Abstract
Using daily diary data, this study examined the associations between positive and negative parent-youth experiences and youth cortisol and physical health symptoms among a sample of adolescents (N=132, Mean Age = 13.39). On days when girls reported more negative experiences than usual, they exhibited more physical health symptoms and flatter evening cortisol slopes than usual. Negative experiences with mothers were associated with higher dinner and bedtime youth cortisol levels (between-person). Daily positive experiences with fathers were linked with lower dinner cortisol levels. Youth with high levels of negative experiences, on average, were less sensitive to daily variation in negative experiences than youth who experienced lower parental negativity. We discuss the benefits of a daily diary approach.
Keywords: cortisol, daily diary methods, HPA axis, physical health symptoms, parent-child relationships
Poor parent-youth relationships in childhood predict physical health problems in adulthood. For example, youth who experience harsh parenting or are maltreated are more likely to experience heart disease and cancer later in life (Miller, Chen, & Parker, 2011; Repetti, Robles & Reynolds, 2011; Russek, & Schwartz, 1997; Wegman & Stetler, 2009). Although long-term patterns linking parenting and physical health seem evident, we know little about the proximal effects of everyday experiences with parents on youth physical health. Such information would better our understanding of the links between experiences with parents and later health problems (Repetti et al., 2011). By extension, less extreme stressors in the parent-child relationship such as harsh parenting or cold and unsupportive parent-youth relationships may give rise to later health problems through their impact on youths’ everyday somatic symptoms, such as headaches and stomachaches, and their stress-related physiology, including the operation of the hypothalamic-pituitary-adrenocortical (HPA) system, the effects of which may cumulate over the life course (Repetti et al., 2011). Accordingly, this study used a daily diary approach to investigate the links between daily positive and negative parent-youth experiences and both youth cortisol levels, a biomarker of HPA axis functioning, and youth-reported physical health symptoms. We also moved beyond testing a universal model of these processes to determine whether the links between daily parent-youth experiences and both daily physical health and cortisol were moderated by youth or parent gender or by youths’ average experiences with their parents.
Daily Positive and Negative Experiences
Many theories and models of parenting are grounded in the assumption that positive and negative experiences with parents may be highly stable (e.g., parenting style; Baumrind, 1991). Probably for this reason, many studies of parenting and youth outcomes rely on global reports. Yet, youths’ experiences with their parents may vary from day to day: Some days may be filled with more negative experiences (e.g., conflict, parental harshness, criticism) or positive parent-youth experiences (e.g., warmth, praise, parental interest in youths’ activities) than others. This variation is not captured in studies that rely on global measures (Almeida, 2005). Further, the absence of a positive experience may be distinct from the occurrence of a negative experience with correspondingly different implications for youth HPA functioning and physical health (Dallaire et al., 2006). Accordingly, in this study we assessed positive and negative experiences with parents as distinct constructs and examined their linkages with youth physical health symptoms and diurnal patterns and levels of cortisol.
A Family Risk Perspective
A family risk perspective (Repetti et al., 2011) posits that repeated exposure to daily hassles and stressors, such as conflicts with parents or harsh and unsupportive parent-youth interactions, can have negative implications for youths’ neuroendocrine systems, as evidenced in the operation of the HPA axis, and for their physical health. Indeed, studies on adults find daily hassles and stressors are linked to both cortisol and physical health (Almeida, McGonagle & King, 2009; Odgers & Jaffee, 2013; Piazza, Charles, Sliwinski, Mogle, & Almeida, 2013) as well as physical illness and mortality (Piazza et al., 2013). We built on the research on stress and health in adulthood to study the role of daily experiences with parents in adolescents’ cortisol and physical health symptoms. A day filled with negative parent-youth exchanges may be stressful for youth-- with proximal implications for their health and stress physiology on that particular day. Further, repeated HPA responses across time may strain the stress physiology system (Charles, Piazza, Mogle, Sliwinski, & Almeida, 2013; Repetti et al., 2011). Thus, daily stressful parent-child interactions that occur repeatedly may lead to chronic stress such that youth who have frequent negative experiences with parents respond differently to negative events than youth who experience parental negativity less often. In contrast, a day filled with positive parent-youth experiences may mitigate youths’ physical health symptoms and promote healthy HPA functioning. Collecting daily data on youths’ experiences with parents and their health and cortisol allows for analysis of both daily linkages and cross-time average linkages between parenting and youth functioning.
Animal studies, wherein researchers experimentally manipulate stress have found strong evidence of linkages between early parental experiences and a host of physical diseases, suggesting that causal mechanisms are at play (Miller et al., 2011), but the processes linking stress to disease in humans are not yet clear (Adam, Hawkley, Kudielka & Cacioppo, 2006). Miller, Chen, and Parker (2011) have proposed a Biological Embedding of Childhood Adversity Model, which holds that stressors impact inflammatory processes that in turn affect cortisol, which is released to reduce inflammation. As such, both cortisol and chronic inflammatory processes may play a key role in the development of disease. Indeed, studies of adults show that diurnal patterns and levels of cortisol were associated with an increased risk of disease as well as disruption of immune processes that may increase the risk of disease (Kemeny, 2003; Miller et al., 2011; Neeck, Federlin, Graef., Rusch Schmidt, 1990; Repetti et al., 2011). Although cross-sectional studies have established linkages between cortisol and physical health, the long-term relations and causal mechanisms linking cortisol and physical health are not fully established (Adam et al., 2006). Because of this, we study HPA functioning and physical health symptoms separately in this study.
Family Impacts on Youth HPA Functioning
Healthy patterns of cortisol are marked by a diurnal rhythm wherein cortisol levels peak shortly after waking and then decline over the course of the day (McEwen, 1998). A dysregulated HPA system is characterized by either hypercortisolism (over-reactivity) or hypocortisolism (underactivity) (McEwen, 1998; Sturge-Apple, Davies, Cicchetti, & Manning, 2012). Stressful parent-youth interactions such as harsh, cold, or critical parenting may trigger over-reactivity in youths’ HPA systems such that elevated levels of cortisol do not decrease across the course of the day-- a hypercortisolism response. In this study, high levels of youth cortisol assayed from saliva samples taken before dinner and at bedtime were conceptualized as markers of hypercortisolism. Alternatively, chronic stress exposure and negative parent-child interactions may cause the HPA axis to become less reactive to stressors, as marked by lower levels of cortisol, because the system fails to activate in response to stressful situations (Sturge-Apple, Skibo, Rogosch,, Ignjatovic, & Heinzelman, 2011). Both hypercortisolism and hypocortisolism have been linked to long-term health problems (Adam & Kumari, 2009; Piazza et al., 2013).
Despite the central role of parent-youth relationships in youth psychological and behavioral adjustment, few studies have explored links between these relationships and youth HPA functioning in a normative context. Many studies have examined the effects of extreme parental negativity, such as maltreatment and abuse, or the role of family conflict and violence in HPA axis functioning. Youth in these circumstances may exhibit an inability to regulate arousal processes, such as calming down after a stressful interaction (Cicchetti & Rogosch, 2001; Pollack, Vardi, Putzer Bechner, & Curtin, 2005) and dysregulated cortisol patterns, including blunted morning rise or high evening levels (Gonzales et al, 2012; Miller et al., 2011). Yet, parental negativity need not be extreme for it to influence HPA functioning. Everyday negative experiences with parents or even the lack of positive experiences may engender stress and impact HPA functioning (Odgers & Jaffee, 2013).
