Abstract
Improving school water, sanitation and hygiene (WASH) conditions has been shown to be effective in reducing pupil absence and illness. However, the benefit of sanitation and hygiene promotion improvements at school may depend on the conditions of the latrines and availability of consumables. We employed a three-arm, cluster-randomized trial to determine if a low-cost, policy-relevant, environmental-level latrine cleaning intervention could a) improve latrine cleanliness, b) increase latrine use, and c) reduce absenteeism. We assessed absence via periodical roll-call among 17,564 pupils in 60 schools that previously received WASH Improvements as part of the SWASH+ project. Latrine conditions and use were also assessed using structured observation. Latrine cleanliness increased significantly during the post-intervention period among schools receiving the latrine-cleaning package compared to controls. Handwashing with soap increased as well in intervention schools relative to controls. We found no difference in latrine use and absence across arms. The additive impact of cleaning may not have been strong enough to impact absence above and beyond reductions attributable to the original WASH infrastructure improvements and basic hygiene education the schools previously received. Improving latrine conditions is important for the dignity and well being of pupils, and investments and strategies are necessary to ensure school sanitation environments are clean and pupil-friendly.
Introduction
Improved access to sanitation has been shown to reduce helminth infection and diarrheal disease by providing a space for excreta disposal (Ziegelbauer et al., 2012, Cairncross et al., 2010). Sanitation facilities, however, may also increase exposure to pathogens if poorly maintained, used incorrectly, or if personal and hand hygiene materials are not available during and after use. High levels of microbial contamination have been found in sanitation facilities (Majra and Gur, 2010, Pickering et al., 2012, Sinclair and Gerba, 2011) and the spread of infectious diseases, including diarrhea, dysentery, and Hepatitis A, have been linked to unsanitary toilets (Koopman, 1978, Rajaratnam et al., 1992, Thomas and Tillett, 1973).
Water, sanitation and hygiene (WASH) related illnesses have been estimated to result in hundreds of millions of days of school absence (Hutton and Haller, 2004), yet these projections are based on conditions in the home and do not account for the burden of disease resulting from inadequate access in the school setting. Data on school WASH access is poor, however, UNICEF estimates that 49% of schools in low income settings have inadequate access to water, 55% have inadequate access to sanitation (UNICEF, 2012); no current estimates exist for the availability of soap or handwashing facilities.
Improving school WASH conditions has been shown to be effective in reducing pupil absence and illness (Freeman et al., 2014, Freeman et al., 2012, Freeman et al., 2013). School-based handwashing interventions have shown reductions in pupil absenteeism of 21% to 54% (Talaat et al., 2011, Bowen et al., 2007) and interventions that include both handwashing and water treatment have shown reductions in pupil absenteeism of 26% to 58% (Blanton et al., 2010, O’Reilly et al., 2008) and specifically for girls (Freeman et al., 2012).
The benefit of sanitation and hygiene improvements at school may depend on the consistent availability of soap and water for handwashing and on the conditions of the latrines, rather than on pupil to latrine ratios. In Kenya, baseline data from a cluster-randomized trial of school-based WASH interventions suggested that the quality of latrine facilities had a stronger correlation with recent absence (Dreibelbis et al., 2013), and the impact evaluation of the trial did not find evidence that construction of new latrines reduced absence compared to controls (Freeman et al., 2012). Pupils in schools that received new latrines had higher levels of fecal pathogens on their hands than those in schools that did not (Greene et al., 2012) and pupils reported latrine conditions—the presence of urine, feces, mud, blood, flies and smell—to be a barrier to use (Caruso et al., In Press).
Informed by these findings, we employed a three-arm, cluster-randomized trial to determine if the sustained provision of a latrine cleaning intervention could reduce pupil absence from rural primary schools in Western Kenya. We hypothesized that these low-cost, environmental-level interventions would a) improve latrine cleanliness, b) increase latrine use, and c) reduce absenteeism.
Methods
Context
This study included schools previously enrolled in a cluster-randomized trial assessing the impact of a school-based hygiene promotion, water treatment, sanitation and water supply improvement program on pupil absence in Nyanza Province, Kenya (Freeman et al., 2012). This study took place in Nyando, Kisumu and Rachuonyo Districts in Nyanza Province, the western-most province of Kenya on the eastern shore of Lake Victoria. Rachuonyo District is considered geographically more rural than Nyando and Kisumu. Nyanza has 5.4 million inhabitants with 1.5 million (28%) attending primary school (KNBS, 2011a, KNBS, 2011b, KNBS, 2010).
Sample size
Data from the previous trial revealed that children in schools with better latrine conditions had a two-week absence period prevalence of 0.126, compared to 0.147 in those with poorer latrine conditions. To detect a significant risk ratio of 0.86 in absence, the present study required 20 schools per intervention arm and 20 schools in the control arm, assuming a mean enrollment of 300 pupils per school (k= 0.087, alpha=0.05, beta=0.20) (Hayes and Bennett, 1999).
School selection
Schools were eligible for inclusion in the study if they were: enrolled in the SWASH+ study that did not receive an improved water source as part of the intervention (n=135), had a dry season water source less than 1000 meters (1 km) away, and had greater than 25% of their school’s latrines identified as dirty (excess smell, flies, and/or presence of feces) in a 2009 program facilities assessment). Sixty-two schools met eligibility criteria. Two schools were omitted from participation because of participation in pilot testing of intervention components and flooding that disrupted school grounds, facilities, and regular school activities. Stratified random assignment was used to allocate the remaining 60 schools to one of three intervention arms: Latrine Cleaning plus Handwashing (LC+HW), Handwashing (HW), and a control (C) (Figure 1). A latrine cleaning intervention without the handwashing component was considered, however latrine cleaning may increase risk of pathogen exposure and it was deemed necessary to include a handwashing component to reduce that risk. Schools were stratified by both geographic strata (Rachuonyo or Nyando/Kisumu) and by the intervention previously received as part of SWASH+. Stratification was undertaken to ensure geography and previous intervention types were distributed across arms in similar proportion. Schools were then assigned using the random number generator in Microsoft Excel (Redmond, WA) prior to baseline data collection.
Figure 1.
