-modifying therapy in type 1 diabetes.
Table 1.
Similarities between JIA and childhood-onset type 1 diabetes
| • Pediatric and adult forms of both diseases are similar to each other but not identical. |
| • Both diseases are chronic without known curative treatment and require ongoing therapy. |
| • Both diseases are associated with increased morbidity and mortality. |
| • Both diseases have complex and multifactorial effects on the lives of patients and their families requiring a multidimensional assessment of clinical effect of treatments (e.g., pain, health-related QOL, social function, school function, etc.). |
| • Prevalence: |
| • JIA: 1 per 1,000 individuals (91). |
| • Type 1 diabetes: ∼2 per 1,000 aged ≤20 years (4). |
| • Relatively rare diseases in which market incentives are unlikely to lead pharmaceutical firms to focus on them. |
| • Moderate polygenetic predisposition. |
| • Etiologic agent(s) unknown. |
| • Preclinical phase can extend over years, is poorly understood, and remains without therapeutic options. |
| • In JIA, time is critical in the clinical phase—each month of delay of treatment onset during the first 12 months after the disease onset decreases the ability to reach clinical remission by 1.7 fold (92). Analysis of teplizumab response in recently diagnosed type 1 diabetes showed better preservation of C-peptide if treatment was initiated <6 weeks after the diagnosis (74). |
Participation of Children in Type 1 Diabetes Trials
Children with recent-onset type 1 diabetes have been enrolled in trials of disease-modifying therapies since the early 1980s and constitute the majority of participants in many trials. The proportion of subjects aged <16 years enrolled in 10 NIH- and industry-sponsored multicenter clinical trials conducted since 2001 has ranged between 24% and 84% (Supplementary Table 2). Similarly, the majority of participants are children in 10 trials of disease-modifying therapies given prior to the onset of clinical disease (that is, type 1 diabetes prevention trials) that were or are being performed in the U.S. and Europe (Supplementary Table 3).
It is important to recognize that parents and children are eager to participate in type 1 diabetes studies, such that the pace of enrollment is markedly greater in trials open to pediatric participants. For example, the rate of enrollment markedly increased in both the TrialNet abatacept (66) and GAD65 (67) trials once the enrollment age was reduced (Supplementary Fig. 2). This is in marked contrast to studies enrolling adults only, some of which are unable to fully complete enrollment in the planned time period (68).
Effect of Age on Efficacy
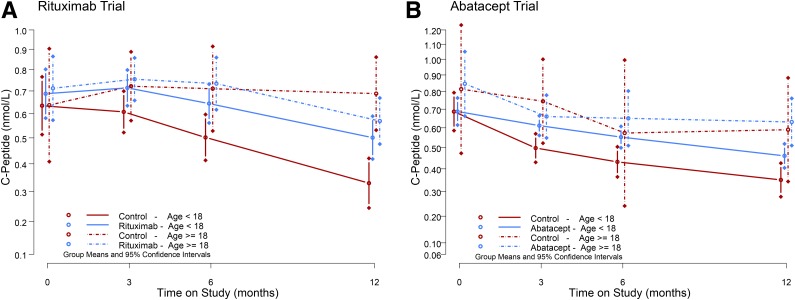
Of all the fully powered multicenter clinical trials in recently diagnosed type 1 diabetes conducted since 2001, three therapeutic approaches had positive outcomes, with active drug–treated subjects experiencing significant reductions in the rate of decline in C-peptide compared with placebo-treated subjects. These therapies are rituximab (anti-CD20 monoclonal antibody) (69), abatacept (CTLA4-Ig) (66), and the anti-CD3 monoclonal antibodies teplizumab (70,71) and otelixizumab (72). All of these trials included many pediatric participants. Most importantly, the significant effect of drug treatment in the rituximab and abatacept trials was largely driven by the positive response noted in the pediatric population (Fig. 4). In two trials of an anti-CD3 monoclonal antibody (71,73), subjects younger than 15 years of age had a more robust response compared with those who were older. The effects of young age were not limited to change in C-peptide: the treatment effect on insulin use was significantly different in subjects younger than 15 years of age (P = 0.02), but not in older subjects (P = 0.8). If enrollment in these studies had been limited to adults, then the study results would have likely been negative, and promising therapies for children would have been inappropriately discarded. In most of the clinical trials in which the overall result was negative, neither the pediatric nor adult populations had any benefit, as illustrated by the results from the GAD trial (67). In contrast, in the Study of Antithymocyte Globulin for Treatment of New-onset T1DM (START) (ClinicalTrials.gov identifier NCT00515099), which only enrolled subjects 12 years of age or older, post hoc analysis pointed to improved C-peptide responses after 12 months in older (aged >22 years) but not younger subjects (P = 0.04) (74).
Figure 4.
Impact of age on response to disease-modifying therapy. A: C-peptide over time in TrialNet participants randomized to treatment with rituximab (blue line) or placebo (red line) who were aged <18 years (solid lines) or aged ≥18 years (dashed lines) at the time of randomization (69). B: C-peptide over time in TrialNet participants randomized to treatment with abatacept (blue line) or placebo (red line) who were aged <18 years (solid lines) or aged ≥18 years (dashed lines) at the time of randomization (66).
