1. Introduction
Charcot–Marie–Tooth disease (CMT) is classified into either dysmyelinating or axonal type. The former exhibits slowed conduction velocities on nerve conduction studies (NCS) and abnormally developed myelin on nerve biopsies. In contrast, the latter shows normal or minimally slowed conduction velocities with axonal loss in its neuropathology. CMT can be transmitted in autosomal dominant, recessive or X-linked mode [3].
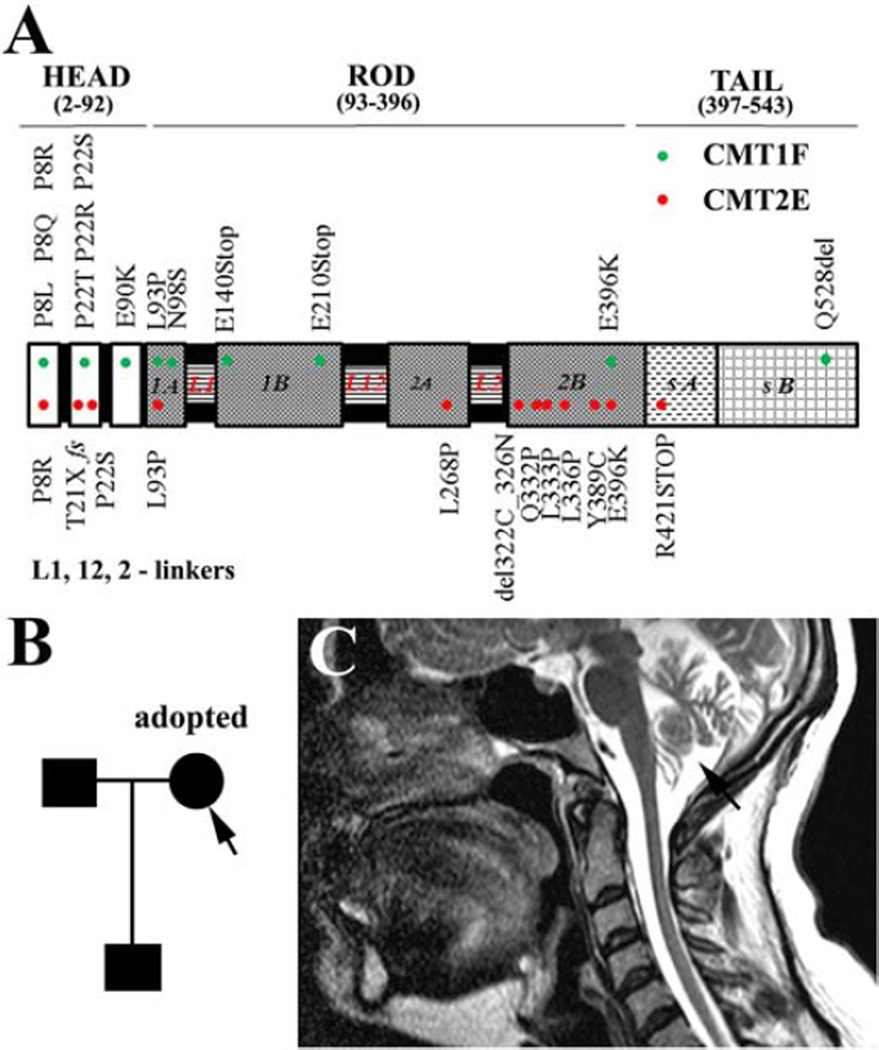
The neurofilament light polypeptide (NEFL) gene is located on 8p21. It encodes a neuronal protein that serves as a key element in the formation of neurofilaments and, therefore, affects axonal transport and nerve conduction velocity [4,6]. At least 20 missense mutations and a few truncation or frame-shift mutations in NEFL have been reported to cause either axonal CMT2E or dysmyelinating CMT1F (Fig. 1, upper panel). Patients may develop sensory loss and muscle atrophy/weakness in limbs.
Fig. 1.