Little is known, however, about whether and how everyday positive and negative experiences with parents’ have implications for HPA functioning, especially during adolescence (Odgers & Jaffee, 2013). Most extant studies focus on infants and toddlers, and findings are mixed (Gunnar & Quevedo, 2007). For example, maternal insensitivity during infancy and toddlerhood was linked to higher levels of cortisol and a compromised ability to recover from an induced stressful event in some studies (Albers, Riksen-Walraven, Sweep, & Weerth, 2008; Spangler & Schieche,1994) but not in others (Jansen, Beijers, Riksen-Walraven, & de Weerth, 2010). Parent-child conflict has also been linked to flatter cortisol slopes across the day and lower waking cortisol levels among preschoolers (Slatcher & Robles, 2012). Findings from the few studies of older children and adolescents also are inconsistent. Strained relationships were linked to lower morning cortisol levels among adolescents (Byrd-Craven, Auer, Granger, & Massey, 2012), but another study found no linkages between parental rejection and youth basal cortisol levels (Marsman et al, 2012). Findings are also mixed regarding the role of positive experiences. Positive parent-child relationships have been linked to basal cortisol levels (Marsman et al., 2012) and steeper diurnal cortisol slopes (Pendry & Adam, 2007) in some studies. However, Smeekens, Riksen-Walraven, & Van Bakel, (2007) found that only negative, but not positive parent-child interactions were linked to cortisol levels following a stress-inducing discussion task. To address these inconsistencies, in this study we moved beyond a universal model to test potential moderators of the links between positive and negative parent-child experiences and youth HPA functioning.
Parent-Youth Experiences and Linkages to Youth Physical Health
Stressful family interactions may also impact youth physical health such as whether or not youth experience colds, flus, and other physical symptoms. Parental maltreatment, for example, predicts cardiovascular disease and autoimmune disorders later in adulthood (see Wegman & Stetler, 2009 for a meta-analysis), and maltreated youth also exhibit more proximal reactions in the form of somatic symptoms such as stomachaches and headaches (Gonzales et al., 2012; Miller et al., 2011). Harsh and unsupportive parenting is associated with immune system pro-inflammatory responses (Miller et al., 2011; Kiecolt-Glaser et al., 2011), physical health symptoms (Gottman, Katz, & Hooven, 1996) and increased risk for illnesses such as asthma (Lim, Wood, & Miller, 2008; Wood et al., 2006). Toward illuminating the proximal links between stressors and physical health, we used a daily diary approach to test the associations between negative and positive experiences with parents and youths’ reports of their physical health symptoms.
The Role of Gender in Links between Parent-Youth Relationships and Youth Health
One way that we move beyond a universal model is to test the roles of both youth and parent gender in the links between parenting and both youth HPA functioning and physical health symptoms. Several lines of study led us to hypothesize that these linkages would be stronger for girls than for boys. First, theory and research document that girls tend to more oriented to interpersonal relationships than boys (Maccoby, 1998), and in turn, may be more sensitive to interpersonal stressors (Hankin & Abramson, 2001; Kessler, Ronald, & McLeod, 1984; Leaper, 2002), including negative experiences with parents (Leaper, 2002; McHale, Crouter, & Whiteman, 2003; Pasterski, Golombok, & Hines, 2011). Other studies indicate that girls take longer than boys to recover from stressful experiences, and may have higher levels of cortisol output as well (Nolen-Hoeksema, 2001; Pendry & Adam, 2007). Thus girls may find negative experiences to be more stressful than boys and react more strongly to parental negativity.
Parent gender may also moderate the effects of parent-youth experiences on youth HPA functioning and physical health. Most literature focuses on relationships with mothers (Gunnar & Quevedo, 2007), so an important step is to assess the role of father-child relationships in youth stress processes and health outcomes (Byrd-Craven et al., 2012). In line with theories of gender, youth tend to be closer to their mothers, and mothers tend to be more involved with their children than fathers (McHale et al., 2003). As such, maternal influences on youth health may be stronger than paternal influences (Hastings, McShane, Parker, & Ladha, 2007). Accordingly, we tested the hypothesis that relationships with mothers would have stronger associations with youth cortisol and physical health than relationships with fathers.
The Larger Context of Youth’s Experiences with Parents
Daily experiences with parents take place within a larger relationship context, and the larger context of youth experiences may have implications for how youth react to positive and negative experiences with their parents on any given day. For example, youth who have infrequent negative experiences with their parents may find negative interactions to be highly stressful and exhibit corresponding increases in their cortisol levels or physical health symptoms. In contrast, youth whose experiences with parents are generally more negative may exhibit hyper- or hypocortisol patterns, maintaining higher levels of cortisol even on days with no parental stressors, or exhibiting a blunted diurnal pattern, consistent with a chronic stress response (Sturge-Apple et al. 2012). In a similar way, the relation between positive parent-youth experiences and youth’s physical health symptoms also may vary depending on average levels of positivity in parent-youth relationships. Moving beyond a universal model and in an effort to better understand the role of the larger relationship context in youth reactions to parent positivity and negativity, we tested whether the average level of negative parent-youth experiences and/or positive parent-youth experiences moderated the link between youths’ daily experiences with parents and their daily health.
A Daily Diary Approach
Mixed findings of prior research on the role of parent-youth relationships in youth HPA functioning also may be attributable to methodological factors, including differences in study designs and sample characteristics. For example, some studies were conducted in laboratory settings which allow for a high level of experimenter control but are less ecologically valid (Spangler & Schieche, 1994). Other studies measured cortisol in natural settings to increase ecological validity, but relied on experimenter-imposed tasks conducted at a single point in time to study stress responses (Smeekens et al., 2007). Studies also vary in how parenting is measured (Albers, et al., 2008). Studies that rely on global self-reports, especially retrospective reports, can be limited by social desirability biases, memory demands, and the need for mental arithmetic as when estimates of frequency are averaged over long periods of time (Almeida, 2005).
Daily diary studies may shed new light on the links between positive and negative experiences with parents and youth HPA functioning and physical health because they examine life “as it is lived” (Bolger, Davis, & Rafaeli, 2003), thereby enhancing ecological validity. Diary designs also capture that some days are characterized by more negative or positive parent-youth experiences than other days—that is, that individuals and families often differ as much from themselves on a day to day basis as they differ from other families (Almeida, 2005; Bolger, et al., 2003). In addition, analyses of diary data can be set up to control for stable between-person differences, or selection effects, and thereby allow for stronger inferences about the links between experiences with parents and youth HPA functioning and physical health. Finally, as noted, this approach can illuminate proximal processes that may link parent-youth experiences to youth health. For these reasons, in this study we used a daily diary approach, collecting data on eight consecutive days, to examine the links between youth’s experiences of negativity and positivity with parents and their physical health symptoms and HPA functioning.
The Current Study
In sum, this study addressed three goals. First, we assessed the links between youths’ positive and negative experiences with parents and their daily physical health and cortisol, testing two kinds of hypotheses (a) that youth who reported more negative experiences, on average, would also report more physical health symptoms and exhibit less healthy patterns of cortisol (i.e., between-person effects); and (b) controlling for average parenting, on days when youth experienced more negative parent-youth experiences than usual, they would also exhibit more physical health symptoms and less healthy patterns of cortisol than usual (i.e., within-person effects). We also expected that youth’s positive experiences with their parents would be linked to fewer physical health symptoms and more healthy patterns of cortisol at both the between- and within-person levels. Our second goal was to explore whether the links between parent-youth experiences and youth health were moderated by youth or parent gender. We expected to find stronger associations between parent-youth relationships and health outcomes for girls than boys and for experiences with mothers than fathers. Our third goal was to determine whether youths’ average levels of negative and positive experiences with parents moderated the effects of daily parent-youth experiences on daily health. Here we tested the hypothesis that the within-person links between parenting and youth health would be stronger for youth who experienced lower average levels of parent negativity. Further, we expected that youth who experienced high average levels of parental negativity would also exhibit unhealthy patterns of cortisol on days when they experience less negativity than usual (e.g., high levels of cortisol before dinner and at bedtime or a flatter dinner to bedtime slope). We also expected that the within-person links between positive parenting and youth cortisol and physical health would be stronger for youth who experienced less positive parenting, on average.
