Abstract
Optimized glycemic control prevents and slows the progression of long-term complications in patients with type 1 and type 2 diabetes. In healthy individuals, a decrease in plasma glucose below the physiological range triggers defensive counterregulatory responses that restore euglycemia. Many individuals with diabetes harbor defects in their defenses against hypoglycemia, making iatrogenic hypoglycemia the Achilles heel of glycemic control. This Profile in Progress focuses on the seminal contributions of Philip E. Cryer, MD, to our understanding of hypoglycemia and glucose counterregulation, particularly his discovery of the syndrome of hypoglycemia-associated autonomic failure (HAAF).
Philip E. Cryer, as a mature professor and as a U.S. Naval officer.
Early Promise Fulfilled
Philip E. Cryer was born in 1940 in El Paso, IL, where his father was a country doctor. The founding of the American Diabetes Association (ADA) in the same year was an interesting coincidence, given his later career path in diabetes research and his leadership role in the ADA. An outstanding student, Cryer was valedictorian of his high school class in 1958 and a Phi Beta Kappa graduate (1962) of Northwestern University in Evanston, IL. He obtained his MD (Alpha Omega Alpha) from the same institution in 1965, with “highest distinction.” Cryer received clinical and research training in endocrinology and metabolism under the direction of Drs. William H. Daughaday and David M. Kipnis at Barnes Hospital/Washington University School of Medicine in St. Louis (St. Louis, MO). After his completion of endocrinology training in 1969, he served in the U.S. Navy at the Naval Medical Research Institute in Bethesda, MD, until 1971. After that, he returned to Barnes Hospital/Washington University School of Medicine in St. Louis, where he has spent his entire career.
Cryer rose to leadership positions at the Washington University School of Medicine. He was director of the Division of Endocrinology, Diabetes and Metabolism (1985–2002), director of the General Clinical Research Center (GCRC) for decades, and associate director of the Diabetes Research Center (2002–2014), among other roles. To his great credit, he led the GCRC through six successful competitive renewal applications to the National Institutes of Health over a period spanning 33 years. Cryer was named the Irene E. and Michael M. Karl Professor of Endocrinology and Metabolism in Medicine at Washington University in St. Louis in 1995, a position he held until he became emeritus in 2014. Despite the numerous demands on his time, Cryer’s major focus has been on patient-oriented, translational research. His research training in the late 1960s included experiences in both clinical research and then–state-of-the-art basic research. His first research publication, with Dr. Daughaday, was on the regulation of growth hormone secretion (1); his second article (with Drs. Jarett and Kipnis), titled “Nucleotide Inhibition of Adenyl Cyclase Activity in Fat Cell Membranes” (2), antedated the discovery of G proteins. Cryer’s independent research work coalesced around the sympathoadrenal system, glucose counterregulation, and hypoglycemia in general. In a career spanning more than four decades, Cryer has contributed three single-authored books, 94 book chapters, and 374 published articles to the medical literature.
Sympathoadrenal System and Glucose Counterregulation
In the 1970s, Cryer developed a sensitive single-isotope derivative (radioenzymatic) assay for catecholamines (3). The advantages of that assay over the original double-isotope derivative method of Engelman et al. (4) included the use of smaller sample volumes and methodological simplicity. By dispensing with the need for internal standards (without compromising accuracy or precision), the Cryer assay also had an edge over the single-isotope derivative method of Passon and Peuler (5). With that tool, Cryer launched pioneering studies on the physiology and pathophysiology of the human sympathoadrenal system (6), as well as mechanistic studies on the metabolic actions of epinephrine in humans (7–10). The achievement of precision and efficiency in the measurement of catecholamines and other hormones enabled Cryer and his colleagues to chronicle the temporal pattern in the secretion of the glucose counterregulatory hormones during insulin-induced hypoglycemia. Those early studies set the stage for the discovery of the physiology of “glucose counterregulation,” a then-novel term that appeared as a running title of the 1976 publication authored by Alan Garber, Cryer, Julio Santiago, Morey Haymond, Anthony Pagliara, and David Kipnis (11).
Hierarchy of Counterregulatory Responses
Subsequent work led by John Gerich and Cryer (12–15) discovered the principles of counterregulatory physiology by clarifying the hierarchy of changes in neuroendocrine hormones, symptoms, and cognitive function in response to decrements in blood glucose. In pivotal studies reported in 1979, Gerich and Cryer (12), along with their colleagues Jonathan Davis, Mara Lorenzi, Robert Rizza, Nancy Bohannon, John Karam, Stephen Lewis, Roy Kaplan, and Thomas Schultz, investigated the mechanisms for recovery of plasma glucose from insulin-induced hypoglycemia in healthy subjects and individuals who had undergone bilateral adrenalectomy. The study protocol included somatostatin infusion to inhibit glucagon and growth hormone secretion, with and without separate infusion of either hormone, to better understand the hierarchy of counterregulatory hormones. Those studies generated the now axiomatic knowledge that glucagon and epinephrine play critical roles, while the immediate contributions of growth hormone and cortisol are less critical, in the hierarchy of counterregulatory responses to acute insulin-induced hypoglycemia. The findings extended previous observations by Robert Brodows, F. Xavier Pi-Sunyer, and Robert Campbell (16) that demonstrated the neurohormonal control of counterregulatory responses during 2-deoxy-glucose–induced glucoprivation in healthy subjects and patients with spinal cord transection.