Effect of Age on Safety
Disease-modifying therapies that alter immune function share similar theoretical risks among each other: in the short term, risks of infection and, potentially in the longer term, additional adverse effects with chronic use or if there is persistence of immune modulation. Thus, careful monitoring of short- and long-term safety is imperative. It is reassuring that in the treatment of many rheumatologic disorders, the adverse event profile is similar between adults and children. Similar data have been seen in type 1 diabetes trials using disease-modifying therapies to date wherein the safety profiles have not differed between children and adults, including studies testing teplizumab (75), abatacept (66), and rituximab (69). Additionally, the effect of therapy on immunization was directly studied in some of these trials and demonstrated no compromise in efficacy (66,69).
Regulatory Issues
Including children in product development trials is necessary to ensure effective dosing for the pediatric population (for example, to characterize differences in absorption, distribution, elimination, and metabolism between adults and children of different ages) and to address potential differences in the safety profile between the pediatric and the adult populations.
The U.S. Congress passed the Best Pharmaceuticals for Children Act (BPCA) in 1997 to encourage pharmaceutical makers to voluntarily conduct studies in children, providing sponsors with specific incentives. The Pediatric Research Equity Act (PREA) of 2003 mandates pediatric studies (76). As a result, more than 500 products were studied in U.S. pediatric populations and now carry pediatric information on the label. Similar pediatric legislation exists in the European Union (EU) (77).
Government agency regulation of clinical research and drug development process is critical to ensure trial participant safety. Pediatric development is global in nature, but legal and regulatory differences exist. These include the timing of when the pediatric investigation plans should be submitted and who is responsible for approving the pediatric development plan. In the U.S., this is within the relevant U.S. Food and Drug Administration (FDA) division that may receive advice or guidance from the Office of Pediatric Therapeutics, whereas in the EU, an external group of advisors (Paediatric Committee [PDCO]) (78) has decision-making authority. Both the FDA and the European Medicines Agency (EMA) recommend that industry should request early discussions with relevant regulatory agencies to enable a global discussion of drug development and study end points.
A pediatric investigative plan, although required by both the FDA and the EMA in any new drug submission, does not always necessitate a pediatric clinical trial. Both the FDA and the EMA support extrapolation of well-controlled adult efficacy data to the pediatric population when possible and relevant.
Guidance (EU [79]) and draft guidance (FDA [80]) on the development of disease-modifying therapies for type 1 diabetes are available. EU guidance specifically recommends an approach whereby studies in younger age-groups require prior demonstration of efficacy and safety in older subjects.
Orphan Drug Status
FDA’s Orphan Drug Act grants special status to a drug or biological product (“drug”) to treat a rare (for example, affects <200,000 people in the U.S.) disease or condition (81). Similar statutes exist in the EU (82). There are significant incentives to encourage drug manufacturers to develop therapies for small populations, where the financial rewards would otherwise be nonexistent. The same regulatory requirements for safety and efficacy must be established for orphan drugs as with all therapies.
As there are <200,000 children with type 1 diabetes in the U.S., development of disease-modifying therapies in type 1 diabetes could possibly meet these criteria. In the U.S., but not in the EU, there are several new products for β-cell preservation in new-onset type 1 diabetes designated as orphan drugs.
Ethical Aspects
It is critical to conduct research aimed at improving health care for children with diabetes. At the same time, children are not able to consent for themselves, and it is of paramount importance to protect the children who participate. To achieve this balance, the Institute of Medicine has six requirements for pediatric research (83). The present analysis focuses on the first four of these requirements.
First, children should be enrolled in research only when it has the potential to collect valuable data. Each intervention included in the study should have sufficient scientific value to justify the risks and burdens it poses to participants.
Second, it is important to ensure that there is a compelling reason to enroll children. If the same data could be obtained by studying adults, then children should not be enrolled. When to initiate trials in children needs to be determined on a case-by-case basis, taking into account the extent to which similar data can be collected in adults, the effectiveness and safety of available treatments for children, and the risks and potential benefits of the interventions under study (84). Typically, it is acceptable to enroll children in research when it offers them a favorable risk-to-benefit ratio or it poses low net risks.
Third, whether research offers a favorable risk-to-benefit ratio depends on two assessments. Is the risk-to-benefit profile of the interventions included in the study favorable for eligible participants and at least as favorable as the available alternatives (85)? If there is compelling evidence that an intervention poses no chance of serious harm to children with type 1 diabetes, then even a theoretical chance of an important benefit could be enough to make an intervention’s risk-to-benefit profile favorable. In contrast, if there is reason to believe that an intervention poses some serious risks to children with diabetes, one would need evidence of efficacy to categorize the intervention as offering a favorable risk-to-benefit ratio. The degree of benefit and level of evidence in this case needs to be commensurate with the level of potential harm and the degree of evidence supporting that potential.
In practice, one way to determine whether a study offers a favorable risk-to-benefit ratio is to consider, or determine through consultation, the following: Given what is known about the interventions included in the study and what is known about the available alternatives, would an independent and expert clinician regard enrolling children who have diabetes as promoting the children’s clinical interests? If so, the study offers a favorable risk-to-benefit ratio. If not, the study involves an unfavorable risk-to-benefit ratio and thereby poses some degree of net risk to participants.
Fourth, when one or more of the interventions included in a study pose net risks, one needs to determine whether the net risks of the intervention and the cumulative net risks of the study are acceptable. Exposing children to research risks and burdens to collect data to benefit future patients raises important ethical issues (86,87). However, outside of the research context, children frequently engage in activities that pose some risks and are designed to benefit others, such as collecting money for a charity. Widespread acceptance of these activities suggests that pediatric research that does not offer a prospect of direct benefit can also be acceptable when it has the potential to gather valuable data and the net risks are low. This view is supported by empirical studies that found that children and their parents are overall equally willing to have the child help others by participating in research or a charitable activity (88,89).