Method
Participants
The study used data from a subsample of families that participated in the daily diary component of the Work, Family Health Network Study, a study of a workplace intervention designed to reduce work-family conflict and improve the health of employees and their families (Bray et al., 2013; King et al., 2012). Participants for the current analyses included 132 employees (45% female; mean age = 45.24, SD = 6.30) from the larger sample of workers in an information technology division of a Fortune 500 company, and their child, aged 9–17 who lived with them for at least four days a week. During recruitment, parents were given a brochure describing the daily diary portion of the study and asked if their child would be willing to participate. The employee-parent signed separate consent forms for his/her own and child’s participation, and youth assent was provided during home interviews that followed the employee workplace interviews. Families in which both employee and youth agreed to do the diary calls and saliva collection were eligible to participate in the diary data collection. Eighty four percent of parents and 88% of youth who agreed to participate in the diary component of the study completed all eight days of interviews.
The majority of youth were White (59%); 3% were African American, 15% were Hispanic, 11% were Indian Asian, 7% were other Asian, less than 1% were American Indian/Alaska Native or Pacific Islander, and 3% chose more than one race/ethnicity. Most parents graduated from college (78%), and their annual incomes averaged between $110,000 and $119,999. Most parents were married (81%), 6% were cohabiting, and 13% were single. Youth (55% female) averaged 13.39 years of age (SD = 2.40).
Procedures
Employee-parents and their children provided information on their daily activities, emotions, and experiences via telephone calls on 8 consecutive evenings (Mdn youth interview start time = 8:01 PM, SD = 1.62 hrs.). On four of the diary days (days 2, 3, 4, and 5), saliva samples were collected from youth at four time points: upon awakening - before getting out of bed, 30 minutes after waking, before dinner, and before going to bed. Of the youth who participated in the diary calls, 96% (N = 126) also provided saliva samples, yielding a total of 1829 samples. During the home interviews, saliva collection kits with instructions were provided to participating families. Each kit contained 16 salivettes for collecting youth cortisol (4 salivettes a day and samples were collected for a total 4 days) along with a DVD that demonstrated saliva collection. Youth were instructed to roll a cotton swab across their tongue for two minutes and then return the swab to the tube without touching it. They also were instructed not to eat, drink or brush their teeth for 30 minutes prior to saliva collection. Youth recorded the time each saliva sample was taken on a separate data collection sheet on which they also recorded any medications they were taking during this saliva collection period. Instructions for saliva collection and questionnaire completion were reviewed with parents and youth during the first phone interview, and youth were reminded about the saliva collection on the evenings prior to scheduled collections. Participants refrigerated saliva samples after collection and at the end of the saliva collection period mailed the samples to the laboratory using prepaid overnight delivery. Upon receipt at the laboratory, saliva samples were weighed and frozen at −80 °C until later assay of cortisol in the Biomarker Core Laboratory at The Pennsylvania State University using commercially available EIA kits (Salimetrics, LLC, State College, PA). Assays were run on a rolling basis throughout the entire study period. Dyad samples were run in duplicate on the same assay plate. The assay had a lower limit of sensitivity of 0.003 ug/dL, with average inter- and intra-assay covariances (%) of less than 7% and 4%. Eleven before dinner samples and 54 bedtime samples were below 0.003 ug/dL and were designated as off-the-curve low and set to the lowest level of sensitivity to the assay. Cortisol data were converted to nmol/l (ug/dL X 27.59), as a universal conversion.
Measures
Positive experiences with parents
Two scales, adapted from the Parent-Child Affective Quality Questionnaire (Conger, 1989; Spoth, Redmond, & Shin, 1998), were used to assess parent-youth relationship experiences. On a six-item scale e.g., “How often did your parent say something nice about you?”, “How often did your parent show that s/he understands how you feel?” youth used a three-point rating scale (1 = not at all, 2 = once, 3 = more than once) to describe the behavior of their employee-parent from the time of the previous call until the time of the current call, and ratings were averaged to create a daily score of positive experiences. The between-person reliability was .76 and the within-person reliability was .47 (Cranford et. al., 2006; Mogle, Almeida, & Stawski, in press).
Negative experiences with parents
This 7-item scale (Spoth et al., 1998) assessed the frequency of negative experiences with their employee-parent from the time of the previous call until the time of the current call. Items included negative experiences with their parents in a particular day, e.g., “How often did your parent yell at you?”, “How often did your parent criticize you?” Parent behaviors were rated on a three-point scale (1 = not at all, 2=once, 3=more than once) and averaged to create a daily score. The between-person reliability was .68 and the within-person reliability was .42.
Youth physical health symptoms
This six-item scale assessed how many physical health symptoms the youth experienced since the time of prior day’s call (adapted from Larsen & Kasimatis, 1991). For each of six items (headache, cold/flu, tired, allergies, stomachache, other physical problems) youth reported whether they had or had not experienced that symptom (0 = no; 1 = yes). The items were summed so that higher scores indicated more daily physical health symptoms.
Youth cortisol
We used three indicators of HPA-axis function: level of cortisol before dinner, level at bedtime, and the before dinner to bedtime (evening) slope. We focused on end of the day measures, reasoning that they would best reflect youths’ reactions to experiences with their parents on a given day. The evening slope was calculated by subtracting the before dinner from the bedtime cortisol score and dividing by the duration of time between the samplings. Cortisol values were converted to nmol/l and natural log transformed before analysis (Adam & Kumari, 2009).
Control variables and moderators
Models also included youth and parent gender (0 = male, 1 = female) and the cross-time average of parenting as moderators and controlled for youth age in years (centered at the grand mean), race/ethnicity (0 = White; 1= Non-white), and parent education (0 = Not a college graduate, 1= College graduate). Consistent with prior research, cortisol models also included time of cortisol sample collection and whether or not the youth was taking any medications (0 = no medications, 1= 1 or more medications) as control variables (Adam & Kumari, 2009).
Results
Descriptive Statistics
Means and correlations for study variables can be found in Table 1. There were no statistically significant differences between boys and girls or experiences with mothers and fathers for any of our predictor or outcome variables (not shown). Intraclass correlations for our outcome variables ranged from .08 to .26, suggesting that the vast majority of variation in our outcome variables occurred within-people across study days. That is, individuals differed from themselves across days more than they differed from other individuals.
Table 1.
Means, Standard Deviations, Intra-Class Correlations, and Between-Person Pearson Correlations for Study Variables
| Mean | BP SD | WP SD | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Negative P-Y Experiences | 1.32 | 0.33 | 0.25 | ||||||||
| 2. Positive P-Y Experiences | 2.48 | 0.46 | 0.26 | −.28** | |||||||
| 3. Child Physical Symptoms | 0.61 | 0.56 | 0.75 | .13 | −.34** | ||||||
| 4. Before Dinner Cortisol Level | 2.34 | 2.29 | 2.92 | .14 | .01 | .03 | |||||
| 5. Bedtime Cortisol Level | 1.46 | 1.45 | 1.80 | .23** | −.15 | .02 | .60*** | ||||
| 6. Before Dinner to Bedtime Slope | −0.09 | 0.19 | 0.29 | .07 | −.18 | .01 | −.54*** | .06 | |||
| 7. Child Gender | -- | -- | -- | −.09 | .12 | .16 | .06 | .07 | −.03 | ||
| 8. Parent Gender | -- | -- | -- | −.08 | .13 | −.02 | .04 | .05 | .14 | −.06 | |
| Intra-Class Correlation | 0.59 | 0.71 | 0.26 | 0.34 | 0.29 | 0.08 | -- | -- |
p < .01, *** p < .001.
BP = between-person. WP = within-person. P-Y = Parent-Youth. All cortisol values were log transformed before calculating correlations.