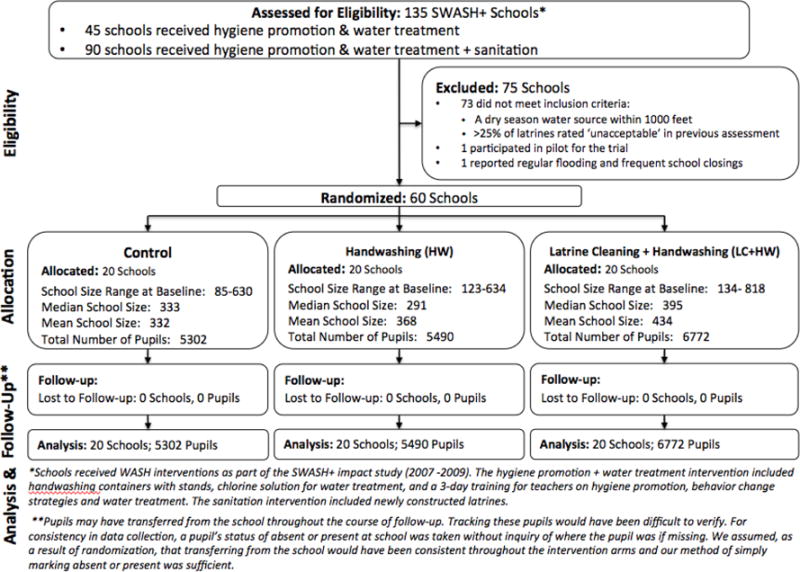
Flow Chart indicating School and Pupil Eligibility, Randomization, Allocation, Follow-up and Analysis.
Interventions
The interventions selected for this trial focused on changing the school environment and were designed to be low cost, policy relevant, and easily replicable at scale (see Table 1). Inputs were informed by focus group discussions and interviews with pupils between July and October 2009 (Caruso et al., In Press) and were piloted in three schools (February–March 2010). Inputs for the two intervention arms—Latrine Cleaning plus Handwashing (LC+HW) and Handwashing (HW)—are described in Table 1.
Table 1.
Intervention components and input costs by study arm
| Latrine Cleaning + Handwashing (LC+HW) | Handwashing (HW) | |||
|---|---|---|---|---|
a. Clean latrine package1
|
||||
b. Handwashing Materials
|
a Handwashing Materials
|
|||
c Head Teacher and Health Patron Training
|
b. Head Teacher and Health Patron Training
|
|||
|
Per school
|
Per pupil
|
|||
| Kenya Shillings | US Dolars | Kenya Shillings | US Dolars | |
| Average Intervention Input Costs at Implementation | ||||
| LC+HW | 8,530.00 | 110.59 | 28.43 | 0.37 |
| HW | 780.00 | 10.11 | 2.60 | 0.03 |
| Average Intervention Input Costs at Midpoint2 | ||||
| LC+HW | 5,089.25 | 65.98 | 16.96 | 0.22 |
| HW | 666.50 | 8.64 | 2.22 | 0.03 |
| Total Intervention Costs for 2 Terms | ||||
| LC+HW | 13,619.25 | 176.57 | 45.40 | 0.59 |
| HW | 1,446.50 | 18.75 | 4.82 | 0.05 |
Schools received 1 latrine cleaning package for every 4 latrine doors. Even numbers of latrine packages were distributed per school for equity of supply availability among girls and boys. Four packages per school were distributed on average.
After 1 term, supply levels were refreshed as needed. At a minimum, all schools received an additional 3.5 kg bag of Omo for handwashing and all LC+HW schools received 4 3.5 kg bags of Omo and 4 bottles Jik for cleaning.
Schools in the LC+HW arm received reusable hardware (buckets, brooms, hand brushes, plastic scoop), consumables (bleach, powdered soap), toilet tissue, handwashing materials, sheets for pupils to monitor latrines conditions daily, and training for two teachers—the head teacher and health patron.
Toilet tissue was included as a type of preventative cleaning supply to dissuade smearing of feces on walls, a behavior pupils reported performing when they lack anal cleansing materials (McMahon et al., 2011a). Kenya’s National School Health Guidelines indicate that schools should be providing appropriate anal cleansing materials like toilet paper to pupils (MOPHS, 2009) and pupils involved in focus group discussions from rural schools in the same province indicated that toilet paper was a preferred anal cleansing material (McMahon et al., 2011a). We piloted toilet tissue in three schools prior to the trial and in informal interviews, pupils responded positively to having it available for use (data unpublished). Recognizing the potential risk of pathogen exposure to pupils engaged in latrine cleaning, materials were provided to make soapy water for handwashing, which including powdered soap and plastic bottles (Saboori et al., 2010).
Training sessions were conducted with one head teacher and one health patron from each school in the LC+HW arm. Health patrons were selected for inclusion because they are teachers who are specifically responsible for the school WASH environment (no additional pay provided for this responsibility). Head teachers were included because they supervise health patrons and are responsible for the pupils and the overall school environment.
All head teachers and health patrons were trained to instruct pupils to: 1) use the materials provided for latrine cleaning; 2) monitor latrine conditions with a structured observation sheet; and 3) make soapy water. For latrine cleaning, methods for cleaning were demonstrated with all necessary supplies during the training. Teachers were provided with a step-by-step instruction sheet, which included a list of the materials needed; how to prepare, use, and store cleaning materials; and a reminder to wash hands after cleaning. Instructions were informed by conversations with and observations of teachers and pupils in the pilot schools. For latrine monitoring, teachers were provided with a binder of monitoring sheets and were shown how to use them. Teachers were advised to have two pupils—one girl and one boy—observe latrines each day before lunch. Pupils would use a structured monitoring sheet to indicate which latrines had a bad, good, or very good conditions, specifically, smell, flies, presence of feces on walls and floor, and urine. Pupils also recorded the amount of supplies available at the beginning and end of the week, which allowed the research team to see if more supplies were needed and how fast they were used. Teachers were also advised to come up with a system to equitably assign these responsibilities to students at their school. Finally, teachers were reminded of the critical times to wash hands and encouraged to remind the students in their schools. Inputs for the LC+HW arm cost 176.57USD per school, approximately 0.59USD per pupil.
The HW arm was included in order to determine if handwashing inputs alone have an impact on absenteeism. Schools in the HW arm received powdered soap, plastic bottles and training, which cost 18.75USD per school, approximately 0.06USD per pupil.