Empirical data suggest that adolescents aged ≥12–14 years are able to understand research and make their own decisions whether to enroll (90). This suggests that enrolling adolescents who understand and agree (assent) poses significantly fewer ethical concerns than enrolling younger children who cannot understand the research in question. For this reason, it may be acceptable to expose adolescents who give their assent to somewhat higher net risks than younger children who cannot understand the research in question.
Summary
The burden of type 1 diabetes, whether diagnosed in childhood or adulthood, with regard to daily management, glycemic control, and acute and chronic complications, remains despite improvements in treatment regimens. Moreover, the burden of type 1 diabetes on society is likely to increase in the future with the increasing incidence of the disease and longer life expectancy. Importantly, there are unique aspects of disease burden in those diagnosed as children including worse glycemic control during teenage years, emotional distress of parents, and more significant neurocognitive effects in the youngest individuals. Disease-modifying therapy that can delay the onset of clinical disease or preserve endogenous secretion after the diagnosis has the potential to significantly reduce the burden of the disease on society, individuals, and families.
Robust data obtained from observational and clinical trials indicate that the development of the disease and the subsequent clinical course are significantly different between adults and children. Children, particularly younger children, may stand to benefit the most from disease-modifying therapy because they are at an increased risk of cognitive dysfunction, progress faster through the stages of the disease, have at the time of diagnosis a lower C-peptide that then declines more quickly over time, and pose the greatest challenges for clinical management. There are also differences in therapeutic response in trials of disease-modifying therapies in adults compared with pediatric participants. Although disease-modifying therapies are important goals for all those with type 1 diabetes, these data emphasize the need to design studies that account for age-related differences and to avoid reliance on efficacy outcomes in adults in order to study children. Important differences in pathophysiology suggest that different therapeutic approaches may be needed.
There is widespread agreement that there needs to be a favorable risk-to-benefit ratio for each therapy being considered for a clinical trial. The challenge is how to understand the level of evidence needed to support potential benefit. Thus, the standard strategy of requiring both safety and efficacy to be demonstrated in adults first has the real possibility to deny or delay the use of a potentially useful therapy to the pediatric population. Risks must be understood in the context of the current clinical burden and QOL experienced by children and their families. Evidence other than proof of efficacy in an adult population should be considered in evaluating potential benefits of therapy. Considering the risks and benefits of each therapy must be a dynamic process; information relevant to the disease burden, disease course, and response to therapy must be examined and reexamined over time (Table 2). As evident from the enthusiasm and passion manifest at the consensus conference, patients, families, industry, academia, advocacy groups, funders, and regulators all have important perspectives to contribute to the discussion; all are interested in improving the lives of those with type 1 diabetes.
Table 2.
Key messages from the conference and open research questions
| Key messages |
|---|
| 1. Differences between childhood- and adult-onset type 1 diabetes should be part of the design of studies of disease-modifying therapies. |
| 2. Studying disease-modifying agents in children should not require efficacy data from adults. |
| 3. Children may benefit more from disease-modifying therapies due to the more rapid loss of insulin secretion before and after their diagnosis, the unique burdens on them and their families, and the greater vulnerability of young children’s neurocognitive development. |
| 4. Investigators should work with regulatory agencies early in the study design process and leverage the pediatric expertise of the agencies. |
| 5. A practical approach to assessing risk-to-benefit ratio is to consider the following: Given what is known about the intervention and the limited alternatives, would an independent and expert clinician regard enrolling children with type 1 diabetes as promoting the children’s clinical interests? |
| Open research questions |
| 1. What is the long-term effect of age at onset and early glycemic control on complication risk both within childhood and adolescence (i.e., pre- vs. peri- or postpuberty) and in comparison with adult-onset type 1 diabetes? |
| 2. What are the biological mechanisms underlying the varying pathways to type 1 diabetes? Which mechanisms are seen in all individuals and which are age dependent? |
| 3. Given the high frequency of residual β-cell function in adults, how should type 1 diabetes in adults be defined? What is the incidence and prevalence of the disease in adults? |
| 4. Are there differences in loss of residual insulin secretion rates in young adults compared with older adults? |
| 5. How is QOL affected by disease-modifying therapies? Do effects differ between adults and children? |
| 6. Are there biomarkers of responses to immune therapies that can discriminate responses in children and adults? |
Supplementary Material
Article Information
Acknowledgments. The authors acknowledge the ADA for organizing and sponsoring the conference; JDRF, the T1D Exchange, and the Benaroya Research Institute for their contributions and sponsorship; and TrialNet, the Immune Tolerance Network, and the International Society for Pediatric and Adolescent Diabetes for their advisory input. The authors thank Dianne Murphy, MD (FDA), and Paolo Tomasi, MD, PhD (EMA), for thoughtful presentations on the role of regulators in the drug development process and review of the manuscript and Jean-Marc Guettier, MD (FDA), for his important role as a panelist at the consensus conference. Additionally, the authors express gratitude to Erika Gebel Berg, PhD (ADA), for her excellent editorial support.