A: This diagram lists all published mutations in the NEFL gene and their associated phenotypes; B: The pedigree shows the adopted proband, unaffected father and her affected son. C: MRI of the proband shows the atrophic cerebellum (arrow). In addition, there was diffuse atrophy in the entire spinal cord, but only the cervical cord was included in the image.
Of these missense mutations, N98S mutation was only briefly described in de novo subjects. Thus, it is unknown if the mutation is heritable. Here, we report a CMT family with a dominantly inherited N98S mutation.
2. Case report
The proband (a 40-year-oldwoman)was an adopted child (Fig. 1B). She did not start walking until the age of 3 years and even then had a “drunken” gait and frequent falls. By the age of 8 years, she developed foot deformities and underwent bilateral Achilles tendon release. Throughout adolescence and early adulthood, she used ankle-foot orthoses to walk and experienced a continued progression of unsteady gait and falls. She acquired a scooter 4–5 years ago. Since 2 years ago, she has noted the inability to transfer herself out of the scooter.
Her neurological examination showed normal cognitive functions. She had a right eye esotropia and hearing loss. She had flat feet with hammer toes. Her muscle strength was 0–2 on MRC scale for distal muscles and 3–4 for proximal muscles. There was no truncal ataxia. Severe limb weakness made the examination of coordination difficult. Her sensory functions were diminished to all modalities in her limbs. Tendon reflexes were absent. Her CMT Neuropathy score (CMTNS) was 31. The CMTNS is a validated measurement of impairment in patients with CMT [5] with a maximum of 36. It is classified as: the presence of mild (1–10), intermediate (11–20) or severe disability (≥21). In addition, she had a brain MRI that revealed severe cerebellar and spinal cord atrophy (Fig. 1C).
The proband's son (8 years old) is her only biological child. He did not walk until 19 months. Frequent falls were noted throughout childhood and he struggled with manipulating buttons and shoelaces. He was also found to have mild, bilateral sensorineural hearing loss. Academic performance was reportedly normal. He had bilateral Achilles tendon release surgery at 7 years of age.
Neurological examination showed normal cognitive functions. He had high-arched feet. His muscle strength was 4/4 in bilateral ankle dorsal flexors but 5/5 in the remaining muscles. Sensation to all modalities was reduced in his feet. Tendon reflexes were absent.
NCS in the proband showed that all sensory nerves were nonresponsive. CMAP was not recordable in distal muscles but was recordable in forearm muscles. The amplitude (0.5 mV) and conduction velocity (31 m/s) were reduced in the median nerve. CMAP was absent for the ulnar nerve. For the son, the sensory nerves were also nonresponsive. The distal latency, amplitude and conduction velocity in the son's median, ulnar and peroneal nerves were 6.3 ms, 3.1 mV, 25 m/s; 4.0 ms, 6.0 mV, 31m/s and 5.9ms, 3.0mV, 32 m/s, respectively.
Their DNA tests were done by Medical Neurogenetics, Inc. in Atlanta. It demonstrated a N98S missense mutation of NEFL in the proband and the son. This study was approved by the Vanderbilt Institutional Review Board. The consent was obtained from the proband.
3. Discussion and conclusion
N98S mutation has been reported in four patients. All of them were de novo mutations with no detailed phenotypic description. It has been speculated that this mutation is embryonically lethal. The family in this report demonstrates that the N98S mutation is still heritable via an autosomal dominant mode.
This notion is further supported by another family that was reported shortly after our manuscript submission. A 6-year-old boy inherited a heterozygous N98S mutation from his affected mother [2]. However, in contrast to our study, the boy reported by Berciano et al. was mildly affected and the atrophy in the proband only affected cerebellum but not spinal cord. The two families together do not show obvious anticipation. In addition, sequencing of spinocerebellar ataxia (SCA) genes showed no mutation in the Berciano-reported family.