Distribution of intervention supplies and training of head teachers and school health patrons on use of materials was led by CARE Kenya with support from the research team in June 2010 after baseline data collection. All schools in the intervention arms were provided additional supplies after the August school holiday as needed. Neither the schools nor the field enumerators were blinded to the intervention assignments.
Data Collection
Trained enumerators from the Great Lakes University of Kisumu collected data in all schools at baseline (June 2010) and every two weeks from July through November 2010 (excluding August school break), for a total of five rounds of data collection post-implementation.
Latrine and handwashing conditions
Latrine and handwashing conditions were observed at each round and recorded using Syware Visual CE v10 software (Cambridge, MA) on Dell Axim x51 (Round Rock, TX) personal digital assistants. Five latrine conditions were assessed and rated from 0 (absence) to 2 (strong presence): presence of feces, urine, flies, smell, and mud. At baseline, two enumerators independently collected conditions data at schools. Each enumerator followed standard data collection protocols, but start times were arranged such that that conditions were observed without the presence of the other enumerator but close enough in time to ensure that the observed conditions had not changed between these two observations. Data from the two baseline observations were used to assess inter-rater reliability and internal consistency of conditions reporting. At the time of baseline data collection, enumerators were unaware of intervention allocation. For consistency and precision of subsequent data collection rounds, all latrines doors in each school were labeled at baseline using black permanent marker and were observed at the start of a school visit. Availability of handwashing water and soap / soapy water was assessed at the start of recess periods as teachers were advised to keep soapy water bottles in classrooms when not on recess to avoid theft and to assign a student to be in charge of bringing the bottles to the handwashing facility at the start and end of recess periods. Teachers were also advised to put bottles in an accessible and visible location for those accessing facilities during class time. Guidance to teachers was informed by feedback from teachers who were involved in the pilot phase.
Latrine use and handwashing behavior
Latrine use and handwashing behavior were observed during 30-minute morning class recess. Structured observations were conducted with paper tools by trained enumerators who recorded if a girl or boy pupil entered a latrine block, what block it was, and whether or not the pupil washed their hands afterwards. Enumerators placed themselves in discrete locations where they each monitored a different set of latrines.
Absenteeism
Pupil absence was assessed via roll call. Enumerators created school-specific registries at baseline that included the names of all pupils enrolled at the school and their sex and age (if known). Roll was called at each unannounced visit, pupils announced if they were present, and they were marked absent or present.
Statistical Methods
School enrollment and WASH data, including number of pupils per school, use of improved water source, distance to primary water source within less than 1 km, and sex-specific pupil to latrine ratios, were calculated and qualitatively compared at baseline to assess balance of intervention arms. All data were cleaned and analyzed using SAS v9.2 (Cary, NC).
Latrines were analyzed at the individual door level to determine if the intervention improved conditions. A latrine cleanliness score was calculated as the sum of five latrine conditions: presence of smell, feces, urine, flies, and mud. Baseline inter-rater reliability (ICC 1,k =0.88) and internal consistency (ICC 3,k= 0.79) of the score were high (Portney and Watkins, 1999). Post-implementation, each latrine cleanliness score was averaged across rounds and linear regression models accounting for clustering of data at the school-level were used to assess magnitude and significance of change.
To determine if the intervention improved school latrine use, handwashing conditions, and handwashing, school-level aggregated proportions of each set of indicators (averaged over each of the follow-ups) were compared between the intervention and control arms. Baseline levels were included in the model to enable a comparison of the change in each set of indicators from baseline to follow-up between the intervention and control arms. All models account for the stratified randomization (by geographic strata), baseline conditions, and the clustering in the study design, by using SAS survey procedures (e.g. PROC SURVEYREG).
To test our hypothesis that the latrine cleaning intervention would reduce absence, we employed multivariable linear regression models. Absence was determined for each pupil as the number of days absent from school over the total number of days observed post-implementation. The proportion of days of absence for each pupil was modeled against intervention status controlling for geographic strata and baseline school-level absence. A full model also included potential confounders: baseline school enrollment and community socioeconomic status (SES). Community SES was calculated using principal components analysis during the initial trial (Freeman et al., 2012). School-specific baseline absence is the proportion of students absent at baseline in each school specific to sex and grade. Accurate absenteeism data were not available at baseline for 8 of the schools (2 HW, 6 C) because pupils were elsewhere for ‘athletic days’ on the date of visit. Subsequent rounds could not be used as a proxy for baseline as some schools had received interventions at that time. Regression imputation was used to estimate school-specific baseline absence by sex and grade for the schools missing data. Standard errors were adjusted to account for clustering at the school level (PROC SURVEYREG).
Results are presented for the entire school-population and are also stratified by sex and grade group. Sex stratification was determined a priori based on known differences in absence by sex. Grade groups were developed to reflect pupil schedules: pupils in grades 1–3 only attend school in the morning; pupil in grades 4–7 attend school all day; and pupils in grade 8 have a rigorous examination schedule that determines secondary school placement and is hypothesized to influence attendance.
Ethics
Ethics approval was granted by the Institutional Review Board at Emory University (Atlanta, GA) and the Ethical Review Committee at the Great Lakes University of Kisumu (Kisumu, Kenya). All schools in both the HW and Control arms received the same inputs as the LC+HW arm at the end of the study.
Results
Baseline pupil and school characteristics
A total of 17,564 pupils enrolled in 60 participating schools at baseline were tracked for absence. There were more pupils enrolled in the LC+HW schools (6,772) than in the HW (5,490) or control (5,302) schools (Table 2). The proportion of pupils absent at baseline was lowest among control schools (9.8%) and highest among HW schools (12.9%). A greater proportion of LC+HW schools had an improved water source (85%) compared to other arms (65%). HW schools had a lower proportion of pupils per latrine (girls: 29.1, boys: 31.1), than those in the LC+HW (girls: 40.6, boys: 45.0) or control (girls: 42.4, boys, 34.2) arms.
Table 2.
