Abstract
Despite the clinically-significant association between perceived stress and smoking, there is little understanding of the mechanisms underlying this relation. The present study examined smoking-specific experiential avoidance as an explanatory mechanism linking perceived stress and smoking, including nicotine dependence, perceived barriers to cessation, and problems reported during past quit attempts among treatment-seeking daily smokers (n = 365; 48.5% female; Mage = 38.02; SD = 13.10). Results indicated that smoking-specific experiential avoidance had a significant, indirect effect on perceived stress and the studied smoking criterion variables. The present findings provide initial empirical support that smoking-specific experiential avoidance may help explain how perceived stress is associated with smoking. These data suggest that there may be merit to targeting smoking-specific experiential avoidance during smoking cessation among smokers with elevated perceived stress.
Keywords: perceived stress, experiential avoidance, smoking, tobacco
There is a long-standing interest in the interconnection between stress and substance use behavior (Sinha, 2001). Clinical reports, epidemiologic sources, and laboratory investigations converge on a consistent and robust association between elevated objective and subjective indices of stress and substance use and relapse (Brewer, Catalano, Haggerty, Gainey, & Fleming, 1998; Sinha, 2001).
Although numerous types of stress have been studied, Lazarus and Folkman (1984) posit that the most critical element of an event’s impact is how it is appraised. Specifically, the degree to which an individual evaluates an event in terms of its significance (primary appraisal) and his/her ability to effectively deal with it (secondary appraisal) largely determines whether the event produces a negative (emotional) response (Cohen, Kamarck, & Mermelstein, 1983). In line with this perspective, research suggests perceived stress, defined as the degree to which individuals experience life events as unpredictable, uncontrollable, or generally overloading (Cohen et al., 1983), is associated with greater negative emotional responsivity (Zvolensky et al., 2002) as well as avoidant coping (Soderstrom, Dolbier, Leiferman, & Steinhardt, 2000). It is important to highlight that while some work conceptualizes perceived stress and negative affect as a uni-dimensional construct (Cohen, Tyrrell, & Smith, 1993; Watson, 1988; Watson & Clark, 1992), they are theoretically distinct. Specifically, perceived stress taps into the stress appraisal process by considering one’s coping resources (Cohen et al., 1983), whereas negative affect pertains to the emotional states, regardless of coping resources (Kassel, Stroud, & Paronis, 2003). Therefore, perceived stress is theoretically more of a multifaceted construct that captures influences of stress appraisal that may not be captured by negative affect.
There is also an established relation between perceived stress and smoking, presumably due to its relation to affective processes and their regulation. For example, current smokers report higher levels of perceived stress than nonsmokers (Ng & Jeffery, 2003) as well as smokers who are able to quit successfully (Carey, Kalra, Carey, Halperin, & Richards, 1993; Cohen & Lichtenstein, 1990). Higher perceived stress is also related to higher levels of nicotine dependence (Leung, Lam, & Chan, 2010), less confidence to refrain from smoking (Leung et al., 2010; Ng & Jeffery, 2003), and lower odds of quit success and less time to relapse (al’Absi, Hatsukami, & Davis, 2005). In fact, perceived stress is commonly cited as a key barrier to cessation (Tsourtos & O’Dwyer, 2008). These data collectively indicate that perceived stress is related to several aspects of smoking, but the mechanisms by which perceived stress relates to smoking remain unclear.
One possible mechanism that may help elucidate the perceived stress-substance use relation is experiential avoidance. Experiential avoidance reflects an unwillingness to experience or remain in contact with aversive internal experiences and attempt to control the frequency or form of the experiences and the contexts in which they occur (Hayes et al., 2004). Experiential avoidance related to smoking is associated with increased odds of quit failure (Gifford et al., 2004), perceived barriers to cessation (Zvolensky, Farris, Schmidt, & Smits, 2014), and mood-management motives and nicotine dependence (Farris, Zvolensky, Norton, et al., 2014). Within the context of smoking cessation treatment, smoking-specific avoidance mediates the relation between treatment condition and smoking outcomes (Gifford et al., 2011). Additionally, during the course of smoking cessation treatment, smoking-specific experiential avoidance is related to more severe nicotine withdrawal, craving, and poorer quit-day success (Farris, Zvolensky, & Schmidt, 2014). Importantly, experiential avoidance is related to, but empirically distinct from, other cognitive constructs linked to smoking including distress tolerance (Schloss & Haaga, 2011), coping (Karekla & Panayiotou, 2011), and negative affect (see Hildebrandt & Hayes, 2012). Specifically, although these constructs generally focus on how individuals relate and respond to emotional experiences, experiential avoidance tends to emphasize rigidly avoiding uncomfortable thoughts, feelings, and bodily sensations associated with internal experiences.
