Abstract
Animal studies have shown that the systemic inflammatory response to major injury impairs bone regeneration. It remains unclear whether the systemic immune response contributes to impairment of fracture healing in multitrauma patients. It is well known that systemic inflammatory changes after major trauma affect leukocyte kinetics. We therefore retrospectively compared the cellular composition of peripheral blood during the first 2 weeks after injury between multitrauma patients with normal (n=48) and impaired (n=32) fracture healing of the tibia. The peripheral blood-count curves of leukocytes, neutrophils, monocytes, and thrombocytes differed significantly between patients with normal and impaired fracture healing during the first 2 weeks after trauma (P-values were 0.0122, 0.0083, 0.0204, and <0.0001, respectively). Mean myeloid cell counts were above reference values during the second week after injury. Our data indicate that leukocyte kinetics differ significantly between patients with normal and impaired fracture healing during the first 2 weeks after major injury. This finding suggests that the systemic immune response to major trauma can disturb tissue regeneration.
Keywords: SIRS, inflammation, neutrophils, myelopoiesis, regeneration
Introduction
In developed countries each year, approximately one in 100 inhabitants suffers a fracture.1 In 5%–10% of all cases, fractures fail to heal within 9 months after injury, which is referred to as nonunion.2 Impaired bone healing has a detrimental effect on quality of life and carries a substantial cost to society.3 The direct costs of treating nonunions of the tibia have been estimated between £15,566 and £17,200 per nonunion in the UK, with considerable additional costs due to the loss of productivity of patients during the period of postinjury disability.3
The incidence of nonunion is significantly higher in trauma patients with multiple injuries than in patients with isolated injuries.4 Impaired bone regeneration in multitrauma patients may be caused by several local changes that occur after high-energy impact, such as open fractures, poor condition of the surrounding soft tissue, and large-bone defects.4 However, animal studies suggest that not only local but also systemic changes after multitrauma could disturb fracture healing.5–7 A recent animal study showed that experimental blunt chest injury altered the cellular composition of the fracture hematoma in rats and negatively affected the outcome of bone repair by inducing hypertrophic callus formation.8 Also, intraperitoneal injection of lipopolysaccharides, a frequently used model that mimics a trauma-induced systemic immune response, disturbed fracture healing in rats by inducing hypertrophic callus formation.9 The mechanism through which these systemic changes impaired bone regeneration remains unclear.
Leukocytes play an important role in fracture healing, as leukocytes not only initiate10 but also direct11 bone repair. Changes in the early inflammatory phase of bone repair may thus disturb downstream processes of fracture healing.12 Cytokines released systemically after severe trauma affect leukocyte kinetics, such as leukocyte mobilization from the bone marrow and leukocyte migration toward injured tissue, as well as the phenotype of peripheral blood leukocytes and hematopoiesis.5,8,13 Peripheral blood concentrations of leukocyte subsets, but also of erythrocytes and thrombocytes, thus reflect the systemic immune response to tissue injury.14,15
We hypothesized that these systemic changes after severe injury can impair fracture healing by disturbing the inflammatory phase of bone regeneration. This impairment could be the result of either a changed number or phenotype of inflammatory cells within the fracture hematoma.5 To test whether the systemic immune response to trauma is associated with the outcome of fracture healing, we compared the peripheral blood-count curves of leukocytes, neutrophils, monocytes, lymphocytes, thrombocytes, and hemoglobin during the first 2 weeks after injury between multitrauma patients with normal and impaired fracture healing of the tibia.