Hypoglycemia Unawareness
Elucidation of the hierarchy of counterregulatory responses soon was followed by the discovery (by Geremia Bolli, Gerich, Cryer, and colleagues) that these physiological defenses against hypoglycemia were compromised in people with type 1 diabetes (17,18). Those discoveries provided a conceptual framework for understanding hypoglycemia unawareness as the clinical expression of defective glucose counterregulation in people with diabetes. Probing the cause of the loss of glucagon response to hypoglycemia, insightful work from Cryer’s group suggested that β-cell failure (and thus inability to modulate intraislet insulin levels) may be a mechanism for the aglucagonemic response to hypoglycemia (19,20). The neurogenic symptoms of hypoglycemia trigger a behavioral response (carbohydrate consumption) to abort hypoglycemia and restore euglycemia. Patients with hypoglycemia unawareness do not perceive neurogenic warning symptoms and thus are at risk for severe hypoglycemia, neuroglycopenia, coma, seizure, and even death. It had been generally believed that the neurogenic symptoms of hypoglycemia were of adrenomedullary origin (hence the term “adrenergic”). However, given the assessment of neurogenic symptoms, norepinephrine kinetics, and hemodynamic changes under clamped euglycemic and stepped hypoglycemic conditions in healthy subjects and adrenalectomized patients, Cryer convincingly showed that the neurogenic symptoms of hypoglycemia are indeed largely the result of sympathetic neural, rather than adrenomedullary, activation (21). The clinical importance of these observations from studies championed by Cryer and colleagues is underscored by the demonstration that the combination of hypoglycemia unawareness and defective glucose counterregulation confers a 25-fold increased risk for severe hypoglycemia (22,23).
Hypoglycemia Begets Hypoglycemia: Early Clues to a Syndrome
The benefits of glycemic control were clearly demonstrated in the Diabetes Control and Complications Trial (DCCT) (24), but the risk of iatrogenic hypoglycemia did not escape notice (24–26). The overall rates of severe hypoglycemia (including coma and seizure) were 61.2 per 100 patient-years versus 18.7 per 100 patient-years in the intensive and conventional treatment groups, respectively (25,26). DCCT participants who experienced severe hypoglycemia were at increased risk of subsequent episodes. Indeed, approximately one-third of the patients in each group experienced a second episode within the 4 months following the first episode of severe hypoglycemia (25,26). Analysis of several risk factors revealed that the number of prior episodes of hypoglycemia was the strongest predictor of the risk of future hypoglycemia (25,26). Elegant work in the late 1980s by Robert Sherwin and colleagues (27,28) (notably, Stephanie Amiel, Don Simonson, and William Tamborlane) linked strict glycemic control to impaired glucose counterregulation/hypoglycemia unawareness; however, a causal link between the latter and antecedent hypoglycemia had not been established at that time.
Indeed, conventional wisdom of that era had (mis)attributed the cause of hypoglycemia unawareness to diabetic autonomic neuropathy, until a convincing study in 1990 debunked that conclusion (29). Using an extensive battery of tests for autonomic function, Ryder et al. (29) observed that 12 patients with diabetes with hypoglycemia unawareness and 7 patients with defective glucose counterregulation showed “little evidence of autonomic neuropathy.” If not autonomic neuropathy, then what was the cause of impaired counterregulation and hypoglycemia unawareness? Extrapolating from their data, the extant literature (27,28,30), and clinical observations of pseudohypoglycemic symptoms in some normoglycemic (or even hyperglycemic) patients, Ryder et al. (29) speculated that “frequent hypoglycaemia might cause a downward resetting” of putative hypothalamic sites “to explain the hypoglycaemic counterregulatory defect.” From about the late 1980s onward, Cryer’s investigative efforts concentrated on the specific role of hypoglycemia in the etiology of hypoglycemia. Those efforts culminated in his maxim—“hypoglycemia begets hypoglycemia,”quod erat demonstrandum! In 1991, Simon Heller and Cryer (31) demonstrated that a single episode of hypoglycemia in the afternoon impaired the hormonal, neurogenic, and neuroglycopenic symptom responses to subsequent hypoglycemia the following morning in healthy volunteers. Those findings were subsequently replicated in patients with type 1 diabetes who were carefully selected for the absence of autonomic neuropathy (32).