It is presently unknown if smoking-specific experiential avoidance explains the relation between perceived stress and smoking. Research suggests individual differenes in mood amplifying factors (e.g., worry, anxiety sensitivity) indirectly relates to greater barriers to cessation, number of prior quit attempts, and greater mood-management smoking expectancies through smoking-specific experiential avoidance (Farris, Zvolensky, Norton, et al., 2014; Zvolensky, Farris, Schmidt, & Smits, 2014). These findings invite further empirical exploration of the role of smoking-specific experiential avoidance in other mood-modulating constructs such as perceived stress. It may be that smokers with greater levels of perceived stress perceive life events and internal sensations as more personally distressing (Zvolensky et al., 2002). Accordingly, these smokers may be more apt to respond to such distress with escape/avoidance, and therefore, use smoking as a means to attenuate their distress (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004). This behavior, in turn, may be related to more severe or problematic smoking behavior (e.g., greater levels of dependence, more perceived obstacles to quitting, and more problems during quit attempts).
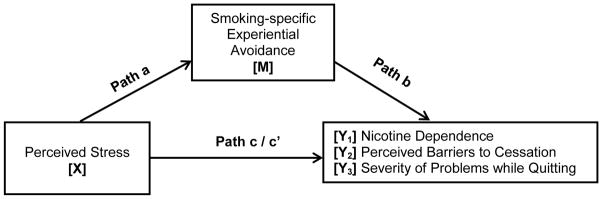
The present study evaluated whether smoking-specific experiential avoidance, in part, explains the relation between perceived stress and nicotine dependence, perceived barriers to cessation, and severity of problematic symptoms during past quit attempts among treatment-seeking smokers (see Figure 1). These smoking variables represent a wide array of smoking processes related to quit history and maintenance of cigarette use, which consistently are related to poorer treatment outcome (Cosci et al., 2009; Ockene et al., 2000; Schnoll et al., 2011). It was hypothesized that perceived stress would have an indirect effect on smoking variables through experiential avoidance.
Figure 1.
Smoking-specific experiential avoidance as anindirect explanatory variable for perceived stress and smoking.
Note: a = Effect of X on M; b = Effect of M on Yi; c = Total effect of X on Yi; c′ = Direct effect of X on Yi controlling for M; a*b = Indirect effect of M; three separate models were conducted, one for each criterion variable (Y1-3). Covariates included Gender, Axis I Disorder, and PANAS-NA = Positive and Negative Affect Scale-Negative Affect subscale (Watson et al., 1988).
Methods
Participants
Adult daily smokers were recruited from the community to participate in a randomized controlled dual-site clinical trial examining the efficacy of two smoking cessation interventions. The sample consisted of 365 treatment-seeking adult daily smokers (48.7% female; Mage = 38.06; SD = 13.11; age range: 18–65 years) who had an expired carbon monoxide level at baseline of at least 8 parts per million (ppm; Jarvis, Tunstall-Pedoe, Feyerabend, Vesey, & Saloojee, 1987) and at least one serious lifetime quit attempt, as indexed by the Smoking History Questionnaire (Brown, Lejuez, Kahler, & Strong, 2002). Exclusion criteria included current suicidality and psychosis. See Table 1 for the sample characteristics.
Table 1.
Participant characteristics
| M(SD)/N[%] | |
|---|---|
| Age | 38.02 (13.10) |
| Gender | |
| Male | 188 [51.5] |
| Female | 177 [48.5] |
| Race/ethnicity | |
| White | 319 [87.4] |
| Black Non-Hispanic | 25 [6.8] |
| Black Hispanic | 2 [0.5] |
| Hispanic | 8 [2.2] |
| Asian | 4 [1.1] |
| Other | 7 [1.9] |
| Education Completed | |
| Less than high school | 14 [3.8] |
| High school graduate or equivalent | 85 [23.3] |
| Some college | 115 [31.5] |
| Associates degree | 36 [9.9] |
| Bachelor degree | 58 [15.9] |
| Some graduate or professional school | 24 [6.6] |
| Graduate or professional school | 33 [9.0] |
| Marital Status | |
| Married or living with someone | 137 [37.5] |
| Widowed | 7 [1.9] |
| Separated | 18 [4.9] |
| Divorced or annulled | 67 [18.4] |
| Never married | 136 [37.3] |
| Baseline CO (ppm) | 21.54 (11.32) |
| Smoking Rate | 17.52 (9.23) |
| Years a Daily Smoker | 19.66 (12.95) |
| Number of Past Serious Quit Attempts | 3.66 (2.31) |
| Axis I Disorder | |
| Absent | 203 [55.6] |
| Present | 162 [44.4] |
| PANAS-NA | 18.95 (6.80) |
| PSS | 24.29 (7.44) |
| AIS | 45.34 (10.89) |
| Nicotine Dependence | 5.38 (2.21) |
| Barrier to Smoking Cessation | 25.32 (11.26) |
| Severity of Problems During Quit Attempt | 2.10 (0.66) |
Note. N = 365; M(SD) = Mean (Standard Deviation). CO (ppm) = Carbon Monoxide (parts per million); PANAS-NA = Positive and Negative Affect Scale-Negative Affect subscale (Watson et al., 1988); PSS (Cohen et al., 1983); AIS = Avoidance and Inflexibility Scale (Gifford et al., 2004).
