In 1911 Paton and Holmes1 published a seminal paper on the pathology of papilledema which established that papilledema was a consequence of intracranial hypertension and not, as previously thought, an inflammatory process.2 Their study also included several incidental observations about folds in papilledema, now occasionally referred to as “Patons folds”. In their words:
“ as the disc swells lateralwards, it displaces the retina...throwing it into a series of folds which run concentric with the edge of the disc. This lateral bulging is due to the distension of the most peripheral nerve fibers ..”(1a).1
Their histopathological photographs showed peripapillary intra-retinal folds that spared the retinal nerve fiber layer (RNFL) and the choroid. They correlated the histopathology to ophthalmoscopy:
“ ..the greyish-white lines that run concentric with the outer edge of the disc are obviously due to the retinal folds, their presence being occasionally accentuated by hemorrhages lying within them”. 1, 3
Their assertion that the “greyish-white lines” (in the fundus) correspond to the intra-retinal folds (histopathologically) appears to be inconsistent with Paton's fundus drawings 3 that seem to show folds in the RNFL.
By correlating SD-OCT images [Zeiss-Meditech, Cirrus-5000] with fundus photographs over time in a signature case, and confirming our observations with the dataset from the Idiopathic Intracranial Hypertension Treatment Trail (IIHTT) OCT Sub-study4, we found that the intra-retinal folds (seen histopathologically) and the fundus folds both described by Paton are actually quite different. Each has its own unique OCT and photographic characteristics, some of which have not been previously described as such.
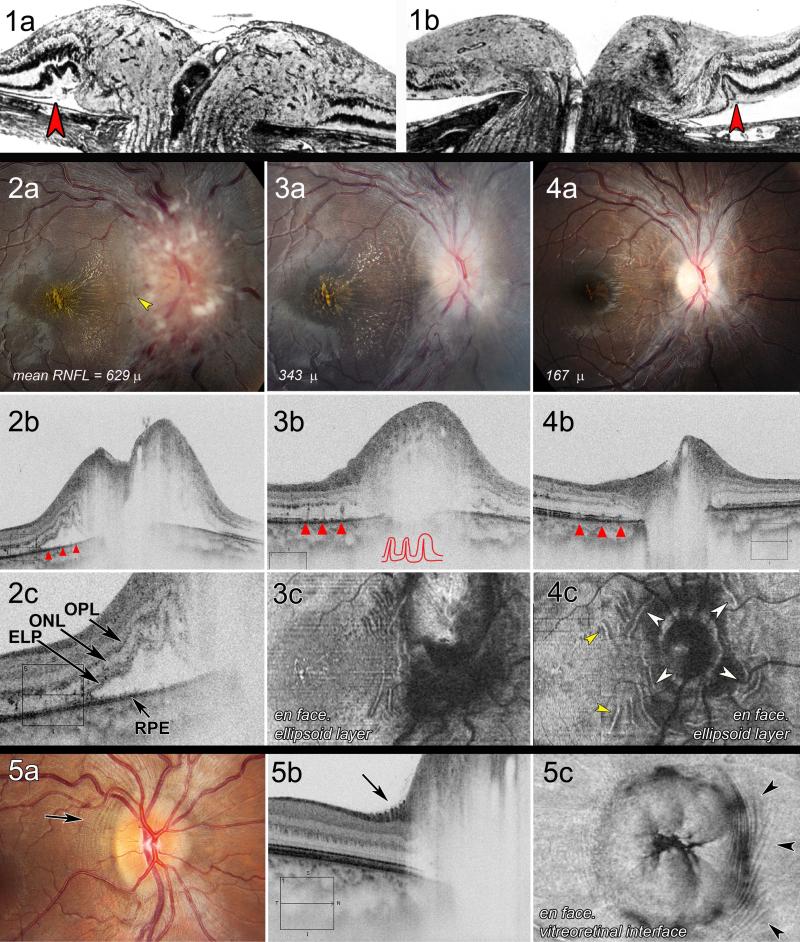
Figure 1 (2a) is a fundus photo from our signature case showing Grade IV papilledema and a macular star. The axial raster (2bc), shows subretinal fluid temporal to the disc with sinusoidal folds in the outer plexiform(OPL), outer nuclear(ONL) and ellipsoid(ELP) layers of the retina sparing the RNFL and choroid. The appearance is remarkably similar to Paton's photomicrograph (1a). The fundus photo shows several subtle “greyish lines” temporally (2a, yellow arrow) that correspond to the outer-retinal folds seen on the OCT (2bc).