Hypoglycemia-Associated Autonomic Failure
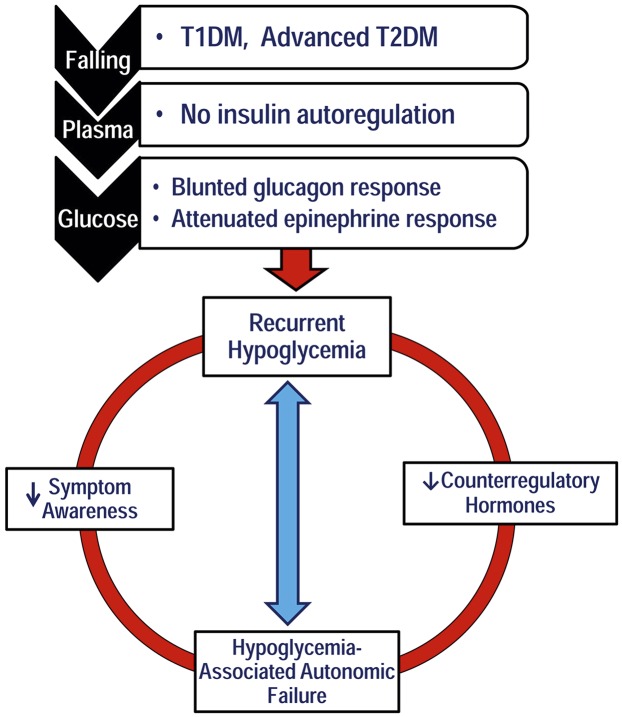
Cryer coined the term hypoglycemia-associated autonomic failure (HAAF) in a review article in 1992 (33) and subsequently used it as the title of the description of the syndrome in a 1993 publication (32). As originally proposed (32,33), the concept of HAAF in diabetes posits that recent antecedent hypoglycemia causes both defective glucose counterregulation and hypoglycemia unawareness during subsequent hypoglycemia, thus creating a vicious cycle of recurrent hypoglycemia (Fig. 1) (34). The syndrome of HAAF was demonstrated in subjects without diabetes (31), in patients with type 1 diabetes (32), and in those with advanced type 2 diabetes (35). Rodent models of HAAF soon appeared (36), and additional features (including decreased baroreflex sensitivity and muscle sympathetic nerve activity) were described following recent antecedent hypoglycemia in humans (37). An important question is whether HAAF is adaptive or maladaptive. Clearly, the vicious cycle of severe iatrogenic hypoglycemia triggered by HAAF is maladaptive. However, HAAF appears to protect against brain damage (38) and fatal cardiac arrhythmias (39) from subsequent severe hypoglycemia in rats, findings that raise the possibility of an adaptive response, somewhat akin to ischemic preconditioning (40). Recurrent hypoglycemia and HAAF also increased gene expression of GAD and levels of the inhibitory neurotransmitter γ-aminobutyric acid (GABA) in rat neurons (41).
Figure 1.
Schematic representation of the concept of HAAF. Adapted with permission from Awoniyi et al. (34). T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus.
Cryer, Washington University School of Medicine in St. Louis (Washington Magazine, Fall 2002, p. 48).
Although recent antecedent hypoglycemia was pivotal in the initial description of HAAF, prior exercise (42) and sleep (43) were demonstrated to induce similar syndromes, thereby linking defective glucose counterregulation to the well-known increased vulnerability to hypoglycemia after exercise and during sleep. Indeed, the demonstration of sleep-induced HAAF by Salomon Banarer and Cryer (43) helps explain the predilection of most episodes of severe hypoglycemia for nocturnal hours (25). Although insulin action is highest at nighttime (44), that factor alone ought not pose a particular hazard for hypoglycemia if counterregulatory function were intact. Cryer often stresses that HAAF is pathophysiologically distinct from classic diabetic autonomic neuropathy—a structural disorder characterized by nerve fiber loss. The veracity of that assertion is underscored by the discovery by Fanelli et al. (45), Amiel and colleagues (46), and Cryer and colleagues (47,48) that components of the HAAF syndrome are reversible in as little as 2–3 weeks of scrupulous avoidance of iatrogenic hypoglycemia. It is now standard clinical practice to recommend cautious relaxation of glycemic control and strict avoidance of hypoglycemia as a therapeutic strategy in patients with recurrent hypoglycemia and HAAF (49,50). Seldom has a research finding found its way so quickly into clinical practice.