Measures
Primary Predictor Variable
Perceived Stress Scale (PSS)
Perceived stress scale (Cohen et al., 1983) assessed perceived stress. PSS is a 14-item scale that measures the degree to which situations in one’s life is appraised as stressful during the past month on a 0 (never) to 4 (very often) scale. The PSS has good internal consistency (r=.84 – .86) and test-retest reliability (r=.85; (Cohen et al., 1983). In the present study, the PSS total score was utilized (Cronbach’s α=0.86).
Avoidance and Inflexibility Scale (AIS)
The AIS assessed smoking-specific experiential avoidance and inflexibility (Gifford et al., 2004). Participants respond to 13-items according on a 1 (not at all) to 5 (very much) scale. Higher scores represent more smoking-specific avoidance or inflexibility in the presence of uncomfortable or difficult sensations or thoughts, whereas lower scores suggest more ability to accept difficult feelings or thoughts without allowing them to trigger smoking. Past work found good convergent and predictive validity of the AIS for smoking processes (Farris, Zvolensky, DiBello, & Schmidt, in press). The total score was utilized in the current study (Cronbach’s α=0.93).
Dependent Measures
Fagerström Test for Nicotine Dependence (FTND)
The FTND is a 6-item scale that assesses gradations in tobacco dependence (Heatherton, Kozlowski, Frecker, & Fagerström, 1991). Higher scores reflect high levels of physiological dependence on nicotine. The FTND has adequate internal consistency, positive relations with key smoking variables (e.g., saliva cotinine), and high test-retest reliability (Heatherton et al., 1991; Pomerleau, Carton, Lutzke, Flessland, & Pomerleau, 1994). In the current sample, the FTND total score characterized nicotine dependence (Cronbach’s α = 0.63).
Barriers to Cessation Scale (BCS)
The BCS assesses perceived barriers associated with smoking cessation (Macnee & Talsma, 1995). The BCS is a 19-item measure on which respondents indicate, according to a 4-point scale (0 [not a barrier] to 3 [large barrier]), the extent to which they identify with each specified barrier to cessation. Researchers report good internal consistency regarding the total score, and good content and predictive validity of the measure (Macnee & Talsma, 1995). The total score was utilized (Cronbach’s α=0.90).
Smoking History Questionnaire (SHQ)
The SHQ (Brown et al., 2002) is a self-report questionnaire used to assess smoking history, pattern, and problematic symptoms experienced during past quit attempts (Brown et al., 2002). As is in past work (Zvolensky, Lejuez, Kahler, & Brown, 2004), a mean composite score of severity of problem symptoms experienced during past quit attempts was derived from this measure. The SHQ was also employed to describe the sample smoking history.
Additional Measures used as Covariates or Sample Descriptors
Demographics Questionnaire
Demographic information collected included gender, age, and race. Gender was entered as a covariate in all analyses.
Carbon Monoxide
Biochemical verification of smoking status was assessed by expired carbon monoxide (CO) analysis of breath samples collected using a CMD/CO Carbon Monoxide Monitor (Model 3110; Spirometrics, Inc.). A cut-off of 8 ppm has demonstrated excellent properties at distinguishing smokers from nonsmokers (Jarvis et al., 1987).
Structured Clinical Interview-Non-Patient Version for DSM-IV (SCID-I/NP)
Diagnostic assessments of past year Axis I psychopathology were conducted using the SCID-I/NP (First, Spitzer, Gibbon, & Williams, 1994). All SCID-I/NP interviews were administered by trained research assistants or doctoral level staff and supervised by independent doctoral-level professionals. Interviews were audio-taped and the reliability of a random selection of 12.5% of interviews was checked (MJZ) for accuracy; no cases of (diagnostic coding) disagreement were noted. Based on work indicating a relation between presence of a psychiatric disorder and smoking (Lasser et al., 2000), the presence or absence of an Axis I disorder was included as a covariate.
Positive and Negative Affect Scale (PANAS)
The PANAS (Watson, Clark, & Tellegen, 1988) is a self-report measure that requires participants to rate the extent to which they experience 20 different feelings and emotions on a scale ranging from 1 (Very slightly or not at all) to 5 (Extremely). The measure yields two factors, negative and positive affect, and has strong documented psychometric properties (Watson et al., 1988). The PANAS negative affect subscale (PANAS-NA; 10 items) is characterized as the propensity to experience negative affect. This subscale was utilized in the present study (Cronbach’s α=0.91).