Funding and Duality of Interest. All authors have completed the Unified Competing Interest form at www.icmje.org/conflicts-of-interest (available upon request from J.L.C.) and declare the following conflicts of interest. L.A.D. reports personal fees from Sanofi and grants from Novo Nordisk, outside the submitted work. P.A.G. reports grants from Pfizer, JDRF, Novartis, the NIH, and Omni Bio Pharmaceutical and nonfinancial support from ViaCyte, Genentech, and Baxter, outside the submitted work. P.A.G. has a patent related to the use of AAT for the treatment of type 1 diabetes with royalties paid to Omni Bio Pharmaceutical. D.J.L. reports grants from Bristol-Myers Squibb and other support from AstraZeneca, Bristol-Myers Squibb, AbbVie, Pfizer, Roche, Novartis, UBC, Forest Laboratories, Horizon Pharma, Johnson & Johnson, Biogen, Takeda, Genentech, GlaxoSmithKline, Boehringer Ingelheim, and Celgene, outside the submitted work. T.J.O. reports grants from the National Institute of Diabetes and Digestive and Kidney Diseases, during the conduct of the study; personal fees from the Profil Institute for Clinical Research, Eli Lilly, Abbott Laboratories, and Gilead; and other support from Bristol-Myers Squibb, outside the submitted work. C.M.R. reports personal fees from Novo Nordisk, outside the submitted work. C.J.G. reports grants from Novo Nordisk and Novartis, outside the submitted work. No other potential conflicts of interest relevant to this article were reported.
Footnotes
This consensus report was reviewed and approved by the American Diabetes Association Professional Practice Committee in June 2015 and ratified by the American Diabetes Association Board of Directors in June 2015.
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc15-1429/-/DC1.
*The complete list of the Type 1 Diabetes TrialNet Study Group and Affiliate Investigators can be found in the Supplementary Data.
References
- 1.Lawrence JM, Imperatore G, Dabelea D, et al.; SEARCH for Diabetes in Youth Study Group . Trends in incidence of type 1 diabetes among non-Hispanic white youth in the U.S., 2002-2009. Diabetes 2014;63:3938–3945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vehik K, Dabelea D. The changing epidemiology of type 1 diabetes: why is it going through the roof? Diabetes Metab Res Rev 2011;27:3–13 [DOI] [PubMed] [Google Scholar]
- 3.Dahlquist GG, Nyström L, Patterson CC; Swedish Childhood Diabetes Study Group; Diabetes Incidence in Sweden Study Group . Incidence of type 1 diabetes in Sweden among individuals aged 0-34 years, 1983-2007: an analysis of time trends. Diabetes Care 2011;34:1754–1759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hamman RF, Bell RA, Dabelea D, et al.; SEARCH for Diabetes in Youth Study Group . The SEARCH for Diabetes in Youth study: rationale, findings, and future directions. Diabetes Care 2014;37:3336–3344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pettitt DJ, Talton J, Dabelea D, et al.; SEARCH for Diabetes in Youth Study Group . Prevalence of diabetes in U.S. youth in 2009: the SEARCH for Diabetes in Youth study. Diabetes Care 2014;37:402–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Imperatore G, Boyle JP, Thompson TJ, et al.; SEARCH for Diabetes in Youth Study Group . Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care 2012;35:2515–2520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. 2014 National Diabetes Statistics Report [Internet]. Available from www.cdc.gov/diabetes/data/statistics/2014statisticsreport.html. Accessed 1 March 2015
- 8.Menke A, Orchard TJ, Imperatore G, Bullard KM, Mayer-Davis E, Cowie CC. The prevalence of type 1 diabetes in the United States. Epidemiology 2013;24:773–774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Diabetes Association Standards of medical care in diabetes—2015. Diabetes Care 2015;38(Suppl. 1):S5–S87 [PubMed] [Google Scholar]
- 10.Miller KM, Foster NC, Beck RW, et al.; T1D Exchange Clinic Network . Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care 2015;38:971–978 [DOI] [PubMed] [Google Scholar]
- 11.de Beaufort CE, Swift PGF, Skinner CT, et al.; Hvidoere Study Group on Childhood Diabetes 2005 . Continuing stability of center differences in pediatric diabetes care: do advances in diabetes treatment improve outcome? The Hvidoere Study Group on Childhood Diabetes. Diabetes Care 2007;30:2245–2250 [DOI] [PubMed] [Google Scholar]
- 12.Dabelea D, Rewers A, Stafford JM, et al. ; SEARCH for Diabetes in Youth Study Group. Trends in the prevalence of ketoacidosis at diabetes diagnosis: the SEARCH for Diabetes in Youth Study. Pediatrics 2014;133:e938–e945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rewers A, Dong F, Slover RH, Klingensmith GJ, Rewers M. Incidence of diabetic ketoacidosis at diagnosis of type 1 diabetes in Colorado youth, 1998-2012. JAMA 2015;313:1570–1572 [DOI] [PubMed] [Google Scholar]
- 14.Brands AMA, Biessels GJ, de Haan EHF, Kappelle LJ, Kessels RPC. The effects of type 1 diabetes on cognitive performance: a meta-analysis. Diabetes Care 2005;28:726–735 [DOI] [PubMed] [Google Scholar]
- 15.Tonoli C, Heyman E, Roelands B, et al. Type 1 diabetes-associated cognitive decline: a meta-analysis and update of the current literature. J Diabetes 2014;6:499–513 [DOI] [PubMed] [Google Scholar]