Patients and methods
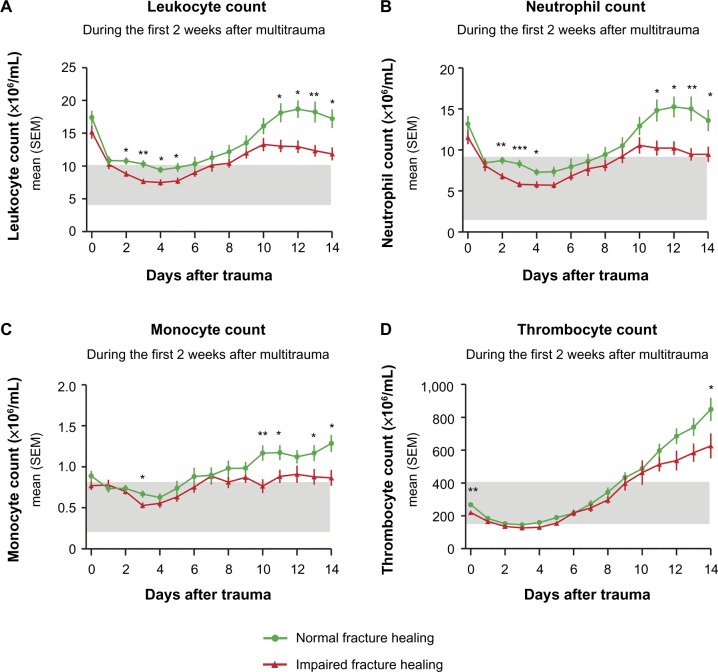
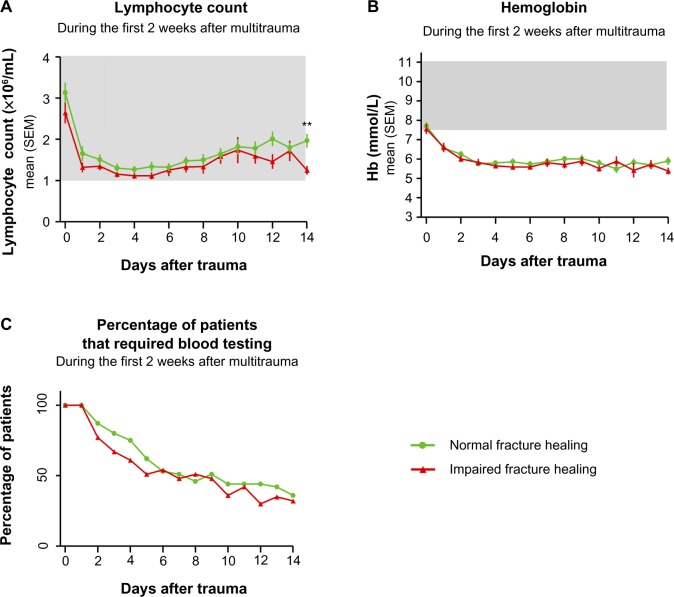
The peripheral blood-count curves of several hematological parameters during the first 2 weeks after injury were compared between multitrauma patients with normal and impaired fracture healing of the tibia. The primary focus of our analysis was comparing the peripheral blood-count curves of leukocytes between both healing groups (Figure 1). In addition to this analysis, peripheral blood-count curves of neutrophils, monocytes, lymphocytes, thrombocytes, and hemoglobin were compared between both healing groups in the context of an explorative subanalysis (Figures 1 and 2). The P-values of these explorative subanalyses were therefore not corrected for multiple testing.
Figure 1.
Peripheral blood counts of leukocytes (A), neutrophils (B), monocytes (C), and thrombocytes (D) during the first 2 weeks after major trauma.
Notes: Patients with normal (green) and impaired (red) fracture healing of the tibia. The peripheral blood-count curves of leukocytes, neutrophils, monocytes, and thrombocytes were analyzed with mixed linear models, and differed significantly between healing groups during the first 2 weeks after trauma (P-values were 0.0122, 0.0083, 0.0204, and <0.0001, respectively). In addition, each separate time point was compared between outcome groups using an independent t-test or nonparametric equivalent. For these subanalyses: *P<0.05; **P<0.01; ***P<0.001. Gray bars represent reference values.
Abbreviation: SEM, standard error of mean.
Figure 2.
Peripheral blood lymphocyte counts (A), hemoglobin values (B) and the percentage of patients that required blood testing on each day (C) during the first two weeks after major trauma for patients with normal (green) and impaired (red) fracture healing of the tibia.
Notes: The peripheral blood lymphocyte counts and hemoglobin values were analyzed with mixed linear models, and these analyses showed no significant differences between the healing groups (P-values 0.0688 and 0.9275, respectively). In addition to the analyses with mixed linear models, each separate time point was also compared between outcome groups using an independent t-test or nonparametric equivalent. For these subanalyses: **P<0.01. Gray bars represent reference values.
Abbreviation: SEM, standard error of mean.
Patient population
From a prospectively collected trauma register, all severely injured trauma patients with tibia fractures who were aged 18 years or older and required clinical admission to the University Medical Center of Utrecht (UMC Utrecht) between January 1, 2005 and May 1, 2012 were evaluated. Severe trauma was defined as an Injury Severity Score (ISS) of 16 or higher.16,17 The following clinical data were obtained: age, sex, trauma mechanism, ISS, associated injuries (abbreviated injury score), characterization of the tibia fracture according to the AO (Arbeitsgemeinschaft für Osteosynthesefragen [association for study of internal fixation]) classification, soft-tissue injury according to the Gustilo classification,18 duration from injury until definitive fracture fixation, type of fracture fixation, number and date of additional surgical interventions, total intensive care stay, total hospital stay, complications, and the outcome of fracture healing. Impaired fracture healing was defined as lack of clinical or radiological evidence of union at the fracture site at least 16 weeks after the index injury or at the most recent intervention.19 Delayed healing was defined as lack of clinical or radiological evidence of union 16–36 weeks after trauma. Nonunion was defined as lack of clinical or radiological evidence of union 36 weeks after trauma or when the patient was subjected to secondary procedures to promote healing. Missing data were retrieved from the hospital’s central electronic medical record if possible. Our study was a retrospective database study with anonymized data, and thus did not need a formal review by an institutional review board.