Procedure
Participants provided written informed consent, and completed an interview and a computerized battery of self-report questionnaires during the baseline appointment. The Institutional Review Board at each study site approved the study protocol; all study procedures and treatment of human subjects were conducted in compliance with ethical standards of the American Psychological Association. The current study is based on secondary analyses of baseline data from a sub-set of participants who met the current study inclusion criteria and had complete data for all studied variables.
Analytic Strategy
Listwise deletion was employed to address missing data (Allison, 2001). Sample descriptive statistics and zero-order correlations among study variables were examined. Site differences were also examined. Analyses were conducted using bootstrapping techniques through PROCESS, a conditional modeling program that utilizes an ordinary least squares-based path analytical framework to test for both direct and indirect effects (Hayes, 2013). An indirect effect is assumed to be significant if the confidence intervals (CIs) around the product of path a and path b do not include zero (Preacher & Hayes, 2008; Zhao, Lynch, & Chen, 2010). Models included PSS as the predictor and AIS as the explanatory variable. Covariates included gender (Zvolensky et al., 2014), presence of Axis I psychiatric disorder (Lasser et al., 2000), and PANAS-NA (Zvolensky et al., 2014). Three independent models were run with nicotine dependence (Model 1), perceived barriers to cessation (Model 2), and severity of problem symptoms experienced during past quit attempts (Model 3) as criterion variables. See Figure 1. All models were subjected to 10,000 bootstrap re-samplings and a 95-percentile confidence interval (CI) was estimated (as recommended by Hayes, 2009; Preacher & Hayes, 2004, 2008).
Results
Descriptive Analyses
Participant with missing data (n = 23) were removed using listwise deletion. The removal of these cases did not influence the overall pattern or statistical significance of the results. Retained participants (n = 365) were primarily White (87.4%) adults. Of the sample, 44.4% met criteria for at least one past year psychological disorder, which included: social anxiety disorder (10.1%), posttraumatic stress disorder (3.3%), major depressive disorder (4.9%), generalized anxiety disorder (5.2%), specific phobia (4.4%), panic disorder with or without agoraphobia (1.7%), alcohol use disorder (3.3%), anxiety disorder not otherwise specified (1.9%), obsessive-compulsive disorder (1.1%), dysthymia (1.9%), cannabis use disorder (2.5%), bipolar disorder (0.3%), seasonal major depressive disorder (0.3%), other substance use disorder (0.9%), agoraphobia without panic disorder (0.3%), depressive disorder not otherwise specified (0.5%), and other (1.6%). See Table 1 for participant characteristics. Finally, the two recruitment sites significantly differed on age (p < .001), education (p = .004), years a daily smoker (p < .001), and age when became a daily smoker (p = .007).
PSS was significantly correlated with nicotine dependence, perceived barriers to cessation, and severity of problem symptoms experienced during past quit attempts. AIS was significantly correlated with nicotine dependence, perceived barriers to cessation, and severity of problem symptoms experienced during past quit attempts. PSS and AIS were significantly correlated. Nicotine dependence, barriers to cessation, and severity of problems experienced during past quit attempts all significantly correlated. Zero-order correlations are presented in Table 2.
Table 2.
Correlations among variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | |
|---|---|---|---|---|---|---|---|---|
| 1. Gendera | -- | |||||||
| 2. Axis I Disordera | .13* | -- | ||||||
| 3. PANAS-NAa | .13* | .37*** | -- | |||||
| 4. PSSb | .17** | .34*** | .63*** | -- | ||||
| 5. AISc | .22*** | .14** | .24*** | .27*** | -- | |||
| 6. FTNDd | −.02 | .14** | .05 | .11* | .26*** | -- | ||
| 7. BCSd | .25*** | .17** | .41*** | .36*** | .60*** | .18*** | -- | |
| 8. SPEQd | .32*** | .27*** | .41*** | .35*** | .46*** | .16** | .57*** | -- |
Note. N = 365
p < .001,
p < .01,
p < .05.
Covariate;
Predictor;
Explanatory Variable;
Outcome.
Gender: 1 = Male and 2 = Female; Axis I Disorder: 0 = Disorder Absent and 1 = Disorder Present; PANAS-NA = Positive and Negative Affect Scale-Negative Affect subscale (Watson et al., 1988); PSS (Cohen et al., 1983); AIS = Avoidance and Inflexibility Scale (Gifford et al., 2004); FTND = Fagerström Test for Nicotine Dependence (Heatherton et al., 1991); BCS = Barriers to Cessation Scale (Macnee & Talsma, 1995); SPEQ = Severity of Problems Experienced while Quitting (Brown et al., 2002).