- 16.Gaudieri PA, Chen R, Greer TF, Holmes CS. Cognitive function in children with type 1 diabetes: a meta-analysis. Diabetes Care 2008;31:1892–1897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barnea-Goraly N, Raman M, Mazaika P, et al.; Diabetes Research in Children Network (DirecNet) . Alterations in white matter structure in young children with type 1 diabetes. Diabetes Care 2014;37:332–340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patiño-Fernández AM, Delamater AM, Applegate EB, et al. Neurocognitive functioning in preschool-age children with type 1 diabetes mellitus. Pediatr Diabetes 2010;11:424–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwartz DD, Axelrad ME, Anderson BJ. Neurocognitive functioning in children and adolescents at the time of type 1 diabetes diagnosis: associations with glycemic control 1 year after diagnosis. Diabetes Care 2014;37:2475–2482 [DOI] [PubMed] [Google Scholar]
- 20.Jacobson AM, Ryan CM, Cleary PA, et al.; Diabetes Control and Complications Trial/EDIC Research Group . Biomedical risk factors for decreased cognitive functioning in type 1 diabetes: an 18 year follow-up of the Diabetes Control and Complications Trial (DCCT) cohort. Diabetologia 2011;54:245–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin A, Northam EA, Werther GA, Cameron FJ. Risk factors for decline in IQ in youth with type 1 diabetes over the 12 years from diagnosis/illness onset. Diabetes Care 2015;38:236–242 [DOI] [PubMed] [Google Scholar]
- 22.Pambianco G, Costacou T, Ellis D, Becker DJ, Klein R, Orchard TJ. The 30-year natural history of type 1 diabetes complications: the Pittsburgh Epidemiology of Diabetes Complications Study experience. Diabetes 2006;55:1463–1469 [DOI] [PubMed] [Google Scholar]
- 23.Miller RG, Secrest AM, Sharma RK, Songer TJ, Orchard TJ. Improvements in the life expectancy of type 1 diabetes: the Pittsburgh Epidemiology of Diabetes Complications study cohort. Diabetes 2012;61:2987–2992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Groop P-H, Thomas MC, Moran JL, et al.; FinnDiane Study Group . The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes 2009;58:1651–1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orchard TJ, Secrest AM, Miller RG, Costacou T. In the absence of renal disease, 20 year mortality risk in type 1 diabetes is comparable to that of the general population: a report from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetologia 2010;53:2312–2319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Secrest AM, Becker DJ, Kelsey SF, Laporte RE, Orchard TJ. Cause-specific mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes. Diabetes 2010;59:3216–3222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Livingstone SJ, Levin D, Looker HC, et al.; Scottish Diabetes Research Network epidemiology group; Scottish Renal Registry . Estimated life expectancy in a Scottish cohort with type 1 diabetes, 2008-2010. JAMA 2015;313:37–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lind M, Svensson A-M, Kosiborod M, et al. Glycemic control and excess mortality in type 1 diabetes. N Engl J Med 2014;371:1972–1982 [DOI] [PubMed] [Google Scholar]
- 29.Möllsten A, Svensson M, Waernbaum I, et al.; Swedish Childhood Diabetes Study Group; Diabetes Incidence Study in Sweden; Swedish Renal Registry . Cumulative risk, age at onset, and sex-specific differences for developing end-stage renal disease in young patients with type 1 diabetes: a nationwide population-based cohort study. Diabetes 2010;59:1803–1808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Orchard TJ, Nathan DM, Zinman B, et al.; Writing Group for the DCCT/EDIC Research Group . Association between 7 years of intensive treatment of type 1 diabetes and long-term mortality. JAMA 2015;313:45–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nathan DM, Zinman B, Cleary PA, et al.; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Research Group . Modern-day clinical course of type 1 diabetes mellitus after 30 years’ duration: the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications and Pittsburgh Epidemiology of Diabetes Complications experience (1983-2005). Arch Intern Med 2009;169:1307–1316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yip J, Mattock MB, Morocutti A, Sethi M, Trevisan R, Viberti G. Insulin resistance in insulin-dependent diabetic patients with microalbuminuria. Lancet 1993;342:883–887 [DOI] [PubMed] [Google Scholar]
- 33.Forrest KY, Maser RE, Pambianco G, Becker DJ, Orchard TJ. Hypertension as a risk factor for diabetic neuropathy: a prospective study. Diabetes 1997;46:665–670 [DOI] [PubMed] [Google Scholar]
- 34.Miller RG, Secrest AM, Ellis D, Becker DJ, Orchard TJ. Changing impact of modifiable risk factors on the incidence of major outcomes of type 1 diabetes: the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care 2013;36:3999–4006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Steffes MW, Sibley S, Jackson M, Thomas W. Beta-cell function and the development of diabetes-related complications in the Diabetes Control and Complications Trial. Diabetes Care 2003;26:832–836 [DOI] [PubMed] [Google Scholar]