Hematological parameters
The aforementioned hematological parameters were obtained from the Utrecht Patient Oriented Database (UPOD). The technical details of the UPOD are described elsewhere.20 In short, the UPOD is an infrastructure of relational databases that allows (semi)automated transfer, processing, and storage of data, including administrative information, medical and surgical procedures, medication orders, and laboratory-test results for all clinically admitted patients and patients attending the outpatient clinic of UMC Utrecht since 2004. The process and storage of data are in accordance with privacy and ethics regulations. UPOD data acquisition and data management is in line with current Dutch regulations concerning privacy and ethics and is approved by the institution’s medical ethics committee (UMC Utrecht). Because no extra material were taken from patients eg blood samples, there was no requirement to obtain informed consent from individual patients. The data were analyzed anonymously. Routine hematological analysis was performed by using the Cell-Dyn Sapphire hematology analyzer (Abbott Laboratories, Abbott Park, IL, USA).21,22 The reliability and validity of the laboratory results were monitored through routine quality control. The percentages of patients that required blood testing on each day during the first 2 weeks after injury are depicted in Figure 2C.
Statistical analysis
Categorical variables were compared between the healing groups with the χ2 test. Based on whether continuous data were normally distributed, an independent t-test or Mann–Whitney U test was used. The equality of variances was assessed with a Levene’s test.
The mean hematological parameters (leukocytes, leukocyte subsets, thrombocytes, and hemoglobin) are considered repeated measurements, and the values of each patient for different time points are thus not completely independent. We analyzed the course of hematological parameters over time using linear mixed models, because these models can adequately compare repeated measurements between outcome groups, they allow correction for possible confounders, and they work well in the presence of missing data in repeated measurements.23 This analysis only indicates whether the course of hematological parameters differs between outcome groups during the first 2 weeks after injury, but does not allow determination of which days exactly the outcome groups differ. We could not use the same linear mixed model technique to perform a post hoc subanalysis on the first and second weeks separately to determine whether the difference in hematological parameters occurred early or late after injury. Such analyses should have either been defined as primary analysis (not post hoc on the same data set) or should be performed on a different data set than on which the original analysis was performed.
However, in order to speculate on which days the differences between outcome groups was most evident, we additionally compared all hematological parameters between outcome groups with an independent t-test or nonparametric equivalent for each time point (Figures 1 and 2). The results of the independent t-tests and nonparametric equivalents are thus mainly illustrative, and we base our conclusions on the results of the linear mixed models.
We first determined whether the trends of hematological parameters over time were best described by a linear, quadratic, or cubic function. To test whether the trends of hematological parameters differed between outcome groups, we fitted two models for each hematological parameter.
The first model allowed the outcome groups to differ both on average and in trend over time, and thus included fixed effects for the appropriate polynomial time trends: an indicator for “outcome group” (normal versus impaired fracture healing), and the interaction between “outcome group” and time trends. The second model assumes that the outcome groups have the same average and trend over time, and thus only had fixed effects for time trends. We corrected for possible confounding by adding clinical parameters to both of these models that significantly differed between outcome groups. The percentage of patients that were treated nonoperatively and the percentage of patients that had open fractures (Gustilo grade I and higher)18 significantly differed between outcome groups, and thus these parameters were added to both models. The given P-values therefore represent differences between outcome groups that cannot solely be explained by differences in type of management or presence of open fractures. The two models were compared using a likelihood-ratio test: when the first model significantly fitted the observed data better than the second model (which assumes that both outcome groups have the same average and trend over time), it was concluded that the curve of that hematological parameter significantly differed between outcome groups after correcting for possible confounders. In order to minimize multicollinearity of the polynomial terms for time, orthogonal polynomials were used.23 For each outcome, random effects per patient for the intercept and time trends were used in the models to account for the correlation of repeated measurements within patients. P<0.05 was considered statistically significant. Mixed model analysis was performed using R software version 2.10.0.24 All other statistical analyses were performed with IBM SPSS version 20.