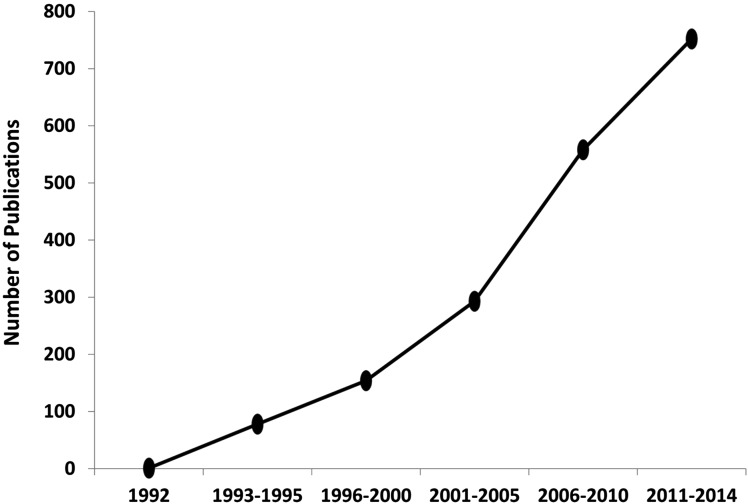
A search of the medical literature showed just one article with specific reference to HAAF in 1992; the term has since appeared in the title, subtitle, or text of several thousand articles (Fig. 2). Twenty-five years ago, few would have imagined that an episode of hypoglycemia could elicit such a panoply of neuroendocrine, electrophysiological, cardiovascular, genomic, biochemical, neurocognitive, and behavioral responses! Cryer opened a Pandora’s box: his healthy infatuation with the mechanisms of hypoglycemia stretched a field far beyond its traditional boundaries, opening up new vistas for inquiry and discovery. Unraveling the intricacies of this new physiology is an ongoing effort in numerous laboratories. To begin with, we do not yet have a unifying mechanism for the myriad manifestations of HAAF. Several groups, including Cryer’s, have been testing a number of interesting potential mechanisms of HAAF (41,51–55). These studies suggest possible contributions from glucocorticoids (52), inhibitory thalamic centers (53), altered gene expression in GABAergic neurons (41), and excitotoxicity pathways (55), among others, as possible mechanisms underlying the syndrome of HAAF. The field opened up by Cryer and a coterie of dedicated hypoglycemia researchers no doubt will continue to intrigue and attract creative minds well into the future.
Figure 2.
Publications with HAAF in the title, subtitle, or text, 1992–2014 (source: Google Scholar).
Family portrait taken circa June 1997. Seated (center): Cryer and Carolyn Havlin-Cryer. From left: Mary Gudermuth Cryer (wife of Philip Clifford Cryer), Justine Laurel Cryer Dugan, Philip Clifford Cryer, Anthony Victor Havlin, Krista Victoria Havlin, and Rebecca Elizabeth Havlin Eberhart.
Case for a New Taxonomy
As originally proposed by Cryer, HAAF is characterized by a clinical or subclinical event (recent antecedent hypoglycemia), biochemical features (defective glucose counterregulation, evidenced by attenuated glucagon and epinephrine responses), and subjective manifestations (absent or impaired awareness of neurogenic symptoms, arising from attenuated sympathetic neural responses to hypoglycemia) (32,33,51,54). Subsequent reports have identified additional features associated with recent antecedent hypoglycemia, including decreased baroreflex sensitivity and muscle sympathetic nerve activity in humans (37). Furthermore, HAAF is associated with neurocognitive/antiarrhythmogenic preconditioning (38,39) and increased GABAergic (41) tone in rodents. The etiology of the syndrome itself has expanded to include exercise (42) and sleep (43); thus, induction of HAAF is no longer restricted to the stimulus of recent antecedent hypoglycemia. Although his disquisitive reviews (51,54) now recognize the diverse causes of HAAF (51,54), Cryer would admit that, semantically, HAAF has become somewhat of a misnomer for a functional autonomic disorder that is inducible by nonhypoglycemic stimuli. The taxonomic mismatch is likely to widen in the future, as additional inducers of HAAF are recognized. Perhaps it is time to consider “Cryer syndrome” as a descriptor for the foundational construct of a reversible autonomic disorder characterized by defective glucose counterregulation, hypoglycemia unawareness, and increased risk for severe hypoglycemia that is induced by antecedent hypoglycemia, prior exercise, sleep, or other putative factors.