Plan of Analysis
We used multilevel modeling (Raudenbush & Bryk, 2002) to take into account the non-independence of the data, i.e., days clustered within individuals. Two level models were estimated in SAS 9.3 using Proc Mixed, with days (level 1, within-person) nested within individuals (level 2, between-person). At level 1, we included person-centered measures of the time varying parenting measures. At level 2, we entered the between-person variables, which were grand mean centered, including the cross time averages of the parenting measures (person-mean) and youth age; we also included here dichotomized youth gender and parent gender. Education and race/ethnicity were entered as control variables. Cortisol models also included time of sample collection and medication use as control variables.
| (1a) |
| (1b) |
| (1c) |
At Level 1 (daily level, equation 1a), youth i’s health outcomes on day t were modeled as a function of their daily intercept (B0i) and daily slope (B1i), and residual variance (eti.). The daily slope reflects changes in youth outcomes on days when youth have more positive or negative experiences than usual (within-person). At Level 2 (person-level), the level 1 intercept (equation 1b) was modeled as a function of the sample average intercept (π00), and slope (π01), as well as random effects (u0i). The Level 2 slope (π01) reflects changes in youth outcomes associated with the cross-time averages of experiences with parents (between-person). The level 1 slope (equation 1c) was modeled as the sample average daily within-person effect (π10) and random effects (u1i).
We estimated four models for each outcome variable (i.e., physical symptoms and 3 cortisol indicators; see Table 2). First, we tested the main effects of youth experiences with the employee-parent on their physical health (Model 1). Negative and positive experiences with parents were tested separately. Second, we tested whether the links between positive and negative experiences with the employee-parent and health outcomes were moderated by youth gender (Model 2) or parent gender (Model 3). Moderation for youth and parent gender was tested at the between-person level by adding an interaction term with gender and between-person parent experiences to Level 2 (Gender *π01 added to equation 1b). Moderation was also tested at the within-person level by adding gender to equation 1c, resulting in a cross-level interaction term with gender (Level 2) moderating the within-person effects of experiences with parents (Level 1). Follow-up tests of the simple slopes were conducted when interaction terms were significant at p < .05 or lower. Third, we tested whether the links between youth daily experiences with the employee-parent and the health indicators at Level 1 were moderated by the across-time averages of the parenting indices at Level 2 (i.e., the within-person by between-person interaction terms; Model 4). Separate models were run for positive and negative experiences with the employee-parent for each health outcome. It should be noted that we conducted additional analyses with positive and negative experiences in the same model and found the same pattern of results (not shown). We present our results with positive and negative experiences separately to allow for easier assimilation by the reader, given the large number of predictors and steps in each table.
Table 2.
Negative Parent-Youth Experiences and Youth Health Outcomes
| Physical Health Symptoms | Before Dinner Level of Cortisol | Bedtime Level of Cortisol | Before Dinner to Bedtime Slope | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Est | SE | Est | SE | Est | SE | Est | SE | |
|
| ||||||||
| Model 1: Main Effects | ||||||||
| Fixed Effects | ||||||||
| BP Neg P-Y Experiences | 0.27† | 0.14 | 0.14 | 0.10 | 0.18† | 0.10 | 0.07 | 0.08 |
| WP Neg P-Y Experiences | 0.24* | 0.10 | −0.01 | 0.10 | 0.01 | 0.10 | 0.06 | 0.06 |
| Random Effects | ||||||||
| Intercept | 0.21*** | 0.02 | 0.09*** | 0.02 | 0.09*** | 0.02 | 0.02** | 0.01 |
| Residual | 0.65*** | 0.02 | 0.17*** | 0.02 | 0.21*** | 0.02 | 0.10*** | 0.01 |
| Model 2: Moderation by Youth Gender | ||||||||
| Fixed Effects | ||||||||
| BP Neg P-Y Experiences | 0.24 | 0.20 | 0.20 | 0.15 | 0.24† | 0.14 | −0.08 | 0.10 |
| WP Neg P-Y Experiences | −0.01 | 0.14 | 0.03 | 0.13 | −0.04 | 0.14 | 0.04 | 0.09 |
| Youth gender | 0.19† | 0.10 | 0.09 | 0.07 | 0.06 | 0.07 | −0.04 | 0.05 |
| BP Neg P-Y Experiences x Youth gender | 0.07 | 0.28 | 0.13 | 0.21 | 0.12 | 0.21 | 0.02 | 0.13 |
| WP Neg P-Y Experiences x Youth gender | 0.52* | 0.21 | −0.08 | 0.19 | −0.14 | 0.19 | 0.33* | 0.15 |
| Model 3: Moderation by Parent Gender | ||||||||
| Fixed Effects | ||||||||
| BP P-Y Neg Experiences | 0.05 | 0.20 | −0.10 | 0.14 | −0.05 | 0.14 | 0.14 | 0.09 |
| WP P-Y Neg Experiences | 0.37 | 0.15 | 0.12 | 0.08 | −0.03 | 0.14 | −0.05 | 0.10 |
| Parent gender | −0.04 | 0.09 | −0.01 | 0.07 | 0.02 | 0.06 | 0.08† | 0.05 |
| BP P-Y Neg Experiences x Parent gender | 0.44 | 0.28 | 0.47* | 0.21 | 0.45* | 0.19 | −0.17 | 0.13 |
| WP P-Y Neg Experiences x Parent gender | −0.27 | 0.21 | −0.27 | 0.19 | 0.15 | 0.21 | 0.27† | 0.15 |
| Model 4: Moderation by Average Negative Experiences | ||||||||
| Fixed Effects | ||||||||
| BP P-Y Neg Exp | 0.27† | 0.14 | 0.14 | 0.11 | 0.17† | 0.10 | 0.05 | 0.10 |
| WP P-Y Neg Exp | 0.42** | 0.13 | 0.04 | 0.12 | 0.19 | 0.13 | 0.14 | 0.06 |
| WP P-Y Neg Exp x BP P-Y Neg Exp | −0.75** | 0.28 | −0.15 | 0.25 | −0.59* | 0.26 | −0.21 | 0.19 |
Note. * p < .05, ** p < .01, *** p < .001, † p < .10.
BP indicates between-person effects (Level 2, average level). WP indicates within-person effects (Level 1, daily level). P-Y = Parent-Youth. All models control for youth gender, age, education, and race. Cortisol models also control for medication use and time of sample. Moderation models include random effects (not shown). Significant estimates are in bold.
For significant results, we calculated the percent change in the outcome variable as a result of a one unit increase in the predictor variable using the following equation:
Similar to calculating effect sizes, calculating the percent change enabled us to ascertain the strength of these associations with the outcome variables (see Adam et al., 2006).
Links between Daily Parent-Child Experiences and Youth Health
Beginning with the main effects of positive and negative parent-youth experiences on youth health (Table 2, Model 1), findings revealed that youths’ negative experiences with their employee-parent were associated with their physical symptoms at the within-person level. The significant effect of negative parent-youth experiences at the within-person level indicates that, controlling for average level of negative parent-youth experiences, on days when youth reported more negative experiences with their employee-parent than usual, they also reported more physical health symptoms than usual. This coefficient (B = .24) is equivalent to a 30.9% percent change: For every one unit increase in negative experiences, there is a 30.9% increase in physical health symptoms (Adam et al., 2006). Given the scaling of our measures, a one unit increase in negative experiences would indicate a change from negative experiences occurring “not at all” to “once” or from “once” to “more than once”. No effects were found for dinner levels or evening slope of cortisol. Positive parental experiences were related only to youth physical health symptoms at the between-person level (not shown). Youth with higher average positive experiences reported fewer physical health problems relative to other youth, B = −0.48, SE = 0.10, p < .001. For every one unit increase in average positive experiences there was a 61.5% decrease in physical health symptoms. A one unit increase in positive experiences would indicate a change from positive experiences occurring “not at all” to “once” or from “once” to “more than once”.