Results
Patient characteristics
A total of 123 multitrauma patients with a tibia fracture were treated in UMC Utrecht between January 1, 2005 and May 1, 2012; 16 patients died during their hospital stay, and 13 were lost to follow-up. Another 14 patients were excluded, due to bone disease (n=2), a history of malignancy (n=4), paraplegia (n=1), or amputation of the affected leg (n=7). Of the remaining 80 patients, 13 (16.3%) developed delayed union, and 19 patients (23.8%) developed nonunion that required intervention, leading to a total of 32 patients (40%) with impaired fracture healing. Clinical parameters of separate fracture healing groups (normal versus impaired) are shown in Table 1. There was no significant difference in the age, sex, extent of injuries based on the ISS and New ISS, distribution or severity of associated injuries (data not shown), the localization of the tibia fracture (proximal, shaft, distal, or intra-articular), the complexity of the fracture (AO classification), or the incidence of (infectious) complications between the healing groups. There were significantly more open fractures (56% versus 31%, P=0.037) and significantly more operatively treated fractures (19% versus 0, P=0.010) in the impaired-healing group compared to patients with normal fracture healing. Nonoperative treatment and open fractures were thus both considered as potential confounders and added to the statistical model used to test whether the curves of hematological parameters differed significantly between healing groups.
Table 1.
Overview of clinical parameters of patients with normal and impaired fracture healing of the tibia
| All patients, n=80 | Normal healing, n=48 (60%) | Impaired healing, n=32 (40%) | P-value | |
|---|---|---|---|---|
| Age | 40 [24–55] | 37 [24–58] | 42 [25–54] | NS |
| Sex | 58% male | 54% male | 63% male | NS |
| Injury severity Score | 25 [19–34] | 25 [18–34] | 24 [19–33] | NS |
| New Injury severity Score | 27 [22–41] | 31 [22–34] | 27 [22–41] | NS |
| Number of fractures | 4 [2–5] | 3 [2–5] | 4 [2–6] | NS |
| Tibia-fracture localization | ||||
| – proximal | 20% | 20% | 19% | NS |
| – shaft | 49% | 48% | 52% | NS |
| – distal | 31% | 32% | 29% | NS |
| Type of tibia fracture (AO) | ||||
| – multifragmentary/complex | 37% | 32% | 45% | NS |
| – intra-articular | 31% | 32% | 29% | NS |
| Soft-tissue injury (Gustilo) | ||||
| – 0 closed fracture | 59% | 69% | 44% | 0.037 |
| – I wound <1 cm | 14% | 13% | 16% | NS |
| – II wound >1 cm with moderate soft tissue damage | 15% | 10% | 22% | NS |
| – III wound >1 cm with | ||||
| ➢IIIa adequate soft-tissue cover | 6% | 6% | 6% | NS |
| ➢IIIb inadequate soft-tissue cover | 5% | 2% | 9% | NS |
| ➢IIIc associated arterial injury | 1% | 0% | 3% | NS |
| Time until tibia fixation (days) | 0 [0–5] | 0 [0–5] | 1 [0–6] | NS |
| Type of fixation | ||||
| – nonoperative | 11% | 19% | 0% | 0.010 |
| – ORIF | 43% | 44% | 41% | NS |
| – nail (ETN, UTN, or CTN) | 44% | 38% | 53% | NS |
| – external | 3% | 0% | 6% | NS |
| Number of operations | 2 [1–4] | 2 [1–3] | 2 [1–5] | NS |
| ICU stay (days) | 0 [0–8] | 1 [0–9] | 0 [0–7] | NS |
| 5.1 (8.3) | 4.9 (7.5) | 5.4 (9.4) | ||
| Hospital stay (days) | 27 [14–50] | 27 [14–50] | 28 [12–46] | NS |
| Complications | 56% | 56% | 56% | NS |
| – infectious | 41% | 44% | 38% | NS |
| – sepsis | 9% | 8% | 9% | NS |
| – noninfectious | 31% | 27% | 38% | NS |
| Delayed union | 16% | – | 41% | – |
| Nonunion | 24% | – | 59% | – |
| – atrophic | – | – | 47% | – |
| – hypertrophic | – | – | 53% | – |
Note: Data shown as median ± [interquartile range] or mean ± (standard deviation).
Abbreviations: NS, not significant; AO, arbeitsgemeinschaft für Osteosynthesefragen (association for study of internal fixation); ORIF, open reduction internal fixation; ETN, expert tibial nail; UTN, unreamed tibial nail; CTN, cannulated tibial nail; ICU, intensive care unit.