Regression Analyses
Model 1 for nicotine dependence revealed a significant total effect (R2=.03, F[4, 360]=2.45, p=.05). The direct effect model with AIS was significant (R2=.09, F[5, 359]=6.81, p<.001). The indirect effect of PSS on nicotine dependence was significant. Model 2 for perceived barriers to cessation revealed a significant total effect (R2=.22, F[4, 360]=25.01, p<.001). The direct effect model with AIS was significant (R2=.45, F[5, 359]=57.89, p<.001). The indirect effect of PSS on perceived barriers to cessation was significant. Model 3 for severity of problem symptoms experienced during past quit attempts revealed a significant total effect (R2=.25, F[4, 360]=30.61, p<.001). The direct effect model with AIS was significant (R2=.35, F[5, 359]=38.68, p<.001). The indirect effect of PSS on severity of problem symptoms experienced during past quit attempts was significant. Regression results for paths a, b, c, and c′ are presented in Table 3.
Table 3.
Regression models
| Y | Model | b | SE | t | p | CI (lower) | CI (upper) |
|---|---|---|---|---|---|---|---|
| 1 | PSS → AIS (a) | .245 | .095 | 2.589 | .010 | .059 | .430 |
| AIS → FTND (b) | .053 | .011 | 4.861 | <.001 | .032 | .074 | |
| PSS→ FTND (c′) | .020 | .020 | 0.965 | .335 | −.020 | .058 | |
| PSS→ FTND (c) | .032 | .020 | 1.588 | .113 | −.008 | .071 | |
| PSS → AIS → FTND (a*b) | .013 | .006 | .004 | .027 | |||
|
| |||||||
| 2 | AIS → BCS (b) | .526 | .043 | 12.183 | <.001 | .441 | .610 |
| PSS→ BCS (c′) | .109 | .078 | 1.391 | .165 | −.045 | .262 | |
| PSS→ BCS (c) | .237 | .092 | 2.583 | .010 | .057 | .418 | |
| PSS→ AIS → BCS (a*b) | .129 | .050 | .032 | .227 | |||
|
| |||||||
| 3 | AIS → SPEQ (b) | .020 | .003 | 7.293 | <.001 | .015 | .025 |
| PSS → SPEQ (c′) | .004 | .005 | 0.852 | .395 | −.006 | .014 | |
| PSS→ SPEQ (c) | .009 | .005 | 1.733 | .084 | −.001 | .019 | |
| PSS → AIS → SPEQ (a*b) | .005 | .002 | .001 | .009 | |||
Note. a = Effect of X on M; b = Effect of M on Yi; c = Total effect of X on Yi; c′ = Direct effect of X on Yi controlling for M; Path a is equal across all models; therefore, it presented only in the model with Y1 to avoid redundancies. N = 365 for analyses of models Y1-Y4. The standard error and 95% CI for a*b are obtained by bootstrap with 10,000 re-samples. PSS (Perceived Stress Scale) is the predictor, AIS (Avoidance and Inflexibility Scale) is the explanatory variable, and FTND (nicotine dependence; Y1), BCS (Barriers to Cessation Scale; Y2), and SPEQ (Severity of Problems Experienced while Quitting; Y3) are the outcome variables. CI (lower) = lower bound of a 95% confidence interval; CI (upper) = upper bound; → = affects.
Specificity Analyses
To further strengthen interpretation of results, PSS and AIS variables were reversed for each of the three models tested previously (Preacher, 2004). Tests of the indirect effects in these models were estimated based on 10,000 bootstrap re-samples. All results of the reversed models were non-significant.
Discussion
As hypothesized, perceived stress had an indirect effect on the studied dependent measures through smoking-specific experiential avoidance. The observed effects were evident after accounting for gender, presence of an Axis I disorder, and negative affectivity. Although the present research design did not permit explication of the temporal ordering of the observed associations, confidence in the observations was improved by evaluating an alternative model in which the predictors (i.e., PSS and AIS) were reversed. All alternative models emerged as non-significant, indicating that the studied smoking variables are not solely a set of ‘interrelated constructs.’ These data collectively suggest smoking-specific experiential avoidance may be a mechanism linking perceived stress and smoking behavior. It is possible that smokers with greater levels of perceived stress perceive life events and internal sensations as more personally distressing, and therefore, may be more apt to respond to such distress with escape/avoidance via smoking; a process that may contribute to more severe smoking behavior. Indeed, the present findings corroborate and add to a burgeoning body of work examining experiential avoidance constructs as underlying mechanisms in the relation between neuroticism/negative affectivity related variables (e.g., perceived stress, worry, anxiety sensitivity) and smoking behavior (Buckner, Zvolensky, Farris, & Hogan, 2014; Johnson, Farris, Schmidt, & Zvolensky, 2012; Farris et al., 2014).