Pupil characteristics and school WASH conditions at baseline for all trial arms
| Control
|
HW
|
LC+HW
|
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Pupil enrollment | 5302 | 5490 | 6772 | |||
| Grades 1–3 | 2127 | 40.1% | 2236 | 40.7% | 2680 | 39.6% |
| Girls | 1061 | 49.9% | 1094 | 48.9% | 1307 | 48.8% |
| Grades 4–7 | 2693 | 50.8% | 2822 | 51.4% | 3465 | 51.2% |
| Girls | 1361 | 50.5% | 1403 | 49.7% | 1751 | 50.5% |
| Grade 8 | 482 | 9.1% | 432 | 7.9% | 627 | 9.3% |
| Girls | 193 | 40.0% | 177 | 41.0% | 261 | 41.6% |
| District | ||||||
| Nyando/Kisumu | 2551 | 48.1% | 2884 | 52.5% | 3836 | 56.6% |
| Rachuonyo | 2751 | 51.9% | 2606 | 47.5% | 2936 | 43.4% |
| Pupil absence1 | 375 | 9.8% | 623 | 12.9% | 862 | 12.7% |
| Grades 1–3 | 195 | 12.2% | 317 | 15.9% | 399 | 14.9% |
| Boys | 92 | 11.4% | 162 | 15.9% | 199 | 14.5% |
| Girls | 103 | 13.1% | 155 | 16.0% | 200 | 15.3% |
| Grades 4–7 | 164 | 8.6% | 290 | 11.7% | 418 | 12.1% |
| Boys | 90 | 9.4% | 141 | 11.4% | 225 | 13.1% |
| Girls | 74 | 7.8% | 149 | 12.0% | 193 | 11.0% |
| Grade 8 | 16 | 4.8% | 16 | 4.3% | 45 | 7.2% |
| Boys | 11 | 5.7% | 12 | 5.5% | 25 | 6.8% |
| Girls | 5 | 3.6% | 4 | 2.7% | 20 | 7.7% |
| District | ||||||
| Nyando/Kisumu | 180 | 9.7% | 300 | 12.4% | 466 | 12.1% |
| Rachuonyo | 195 | 9.9% | 323 | 13.4% | 396 | 13.5% |
| School facilities (n = 20) | ||||||
| Water | ||||||
| Current water source improved | 13 | 65.0% | 13 | 65.0% | 17 | 85.0% |
| Current water source >1 km away | 2 | 20.0% | 1 | 5.0% | 1 | 5.0% |
| Sanitation | ||||||
| Mean girls per latrine (SD) | 42.4 | (34.4) | 29.1 | (16.5) | 40.6 | (27.4) |
| Mean boys per latrine (SD) | 34.2 | (32.6) | 31.1 | (19.7) | 45.0 | (34.1) |
Baseline data was collected at all schools, however events were being held at some Control and HW schools which resulted in high rates of absenteeism that day. Therefore, baseline absenteeism was determined for only those schools that did not have an irregular event.
Process outcomes
At each round, at least 79% of the LC+HW schools reported having the brooms, brushes, and buckets provided as part of the intervention (data not shown). There was a slight drop in the availability of disinfectant products among LC+HW schools during the data collection round immediately after the August school holiday. At that time, only 55% of schools had bleach and 75% had powdered detergent; additional cleaning supplies were provided within two weeks. At all subsequent follow-up rounds, over 80% of schools reported having these items. Half (50%) of LC+HW schools, 55% of HW schools, and 25% of control schools had handwashing water available, and only 35% of LC+HW, 10% of HW schools, and 0% of control schools had soap available at all follow-up observations (See: (Saboori et al., 2013)).
Impact on latrine cleanliness, use and handwashing
The mean latrine cleanliness score during the post-intervention period increased among the LC+HW schools only, and was significantly higher (7.8, p=0.01) than cleanliness scores for the control schools (6.9; Table 3). Other latrine conditions, like drainage and proportion with a door, did not change between baseline and follow-up and were not statistically different between arms at follow-up. Latrine use was comparable at baseline between all arms. Aggregated use over follow-up rounds demonstrates an increase in latrine use across all arms. Use in LC+HW schools was not statistically higher compared to other arms.
Table 3.
Baseline and follow-up for each intermediate outcome, reported by study arm
| Control
|
HW
|
LC+HW
|
||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up1 | Baseline | Follow-up1 | p-value2 | Baseline | Follow-up1 | p-value2 | |
| Sanitation | ||||||||
| Latrine conditions | (n = 203 latrines) | (n = 240 latrines) | (n = 237 latrines) | |||||
| Cleanliness score | 7.3 (0.4) | 6.9 (0.3) | 6.6 (0.3) | 6.2 (0.3) | 0.11 | 7.5 (0.3) | 7.8 (0.2) | 0.01 |
| Drainage score | 5.9 (0.0) | 5.8 (0.1) | 5.6 (0.2) | 5.7 (0.1) | 0.35 | 5.7 (0.1) | 5.7 (0.0) | 0.76 |
| Proportion with door | 0.7 (0.0) | 0.7 (0.0) | 0.7 (0.1) | 0.7 (0.0) | 0.13 | 0.7 (0.7) | 0.8 (0.0) | 0.47 |
| School latrine use | (n = 20 schools) | (n = 20 schools) | (n = 20 schools) | |||||
| % of pupils that used a latrine | 12.7% (1.3) | 16.0% (1.7) | 12.2% (1.3) | 17.8% (1.5) | 0.29 | 13.3% (1.7) | 15.0% (1.4) | 0.52 |
| Handwashing | ||||||||
| School handwashing conditions | ||||||||
| Water in HW container | 70.0% (10.7) | 68.3% (7.2) | 65.0% (11.2) | 78.3% (6.4) | 0.27 | 90.0% (7.0) | 84.2% (4.7) | 0.17 |
| Soap available at HW containers | 30.0% (10.8) | 5.0% (2.3) | 10.0% (6.7) | 55.4% (5.5) | <0.01 | 30.0% (10.7) | 72.5% (6.8) | <0.01 |
| % of pupils that handwash after latrine use3 | ||||||||
| Washed with soap and water | 3.6% (2.2) | 2.9% (1.4) | 1.3% (1.0) | 31.3% (3.6) | <0.01 | 6.3% (4.6) | 38.2 (5.55) | <0.01 |
| Any type of handwashing | 11.6% (3.3) | 33.3% (4.0) | 13.9% (5.2) | 48.6% (3.9) | 0.03 | 17.9% (5.4) | 51.7% (5.3) | 0.01 |
Data are mean (SD) or% (SE).
Follow-up values are averaged over all of the follow-up rounds.
P-value comparing intervention arm to control arm, accounting for baseline values, the stratified randomization, and the clustering in the study design.
Denominator is “% of pupils that used a latrine,” as shown above.