Hematological parameters
Figure 1A depicts the mean leukocyte counts in peripheral blood during the first 2 weeks after injury for patients with normal and impaired fracture healing of the tibia. The two leukocyte-count curves differed significantly between both healing groups when the aforementioned confounders were included in the statistical model (P=0.0122). The average leukocyte counts were above reference values (indicated by gray shading) at admittance to the emergency department, and there was no significant difference in leukocyte counts at arrival between the healing groups. After day 1, mean leukocyte counts decreased to reference values. From day 5 onward, leukocyte numbers increased in both healing groups and rose above reference values after day 7 in both groups. Leukocyte counts increased further and peaked at day 12 in the normal-healing group, whereas leukocyte numbers peaked at day 10 in the impaired-healing group. When each time point was analyzed separately, the mean leukocyte counts differed significantly between outcome groups on days 2, 3, 4, 5, 11, 12, 13, and 14 (Figure 1A).
Mean neutrophil counts, monocyte counts, and thrombocyte counts rose above reference values in the second week after trauma (Figure 1, B–D). In contrast, lymphocyte numbers remained within the normal boundaries and hemoglobin values remained below reference values during the entire 2 weeks after trauma (Figure 2, A and B). Neutrophil-, monocyte-, and thrombocyte-count curves were significantly different for both healing groups (P-values 0.0083, 0.0204 and <0.0001, respectively). The curves of lymphocyte-count and hemoglobin values did not significantly differ between healing groups (P-values 0.0688 and 0.9275, respectively). When each time point was analyzed separately, mean neutrophil counts differed significantly between outcome groups on days 2, 3, 4, 11, 12, 13, and 14 (Figure 1B). Mean monocyte counts differed significantly on days 3, 10, 11, 13, and 14 (Figure 1C), and mean thrombocyte counts were significantly different between outcome groups on day 0 and day 14 (Figure 1D).
Complications
A total of 45 patients (56%) developed 69 complications: 33 (41%) patients developed 41 infectious complications, and 25 patients (31%) developed 28 noninfectious complications. Infectious complications included 14 remote wound infections, two wound infections at the tibia-fracture site, nine pneumonias, eight sepses, six urinary tract infections, and two other infectious complications. There was no significant difference between the normal and impaired healing groups in the percentage of patients who developed either infectious or noninfectious complications (Table 1).
Discussion
This is the first clinical study to investigate the relationship between the systemic immune response to severe injury and outcome of bone regeneration. We demonstrated that peripheral blood-leukocyte kinetics differed significantly between multitrauma patients with normal and impaired fracture healing of the tibia during the first 2 weeks after injury (Figure 1A). The difference in leukocyte-count curves between the groups may either reflect increased extravasation of leukocytes toward injured tissue or a blunt trauma-induced bone marrow response. It is well known that the systemic inflammatory response after major trauma affects leukocyte kinetics and increased migratory function of leukocytes,8,25 as well as bone marrow failure,13,26,27 and have both been described in the literature.
Several animal studies have illustrated the importance of local controlled inflammation for adequate bone healing. For instance, transplantation of the early fracture hematoma, which predominantly contains inflammatory cells, into muscle tissue of rats induces ectopic bone formation within muscle tissue.11 These experiments suggest that inflammatory cells can initiate downstream processes of bone healing. Moreover, removal or repetitive irrigation of the early fracture hematoma impairs fracture healing in rats.10
Although these studies illustrate the importance of local controlled inflammation for adequate bone healing, other studies have shown that local or systemic “hyperinflammatory” conditions can impair fracture healing. For instance, injection of β-glucan into the fracture site induces local hyperinflammation and impairs fracture healing in rats.12 In addition, intraperitoneal injection of lipopolysaccharides in rats, which induces systemic inflammation, negatively affects the outcome of bone healing.9 Moreover, blunt chest injury, which is a model of trauma-induced systemic inflammation, also impairs fracture healing in rats.28,29
It is well known that multitrauma patients have an increased risk of developing delayed union and nonunion.4 Based on the aforementioned animal studies, we hypothesized that systemic inflammatory changes after major trauma contribute to this high incidence of impaired bone healing in severely injured individuals.5 We now show a correlation between leukocyte kinetics early after injury and the eventual outcome of bone healing in multitrauma patients, which supports this hypothesis.
The primary focus of our analysis was comparing the peripheral blood-count curves of leukocytes between the healing groups. However, the UPOD also stores the number of leukocyte subsets in peripheral blood, even when clinicians do not request these values. Analysis of these subsets as a secondary outcome contributes to the understanding of the mechanism behind the difference in systemic immune response between outcome groups. However, we did not power our study to include multiple leukocyte subsets, as our research population was too small. Therefore, we did not correct for multiple testing, and only analyzed subsets in the context of an explorative subanalysis.
These explorative subanalyses showed that neutrophil, monocyte, and thrombocyte counts were above reference values during the second week after injury in both healing groups, in contrast to lymphocyte counts and hemoglobin values (Figures 1 and 2). These findings suggest that trauma induces an increased concentration of myeloid cells within peripheral blood during the second week after trauma, potentially by stimulation of myelopoiesis.