Admittedly, the use of eponyms in medicine is in decline, after having peaked in the 1950s (56). Yet, eponyms do have certain advantages, including succinct communication, nosologic synthesis, and diagnostic parsimony. Consider the example of Cushing syndrome: Affected patients could present with weight gain, bruising, striae, osteoporosis, facial plethora, depression, diabetes, hypertension, and hirsutism, among other features. The underlying etiology could be an adrenal tumor, a pituitary tumor, exogenous glucocorticoid exposure, or ectopic ACTH or CRH secretion. Yet, the term Cushing syndrome is immediately informative and directs clinical behavior along established paths. Adoption of Cryer syndrome could deliver a similar parsimonious taxonomy for a complex disorder of diverse etiologies characterized by functional autonomic failure and myriad neuroendocrine, physiological, behavioral, and clinical manifestations. As already noted, the features of Cryer syndrome are reversible (45–48), making it a clinically relevant and treatable syndrome. Pragmatically, a patient with diabetes with a history of severe or recurrent hypoglycemia and hypoglycemia unawareness can be presumed to have Cryer syndrome. Given the impracticality of routine documentation of defective counterregulation in the clinic, a history of hypoglycemia unawareness can be used as a surrogate for defective glucose counterregulation in the setting of recurrent antecedent hypoglycemia. Fortunately, self-reported hypoglycemia awareness status is reliable, as evidenced by assessment of symptom scores during stepped hypoglycemia clamp (47).
One drawback is that eponyms can be fraught with rancorous priority disputes. Witness the eponym in Graves disease, which has been variously substituted with the names of Parry, Basedow, March, Parsons, Flajani, Begbie, and others (57,58). Although Parry first described the condition in 1825, 10 years before Graves and Basedow (57,58), Robert Graves was the first to convincingly link the major diagnostic features of goiter, palpitations, and exophthalmos. The triumph of Graves over other eponyms illustrates Sir Francis Darwin’s dictum that “in science the credit goes to the man who convinces the world, not to the man to whom the idea first occurred” (59).
Back to Cryer
Cryer has had a global impact on the diabetes field through his direct work and the work of the more than 40 fellows he has mentored. The many honors he has received in recognition of his contributions include the Banting Medal for Distinguished Scientific Achievement and the Albert Renold Award (for mentorship), both from the ADA; the Claude Bernard Medal from the European Association for the Study of Diabetes; the Kellion Award from the Australian Diabetes Society; the Rorer Clinical Investigator Award from the Endocrine Society; the David Rumbaugh Scientific Award from JDRF; and an honorary doctorate from the University of Copenhagen, among others. Cryer is the only person in the 75-year history of the ADA to receive its Banting Medal for scientific achievement, serve as editor of its prestigious journal Diabetes, and be elected president of the Association. An advocate for people with diabetes, Cryer frequently reminds his professional colleagues that “hypoglycemia is the limiting factor in the glycemic management of diabetes.” That was the theme of his Banting Lecture (1994) and his Claude Bernard Lecture (2001). Cryer consistently acknowledges the contributions of collaborators and trainees and expresses high regard and gratitude for their collaboration.
Formerly married to Susan Shipman Cryer, Cryer married Carolyn Havlin-Cryer in 1994. Their blended family includes five children—Philip Clifford Cryer, Justine Laurel Cryer Dugan, Anthony Victor Havlin, Krista Victoria Havlin, and Rebecca Elizabeth Havlin Eberhart—and six grandchildren—Kacy Elizabeth Cryer, Benjamin Philip Cryer, Matthew Philip Dugan, Emma Inez Dugan, Mollie Breanne Havlin, and Max Havlin Eberhart. At the time of his retirement from Washington University in St. Louis in 2014, Cryer was greatly honored by the decision of the William and Elaine Wolff Family, including their son Gary Wolff, to endow the Philip E. and Carolyn E. Cryer Professor of Endocrinology and Metabolism Chair at Washington University in St. Louis.
Albeit as a listener and no longer a performer, Cryer is a fan of the tight, four-part harmony of barbershop quartet singing, a classic American art form; he even knows the meaning of the acronym SPEBSQSA! He also enjoys nonmedical reading, mostly of histories and biographies, and counts the American writer and humorist Mark Twain (Samuel Clemens, 1835–1910) and the British mathematician, philosopher, and social critic Bertrand Russell (1872–1970) among his favorite authors. Indeed, Cryer frequently prefaces his lectures with a quote from Russell’s The Conquest of Happiness, first published in 1930: “One of the symptoms of an approaching nervous breakdown is the belief that one’s work is terribly important” (60).
Summary
In closing, work championed by Cryer and others clearly established the legitimacy of a syndrome of functional autonomic failure, defective glucose counterregulation, hypoglycemia unawareness, and increased risk for recurrent severe hypoglycemia. The syndrome is inducible by recent antecedent hypoglycemia, prior exercise, or sleep. Finding a parsimonious descriptor for such a multifarious syndrome that captures the foundational construct and current (and potentially future) diverse etiologies has become a challenge in medical taxonomy. The proposed term Cryer syndrome is an apt, succinct, and attributively congruent solution.
Article Information
Acknowledgments. S.D.-J. was a research fellow in metabolism in Dr. Cryer’s group from 1990 to 1992 and subsequently served as a faculty member in the Division of Endocrinology, Diabetes and Metabolism at the Washington University School of Medicine in St. Louis from 1992 to 2000.