Soap was available at handwashing stations more often during recess in LC+HW (73%, p<0.01) and HW (55%, p<0.01) schools during follow-up than in controls (5%). Water was observed in handwashing containers no more often in the LC+HW (84%, p=0.17) and HW schools (78%, p=0.27) compared to control schools (68%), though a greater percentage of LC+HW and HW schools had water available compared to controls (Table 3).
A greater percentage of pupils in intervention schools practiced any kind of handwashing (LC+HW: 51.7%, p=0.02; HW: 48.6%, p=0.03; control: 33.3%) and handwashing with soap (LC+HW: 38.2%, p<0.01; HW: 31.3%, p<0.01; control: 2.9%) compared to those in control schools. An in-depth discussion of handwashing conditions and behaviors, with sex disaggregated findings and assessment of hand contamination by study arm has been reported elsewhere (Saboori et al., 2013).
Impact on absence
Mean absence over the follow-up rounds was greater for boys and girls in all grade groups across all intervention arms as compared to the single baseline measure with the exception of girls in schools with the LC+HW intervention (Table 4). Except for boys in grades 1–3 of the control schools, this trend is consistent with baseline data demonstrating higher absence in grades 1–3 and declines through subsequent grade groups.
Table 4.
Mean absence among primary school pupils by intervention type, grade group, and sex during follow-up (rounds 4–8) (N = 17,564)
| Control
|
HW
|
LC+HW
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | N | Mean | SD | |
| Overall | 5302 | 0.143 | 0.264 | 5490 | 0.143 | 0.249 | 6772 | 0.140 | 0.244 |
| Grades 1–3 | |||||||||
| Boys | 1066 | 0.128 | 0.244 | 1142 | 0.155 | 0.258 | 1373 | 0.152 | 0.259 |
| Girls | 1061 | 0.152 | 0.280 | 1094 | 0.150 | 0.262 | 1307 | 0.146 | 0.259 |
| Grades 4–7 | |||||||||
| Boys | 1332 | 0.168 | 0.282 | 1419 | 0.149 | 0.247 | 1714 | 0.149 | 0.241 |
| Girls | 1361 | 0.145 | 0.267 | 1403 | 0.135 | 0.240 | 1751 | 0.144 | 0.241 |
| Grade 8 | |||||||||
| Boys | 289 | 0.087 | 0.188 | 255 | 0.081 | 0.178 | 366 | 0.063 | 0.170 |
| Girls | 193 | 0.075 | 0.204 | 177 | 0.127 | 0.266 | 261 | 0.068 | 0.176 |
Data are analyzed at the pupil level and only include pupils registered at the school at the time of baseline data collection.
The adjusted absence rate among pupils in control schools was 12.6% during the intervention period, which was no different than that in HW schools (−0.3% difference, 95% confidence interval [CI]: −3.1;2.5) or LC+HW (+0.1% difference, 95% CI: −2.4;2.6). Neither intervention had a measureable impact on student absence when data were stratified by sex or grade group. Models with only design variables were not substantially different than the full models based on effect estimates and standard errors. All model parameters are shown in supplementary material.
Discussion
This is the first trial designed to assess the impact of a scalable, low-cost, school-level latrine cleaning supply intervention on pupil absence. All trial schools had previously received WASH interventions as part of the SWASH+ impact study, which found no significant difference in absenteeism among schools that just received water treatment and hygiene promotion and those that received new sanitation infrastructure (Freeman et al., 2012). This intervention was designed based on findings that latrine cleanliness was associated with reduced odds of absence (Dreibelbis et al., 2013), and pupils reported latrine conditions to be a barrier to use (Caruso et al., In Press). Handwashing materials and education were included to limit potential exposures among pupils who participated in cleaning given that the addition of new school latrines significantly increased risk of E. coli hand contamination among girls (Greene et al., 2012). We hypothesized that the intervention would improve latrine cleanliness, leading to increased use and reduced absenteeism among schools that had already received WASH infrastructure improvements and basic hygiene education.
Schools that received the LC+HW package had significantly cleaner latrines at follow-up rounds compared with those that did not receive the intervention, however we did not find a significant increase in use or a reduction in absenteeism as hypothesized. There are a few possible explanations. First, improving latrine cleanliness may not have improved latrine conditions enough to encourage use. Certain structural components—like floor, wall or door materials—make cleaning more difficult (Luby et al., 2010) and these components, while improved, may not have been clean enough. Integrity of latrine structures may also impair use. The LC+HW intervention did not aim to improve structural conditions and these did not change as a result of our intervention. Future work should investigate how both cleanliness and structural conditions impact use of specific latrines, and if latrines with specific characteristics are used more frequently than others. Our simple, five-item measure proved reliable and would be easy to adapt to assess latrine cleanliness over time in other locations. A measure for assessing latrine structures should also be created and applied.
Second, the latrine cleaning intervention may not have been in place long enough to influence pupil behavior and to change previously established habits. The intervention was designed to be scalable and focused on environmental-level improvements alone. It did not include a behavior change component that specifically motivated pupils to use latrines and did not train pupils to use latrines correctly. Individual-level training on latrine use has been recommended (Le et al., 2012) and may have been effective, particularly for younger pupils given reports that young pupils are primarily responsible for making the latrines dirty (unpublished findings from piloting phase). In addition, increased emphasis on clean latrines could have made pupils feel intimidated to use latrines if they feared being held responsible for making them dirty.
Finally, the additive impact of cleaning may not have been strong enough to impact absence above and beyond reductions attributable to the original WASH infrastructure improvements and basic hygiene education. While pupils should have access to facilities that are clean, other facility attributes may be more necessary to influence use and absence behavior. For example, girls who are menstruating have indicated that they want access to water and a place to dispose of used sanitary materials inside latrines in order to manage menses effectively in the school setting (Long et al., 2013, Haver et al., 2013, Caruso et al., 2013, Crofts and Fisher, 2012, McMahon et al., 2011b, Sommer et al., 2014). Regardless of cleanliness, girls may elect to not use latrines or not attend school if latrines are not equipped appropriately. Evaluation of latrines that suit the specific needs of girls is needed.