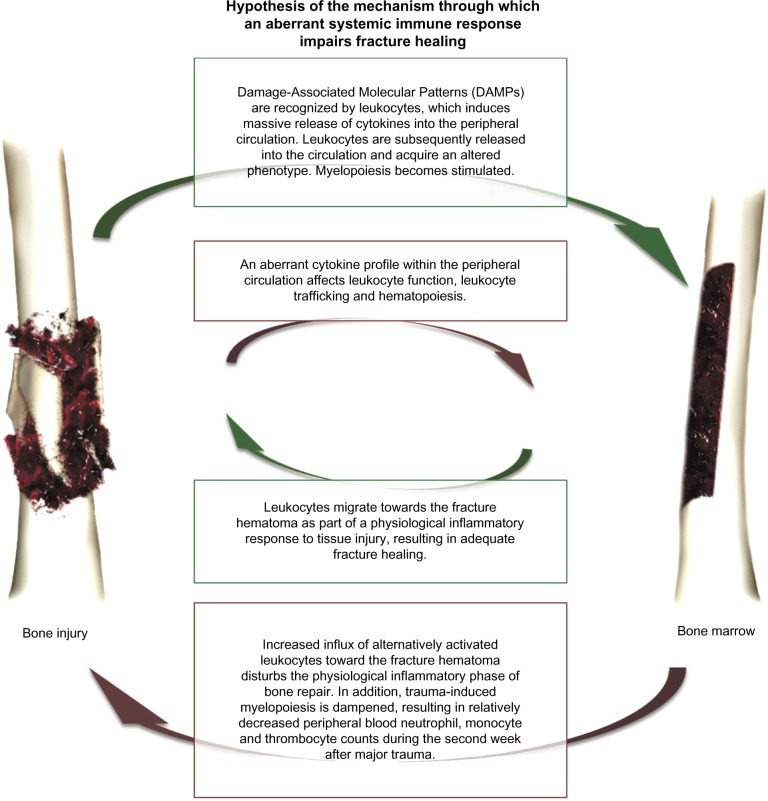
When outcome groups were compared, we found that peripheral blood neutrophil, monocyte, and thrombocyte counts were lower (Figure 1, B–D) in the impaired fracture-healing group. These findings may be explained by relative inhibition of trauma-induced myelopoiesis in the impaired-healing group. It remains unclear whether there is a causal relation between inhibition of trauma-induced myelopoiesis and poor bone regeneration or whether these two phenomena are separate consequences of an aberrant systemic immune response without a causal relation between them. We hypothesize that systemic inflammatory changes after major trauma affect the concentration or phenotype of inflammatory cells within the fracture hematoma and thereby disturb fracture healing (Figure 3).8
Figure 3.
Our hypothesis of the mechanism through which an aberrant systemic immune response to trauma impairs fracture healing.
Note: The green boxes describe a physiological systemic immune response to major trauma, and the red boxes describe a different detrimental systemic immune response.
Factors that may contribute to a different systemic immune response include the type and extent of injury, the time between injury and resuscitation, the amount of ischemia/reperfusion damage, or host factors, such as smoking and genetic background, infectious complications, and the type, timing, and number of operative procedures.5
We found no significant difference in the incidence of infectious complications, total amount of tissue damage, or severity and localization of injuries. However, our study did not have enough power to state that all aforementioned parameters were equally distributed between the outcome groups. Moreover, we were only able to compare the amount of tissue injury based on clinical scales of severity (ISS and New ISS). These scales may not be sensitive enough to detect biological differences in the amount of tissue injury between the groups. The only differences between the two groups were that the impaired-healing group had a significantly higher percentage of open fractures and a higher percentage of operatively treated fractures (Table 1). Open fractures and open surgical treatment have previously been described as risk factors of impaired fracture healing.4 It remains unclear whether these parameters can significantly affect systemic immune response rapidly after injury. Therefore, we considered these factors as possible confounders and added these parameters to all statistical analysis. The difference in systemic immune response remained statistically significant even after correcting for these possible confounders.
The strength of our study lies predominantly in the fact that the UPOD allowed us to analyze retrospectively hematological parameters of multitrauma patients and to correlate these values with the outcome of fracture healing, even when clinicians did not request these parameters. Potential limitations of our study are that it was retrospective, comprised a relatively small cohort, and blood sampling was not performed daily in all patients.
Future research should focus on strategies that enable early identification of multitrauma patients who will mount an undesirable systemic immune response to trauma and may thus require interventions that prevent development of impaired fracture healing. Moreover, the mechanism through which an altered systemic immune response can impair bone regeneration needs to be clarified, in order to develop therapies that prevent nonunion after an undesirable systemic immune response to severe injury.