Although not a primary study aim, two noteworthy finding emerged. First, perceived stress and smoking-specific experiential avoidance were related, but distinct constructs. Indeed, these two constructs shared approximately 7% of variance with one another. This observation lends further empirical support to the construct validity for the clinical relevance of the smoking-specific experiential avoidance construct in tobacco research/practice. Second, consistent with extant work (Cohen et al., 1993; Watson, 1988; Watson & Clark, 1992), perceived stress and negative affect were highly correlated. Despite this correlation, the variance inflation factors (VIF = 1.64) suggests that these measures are distinct constructs (O’brien, 2007).
Clinically, the present data suggest that smoking-specific experiential avoidance may serve as an explanatory mechanism in perceived stress-smoking relations. Understanding such mechanisms may help develop targeted smoking cessation interventions. Pending further replication and extension using prospective methodology, it may be advisable to address smoking-specific experiential avoidance among smokers who report elevated levels of perceived stress. For example, providing acceptance-based training to assist with accepting (versus avoiding) distressing smoking-related sensations, thoughts, and feeling states to smokers making a quit attempt may facilitate greater smoking cessation, particularly for those who report elevated perceived stress. Indeed, acceptance-based interventions demonstrate promising results at reducing smoking among the general population (Bowen & Marlatt, 2009; Brewer et al., 2011; Brown et al., 2008; Gifford et al., 2004; McCallion & Zvolensky, 2015).
There are a number of study limitations that warrant comment. First, the cross-sectional nature of the study design does not allow for testing of temporal sequencing. Although alternate analyses were conducted to strengthen confidence in the observed associations, future prospective studies are needed in further determining directional effects. Prospective studies should examine changes in study variables over time to establish temporal sequencing necessary for a mediation model. Second, the current sample was homogenous and consisted of primarily White, community-recruited, treatment-seeking, daily cigarette smokers with a moderate smoking rate. Future studies may benefit by sampling ethnically diverse, lighter and heavier smokers to ensure the generalizability of the results to the general smoking population. Finally, internal consistency for FTND total score was relatively low. It is not uncommon, however, to find lower internal consistency with shorter scales (e.g., scales with less than 10 items; DeVellis, 2003) and the observed internal consistency was comparable to that of studies exploring the psychometrics of the measure (Haddock, Lando, Klesges, Talcott, & Renaud, 1999; Richardson & Ratner, 2005).
Overall, the present study serves as an initial investigation into the nature of the association among perceived stress, smoking-specific experiential avoidance, and an array of clinically-significant smoking constructs. The findings of the current study suggest smoking-specific experiential avoidance may represent a possible underlying variable linking perceived stress and smoking behavior.
Highlights.
Stress indirectly related to nicotine dependence through experiential avoidance.
Stress indirectly related to barriers to cessation through experiential avoidance.
Stress indirectly related to quit problems through experiential avoidance.
Smoking-specific experiential avoidance links perceived stress and smoking.
Acknowledgments
Grant Support: This work was supported by a National Institutes of Health (NIH) grant awarded to Drs. Michael J. Zvolensky and Norman B. Schmidt (R01-MH076629-01A1).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Bibliography
- al’Absi M, Hatsukami D, Davis GL. Attenuated adrenocorticotropic responses to psychological stress are associated with early smoking relapse. Psychopharmacology. 2005;181(1):107–117. doi: 10.1007/s00213-005-2225-3. [DOI] [PubMed] [Google Scholar]
- Allison PD. Missing data. Vol. 136. Sage publications; 2001. [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychological review. 2004;111(1):33. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Bowen S, Marlatt A. Surfing the urge: brief mindfulness-based intervention for college student smokers. Psychology of Addictive Behaviors. 2009;23(4):666. doi: 10.1037/a0017127. [DOI] [PubMed] [Google Scholar]
- Brewer DD, Catalano RF, Haggerty K, Gainey RR, Fleming CB. A meta-analysis of predictors of continued drug use during and after treatment for opiate addiction. Addiction. 1998;93(1):73–92. [PubMed] [Google Scholar]
- Brewer JA, Mallik S, Babuscio TA, Nich C, Johnson HE, Deleone CM, Weinstein AJ. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug and Alcohol Dependence. 2011;119(1):72–80. doi: 10.1016/j.drugalcdep.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology. 2002;111(1):180. [PubMed] [Google Scholar]