- 36.Lachin JM, McGee P, Palmer JP; DCCT/EDIC Research Group . Impact of C-peptide preservation on metabolic and clinical outcomes in the Diabetes Control and Complications Trial. Diabetes 2014;63:739–748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barton FB, Rickels MR, Alejandro R, et al. Improvement in outcomes of clinical islet transplantation: 1999-2010. Diabetes Care 2012;35:1436–1445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.de Wit M, Pouwer F, Gemke RJBJ, Delemarre-van de Waal HA, Snoek FJ. Validation of the WHO-5 Well-Being Index in adolescents with type 1 diabetes. Diabetes Care 2007;30:2003–2006 [DOI] [PubMed] [Google Scholar]
- 39.Ingersoll GM, Marrero DG. A modified quality-of-life measure for youths: psychometric properties. Diabetes Educ 1991;17:114–118 [DOI] [PubMed] [Google Scholar]
- 40.Varni JW, Burwinkle TM, Jacobs JR, Gottschalk M, Kaufman F, Jones KL. The PedsQL in type 1 and type 2 diabetes: reliability and validity of the Pediatric Quality of Life Inventory Generic Core Scales and Type 1 Diabetes Module. Diabetes Care 2003;26:631–637 [DOI] [PubMed] [Google Scholar]
- 41.Nieuwesteeg A, Pouwer F, van der Kamp R, van Bakel H, Aanstoot H-J, Hartman E. Quality of life of children with type 1 diabetes: a systematic review. Curr Diabetes Rev 2012;8:434–443 [DOI] [PubMed] [Google Scholar]
- 42.Whittemore R, Jaser S, Chao A, Jang M, Grey M. Psychological experience of parents of children with type 1 diabetes: a systematic mixed-studies review. Diabetes Educ 2012;38:562–579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haugstvedt A, Wentzel-Larsen T, Graue M, Søvik O, Rokne B. Fear of hypoglycaemia in mothers and fathers of children with type 1 diabetes is associated with poor glycaemic control and parental emotional distress: a population-based study. Diabet Med 2010;27:72–78 [DOI] [PubMed] [Google Scholar]
- 44.Johnson SR, Cooper MN, Davis EA, Jones TW. Hypoglycaemia, fear of hypoglycaemia and quality of life in children with type 1 diabetes and their parents. Diabet Med 2013;30:1126–1131 [DOI] [PubMed] [Google Scholar]
- 45.Bott U, Mühlhauser I, Overmann H, Berger M. Validation of a diabetes-specific quality-of-life scale for patients with type 1 diabetes. Diabetes Care 1998;21:757–769 [DOI] [PubMed] [Google Scholar]
- 46.Trento M, Trevisan M, Coppo E, et al. Diagnosis of type 1 diabetes within the first five years of life influences quality of life and risk of severe hypoglycemia in adulthood. Acta Diabetol 2014;51:509–511 [DOI] [PubMed] [Google Scholar]
- 47.Valenzuela JM, Patino AM, McCullough J, et al. Insulin pump therapy and health-related quality of life in children and adolescents with type 1 diabetes. J Pediatr Psychol 2006;31:650–660 [DOI] [PubMed] [Google Scholar]
- 48.Lawrence JM, Yi-Frazier JP, Black MH, et al.; SEARCH for Diabetes in Youth Study Group . Demographic and clinical correlates of diabetes-related quality of life among youth with type 1 diabetes. J Pediatr 2012;161:201–207.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Naughton MJ, Ruggiero AM, Lawrence JM, et al.; SEARCH for Diabetes in Youth Study Group . Health-related quality of life of children and adolescents with type 1 or type 2 diabetes mellitus: SEARCH for Diabetes in Youth Study. Arch Pediatr Adolesc Med 2008;162:649–657 [DOI] [PubMed] [Google Scholar]
- 50.Hoey H, Aanstoot HJ, Chiarelli F, et al. Good metabolic control is associated with better quality of life in 2,101 adolescents with type 1 diabetes. Diabetes Care 2001;24:1923–1928 [DOI] [PubMed] [Google Scholar]
- 51.Hilliard ME, Mann KA, Peugh JL, Hood KK. How poorer quality of life in adolescence predicts subsequent type 1 diabetes management and control. Patient Educ Couns 2013;91:120–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Imayama I, Plotnikoff RC, Courneya KS, Johnson JA. Determinants of quality of life in adults with type 1 and type 2 diabetes. Health Qual Life Outcomes 2011;9:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lloyd CE, Orchard TJ. Physical and psychological well-being in adults with type 1 diabetes. Diabetes Res Clin Pract 1999;44:9–19 [DOI] [PubMed] [Google Scholar]
- 54.Watkins KW, Connell CM, Fitzgerald JT, Klem L, Hickey T, Ingersoll-Dayton B. Effect of adults’ self-regulation of diabetes on quality-of-life outcomes. Diabetes Care 2000;23:1511–1515 [DOI] [PubMed] [Google Scholar]
- 55.Insel RA, Dunne JL, Atkinson MA, et al. Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association. Diabetes Care 2015;38:1964–1974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bonifacio E. Predicting type 1 diabetes using biomarkers. Diabetes Care 2015;38:989–996 [DOI] [PubMed] [Google Scholar]
- 57.Orban T, Sosenko JM, Cuthbertson D, et al.; Diabetes Prevention Trial–Type 1 Study Group . Pancreatic islet autoantibodies as predictors of type 1 diabetes in the Diabetes Prevention Trial–Type 1. Diabetes Care 2009;32:2269–2274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Diabetes Prevention Trial–Type 1 Diabetes Study Group Effects of insulin in relatives of patients with type 1 diabetes mellitus. N Engl J Med 2002;346:1685–1691 [DOI] [PubMed] [Google Scholar]
- 59.Skyler JS, Krischer JP, Wolfsdorf J, et al. Effects of oral insulin in relatives of patients with type 1 diabetes: the Diabetes Prevention Trial–Type 1. Diabetes Care 2005;28:1068–1076 [DOI] [PubMed] [Google Scholar]