In conclusion, our data indicate that leukocyte kinetics differ significantly between patients with normal and impaired fracture healing during the first 2 weeks after major injury. This finding supports the hypothesis that certain systemic inflammatory changes after extensive tissue injury can disturb tissue regeneration.
Acknowledgments
The authors would like to acknowledge the financial support provided by the AO Foundation (grant S-09-89L) and the Alexandre Suerman MD/PhD grant provided by UMC Utrecht. The study sponsors were not involved in the study design, collection, analysis, interpretation of data, writing of the manuscript, or the decision to submit the manuscript for publication. The results of this study have been presented as an oral presentation at the 14th European Congress of Trauma and Emergency Surgery, Lyon, France, May 4–7, 2013, and the abstract will be published online in a supplement of the European Journal of Trauma and Emergency Surgery. The authors would like to thank Hanneke den Breeijen and Leon Stijvers for retrieving data from the UPOD, as well as Bob Surie for retrieving data from the trauma register. For this study, data from the UPOD were used. The UPOD is an infrastructure of relational databases comprising data on patient characteristics, hospital-discharge diagnoses, medical procedures, medication orders, and laboratory tests for all patients treated at UMC Utrecht since 2004. UMC Utrecht is a 1,042-bed academic teaching hospital in the center of the Netherlands, with annually about 28,000 clinical and 15,000 day-care hospitalizations and 334,000 outpatient visits. UPOD data acquisition and management is in accordance with current regulations concerning privacy and ethics. The structure and content of the UPOD have been described in more detail elsewhere.21
Footnotes
Author contributions
OB mainly designed the study, performed statistical analysis, and wrote the article, AK acquired data and contributed to drafting of the manuscript, RS performed statistical analysis, contributed to the design of the study, and revised the manuscript, and LK, WVS, LL, and TB contributed to the design of the study and revised the manuscript. All authors approved the final manuscript and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.van Staa TP, Dennison EM, Leufkens HG, Cooper C. Epidemiology of fractures in England and Wales. Bone. 2001;29:517–222. doi: 10.1016/s8756-3282(01)00614-7. [DOI] [PubMed] [Google Scholar]
- 2.Mills LA, Simpson AH. The relative incidence of fracture non-union in the Scottish population (5.17 million): a 5-year epidemiological study. BMJ Open. 2013;3:e002276. doi: 10.1136/bmjopen-2012-002276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kanakaris NK, Giannoudis PV. The health economics of the treatment of long-bone non-unions. Injury. 2007;38(Suppl 2):S77–S84. doi: 10.1016/s0020-1383(07)80012-x. [DOI] [PubMed] [Google Scholar]
- 4.Karladani AH, Granhed H, Kärrholm J, Styf J. The influence of fracture etiology and type on fracture healing: a review of 104 consecutive tibial shaft fractures. Arch Orthop Trauma Surg. 2001;121:325–328. doi: 10.1007/s004020000252. [DOI] [PubMed] [Google Scholar]
- 5.Bastian O, Pillay J, Alblas J, Leenen L, Koenderman L, Blokhuis T. Systemic inflammation and fracture healing. J Leukoc Biol. 2011;89:669–673. doi: 10.1189/jlb.0810446. [DOI] [PubMed] [Google Scholar]
- 6.Claes L, Recknagel S, Ignatius A. Fracture healing under healthy and inflammatory conditions. Nat Rev Rheumatol. 2012;8:133–143. doi: 10.1038/nrrheum.2012.1. [DOI] [PubMed] [Google Scholar]
- 7.Pape HC, Marcucio R, Humphrey C, Colnot C, Knobe M, Harvey EJ. Trauma-induced inflammation and fracture healing. J Orthop Trauma. 2010;24:522–525. doi: 10.1097/BOT.0b013e3181ed1361. [DOI] [PubMed] [Google Scholar]
- 8.Recknagel S, Bindl R, Brochhausen C, et al. Systemic inflammation induced by a thoracic trauma alters the cellular composition of the early fracture callus. J Trauma Acute Care Surg. 2013;74:531–537. doi: 10.1097/TA.0b013e318278956d. [DOI] [PubMed] [Google Scholar]
- 9.Reikerås O, Shegarfi H, Wang JE, Utvåg SE. Lipopolysaccharide impairs fracture healing: an experimental study in rats. Acta Orthop. 2005;76:749–753. doi: 10.1080/17453670510045327. [DOI] [PubMed] [Google Scholar]