- Brown RA, Palm KM, Strong DR, Lejuez CW, Kahler CW, Zvolensky MJ, Gifford EV. Distress tolerance treatment for early-lapse smokers rationale, program description, and preliminary findings. Behavior Modification. 2008;32(3):302–332. doi: 10.1177/0145445507309024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Zvolensky MJ, Farris SG, Hogan J. Social anxiety and coping motives for cannabis use: The impact of experiential avoidance. Psychology of Addictive Behaviors. 2014;28:568–574. doi: 10.1037/a0034545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Kalra DL, Carey KB, Halperin S, Richards CS. Stress and unaided smoking cessation: A prospective investigation. Journal of Consulting and Clinical Psychology. 1993;61(5):831. doi: 10.1037//0022-006x.61.5.831. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983:385–396. [PubMed] [Google Scholar]
- Cohen S, Lichtenstein E. Perceived stress, quitting smoking, and smoking relapse. Health Psychology. 1990;9(4):466. doi: 10.1037//0278-6133.9.4.466. [DOI] [PubMed] [Google Scholar]
- Cohen S, Tyrrell DA, Smith AP. Negative life events, perceived stress, negative affect, and susceptibility to the common cold. Journal of Personality and Social Psychology. 1993;64(1):131. doi: 10.1037//0022-3514.64.1.131. [DOI] [PubMed] [Google Scholar]
- Cosci F, Corlando A, Fornai E, Pistelli F, Paoletti P, Carrozzi L. Nicotine dependence, psychological distress and personality traits as possible predictors of smoking cessation. Results of a double-blind study with nicotine patch. Addictive Behaviors. 2009;34(1):28–35. doi: 10.1016/j.addbeh.2008.08.003. [DOI] [PubMed] [Google Scholar]
- DeVellis R. Scale development: Theory and applications. Thousand Oaks, CA: Sage Publication; 2003. [Google Scholar]
- Farris SG, Zvolensky MJ, DiBello AM, Schmidt NB. Validation of the Avoidance and Inflexibility Scale (AIS) among treatment-seeking smokers. Psychological Assessment. doi: 10.1037/pas0000059. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farris SG, Zvolensky MJ, Norton PJ, Hogan J, Smith AH, Talkovsky AM, Schmidt NB. Smoking-Specific Experiential Avoidance is Indirectly Associated with Trait Worry and Smoking Processes among Treatment-Seeking Smokers. Behavioral Medicine. 2014 doi: 10.1080/08964289.2014.984650. (just-accepted), 00–00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farris SG, Zvolensky MJ, Schmidt NB. Smoking-specific experiential avoidance cognition: Explanatory relevance to pre-and post-cessation nicotine withdrawal, craving, and negative affect. Addictive Behaviors. 2014 doi: 10.1016/j.addbeh.2014.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for Axis I DSM-IV Disorders - Patient Edition (SCID-I/P, Version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute; 1994. [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Antonuccio DO, Piasecki MM, Rasmussen-Hall ML, Palm KM. Acceptance-based treatment for smoking cessation. Behavior Therapy. 2004;35(4):689–705. doi: 10.1016/j.beth.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Pierson HM, Piasecki MP, Antonuccio DO, Palm KM. Does acceptance and relationship focused behavior therapy contribute to bupropion outcomes? A randomized controlled trial of functional analytic psychotherapy and acceptance and commitment therapy for smoking cessation. Behavior Therapy. 2011;42(4):700–715. doi: 10.1016/j.beth.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Haddock CK, Lando H, Klesges RC, Talcott GW, Renaud EA. A study of the psychometric and predictive properties of the Fagerström Test for Nicotine Dependence in a population of young smokers. Nicotine & Tobacco Research. 1999;1(1):59–66. doi: 10.1080/14622299050011161. [DOI] [PubMed] [Google Scholar]
- Hayes A. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Methodology in the social sciences. New York, NY: The Guilford Press; 2013. [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76(4):408–420. [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG, Bissett RT, Pistorello J, Toarmino D, McCurry SM. Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record. 2004;54(4):553–578. [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction to Alcohol and Other Drugs. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hildebrandt MJ, Hayes SC. The contributing role of negative affectivity and experiential avoidance to increased cardiovascular risk. Social and Personality Psychology Compass. 2012;6(8):551–565. [Google Scholar]
- Jarvis MJ, Tunstall-Pedoe H, Feyerabend C, Vesey C, Saloojee Y. Comparison of tests used to distinguish smokers from nonsmokers. American Journal of Public Health. 1987;77(11):1435–1438. doi: 10.2105/ajph.77.11.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson KA, Farris SG, Schmidt NB, Zvolensky MJ. Anxiety sensitivity and cognitive-based smoking processes: Testing the mediating role of emotion dysregulation among treatment-seeking daily smokers. Journal of Addictive Diseases. 2012;31:143–157. doi: 10.1080/10550887.2012.665695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karekla M, Panayiotou G. Coping and experiential avoidance: Unique or overlapping constructs? Journal of Behavior Therapy and Experimental Psychiatry. 2011;42(2):163–170. doi: 10.1016/j.jbtep.2010.10.002. [DOI] [PubMed] [Google Scholar]
- Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychological Bulletin. 2003;129(2):270. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. Jama. 2000;284(20):2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing Company LLC; 1984. [Google Scholar]
- Leung DY, Lam T-h, Chan SS. Three versions of Perceived Stress Scale: validation in a sample of Chinese cardiac patients who smoke. BMC Public Health. 2010;10(1):513. doi: 10.1186/1471-2458-10-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macnee CL, Talsma A. Development and testing of the barriers to cessation scale. Nursing Research. 1995;44(4):214–219. [PubMed] [Google Scholar]
- McCallion EA, Zvolensky MJ. Acceptance and Commitment Therapy (ACT) for smoking cessation: a synthesis. Current Opinion in Psychology. 2015;2:47–51. [Google Scholar]
- Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychology. 2003;22(6):638. doi: 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- O’brien RM. A caution regarding rules of thumb for variance inflation factors. Quality & Quantity. 2007;41(5):673–690. [Google Scholar]
- Ockene JK, Mermelstein RJ, Bonollo DS, Emmons KM, Perkins KA, Voorhees CC, Hollis JF. Relapse and maintenance issues for smoking cessation. Health Psychology. 2000;19(1S):17. doi: 10.1037/0278-6133.19.suppl1.17. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, Pomerleau OF. Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addictive Behaviors. 1994;19(1):33–39. doi: 10.1016/0306-4603(94)90049-3. http://dx.doi.org/10.1016/0306-4603(94)90049-3. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Richardson CG, Ratner PA. A confirmatory factor analysis of the Fagerstrom Test for Nicotine Dependence. Addictive Behaviors. 2005;30(4):697–709. doi: 10.1016/j.addbeh.2004.08.015. [DOI] [PubMed] [Google Scholar]
- Schloss HM, Haaga DA. Interrelating behavioral measures of distress tolerance with self-reported experiential avoidance. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2011;29(1):53–63. doi: 10.1007/s10942-011-0127-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnoll RA, Martinez E, Tatum KL, Glass M, Bernath A, Ferris D, Reynolds P. Increased self-efficacy to quit and perceived control over withdrawal symptoms predict smoking cessation following nicotine dependence treatment. Addictive Behaviors. 2011;36(1):144–147. doi: 10.1016/j.addbeh.2010.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacology. 2001;158(4):343–359. doi: 10.1007/s002130100917. [DOI] [PubMed] [Google Scholar]
- Soderstrom M, Dolbier C, Leiferman J, Steinhardt M. The relationship of hardiness, coping strategies, and perceived stress to symptoms of illness. Journal of Behavioral Medicine. 2000;23(3):311–328. doi: 10.1023/a:1005514310142. [DOI] [PubMed] [Google Scholar]
- Tsourtos G, O’Dwyer L. Stress, stress management, smoking prevalence and quit rates in a disadvantaged area: has anything changed? Health Promotion Journal of Australia. 2008;19(1):40–44. doi: 10.1071/he08040. [DOI] [PubMed] [Google Scholar]
- Watson D. Intraindividual and interindividual analyses of positive and negative affect: their relation to health complaints, perceived stress, and daily activities. Journal of Personality and Social Psychology. 1988;54(6):1020. doi: 10.1037//0022-3514.54.6.1020. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Affects separable and inseparable: on the hierarchical arrangement of the negative affects. Journal of Personality and Social Psychology. 1992;62(3):489. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social pPsychology. 1988;54(6):1063. doi: 10.1637/10T0-3590.19.3.253. [DOI] [PubMed] [Google Scholar]
- Zhao X, Lynch JG, Chen Q. Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research. 2010;37(2):197–206. [Google Scholar]
- Zvolensky MJ, Farris SG, Schmidt NB, Smits JA. The role of smoking inflexibility/avoidance in the relation between anxiety sensitivity and tobacco use and beliefs among treatment-seeking smokers. Experimental and Clinical Psychopharmacology. 2014;22(3):229–237. doi: 10.1037/a0035306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Goodie JL, Ruggiero KJ, Black AL, Larkin KT, Taylor BK. Perceived stress and anxiety sensitivity in the prediction of anxiety-related responding: A multichallenge evaluation. Anxiety, Stress & Coping: An International Journal. 2002;15(3):211–229. [Google Scholar]
- Zvolensky MJ, Lejuez CW, Kahler CW, Brown RA. Nonclinical panic attack history and smoking cessation: An initial examination. Addictive Behaviors. 2004;29(4):825–830. doi: 10.1016/j.addbeh.2004.02.017. [DOI] [PubMed] [Google Scholar]