Funding. S.D.-J. is supported, in part, by grants from the National Institutes of Health (R01 DK067269, DK62203, and DK48411).
References
- 1.Cryer PE, Daughaday WH. Regulation of growth hormone secretion in acromegaly. J Clin Endocrinol Metab 1969;29:386–393 [DOI] [PubMed] [Google Scholar]
- 2.Cryer PE, Jarett L, Kipnis DM. Nucleotide inhibition of adenyl cyclase activity in fat cell membranes. Biochim Biophys Acta 1969;177:586–590 [DOI] [PubMed] [Google Scholar]
- 3.Cryer PE, Santiago JV, Shah S. Measurement of norepinephrine and epinephrine in small volumes of human plasma by a single isotope derivative method: response to the upright posture. J Clin Endocrinol Metab 1974;39:1025–1029 [DOI] [PubMed] [Google Scholar]
- 4.Engelman K, Portnoy B, Lovenberg W. A sensitive and specific double-isotope derivative method for the determination of catecholamines in biological specimens. Am J Med Sci 1968;255:259–268 [DOI] [PubMed] [Google Scholar]
- 5.Passon PG, Peuler JD. A simplified radiometric assay for plasma norepinephrine and epinephrine. Anal Biochem 1973;51:618–631 [DOI] [PubMed] [Google Scholar]
- 6.Cryer PE. Physiology and pathophysiology of the human sympathoadrenal neuroendocrine system. N Engl J Med 1980;303:436–444 [DOI] [PubMed] [Google Scholar]
- 7.Rizza RA, Haymond MW, Miles JM, Verdonk CH, Cryer PE, Gerich JE. Effect of alpha adrenergic stimulation and its blockade on glucose turnover in man. Amer J Physiol 1980;238:E467–E472 [DOI] [PubMed] [Google Scholar]
- 8.Rizza RA, Cryer PE, Haymond MW, Gerich JE. Adrenergic mechanisms for the effects of epinephrine on glucose production and clearance in man. J Clin Invest 1980;65:682–689. doi: 10.1172/JCI109714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galster AD, Clutter WE, Cryer PE, Collins JA, Bier DM. Epinephrine plasma thresholds for lipolytic effects in man: measurements of fatty acid transport with [l-13C]palmitic acid. J Clin Invest 1981;67:1729–1738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berk MA, Clutter WE, Skor D, et al. . Enhanced glycemic responsiveness to epinephrine in insulin-dependent diabetes mellitus is the result of the inability to secrete insulin. Augmented insulin secretion normally limits the glycemic, but not the lipolytic or ketogenic, response to epinephrine in humans. J Clin Invest 1985;75:1842–1851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garber AJ, Cryer PE, Santiago JV, Haymond MW, Pagliara AS, Kipnis DM. The role of adrenergic mechanisms in the substrate and hormonal response to insulin-induced hypoglycemia in man. J Clin Invest 1976;58:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gerich J, Davis J, Lorenzi M, et al. . Hormonal mechanisms of recovery from insulin induced hypoglycemia in man. Amer J Physiol 1979;236:E380–E385. [DOI] [PubMed] [Google Scholar]
- 13.Rizza RA, Cryer PE, Gerich JE. Role of glucagon, catecholamines, and growth hormone in human glucose counterregulation. Effects of somatostatin and combined alpha- and beta-adrenergic blockade on plasma glucose recovery and glucose flux rates after insulin-induced hypoglycemia. J Clin Invest 1979;64:62–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwartz NS, Clutter WE, Shah SD, Cryer PE. Glycemic thresholds for activation of glucose counterregulatory systems are higher than the threshold for symptoms. J Clin Invest 1987;79:777–781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mitrakou A, Ryan C, Veneman T, et al. . Hierarchy of glycemic thresholds for counterregulatory hormone secretion, symptoms, and cerebral dysfunction. Am J Physiol 1991;260:E67–E74 [DOI] [PubMed] [Google Scholar]
- 16.Brodows RG, Pi-Sunyer FX, Campbell RG. Neural control of counter-regulatory events during glucopenia in man. J Clin Invest 1973;52:1841–1844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bolli G, Dimitriadis G, Pehling G, et al. . Abnormal glucose counterregulation after subcutaneous insulin in insulin dependent diabetes mellitus: Exaggerated hypoglycemia and rebound hyperglycemia due to multiple counterregulatory hormone deficiencies and abnormal plasma insulin kinetics. N Engl J Med 1984;310:1706–1711 [DOI] [PubMed] [Google Scholar]
- 18.Cryer PE, White NH, Santiago JV. The relevance of glucose counterregulatory systems to patients with insulin dependent diabetes mellitus. Endocrine Reviews 1986;7:131–139 [DOI] [PubMed] [Google Scholar]