The Role of Gender in Parent-Youth Relationship—Youth Health Linkages
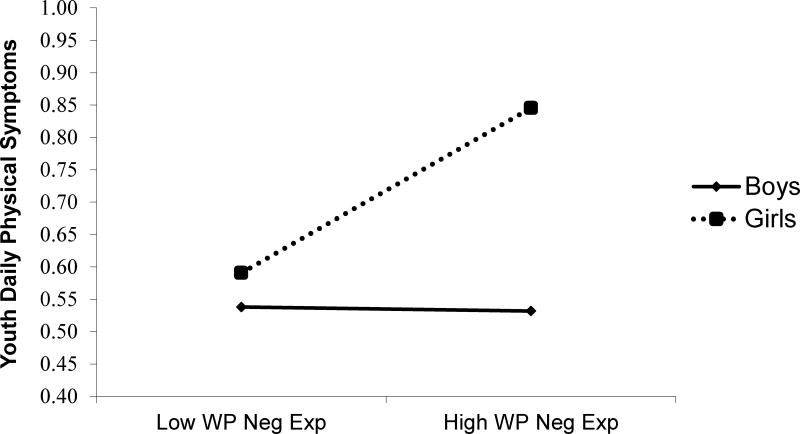
Next, we tested whether the associations between positive and negative parent-youth experiences and youth health outcomes were moderated by youth or parent gender (tests for parent and youth gender were conducted separately). Beginning with youth gender, as seen in Table 2 (Model 2) and Figure 1, results indicated that, at Level 1 (within-person), the link between negative experiences and physical symptoms differed for girls versus boys. Tests of the simple slopes (not shown) revealed that this association was significant for girls, B = 0.51 SE = 0.15, p < .001 but not boys, B = −0.01, SE = 0.14, p = ns: On days when girls had more negative parental experiences than usual, they reported more physical health symptoms than usual, but for boys, daily negative experiences were unrelated to health symptoms. For every one unit increase in negative parent experiences (a change from “not at all” to “once” or from “once” to “more than once”), there was a 66.5% increase in physical symptoms for girls. A similar pattern was found for dinner to bedtime cortisol slopes. A significant interaction between youth gender and negative experiences at Level 1 (Table 2, Model 2), in combination with follow up tests of the simple slopes, indicated that, on days when girls (but not boys) had more negative experiences with their employee-parent than usual, cortisol levels declined less between dinner and bedtime than usual: Girls, B = 0.26, SE =0 .11, p < .05; Boys, B = −0.07, SE = 0.10, ns. We found no youth gender moderation for positive-parent youth experiences.
Figure 1. Daily variation in negative experiences with parents linked to daily youth physical health symptoms: Moderation by youth gender.
Note WP: within-person (Level, 1 daily level). Follow-up tests revealed that the links between daily negative experiences with parents and physical symptoms were significant for girls but not boys.
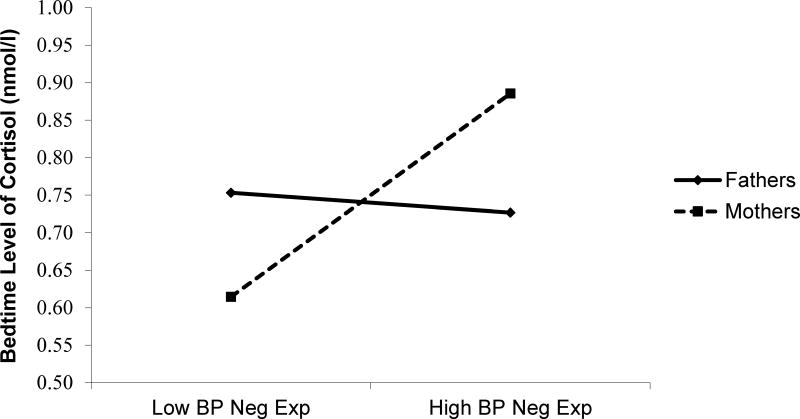
Turning to parent gender, results revealed a significant Level 2 interaction between average negative parent-youth experiences and parent gender predicting before dinner and bedtime cortisol levels (Table 2, Model 3 and Figure 2): Youth who reported higher average negative experiences with a female employee-parent – a mother – had higher dinner, B = 0.38, SE = 0.15, p < .05 and bedtime cortisol levels, B = 0.40, SE = 0.14, p < .01, relative to youth with fewer negative maternal experiences. These associations were not significant for negative experiences a male employee-parent – a father – for dinner, B = −0.12, SE = 0.15, ns, or bedtime cortisol levels, B = −0.05, SE = 0.14, ns. For every one unit increase in negative experiences with mothers, there was a 46.2% increase in dinner and a 49.1% increase in bedtime cortisol levels. One parent gender moderation effect emerged for positive parental experiences, B = 0.48, SE = 0.19, p < .05. On days when youth reported more positive experiences with fathers than usual, they also had lower levels of dinner cortisol than usual B = −0.39, SE = 0.14, p < .01, but this association was not significant for mothers, B = 0.10 SE = 0.14, ns. For every one unit increase in positive experiences with fathers (a change from “not at all” to “once” or from “once” to “more than once”), there was a 47.6% decrease in dinner cortisol levels.
Figure 2. Average negative experiences with parents linked to youth bedtime cortisol levels: Moderation by parent gender.
Note: BP: between-person (Level 2, average level). Follow-up tests revealed that the links between average negative experiences with parents and bedtime cortisol levels were significant for experiences with mothers but not fathers.
The Larger Context of Youths’ Experiences with Parents
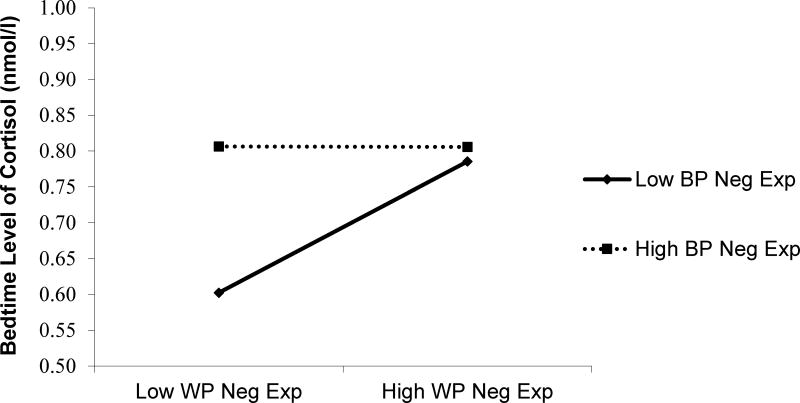
In a last step, we tested whether the daily associations between parent-youth experiences and physical health differed depending on the average level of positive or negative experiences across study days (i.e., within-person by between-person interaction). As seen in Table 2 (Model 4) and Figure 3, a significant interaction between average and daily parenting emerged for negative experiences predicting youth physical symptoms. Tests of the simple slopes revealed that the link between negative parent-youth experiences and youth physical symptoms was significant for youth with lower average levels of negative experiences with parents, B = 0.66, SE =0 .19, p < .001 but the effect was smaller and only reached trend level for youth who reported higher average negative experiences, B = 0.18, SE=0.11, p =.09. This finding suggests that youth who experienced lower average negative experiences were more sensitive to parental negativity when it did occur. Importantly, this pattern also means that youth who had high average levels of negative experiences reported higher levels of physical health symptoms even on days when they experienced less parental negativity than usual. A significant interaction also emerged for the effect of parental negativity on bedtime cortisol. This linkage was significant for youth who had lower average levels of negative experiences, B = 0.38 SE = 0.20, p =.05, but again, those who had higher average levels of negative experiences maintained higher levels of bedtime cortisol even on days when they reported less parental negativity than usual, B = 0.008, SE = 0 .10, ns. For youth with low average levels of negative experiences, a one unit increase in negative experiences was associated with a 93.4% increase in physical health symptoms and a 46.2% increase in bedtime cortisol levels. No significant interactions emerged for positive experiences with parents.
Figure 3. Daily variation in negative experiences with parents linked to youth bedtime cortisol levels: Moderation by average levels of negative experiences.
Note: WP= within-person (Level 1, daily level), BP = between-person (Level 2, average level). Follow-up tests revealed that the links between daily negative experiences with parents and bedtime cortisol levels were significant for youth with low average levels of negative experiences but not for youth with high average levels of negative experiences.