NEFL encodes the neurofilament light polypeptide with 543 amino acids. It provides structural support for the axon and regulates the axon caliber and transport [6]. The N98S mutation promotes protein aggregates in the cytoplasm. These aggregates appear to prevent NEFL from transporting to axons [1,4,8]. Indeed, decrease of neurofilament staining in axons was observed in patients with E396K mutation of NEFL that also resulted in cytoplasmic protein aggregates [7]. Depletion of neurofilaments in axons would result in small caliber of axons, hence, slowed conduction velocity.
A knockin mouse model of N98S has recently been produced [1]. In addition to the expected pathology, such as protein aggregates, in the peripheral nerves and spinal neurons, cerebellar neurons were predominantly affected in the central nervous system. Thus, the concordant findings between human and mouse support the utility of the knockin mouse.
Acknowledgments
This research is supported by grants from NINDS (R01NS066927 to J.L.) and the National Center for Advancing Translational Sciences (UL1TR000445). Yi Yang is an international exchange student supported by the International Program for PhD Candidates of Sun Yat-Sen University.
Contributor Information
Yi Yang, Department of Microsurgery and Orthopedic Trauma, the First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China.
Li-Qiang Gu, Department of Microsurgery and Orthopedic Trauma, the First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China.
William B. Burnette, Department of Neurology, Vanderbilt Brain Institute and Center for Human Genetics Research, Vanderbilt University Medical Center, Nashville, TN, USA
Jun Li, Department of Neurology, Vanderbilt Brain Institute and Center for Human Genetics Research, Vanderbilt University Medical Center, Nashville, TN, USA; Tennessee Valley Healthcare System – Nashville Campus, TN, USA.
References
- 1.Adebola AA, Di CT, He CZ, Salvatierra LA, Zhao J, Brown K, Lin CS, Worman HJ, Liem RK. Neurofilament light polypeptide gene N98S mutation in mice leads to neurofilament network abnormalities and a Charcot-Marie-Tooth Type 2E phenotype. Hum. Mol. Genet. 2015;24:2163–2174. doi: 10.1093/hmg/ddu736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berciano J, Peeters K, Garcia A, Lopez-Alburquerque T, Gallardo E, Hernandez-Fabian A, Pelayo-Negro AL, De VE, Infante J, Jordanova A. NEFL N98S mutation: another cause of dominant intermediate Charcot-Marie-Tooth disease with heterogeneous early-onset phenotype. J. Neurol. 2016;263:361–369. doi: 10.1007/s00415-015-7985-z. [DOI] [PubMed] [Google Scholar]
- 3.Li J. Inherited neuropathies. Semin. Neurol. 2012;32:204–214. doi: 10.1055/s-0032-1329198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li J. Molecular regulators of nerve conduction — lessons from inherited neuropathies and rodent genetic models. Exp. Neurol. 2015 doi: 10.1016/j.expneurol.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy SM, Herrmann DN, McDermott MP, Scherer SS, Shy ME, Reilly MM, Pareyson D. Reliability of the CMT neuropathy score (second version) in Charcot-Marie-Tooth disease. J. Peripher. Nerv. Syst. 2011;16:191–198. doi: 10.1111/j.1529-8027.2011.00350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perrot R, Lonchampt P, Peterson AC, Eyer J. Axonal neurofilaments control multiple fiber properties but do not influence structure or spacing of nodes of Ranvier. J. Neurosci. 2007;27:9573–9584. doi: 10.1523/JNEUROSCI.1224-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pisciotta C, Bai Y, Brennan KM, Wu X, Grider T, Feely S, Wang S, Moore S, Siskind C, Gonzalez M, Zuchner S, Shy ME. Reduced neurofilament expression in cutaneous nerve fibers of patients with CMT2E. Neurology. 2015;85:228–234. doi: 10.1212/WNL.0000000000001773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yum SW, Zhang J, Mo K, Li J, Scherer SS. A novel recessive Nefl mutation causes a severe, early-onset axonal neuropathy. Ann. Neurol. 2009;66:759–770. doi: 10.1002/ana.21728. [DOI] [PMC free article] [PubMed] [Google Scholar]