- 10.Park SH, Silva M, Bahk WJ, McKellop H, Lieberman JR. Effect of repeated irrigation and debridement on fracture healing in an animal model. J Orthop Res. 2002;20:1197–1204. doi: 10.1016/S0736-0266(02)00072-4. [DOI] [PubMed] [Google Scholar]
- 11.Mizuno K, Mineo K, Tachibana T, Sumi M, Matsubara T, Hirohata K. The osteogenetic potential of fracture haematoma: subperiosteal and intramuscular transplantation of the haematoma. J Bone Joint Surg Br. 1990;72:822–829. doi: 10.1302/0301-620X.72B5.2211764. [DOI] [PubMed] [Google Scholar]
- 12.Grundnes O, Reikeraas O. Effects of macrophage activation on bone healing. J Orthop Sci. 2000;5:243–247. doi: 10.1007/s007760050159. [DOI] [PubMed] [Google Scholar]
- 13.Raff G, Livingston DH, Wang MT, Rameshwar P. Hemorrhagic shock abolishes the myelopoietic response to turpentine-induced soft tissue injury. J Surg Res. 1995;59:75–79. doi: 10.1006/jsre.1995.1134. [DOI] [PubMed] [Google Scholar]
- 14.Pillay J, Hietbrink F, Koenderman L, Leenen LP. The systemic inflammatory response induced by trauma is reflected by multiple phenotypes of blood neutrophils. Injury. 2007;38:1365–1372. doi: 10.1016/j.injury.2007.09.016. [DOI] [PubMed] [Google Scholar]
- 15.Hietbrink F, Koenderman L, Althuizen M, Leenen LP. Modulation of the innate immune response after trauma visualised by a change in functional PMN phenotype. Blood. 2009;40:851–855. doi: 10.1016/j.injury.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 17.Copes WS, Champion HR, Sacco WJ, Lawnick MM, Keast SL, Bain LW. The Injury Severity Score revisited. J Trauma. 1988;28:69–77. doi: 10.1097/00005373-198801000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742–746. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Schofer MD, Block JE, Aigner J, Schmelz A. Improved healing response in delayed unions of the tibia with low-intensity pulsed ultrasound: results of a randomized sham-controlled trial. BMC Musculoskelet Disord. 2010;11:229. doi: 10.1186/1471-2474-11-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ten Berg MJ, Huisman A, van den Bemt PM, Schobben AF, Egberts AC, van Solinge WW. Linking laboratory and medication data: new opportunities for pharmacoepidemiological research. Clin Chem Lab Med. 2007;45:13–19. doi: 10.1515/CCLM.2007.009. [DOI] [PubMed] [Google Scholar]
- 21.Müller R, Mellors I, Johannessen B, et al. European multi-center evaluation of the Abbott Cell-Dyn sapphire hematology analyzer. Lab Hematol. 2006;12:15–31. [PubMed] [Google Scholar]
- 22.Kang SH, Kim HK, Ham CK, Lee DS, Cho HI. Comparison of four hematology analyzers, CELL-DYN Sapphire, ADVIA 120, Coulter LH 750, and Sysmex XE-2100, in terms of clinical usefulness. Int J Lab Hematol. 2008;30:480–486. [PubMed] [Google Scholar]
- 23.Hedeker D, Gibbons RD. Longitudinal Data Analysis. Hoboken (NJ): John Wiley and Sons; 2006. [Google Scholar]
- 24.R Project for Statistical Computing [website on the Internet] [Accessed February 2, 2016]. Available from: www.r-project.org.
- 25.Pallister I, Dent C, Topley N. Increased neutrophil migratory activity after major trauma: a factor in the etiology of acute respiratory distress syndrome? Crit Care Med. 2002;30:1717–1721. doi: 10.1097/00003246-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Livingston DH, Anjaria D, Wu J, et al. Bone marrow failure following severe injury in humans. Ann Surg. 2003;238:748–753. doi: 10.1097/01.sla.0000094441.38807.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sifri ZC, Kaiser VL, Ananthakrishnan P, et al. Bone marrow failure in male rats following trauma/hemorrhagic shock (T/HS) is mediated by mesenteric lymph and modulated by castration. Shock. 2006;25:12–16. doi: 10.1097/01.shk.0000188708.97153.ce. [DOI] [PubMed] [Google Scholar]
- 28.Recknagel S, Bindl R, Kurz J, et al. Experimental blunt chest trauma impairs fracture healing in rats. J Orthop Res. 2011;29:734–739. doi: 10.1002/jor.21299. [DOI] [PubMed] [Google Scholar]
- 29.Recknagel S, Bindl R, Kurz J, et al. C5aR-antagonist significantly reduces the deleterious effect of a blunt chest trauma on fracture healing. J Orthop Res. 2012;30:581–586. doi: 10.1002/jor.21561. [DOI] [PMC free article] [PubMed] [Google Scholar]