Discussion
In this study we moved beyond assessment of global measures of experiences with parents to examine how daily experiences with parents—both negative and positive—were linked to daily physical health symptoms and cortisol patterns. Daily experiences of family stressors may be critical for longer term health outcomes due to their implications for the HPA system and physical symptoms (Almeida, 2005; Repetti et al., 2011). Consistent with some prior work, our results suggest that youths’ daily experiences with their parents, especially negative experiences, have important implications for their daily HPA functioning and physical health symptoms. Closer examination revealed that youth and parent gender, as well as the larger parent-child relationship context, moderated these linkages. Inconsistent findings of prior research may be due, in part, to the fact that youths’ responses to parental negativity differ as a function of youth characteristics (i.e., gender) and relationship context (i.e., experiences with mothers but not fathers, overall levels of negativity and positivity).
Overall the effects for parental negativity were more consistent than those for parental positivity, possibly because as stressors, negative experiences may be more closely tied to HPA functioning in this community sample. Lack of positive experiences may not activate the body’s stress response system in the same way as experiences of negativity. Although positive experiences might have the potential to mitigate physical health symptoms and reduce high levels of cortisol, such effects may be evident only for youth who experience high and chronic levels of stress. It is also important to note that the intraclass correlation for parental negativity was lower than that for positivity, meaning that more of the variance in negative experiences was at the within person level, whereas positive experiences varied less from day to day. This lack of daily variability is likely another reason why we found fewer effects for parental positivity These differences in patterns highlight the utility of conceptualizing and testing positivity and negativity as distinct constructs (Dallaire et al., 2006).
As predicted, girls’ HPA functioning and physical health were more closely linked to parents’ negativity than was boys’. On days when girls had more negative experiences with their parents than usual, girls reported more physical health symptoms than usual. They also exhibited flatter cortisol slopes from before dinner to bedtime, suggesting that girls’ cortisol levels may not decline in a healthy manner across the course of the evening. Negative experiences with parents may cause more distress for girls than boys because girls are more strongly oriented to interpersonal relationships and are more strongly affected by interpersonal stressors (Hankin & Abramson, 2001; Kessler, Ronald, & McLeod, 1984; Leaper, 2002). Differences in gender socialization –with girls socialized to greater closeness and more cooperation with their parents -may explain this pattern (Leaper, 2002; McHale et al., 2003).
Negative experiences with employee-parents who were mothers and positive experiences with employee-parents who were fathers were also linked to youth HPA functioning. Youth who had more negative experiences with mothers, on average, were more likely to exhibit higher levels of cortisol before dinner and at bedtime. Such effects were not apparent for fathers. Mother-youth relationships are more intimate and involved and thus negative experiences may be perceived as a greater threat to the relationship, creating stress for youth with implications for HPA functioning (McHale et al., 2003). Yet, youth with low negativity in their maternal relationship had low levels of cortisol. It is possible that maternal relationships with little negativity, on average, are protective against youth stress.
In contrast, positive but not negative experiences with fathers were linked to lower dinner time cortisol. These results are consistent with prior research on fathers’ role in youth positive adjustment, including self-esteem and social competence (Amato, 1994; Lam, McHale, & Crouter, 2012), and with recent work linking positive father-youth interactions to lower cortisol levels (Byrd-Craven et al., 2012). Father-youth interactions tend to be playful and involve leisure activities, and thus the nature of positive interactions with fathers may be more likely to reduce stress for youth than those with mothers (Lam et al., 2012). Further, because fathers are typically less involved than mothers, positive interactions with fathers may be more salient and engender self-esteem, with positive implications for youth stress physiology (Lam et al., 2012). At the most general level, most studies on parenting and youth cortisol have been conducted on samples of mothers, but our findings suggest that studies that test moderation by parent gender are needed to fully understand the role of parenting processes in youth health.
Our findings also suggest that the effects of daily negative parent-youth experiences on youth HPA functioning and physical health are not universal, but depend on whether or not negative experiences are common within the parent-youth relationship. Youth from homes marked by frequent parental negativity (high-average) were less sensitive to daily variation in negative experiences than were youth from homes where negativity was less common across the week, as evidenced by the significant interaction between daily and average parental negativity. The latter group exhibited high levels of bedtime cortisol and physical health symptoms even on days when parental negativity was lower—possibly a chronic stress response. Generally higher levels of parental negativity may make it difficult for these youth to recover from their stressful experiences on days when negativity is lower than usual (Sturge-Apple et al., 2011), lending support to the hypercortisolism hypothesis. An inability to recover after stress is a concern, as failure to recover from stressful experiences has been linked to a host of negative health outcomes (Dienstbier, 1989; Sapolsky Romero, & Munck, 2000). Our study did not show evidence of a blunted cortisol response as a function of average negative experiences with parents. One possible interpretation is that less extreme negative experiences with parents may have different effects on HPA functioning than maltreatment, which has been linked to hypocortisolism in prior studies (Cicchetti & Rogosch, 2001). However, a hypocortisolism response may emerge after long-term exposure to chronic stress. It is possible such a pattern may have emerged if we followed youth over a longer time period.
In contrast, youth who were less accustomed to negative parental experiences (low-average) experienced higher levels of cortisol at bedtime and more physical health symptoms than usual on days when they reported more negative experiences than usual. Indeed, on days when these youth reported more negative experiences than usual, they exhibited cortisol levels that were similar to those of youth whose parents were more generally negative. These findings imply that youth who are less accustomed to negativity find negative experiences to be highly stressful, with corresponding implications for their stress physiology. These youth exhibited a pattern of recovery from days of parental negativity as evidenced by lower cortisol levels on less stressful days; this pattern may protect youth from developing long term health problems. Such findings highlight the importance of considering the larger context of daily experiences when studying parent-youth relationship-health linkages.
Our findings should be interpreted in light of this study’s limitations. The sample included youth with generally well-educated parents who were employed in one industry and are thus are not generalizable to other groups of youth. We relied on self-reports of physical health symptoms, which may contain some bias. We also cannot determine the direction of effects in this study. It is possible that youth with higher cortisol levels or more physical health symptoms are more likely to elicit or perceive parental negativity. Further, we do not have data on parenting that may have been experienced prior to the time of our study. Our measures had low reliability at the within-person level. It is common for within-person reliabilities to be lower than between-person reliabilities (Cranford et. al., 2006; Mogle et al., in press). However low reliabilities may make it more difficult to detect effects. Thus low reliabilities may have led to conservative estimates at the within-person level. In addition, before dinner cortisol levels may be impacted by other factors, such as youth activity level and exercise, which we were unable to control for in these analyses (Scheen et al., 1998). Lastly, given they are distinct constructs (Dallaire et al., 2006), we tested the effects of positive and negative experiences in separate analyses, but testing more models inflates the risk of Type I error.
In the face of its limitations, this study has multiple strengths. By using a daily diary approach, we were able to capture day-to-day fluctuations in parent-youth experiences and youth HPA functioning and physical health and shed light on their proximal linkages. Further, because daily diary analyses can be set up to treat individuals as their own controls, we were able to rule out stable third variable explanations for the results, such as youth temperament or family background characteristics, even when such factors were not directly assessed (Almeida, 2005). Our diary approach was designed to increase the ecological validity and reliability of youths’ reports of their experiences with parents and their health (Bolger et al., 2003). We also moved beyond self-reports of health by including a biomarker of HPA axis functioning as a means of limiting the biases that can arise in correlated self-reports. Further, the percent change in the youth outcome variables associated with a one unit increase in the parenting measures was quite high, ranging between 30 and 93% for the significant predictors. Thus, a one unit increase in positive/negative experiences (a change from “not at all” to “once” or from “once” to “more than once”) was associated with relatively large changes in youth outcomes. These changes are best understood in the context of youth’s average reports of their health. For example, the 61% percent change in physical symptoms associated with every one unit increase in positive parenting experience reflects a .38 reduction in the number of average physical symptoms. Future work should explore how daily variations in parent-youth relationships relate to longer-term global health outcomes and how positive and negative parent-youth experiences can work together to influence youth health. Future studies that involve more time-intensive assessments of parent-youth relationships and youth health, such as ecological momentary assessment approaches, also may shed light on the temporal ordering between these associations.