A significantly greater proportion of LC+HW and HW schools had soap available during recess periods and a significantly greater proportion of students from LC+HW and HW were observed washing their hands after latrine use compared to controls. While handwashing has been shown to decrease risk of diarrhea and respiratory disease (Burton et al., 2011, Cairncross et al., 2010, Rabie and Curtis, 2006), increased availability of supplies and handwashing behavior in the intervention schools did not result in a decrease of absenteeism. Rates of handwashing may not have been high enough to reduce pathogen exposure in the school community and therefore impact health and absence. An assessment of E. coli contamination on pupil hands in a subset of the trial schools (N=24) found that there was a non-significant reduction in contamination compared to controls (Saboori et al., 2013).
While consistent soap provision and moderate teacher training can influence pupil handwashing behavior, a more intensive behavior change intervention directly engaging and motivating students may be more effective at increasing the proportion of students washing hands after latrine use and in decreasing hand contamination. Intensive pupil behavior change efforts will only be effective if water and soap—or equivalent culturally acceptable handwashing solutions—are available. Research has demonstrated that increased budgets for operational WASH costs positively impacted availability of needed supplies in schools, but did not ensure that students had access to those supplies once they were procured (Alexander et al., 2013). More intensive behavior change may also need to occur among those teachers who are responsible for making water and soap available to pupils when they need it. This study did not directly observe or evaluate teacher behaviors or determine what factors motivated or hampered their ability to perform the behaviors they were hoped to perform. Because teachers play such a critical role in helping to sustain an enabling WASH environment, understanding teacher behaviors and creating teacher-specific behavioral programs may positively influence school WASH environments and student practices. In other words, behavior change strategies should focus simultaneously on motivating students to use latrines and wash hands and on encouraging teachers and school management committees to do their part in sustaining the conditions needed to allow students to practice the behaviors they are taught.
Limitations
This study had four primary limitations. First, randomization was expected to result in uniform school conditions across arms. However, more +HW schools had access to an improved water source and had hand-washing three water available at first visit compared to other arms. LC+HW schools also had higher latrine cleanliness scores at baseline, potentially limiting any marginal impact attributable to the intervention. A strength of the design is that randomization should lead to balance of confounders across intervention arms. Second, this intervention was initiated at the start of the second term and ran only through the end of the school year (end of term 3). The intervention may not have been in place long enough to influence and sustain latrine use behavior change. Moreover, starting the intervention during the school year may have been a disadvantage. Habits may have already been formed and harder to change than if it had been initiated at the start of the school year prior to the establishment of habitual behaviors around latrine use. Third, because of study timing and other constraints, we were not able to carry out qualitative work at the close of the study to gain pupil insights about the interventions. We did pilot the interventions and make improvements to the intervention packages prior to the trial, however a follow-up qualitative study may have helped to explain the results found and to provide suggestions for further improvement from the perspective of pupils. Finally, because this was a school-level intervention, blinding was impossible. This may have introduced courtesy bias in intervention schools that were aware of their involvement in the study. However, all school visits were unannounced and schools did not specifically know what conditions were being observed. Any courtesy bias was likely minimal. Despite strong inter-rater reliability of latrine condition observations at baseline, lack of blinding may have also introduced reporting bias on the part of our enumerator team. This bias may have exaggerated differences in conditions between intervention and control schools. However, noted differences are consistent with more objective observation measures (i.e.: soap and water available for handwashing) the impact of this bias was likely minimal.
Conclusion
Provision of low-cost, locally available materials alongside a low-intensity teacher training led to increased latrine cleanliness in +HW schools and greater availability of handwashing materials and increased handwashing behavior in LC+HW and HW schools over the course of the study period. However, we did not find evidence that our intervention increased use of latrines or pupil absence. Regardless, improving latrine conditions is important for the dignity and well being of those pupils who are using the latrines, and investments and strategies should continue to be undertaken that make school sanitation environments clean and pupil-friendly. Soap provision influences handwashing behavior and efforts should be made to ensure supplies are consistently available. For both latrine use and handwashing behavior, more intensive behavior change strategies should be formulated and tested in the school setting to ensure that healthy habits can be established and maintained at school.
Supplementary Material
Table 5.
Adjusted estimates of absence by intervention group, assessing all pupils collectively and stratifying by sex
| Parameter | All pupils
|
Boys
|
Girls
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Proportion absence | 95% CI | p-value | Proportion absence | 95% CI | p-value | Proportion absence | 95% CI | p-value | ||||
| All pupils | ||||||||||||
| Control | 0.126 | 0.101 | 0.150 | 0.126 | 0.098 | 0.155 | 0.125 | 0.101 | 0.150 | |||
| HW vs. control | −0.003 | −0.031 | 0.025 | 0.83 | 0.001 | −0.031 | 0.028 | 0.93 | −0.005 | −0.033 | 0.023 | 0.73 |
| HW+LC vs. control | 0.001 | −0.024 | 0.026 | 0.94 | −0.001 | −0.028 | 0.029 | 0.97 | 0.001 | −0.024 | 0.027 | 0.91 |
| Grades 1–3 | ||||||||||||
| Control | 0.140 | 0.105 | 0.175 | 0.131 | 0.085 | 0.178 | 0.15005 | 0.111 | 0.189 | |||
| HW vs. control | 0.014 | −0.016 | 0.044 | 0.34 | 0.028 | −0.004 | 0.060 | 0.09 | 0.001109 | −0.033 | 0.035 | 0.95 |
| HW+LC vs. control | 0.020 | −0.012 | 0.051 | 0.22 | 0.033 | −0.003 | 0.069 | 0.08 | 0.006336 | −0.029 | 0.042 | 0.72 |
| Grades 4–7 | ||||||||||||
| Control | 0.140 | 0.106 | 0.173 | 0.151 | 0.109 | 0.194 | 0.129 | 0.095 | 0.163 | |||
| HW vs. control | −0.018 | −0.047 | 0.011 | 0.22 | −0.020 | −0.054 | 0.014 | 0.24 | −0.016 | −0.045 | 0.012 | 0.25 |
| HW+LC vs. control | −0.009 | −0.037 | 0.019 | 0.53 | −0.017 | −0.048 | 0.014 | 0.28 | −0.001 | −0.030 | 0.029 | 0.96 |
| Grade 8 | ||||||||||||
| Control | 0.067 | 0.036 | 0.098 | 0.079 | 0.044 | 0.113 | 0.050 | 0.011 | 0.088 | |||
| HW vs. control | 0.020 | −0.040 | 0.080 | 0.50 | −0.007 | −0.052 | 0.038 | 0.76 | 0.062 | −0.030 | 0.153 | 0.18 |
| HW+LC vs. control | −0.013 | −0.046 | 0.019 | 0.41 | −0.018 | −0.050 | 0.014 | 0.26 | −0.008 | −0.059 | 0.044 | 0.77 |
Acknowledgments
This research was conducted under the umbrella of SWASH+. SWASH+ was funded by the Bill & Melinda Gates Foundation. The authors wish to thank all pupils and teachers at the school that participated in this study and to acknowledge staff at the Great Lakes University Kisumu who collected this data and at CARE Kenya who made the intervention possible.