- 60.Mahon JL, Sosenko JM, Rafkin-Mervis L, et al.; TrialNet Natural History Committee; Type 1 Diabetes TrialNet Study Group . The TrialNet Natural History Study of the Development of Type 1 Diabetes: objectives, design, and initial results. Pediatr Diabetes 2009;10:97–104 [DOI] [PubMed] [Google Scholar]
- 61.Ziegler AG, Rewers M, Simell O, et al. Seroconversion to multiple islet autoantibodies and risk of progression to diabetes in children. JAMA 2013;309:2473–2479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Parikka V, Näntö-Salonen K, Saarinen M, et al. Early seroconversion and rapidly increasing autoantibody concentrations predict prepubertal manifestation of type 1 diabetes in children at genetic risk. Diabetologia 2012;55:1926–1936 [DOI] [PubMed] [Google Scholar]
- 63.Greenbaum CJ, Beam CA, Boulware D, et al.; Type 1 Diabetes TrialNet Study Group . Fall in C-peptide during first 2 years from diagnosis: evidence of at least two distinct phases from composite Type 1 Diabetes TrialNet data. Diabetes 2012;61:2066–2073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Davis AK, DuBose SN, Haller MJ, et al. ; T1D Exchange Clinic Network. Prevalence of detectable C-peptide according to age at diagnosis and duration of type 1 diabetes. Diabetes Care 2015;38:476–481 [DOI] [PubMed] [Google Scholar]
- 65.Lovell DJ, Ruperto N, Giannini EH, Martini A. Advances from clinical trials in juvenile idiopathic arthritis. Nat Rev Rheumatol 2013;9:557–563 [DOI] [PubMed] [Google Scholar]
- 66.Orban T, Bundy B, Becker DJ, et al.; Type 1 Diabetes TrialNet Abatacept Study Group . Co-stimulation modulation with abatacept in patients with recent-onset type 1 diabetes: a randomised, double-blind, placebo-controlled trial. Lancet 2011;378:412–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wherrett DK, Bundy B, Becker DJ, et al.; Type 1 Diabetes TrialNet GAD Study Group . Antigen-based therapy with glutamic acid decarboxylase (GAD) vaccine in patients with recent-onset type 1 diabetes: a randomised double-blind trial. Lancet 2011;378:319–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Moran A, Bundy B, Becker DJ, et al.; Type 1 Diabetes TrialNet Canakinumab Study Group; AIDA Study Group . Interleukin-1 antagonism in type 1 diabetes of recent onset: two multicentre, randomised, double-blind, placebo-controlled trials. Lancet 2013;381:1905–1915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pescovitz MD, Greenbaum CJ, Krause-Steinrauf H, et al.; Type 1 Diabetes TrialNet Anti-CD20 Study Group . Rituximab, B-lymphocyte depletion, and preservation of beta-cell function. N Engl J Med 2009;361:2143–2152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Herold KC, Hagopian W, Auger JA, et al. Anti-CD3 monoclonal antibody in new-onset type 1 diabetes mellitus. N Engl J Med 2002;346:1692–1698 [DOI] [PubMed] [Google Scholar]
- 71.Herold KC, Gitelman SE, Ehlers MR, et al.; AbATE Study Team . Teplizumab (anti-CD3 mAb) treatment preserves C-peptide responses in patients with new-onset type 1 diabetes in a randomized controlled trial: metabolic and immunologic features at baseline identify a subgroup of responders. Diabetes 2013;62:3766–3774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Keymeulen B, Vandemeulebroucke E, Ziegler AG, et al. Insulin needs after CD3-antibody therapy in new-onset type 1 diabetes. N Engl J Med 2005;352:2598–2608 [DOI] [PubMed] [Google Scholar]
- 73.Hagopian W, Ferry RJ Jr, Sherry N, et al.; Protégé Trial Investigators . Teplizumab preserves C-peptide in recent-onset type 1 diabetes: two-year results from the randomized, placebo-controlled Protégé trial. Diabetes 2013;62:3901–3908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gitelman SE, Gottlieb PA, Rigby MR, et al.; START Study Team . Antithymocyte globulin treatment for patients with recent-onset type 1 diabetes: 12-month results of a randomised, placebo-controlled, phase 2 trial. Lancet Diabetes Endocrinol 2013;1:306–316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sherry N, Hagopian W, Ludvigsson J, et al.; Protégé Trial Investigators . Teplizumab for treatment of type 1 diabetes (Protégé study): 1-year results from a randomised, placebo-controlled trial. Lancet 2011;378:487–497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.U.S. Food and Drug Administration. Pediatric Product Development [Internet]. Available from http://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/ucm049867.htm. Accessed 2 June 2015
- 77.European Medicines Agency. Paediatric-Medicine Development [Internet]. Available from http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/general/general_content_000023.jsp. Accessed 3 June 2015
- 78.European Medicines Agency. Paediatric Regulation [Internet]. Available from http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/document_listing/document_listing_000068.jsp&mid=WC0b01ac0580025b8b. Accessed 2 June 2015
- 79.European Medicines Agency. Guideline on Clinical Investigation of Medicinal Products in the Treatment or Prevention of Diabetes Mellitus [Internet]. Available from http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2012/06/WC500129256.pdf. Accessed 2 June 2015
- 80.U.S. Food and Drug Administration. Guidance for Industry: Diabetes Mellitus: Developing Drugs and Therapeutic Biologics for Treatment and Prevention [Internet]. Available from http://www.fda.gov/downloads/Drugs/Guidances/ucm071624.pdf. Accessed 2 June 2015