- 19.Banarer S, McGregor VP, Cryer PE. Intraislet hyperinsulinemia prevents the glucagon response to hypoglycemia despite an intact autonomic response. Diabetes 2002;51:958–965 [DOI] [PubMed] [Google Scholar]
- 20.Raju B, Cryer PE. Loss of the decrement in intraislet insulin plausibly explains loss of the glucagon response to hypoglycemia in insulin-deficient diabetes: documentation of the intraislet insulin hypothesis in humans. Diabetes 2005;54:757–764 [DOI] [PubMed] [Google Scholar]
- 21.DeRosa MA, Cryer PE. Hypoglycemia and the sympathoadrenal system: neurogenic symptoms are largely the result of sympathetic neural, rather than adrenomedullary, activation. Am J Physiol Endocrinol Metab 2004;287:E32–E41 [DOI] [PubMed] [Google Scholar]
- 22.White NH, Skor DA, Cryer PE, Levandoski LA, Bier DM, Santiago JV. Identification of type I diabetic patients at increased risk for hypoglycemia during intensive therapy. N Engl J Med 1983;308:485–491 [DOI] [PubMed] [Google Scholar]
- 23.Bolli GB, De Feo P, De Cosmo S, et al. . A reliable and reproducible test for adequate glucose counterregulation in type 1 diabetes mellitus. Diabetes 1984;33:732–737 [DOI] [PubMed] [Google Scholar]
- 24.The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 25.The DCCT Research Group Epidemiology of severe hypoglycemia in the diabetes control and complications trial. Am J Med 1991;90:450–459 [PubMed] [Google Scholar]
- 26.The Diabetes Control and Complications Trial Research Group Hypoglycemia in the Diabetes Control and Complications Trial. Diabetes 1997;46:271–286 [PubMed] [Google Scholar]
- 27.Amiel SA, Tamborlane WV, Simonson DC, Sherwin RS. Defective glucose counterregulation after strict glycemic control of insulin-dependent diabetes mellitus. N Engl J Med 1987;316:1376–1383 [DOI] [PubMed] [Google Scholar]
- 28.Amiel SA, Sherwin RS, Simonson DC, Tamborlane WV. Effect of intensive insulin therapy on glycemic thresholds for counterregulatory hormone release. Diabetes 1988;37:901–907 [DOI] [PubMed] [Google Scholar]
- 29.Ryder RE, Owens DR, Hayes TM, Ghatei MA, Bloom SR. Unawareness of hypoglycaemia and inadequate hypoglycaemic counterregulation: no causal relation with diabetic autonomic neuropathy. BMJ 1990;301:783–787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heller SR, Macdonald IA, Herbert M, Tattersall RB. Influence of sympathetic nervous system on hypoglycaemic warning symptoms. Lancet 1987;2:359–363 [DOI] [PubMed] [Google Scholar]
- 31.Heller SR, Cryer PE. Reduced neuroendocrine and symptomatic responses to subsequent hypoglycemia after 1 episode of hypoglycemia in nondiabetic humans. Diabetes 1991;40:223–226 [DOI] [PubMed] [Google Scholar]
- 32.Dagogo-Jack SE, Craft S, Cryer PE. Hypoglycemia-associated autonomic failure in insulin-dependent diabetes mellitus. Recent antecedent hypoglycemia reduces autonomic responses to, symptoms of, and defense against subsequent hypoglycemia. J Clin Invest 1993;91:819–828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cryer PE. Iatrogenic hypoglycemia as a cause of hypoglycemia-associated autonomic failure in IDDM. A vicious cycle. Diabetes 1992;41:255–260 [DOI] [PubMed] [Google Scholar]
- 34.Awoniyi O, Rehman R, Dagogo-Jack S. Hypoglycemia in patients with type 1 diabetes: epidemiology, pathogenesis, and prevention. Curr Diab Rep 2013;13:669–678 [DOI] [PubMed] [Google Scholar]
- 35.Segel SA, Paramore DS, Cryer PE. Hypoglycemia-associated autonomic failure in advanced type 2 diabetes. Diabetes 2002;51:724–733 [DOI] [PubMed] [Google Scholar]
- 36.Powell AM, Sherwin RS, Shulman GI. Impaired hormonal responses to hypoglycemia in spontaneously diabetic and recurrently hypoglycemic rats. Reversibility and stimulus specificity of the deficits. J Clin Invest 1993;92:2667–2674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adler GK, Bonyhay I, Failing H, Waring E, Dotson S, Freeman R. Antecedent hypoglycemia impairs autonomic cardiovascular function: implications for rigorous glycemic control. Diabetes 2009;58:360–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Puente EC, Silverstein J, Bree AJ, et al. . Recurrent moderate hypoglycemia ameliorates brain damage and cognitive dysfunction induced by severe hypoglycemia. Diabetes 2010;59:1055–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reno CM, Daphna-Iken D, Chen YS, VanderWeele J, Jethi K, Fisher SJ. Severe hypoglycemia-induced lethal cardiac arrhythmias are mediated by sympathoadrenal activation. Diabetes 2013;62:3570–3581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gidday JM. Cerebral preconditioning and ischaemic tolerance. Nat Rev Neurosci 2006;7:437–448 [DOI] [PubMed] [Google Scholar]