References
- Sustainable Sanitation and Water Management: Frameworks and Approaches [Online] Available: http://www.sswm.info/category/planning-process-tools/programming-and-planning-frameworks-Sanitation%20Frameworks%20and%20Approaches [Accessed 31 December 2012.
- ALEXANDER KT, DREIBELBIS R, FREEMAN MC, OJENY B, RHEINGANS R. Improving service delivery of water, sanitation, and hygiene in primary schools: a cluster-randomized trial in western Kenya. J Water Health. 2013;11:507–19. doi: 10.2166/wh.2013.213. [DOI] [PubMed] [Google Scholar]
- BLANTON E, OMBEKI S, OLUOCH GO, MWAKI A, WANNEMUEHLER K, QUICK R. Evaluation of the role of school children in the promotion of point-of-use water treatment and handwashing in schools and households–Nyanza Province, Western Kenya, 2007. The American journal of tropical medicine and hygiene. 2010;82:664–71. doi: 10.4269/ajtmh.2010.09-0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BOWEN A, MA H, OU J, BILLHIMER W, LONG T, MINTZ E, HOEKSTRA RM, LUBY S. A cluster-randomized controlled trial evaluating the effect of a handwashing-promotion program in Chinese primary schools. The American journal of tropical medicine and hygiene. 2007;76:1166–73. [PubMed] [Google Scholar]
- BURTON M, COBB E, DONACHIE P, JUDAH G, CURTIS V, SCHMIDT WP. The effect of handwashing with water or soap on bacterial contamination of hands. International journal of environmental research and public health. 2011;8:97–104. doi: 10.3390/ijerph8010097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CAIRNCROSS S, HUNT C, BOISSON S, BOSTOEN K, CURTIS V, FUNG IC, SCHMIDT WP. Water, sanitation and hygiene for the prevention of diarrhoea. International journal of epidemiology. 2010;39:i193–i205. doi: 10.1093/ije/dyq035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CARUSO B, DREIBELBIS R, OGUTU E, RHEINGANS R. If You Build it Will They Come?: Factors Influencing Rural Primary Pupils’ Urination and Defecation Practices at School in Western Kenya. Journal of Water, Sanitation and Hygiene for Development In Press. [Google Scholar]
- CARUSO BA, FEHR A, INDEN K, SAHIN M, ELLIS A, ANDES KL, FREEMAN MC. WASH in Schools Empowers Girls’ Education in Freetown, Sierra Leone: An Assessment of Menstrual Hygiene Management in Schools. New York: United Nations Children’s Fund; 2013. [Google Scholar]
- CROFTS T, FISHER J. Menstrual hygiene in Ugandan schools: An investigation of low-cost sanitary pads. Journal of Water, Sanitation and Hygiene for Development. 2012;2:50–58. [Google Scholar]
- DREIBELBIS R, GREENE LE, FREEMAN MC, SABOORI S, CHASE RP, RHEINGANS R. Water, sanitation, and primary school attendance: a multi-level assessment of determinants of household-reported absence in kenya. International Journal of Educational Development. 2013;33:457–465. [Google Scholar]
- FREEMAN M, CLASEN T, DREIBELBIS R, SABOORI S, GREENE L, BRUMBACK B, MUGA R, RHEINGANS R. The impact of a school-based water supply and treatment, hygiene, and sanitation programme on pupil diarrhoea: a cluster-randomized trial. Epidemiology and infection. 2014;142:340–351. doi: 10.1017/S0950268813001118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FREEMAN MC, CLASEN T, BROOKER SJ, AKOKO DO, RHEINGANS R. The impact of a school-based hygiene, water quality and sanitation intervention on soil-transmitted helminth reinfection: a cluster-randomized trial. The American journal of tropical medicine and hygiene. 2013;89:875–883. doi: 10.4269/ajtmh.13-0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FREEMAN MC, GREENE LE, DREIBELBIS R, SABOORI S, MUGA R, BRUMBACK B, RHEINGANS R. Assessing the impact of a school-based water treatment, hygiene and sanitation programme on pupil absence in Nyanza Province, Kenya: a cluster-randomized trial. Trop Med Int Health. 2012;17:380–91. doi: 10.1111/j.1365-3156.2011.02927.x. [DOI] [PubMed] [Google Scholar]
- GREENE LE, FREEMAN MC, AKOKO D, SABOORI S, MOE C, RHEINGANS R. Impact of a school-based hygiene promotion and sanitation intervention on pupil hand contamination in Western kenya: a cluster randomized trial. The American journal of tropical medicine and hygiene. 2012;87:385–93. doi: 10.4269/ajtmh.2012.11-0633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HAVER J, CARUSO BA, ELLIS A, SAHIN M, VILLASENOR JM, ANDES KL, FREEMAN MC. WASH in Schools Empowers Girls’ Education in Masbate Province and Metro Manila, Philippines An Assessment of Menstrual Hygiene Management in Schools. New York: United Nation’s Childrens Fund; 2013. [Google Scholar]
- HAYES RJ, BENNETT S. Simple sample size calculation for cluster-randomized trials. International journal of epidemiology. 1999;28:319–26. doi: 10.1093/ije/28.2.319. [DOI] [PubMed] [Google Scholar]
- HUTTON G, HALLER L. Evaluation of the costs and benefits of water and sanitation improvements at the global level. Water, Sanitation, and Health, Protection of the Human Environment, World Health Organization; 2004. [Google Scholar]
- STATISTICS, K. N. B. O., editor. KNBS. Kenya 2009 Population and Housing Census Highlights. 2010. [Google Scholar]
- KNBS. Kenya National Bureau of Statistics: Population and Housing Census- Population Attending School at Different Levels [Online] 2011a Available: http://www.knbs.or.ke/censuseducation.php [Accessed 4 October 2012]
- KNBS. Kenya National Bureau of Statistics: Population and Housing Census- Population Numbers by Province [Online] 2011b Available: http://www.knbs.or.ke/censuspopulation.php [Accessed 4 October 2012]