- 81.U.S. Food and Drug Administration. Designating an Orphan Product: Drugs and Biological Products [Internet]. Available from http://www.fda.gov/ForIndustry/DevelopingProductsforRareDiseasesConditions/HowtoapplyforOrphanProductDesignation/default.htm. Accessed 2 June 2015
- 82.European Medicines Agency. Orphan Designation [Internet]. Available from http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/general/general_content_000029.jsp&mid=WC0b01ac05800240ce. Accessed 2 June 2015
- 83.Institute of Medicine (US) Committee on Clinical Research Involving Children Ethical Conduct of Clinical Research Involving Children [Internet]. Field MJ, Behrman RE, Eds. Washington, DC, The National Academies Press, 2004. Available from http://www.ncbi.nlm.nih.gov/books/NBK25557/. Accessed 2 June 2015 [PubMed] [Google Scholar]
- 84.Gill D; Ethics Working Group of the Confederation of European Specialists in Paediatrics . Ethical principles and operational guidelines for good clinical practice in paediatric research. Recommendations of the Ethics Working Group of the Confederation of European Specialists in Paediatrics (CESP). Eur J Pediatr 2004;163:53–57 [DOI] [PubMed] [Google Scholar]
- 85.Wendler D. Is it possible to protect pediatric research subjects without blocking appropriate research? J Pediatr 2008;152:467–470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sammons HM, Malhotra J, Choonara I, Sitar DS, Matsui D, Rieder MJ. British and Canadian views on the ethics of paediatric clinical trials. Eur J Clin Pharmacol 2007;63:431–436 [DOI] [PubMed] [Google Scholar]
- 87.Wang D, Bahm AL, Seabrook JA, Sammons HM, Rieder MJ. A survey of Canadian medical student attitudes towards the ethics of pediatric clinical trials: are they different from Canadian and British health care professionals? J Popul Ther Clin Pharmacol 2011;18:e10–e16 [PubMed] [Google Scholar]
- 88.Wendler D, Jenkins T. Children’s and their parents’ views on facing research risks for the benefit of others. Arch Pediatr Adolesc Med 2008;162:9–14 [DOI] [PubMed] [Google Scholar]
- 89.Wendler D, Abdoler E, Wiener L, Grady C. Views of adolescents and parents on pediatric research without the potential for clinical benefit. Pediatrics 2012;130:692–699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ondrusek N, Abramovitch R, Pencharz P, Koren G. Empirical examination of the ability of children to consent to clinical research. J Med Ethics 1998;24:158–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Macaubas C, Nguyen K, Milojevic D, Park JL, Mellins ED. Oligoarticular and polyarticular JIA: epidemiology and pathogenesis. Nat Rev Rheumatol 2009;5:616–626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wallace CA, Giannini EH, Spalding SJ, et al.; Childhood Arthritis and Rheumatology Research Alliance (CARRA) . Clinically inactive disease in a cohort of children with new-onset polyarticular juvenile idiopathic arthritis treated with early aggressive therapy: time to achievement, total duration, and predictors. J Rheumatol 2014;41:1163–1170 [DOI] [PubMed] [Google Scholar]
- 93.Gottlieb PA, Quinlan S, Krause-Steinrauf H, et al.; Type 1 Diabetes TrialNet MMF/DZB Study Group . Failure to preserve β-cell function with mycophenolate mofetil and daclizumab combined therapy in patients with new-onset type 1 diabetes. Diabetes Care 2010;33:826–832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Buckingham B, Beck RW, Ruedy KJ, et al.; Diabetes Research in Children Network (DirecNet) Study Group; Type 1 Diabetes TrialNet Study Group . Effectiveness of early intensive therapy on β-cell preservation in type 1 diabetes. Diabetes Care 2013;36:4030–4035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gale EA, Bingley PJ, Emmett CL, Collier T; European Nicotinamide Diabetes Intervention Trial (ENDIT) Group. European Nicotinamide Diabetes Intervention Trial (ENDIT): a randomised controlled trial of intervention before the onset of type 1 diabetes. Lancet Lond Engl 2004;363:925–931 [DOI] [PubMed] [Google Scholar]
- 96.Knip M, Åkerblom HK, Becker D, et al.; TRIGR Study Group . Hydrolyzed infant formula and early β-cell autoimmunity: a randomized clinical trial. JAMA 2014;311:2279–2287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chase HP, Boulware D, Rodriguez H, et al.; Type 1 Diabetes TrialNet Nutritional Intervention to Prevent (NIP) Type 1 Diabetes Study Group . Effect of docosahexaenoic acid supplementation on inflammatory cytokine levels in infants at high genetic risk for type 1 diabetes. Pediatr Diabetes 2015;16:271–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Palmer JP, Fleming GA, Greenbaum CJ, et al. C-peptide is the appropriate outcome measure for type 1 diabetes clinical trials to preserve beta-cell function: report of an ADA workshop, 21-22 October 2001. Diabetes 2004;53:250–264 [DOI] [PubMed] [Google Scholar]
- 99.Näntö-Salonen K, Kupila A, Simell S, et al. Nasal insulin to prevent type 1 diabetes in children with HLA genotypes and autoantibodies conferring increased risk of disease: a double-blind, randomised controlled trial. Lancet 2008;372:1746–1755 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.