At the most general level, the study adds to the small body of research on the role of parents in their youth’s physical health and highlights the importance of taking into account youth and parent characteristics and the larger context of these relationships for illuminating potential influence processes. Positive experiences with fathers were also linked to healthier HPA functioning, documenting both the importance of fathers’ unique role in their adolescent-aged offspring’s development and the importance of incorporating fathers in future research on youth health. Further, negative everyday experiences with parents had important implications for youth HPA functioning and physical health, especially for girls and for experiences with mothers. Yet, the impacts of negative experiences may need to be considered in light of the broader family context, as youth who were accustomed to negative experiences were less likely to recover from negative experiences on less negative days, a chronic stress response that may have implications for their long-term health and well-being.
Acknowledgments
This research was conducted as part of the Work, Family and Health Network (www.WorkFamilyHealthNetwork.org), which is funded by a cooperative agreement through the National Institutes of Health and the Centers for Disease Control and Prevention: Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant # U01HD051217, U01HD051218, U01HD051256, U01HD051276), National Institute on Aging (Grant # U01AG027669), Office of Behavioral and Science Sciences Research, and National Institute for Occupational Safety and Health (Grant # U01OH008788, U01HD059773). Grants from the William T. Grant Foundation, Alfred P. Sloan Foundation, and the Administration for Children and Families have provided additional funding. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of these institutes and offices. Special acknowledgement goes to Extramural Staff Science Collaborator, Rosalind Berkowitz King, Ph.D. and Lynne Casper, Ph.D. for the design of the original Workplace, Family, Health and Well-Being Network Initiative. We also wish to express our gratitude to the worksites, employers, and employees who participated in this research. Full acknowledgements: http://www.kpchr.org/wfhn
Contributor Information
Melissa A. Lippold, Email: mlippold@unc.edu, The University of North Carolina at Chapel Hill, Tate-Turner-Kuralt Building, 325 Pittsboro St CB#3550, Chapel Hill, NC 27599-3550
Susan M. McHale, The Pennsylvania State University, 114 Henderson (North), University Park PA 16802
Kelly D. Davis, Clearinghouse for Military Family Readiness, The Pennsylvania State University, 135 E. Nittany Avenue, Suite 402, State College, PA 16801
David M. Almeida, The Pennsylvania State University, 403 BBH Building, University Park, PA 16802
Rosalind B. King, Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Health Scientist Administrator Population Dynamics Branch, 6100 Executive Blvd., Room 8B07, MSC 7510, Bethesda, MD 20892-7510
References
- Adam E, Kumari M. Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology. 2009;34(10):1423–1436. doi: 10.1016/j.psyneuen. [DOI] [PubMed] [Google Scholar]
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience–cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Sciences. 2006;103(45):17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albers EM, Riksen-Walraven JM, Sweep FC, Weerth CD. Maternal behavior predicts infant cortisol recovery from a mild everyday stressor. Journal of Child Psychology and Psychiatry. 2008;49(1):97–103. doi: 10.1111/j.1469-7610.2007.01818.x. [DOI] [PubMed] [Google Scholar]
- Almeida DM. Resilience and vulnerability to daily stressors assessed via diary methods. Current Directions in Psychological Science. 2005;14(2):64–68. doi: 10.1111/j.0963-7214.2005.00336.x. [DOI] [Google Scholar]
- Almeida DM, McGonagle K, King H. Assessing daily stress processes in social surveys by combining stressor exposure and salivary cortisol. Biodemography and Social Biology. 2009;55(2):219–237. doi: 10.1080/19485560903382338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amato PR. Father-child relations, mother-child relations, and offspring psychological well-being in early adulthood. Journal of Marriage and Family. 1994;56(4):1031–1042. [Google Scholar]
- Baumrind D. The influence of parenting style on adolescent competence and substance use. The Journal of Early Adolescence. 1991;11:56–95. doi: 10.1177/0272431691111004. [DOI] [Google Scholar]
- Bolger N, Davis A, Rafaeli E. Diary methods: Capturing life as it is lived. Annual Review of Psychology. 2003;54(1):579–616. doi: 10.1146/annurev.psych.54. [DOI] [PubMed] [Google Scholar]
- Bray JW, Kelly EL, Hammer LB, Almeida DM, Dearing JW, King RB, Buxton OM. RTI Press publication No MR-0024-1303. Research Triangle Park, NC: RTI Press; 2013. An integrative, multi-level, and transdisciplinary research approach to challenges of work, family, and health. [PubMed] [Google Scholar]
- Byrd-Craven J, Auer BJ, Granger DA, Massey AR. The father-daughter dance: The relationship between father-daughter relationship quality and daughters’ stress response. Journal of Family Psychology. 2012;26(1):87–94. doi: 10.1037/a0026588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles ST, Piazza JR, Mogle J, Sliwinski M, Almeida DM. The wear and tear of daily stressors on mental health. Psychological Science. 2013;24(5):733–741. doi: 10.1177/0956797612462222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. The impact of child maltreatment and psychopathology on neuroendocrine functioning. Development and Psychopathology. 2001;13(4):783–804. [PubMed] [Google Scholar]
- Conger RD. Iowa Youth and Families Project, Wave A (technical report) Ames, IA: Iowa State University Center for Family Research in Rural Mental Health; 1989. [Google Scholar]
- Cranford JA, Shrout PE, Iida M, Rafaeli E, Yip T, Bolger N. A procedure for evaluating sensitivity to within-person change: Can mood measures in diary studies detect change reliably? Personality and Social Psychology Bulletin. 2006;32(7):917–929. doi: 10.1177/0146167206287721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallaire DH, Pineda AQ, Cole DA, Ciesla JA, Jacquez F, LaGrange B, Bruce AE. Relation of positive and negative parenting to children’s depressive symptoms. Journal of Clinical Child and Adolescent Psychology. 2006;35(2):313–322. doi: 10.1207/s15374424jccp3502_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dienstbier RA. Arousal and physiological toughness: implications for mental and physical health. Psychological Review. 1989;96(1):84–100. doi: 10.1037/0033-295X.96.1.84. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Boyle MH, Khu HH, Georgiades K, Duncan L, MacMillan HL. Childhood and family influences on depression, chronic physical conditions, and their comorbidity: Findings from the Ontario Child Health Study. Journal of Psychiatric Research. 2012;46:1475–1482. doi: 10.1016/j.jpsychires.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Gottman JM, Katz LF, Hooven C. Parental meta-emotion philosophy and the emotional life of families: Theoretical models and preliminary data. Journal of Family Psychology. 1996;10:243–268. doi: 10.1037/0893-3200.10.3.243. [DOI] [Google Scholar]
- Gunnar M, Quevedo K. The neurobiology of stress and development. Annual Review of Psychology. 2007;58:145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY. Development of gender differences in depression: An elaborated cognitive vulnerability–transactional stress theory. Psychological Bulletin. 2001;127(6):773–796. doi: 10.1O37//O033-29O9.127.6.773. [DOI] [PubMed] [Google Scholar]
- Hastings PD, McShane KE, Parker R, Ladha F. Ready to make nice: Parental socialization of young sons’ and daughters’ prosocial behaviors with peers. The Journal of Genetic Psychology. 2007;168(2):177–200. doi: 10.3200/GNTP.168.2.177-200. [DOI] [PubMed] [Google Scholar]