- KOOPMAN JS. Diarrhea and school toilet hygiene in Cali, Colombia. Am J Epidemiol. 1978;107:412–20. doi: 10.1093/oxfordjournals.aje.a112559. [DOI] [PubMed] [Google Scholar]
- LE TT, LUU NH, RHEINLANDER T, DALSGAARD A, KONRADSEN F. Sanitation behavior among schoolchildren in a multi-ethnic area of Northern rural Vietnam. BMC public health. 2012;12:140. doi: 10.1186/1471-2458-12-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LONG J, CARUSO BA, LOPEZ D, VANCRAEYNEST K, SAHIN M, ANDES KL, FREEMAN MC. WASH in Schools Empowers Girls’ Education in Rural Cochabamba, Bolivia: An Assessment of Menstrual Hygiene Management in Schools. New York: United Nations Children’s Fund; 2013. [Google Scholar]
- LUBY SP, KADIR MA, YUSHUF SHARKER MA, YEASMIN F, UNICOMB L, SIRAJUL ISLAM M. A community-randomised controlled trial promoting waterless hand sanitizer and handwashing with soap, Dhaka, Bangladesh. Tropical medicine & international health: TM & IH. 2010;15:1508–16. doi: 10.1111/j.1365-3156.2010.02648.x. [DOI] [PubMed] [Google Scholar]
- MAJRA JP, GUR A. School environment and sanitation in rural India. Journal of global infectious diseases. 2010;2:109–11. doi: 10.4103/0974-777X.62882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MCMAHON S, CARUSO BA, OBURE A, OKUMU F, RHEINGANS RD. Anal cleansing practices and faecal contamination: a preliminary investigation of behaviours and conditions in schools in rural Nyanza Province, Kenya. Tropical medicine & international health: TM & IH. 2011a;16:1536–40. doi: 10.1111/j.1365-3156.2011.02879.x. [DOI] [PubMed] [Google Scholar]
- MCMAHON SA, WINCH PJ, CARUSO BA, OBURE AF, OGUTU EA, OCHARI IA, RHEINGANS RD. ‘The girl with her period is the one to hang her head’ Reflections on menstrual management among schoolgirls in rural Kenya. BMC Int Health Hum Rights. 2011b;11:7. doi: 10.1186/1472-698X-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MOPHS. National School Health Guidelines. Nairobi: Ministry of Public Health and Sanitation & Ministry of Education, Government of Kenya; 2009. [Google Scholar]
- O’REILLY CE, FREEMAN MC, RAVANI M, MIGELE J, MWAKI A, AYALO M, OMBEKI S, HOEKSTRA RM, QUICK R. The impact of a school-based safe water and hygiene programme on knowledge and practices of students and their parents: Nyanza Province, western Kenya, 2006. Epidemiol Infect. 2008;136:80–91. doi: 10.1017/S0950268807008060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PICKERING AJ, JULIAN TR, MARKS SJ, MATTIOLI MC, BOEHM AB, SCHWAB KJ, DAVIS J. Fecal contamination and diarrheal pathogens on surfaces and in soils among Tanzanian households with and without improved sanitation. Environmental science & technology. 2012;46:5736–5743. doi: 10.1021/es300022c. [DOI] [PubMed] [Google Scholar]
- PORTNEY L, WATKINS M. Foundations of Clinical Research: Applications to Practice. Prentice Hall; 1999. [Google Scholar]
- RABIE T, CURTIS V. Handwashing and risk of respiratory infections: a quantitative systematic review. Tropical medicine & international health. 2006;11:258–267. doi: 10.1111/j.1365-3156.2006.01568.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RAJARATNAM G, PATEL M, PARRY JV, PERRY KR, PALMER SR. An outbreak of hepatitis A: school toilets as a source of transmission. J Public Health Med. 1992;14:72–7. [PubMed] [Google Scholar]
- SABOORI S, GREENE LE, MOE CL, FREEMAN MC, CARUSO BA, AKOKO D, RHEINGANS RD. Impact of Regular Soap Provision to Primary Schools on Hand Washing and E. coli Hand Contamination among Pupils in Nyanza Province, Kenya: A Cluster-Randomized Trial. The American journal of tropical medicine and hygiene. 2013;89:698. doi: 10.4269/ajtmh.12-0387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SABOORI S, MWAKI A, RHEINGANS R. Research Note: Is soapy water a viable solution for handwashing in schools? Waterlines. 2010;29:329–336. [Google Scholar]
- SINCLAIR RG, GERBA CP. Microbial contamination in kitchens and bathrooms of rural Cambodian village households. Letters in applied microbiology. 2011;52:144–9. doi: 10.1111/j.1472-765X.2010.02978.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SOMMER M, ACKATIA-ARMAH N, CONNOLLY S, SMILES D. A comparison of the menstruation and education experiences of girls in Tanzania, Ghana, Cambodia and Ethiopia. Compare: A Journal of Comparative and International Education. 2014:1–21. [Google Scholar]
- TALAAT M, AFIFI S, DUEGER E, EL-ASHRY N, MARFIN A, KANDEEL A, MOHAREB E, EL-SAYED N. Effects of hand hygiene campaigns on incidence of laboratory-confirmed influenza and absenteeism in schoolchildren, Cairo, Egypt. Emerg Infect Dis. 2011;17:619–25. doi: 10.3201/eid1704.101353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- THOMAS ME, TILLETT HE. Sonne dysentery in day schools and nurseries: an eighteen-year study in Edmonton. The Journal of hygiene. 1973;71:593–602. doi: 10.1017/s0022172400046593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF, editor. UNICEF. Raising Even More Clean Hands: Advancing Health, Learning and Equity through WASH in Schools. 2012. [Google Scholar]
- ZIEGELBAUER K, SPEICH B, MAUSEZAHL D, BOS R, KEISER J, UTZINGER J. Effect of sanitation on soil-transmitted helminth infection: systematic review and meta-analysis. PLoS Med. 2012;9:e1001162. doi: 10.1371/journal.pmed.1001162. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