- 41.Chan O, Cheng H, Herzog R, et al. . Increased GABAergic tone in the ventromedial hypothalamus contributes to suppression of counterregulatory responses after antecedent hypoglycemia. Diabetes 2008;57:1363–1370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Galassetti P, Mann S, Tate D, et al. . Effects of antecedent prolonged exercise on subsequent counterregulatory responses to hypoglycemia. Am J Physiol Endocrinol Metab 2001;280:E908–E917 [DOI] [PubMed] [Google Scholar]
- 43.Banarer S, Cryer PE. Sleep-related hypoglycemia-associated autonomic failure in type 1 diabetes: reduced awakening from sleep during hypoglycemia. Diabetes 2003;52:1195–1203 [DOI] [PubMed] [Google Scholar]
- 44.Boden G, Chen X, Urbain JL. Evidence for a circadian rhythm of insulin sensitivity in patients with NIDDM caused by cyclic changes in hepatic glucose production. Diabetes 1996;45:1044–1050 [DOI] [PubMed] [Google Scholar]
- 45.Fanelli CG, Epifano L, Rambotti AM, et al. . Meticulous prevention of hypoglycemia normalizes the glycemic thresholds and magnitude of most of neuroendocrine responses to, symptoms of, and cognitive function during hypoglycemia in intensively treated patients with short-term IDDM. Diabetes 1993;42:1683–1689 [DOI] [PubMed] [Google Scholar]
- 46.Cranston I, Lomas J, Maran A, Macdonald I, Amiel SA. Restoration of hypoglycaemia awareness in patients with long-duration insulin-dependent diabetes. Lancet 1994;344:283–287 [DOI] [PubMed] [Google Scholar]
- 47.Dagogo-Jack S, Rattarasarn C, Cryer PE. Reversal of hypoglycemia unawareness, but not defective glucose counterregulation, in IDDM. Diabetes 1994;43:1426–1434 [DOI] [PubMed] [Google Scholar]
- 48.Dagogo-Jack S, Fanelli CG, Cryer PE. Durable reversal of hypoglycemia unawareness in patients with type 1 diabetes. Diabetes Care 1999;22:866–867 [DOI] [PubMed] [Google Scholar]
- 49.Seaquist ER, Anderson J, Childs B, et al. . Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care 2013;36:1384–1395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.American Diabetes Association Glycemic targets. Sec. 6. In Standards of Medical in Diabetes—2015. Diabetes Care 2015;38(Suppl. 1):S33–S40 [DOI] [PubMed] [Google Scholar]
- 51.Cryer PE. Diverse causes of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med 2004;350:2272–2279 [DOI] [PubMed] [Google Scholar]
- 52.Bao S, Briscoe VJ, Tate DB, Davis SN. Effects of differing antecedent increases of plasma cortisol on counterregulatory responses during subsequent exercise in type 1 diabetes. Diabetes 2009;58:2100–2108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Arbelaez AM, Powers WJ, Videen TO, Price JL, Cryer PE. Attenuation of counterregulatory responses to recurrent hypoglycemia by active thalamic inhibition. A mechanism for hypoglycemia-associated autonomic failure. Diabetes 2008;57:470–475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cryer PE. Mechanisms of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med 2013;369:362–372 [DOI] [PubMed] [Google Scholar]
- 55.Terpstra M, Moheet A, Kumar A, Eberly LE, Seaquist E, Öz G. Changes in human brain glutamate concentration during hypoglycemia: insights into cerebral adaptations in hypoglycemia-associated autonomic failure in type 1 diabetes. J Cereb Blood Flow Metab 2014;34:876–882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aronson JK. Medical eponyms: taxonomies, natural history, and the evidence. BMJ 2014;349:g7586. [DOI] [PubMed] [Google Scholar]
- 57.Weetman AP. Graves’ disease. N Engl J Med 2000;343:1236–1248 [DOI] [PubMed] [Google Scholar]
- 58.Saraci G, Treta A. Ocular changes and approaches of ophthalmopathy in Basedow - Graves- Parry- Flajani disease. Maedica (Buchar) 2011;6:146–152 [PMC free article] [PubMed] [Google Scholar]
- 59.Darwin F. Francis Galton, 1822–1911. Eugenics Review 1914;6:1–1721259581 [Google Scholar]
- 60.Russell B. The Conquest of Happiness. W. W. Norton & Company, Inc., New York, 2013, p. 72 [Google Scholar]