- Jansen J, Beijers R, Riksen-Walraven M, de Weerth C. Does maternal care-giving behavior modulate the cortisol response to an acute stressor in 5-week-old human infants? Stress: The International Journal on the Biology of Stress. 2010;13(6):491–497. doi: 10.3109/10253890.2010.483298. [DOI] [PubMed] [Google Scholar]
- Kemeny ME. The psychobiology of stress. Current Directions in Psychological Science. 2003;12(4):124–129. doi: 10.1111/1467-8721.01246. [DOI] [Google Scholar]
- Kessler RC, McLeod JD. Sex differences in vulnerability to undesirable life events. American Sociological Review. 1984;49(5):620–631. doi: 10.2307/2095420. [DOI] [Google Scholar]
- Kiecolt-Glaser JK, Gouin JP, Weng NP, Malarkey WB, Beversdorf DQ, Glaser R. Childhood adversity heightens the impact of later-life caregiving stress on telomere length and inflammation. Psychosomatic Medicine. 2011;73(1):16–22. doi: 10.1097/PSY.0b013e31820573b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King RB, Karuntzos GT, Casper LM, Moen P, Davis KD, Berkman L, Durham M, Kossek EE. Work-family balance issues and work-leave policies. In: Gatchel RJ, Schultz IZ, editors. Handbook of occupational health and wellness. New York, NY: Springer; 2012. pp. 323–339. [Google Scholar]
- Lam CB, McHale SM, Crouter AC. Parent–child shared time from middle childhood to late adolescence: Developmental course and adjustment correlates. Child Development. 2012;83(6):2089–2103. doi: 10.1111/j.1467-8624.2012.01826.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen RJ, Kasimatis M. Day-to-day physical symptoms: Individual differences in the occurrence, duration, and emotional concomitants of minor daily illnesses. Journal of Personality. 1991;59:387–423. doi: 10.1111/j.1467-6494.1991.tb00254.x. [DOI] [PubMed] [Google Scholar]
- Leaper C. Parenting girls and boys. In: Bornsten ME, editor. The handbook of parenting. Vol. 1. New Jersey: Lawrence Erlbaum; 2002. pp. 189–225. [Google Scholar]
- Lim J, Wood BL, Miller BD. Maternal depression and parenting in relation to child internalizing symptoms and asthma disease activity. Journal of Family Psychology. 2008;22 (2):264–273. doi: 10.1037/0893-3200.22.2.264. [DOI] [PubMed] [Google Scholar]
- Maccoby EE. The two sexes: Growing up apart, coming together. Cambridge, MA: Harvard University Press; 1998. [Google Scholar]
- Marsman R, Nederhof E, Rosmalen JG, Oldehinkel AJ, Ormel J, Buitelaar JK. Family environment is associated with HPA-axis activity in adolescents: The TRAILS study. Biological Psychology. 2012;89(2):460–466. doi: 10.1016/j.biopsycho.2011.12.013. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences. 1998;840(1):33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McHale SM, Crouter AC, Whiteman SD. The family contexts of gender development in childhood and adolescence. Social Development. 2003;12(1):125–148. doi: 10.1111/1467-9507.00225. [DOI] [Google Scholar]
- Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychological Bulletin. 2011;137:959–995. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogle J, Almeida DM, Stawski RS. Psychometric properties of micro-longitudinal assessments: Between- and within-person reliability, factor structure and discriminate validity of cognitive interference. In: Diehl M, Hooker K, Sliwinski M, editors. Handbook of intraindividual variability across the lifespan. NY: Routledge; pp. xx–xx. in press. [Google Scholar]
- Neeck G, Federlin K, Graef V, Rusch D, Schmidt KL. Adrenal secretion of cortisol in patients with rheumatoid arthritis. Journal of Rheumatology. 1990;17:24–29. [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in depression. Current Directions in Psychological Science. 2001;10:173–176. doi: 10.1111/1467-8721.00142. [DOI] [Google Scholar]
- Odgers CL, Jaffee SR. Routine versus catastrophic influences on the developing child. Annual Review of Public Health. 2013;34:29–48. doi: 10.1146/annurev-publhealth-031912-114447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasterski V, Golombok S, Hines M. Sex differences in social behavior. In: Smith PK, Hart CH, editors. The Wiley-Blackwell handbook of childhood social development, second edition. Malden MA: Blackwell Publishing; 2011. pp. 281–298. [Google Scholar]
- Pendry P, Adam EK. Associations between parents’ marital functioning, maternal parenting quality, maternal emotion and child cortisol levels. International Journal of Behavioral Development. 2007;31(3):218–231. doi: 10.1177/0165025407074634. [DOI] [Google Scholar]
- Piazza JR, Charles ST, Sliwinski MJ, Mogle J, Almeida DM. Affective reactivity to daily stressors and long-term risk of reporting a chronic physical health condition. Annals of Behavioral Medicine. 2013;45(1):110–120. doi: 10.1007/s12160-012-9423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak S, Vardi S, Putzer Bechner AM, Curtin J. Physically abused children’s regulation of attention in response to hostility. Child Development. 2005;76:1467–8624. doi: 10.1111/j.1467-8624.2005.00890.x. [DOI] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A. Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Repetti RL, Robles TR, Reynolds B. Allostatic processes in the family. Development and Psychopathology. 2011;23:921–938. doi: 10.1017/S095457941100040X. [DOI] [PubMed] [Google Scholar]
- Russek LG, Schwartz GE. Feeling of parental caring predict health status in midlife: A 35-year follow-up of the Harvard Mastery of Stress Study. Journal of Behavioral Medicine. 1997;20(1):1–13. doi: 10.1023/A:1025525428213. [DOI] [PubMed] [Google Scholar]
- Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocrine Reviews. 2000;21(1):55–89. doi: 10.1210/edrv.21.1.0389. http://dx.doi.org/10.1210/edrv.21.1.0389. [DOI] [PubMed] [Google Scholar]
- Scheen AJ, Buxton OM, Jison M, Van Reeth O, Leproult R, L’Hermite-Balériaux M, Van Cauter E. Effects of exercise on neuroendocrine secretions and glucose regulation at different times of day. American Journal of Physiology-Endocrinology and Metabolism. 1998;274(6):E1040–E1049. doi: 10.1152/ajpendo.1998.274.6.E1040. [DOI] [PubMed] [Google Scholar]
- Slatcher RB, Robles TF. Preschoolers’ everyday conflict at home and diurnal cortisol patterns. Health Psychology. 2012;31(6):834–838. doi: 10.1037/a0026774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smeekens S, Riksen-Walraven J, Van Bakel HJ. Cortisol reactions in five-year-olds to parent–child interaction: The moderating role of ego-resiliency. Journal of Child Psychology and Psychiatry. 2007;48(7):649–656. doi: 10.1111/j.1469-7610.2007.01753.x. [DOI] [PubMed] [Google Scholar]
- Spangler G, Schieche M. Biobehavioral organization in one-year-olds: Quality of mother-infant attachment and immunological and adrenocortical regulation. Psychologische Beitrage. 1994;36:30–35. [Google Scholar]
- Spoth R, Redmond C, Shin C. Direct and indirect latent-variable parenting outcomes of two universal family-focused preventive interventions: Extending a public health-oriented research base. Journal of Consulting and Clinical Psychology. 1998;66:385–399. doi: 10.1037/0022-006X.66.2.385. [DOI] [PubMed] [Google Scholar]
- Sturge-Apple ML, Skibo MA, Rogosch FA, Ignjatovic Z, Heinzelman W. The impact of allostatic load on maternal sympathovagal functioning in stressful child contexts: Implications for problematic parenting. Development and Psychopathology. 2011;23:831–844. doi: 10.1017/S0954579411000332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturge-Apple ML, Davies PT, Cicchetti D, Manning LG. Interparental violence, maternal emotional unavailability and children’s cortisol functioning in family contexts. Developmental Psychology. 2012;48(1):237–249. doi: 10.1037/a0025419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegman HL, Stetler C. A meta-analytic review of the effects of childhood abuse on medical outcomes in adulthood. Psychosomatic Medicine. 2009;71(8):805–812. doi: 10.1097/PSY.0b013e3181bb2b46. [DOI] [PubMed] [Google Scholar]
- Wood BL, Miller BD, Lim J, Lillis K, Ballow M, Stern T, Simmens S. Family relational factors in pediatric depression and asthma: pathways of effect. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(12):1494–1502. doi: 10.1097/01.chi.0000237711.81378.46. [DOI] [PubMed] [Google Scholar]