Figure 1.
See text for descriptions and abbreviations. 1ab: histopathology from Paton L and Holmes G, 19111; with permission, Oxford University Press. 2a-c: photos and OCT at baseline; 3a-c: at two weeks on treatment; 4a-c: at 6 weeks on treatment. 5a-c: examples of peripapillary wrinkles by photo, raster and en face SD-OCT
Figure 1 (3a-c), from the same patient, taken 2 weeks later while on acetazolamide, shows that the subretinal fluid has resolved and papilledema has improved to Grade III. There are curvilinear greyish lines around the disc that are nicely imaged with the en face (3c) modality. The outer retinal folds (ORF) have been replaced by three vertical lines perpendicular to the RPE layer (3b, red arrowheads). These are deeply furrowed, self-contacting creases in the outer retina (3b, traced in red) that correspond to the curved peripapillary lines seen en face and photographically in 3ac. A histopathological example of a crease can be seen in one of Paton's figures (1b, red arrowhead).
Figure 1 (4a-c), at 6 weeks, shows Grade 1 papilledema surrounded by a series concentric lines (4ac) that correspond to the creases shown on the axial raster (4b, red arrowheads). As the creases unfold, they diminish in size. There are two sets of lines, one group surrounding the disc (4c, white arrowheads), and the other convex to the macula (4c, yellow arrowheads); a pattern that appears to be a consequence of two opposing sources of compression, one from macular edema towards the optic disc and the other radially expanding from the optic nerve head.
We recently surveyed the patterns of retinal and choroidal folds from the study eye of 125 patients in the IIHTT OCT sub-study.5 The most frequent types of folds were peripapillary wrinkles (PPW, 46%), retinal folds (47%) and choroidal folds (10%). We observed ORF on the OCT, but they were difficult to image because the overlying edema shadowed the peripapillary retina.
The signature case was exceptional because the ORF were clearly imaged over time (figures 2-4) and readily distinguished from peripapillary wrinkles (PPW, illustrated in figure 1 [5a-c]). Peripapillary ORF are widely spaced (300-450 μm) and usually associated with subretinal fluid. They may form creases that correspond to the “high water marks” sometimes seen ophthalmoscopically as papilledema resolves(4a). In constrast, PPW are confined to the RNFL on the optic nerve head or juxtapapillary retina, almost invariably located temporally, and usually concentric to the optic disc (5ab). Occasionally they may also spiral away from the disc and extend into the macula as retinal folds (5c). The peak-to-peak distance or spatial wavelength is about 100 μm.5
Our case prompted us to re-examine the IHTT-OCT sub-study 5 data for ORF and creases. We identified ORF or creases in 25/125(20%) of the study eyes at baseline, 9% at three months and 4% at six months. Because of shadowing, it's likely that the frequencies cited underestimates the actual number. Like PPWs, ORF are associated with a higher mean Frisén grade (p=0.035), RNFL thickness (p<0.001) and optic disc volume (p=0.006) but were not significantly associated with anterior deformation of the peripapillary eye wall, vision loss, intracranial pressure or refractive error. That these folds are associated with the severity of papilledema is consistent with Paton's demonstration of distended prelaminar axons compressing the juxtapapillary retina.2
The description of folds by Paton and Holmes has proven to be a helpful sign of pathological optic disc edema, even today. What seemed to be an “obvious” clinical-pathologic correlation at the time, now with OCT imaging shows that papilledema is associated with several distinctive types of folds i.e. PPW, inner retinal folds, choroidal folds5 and ORF/creases. Folds and wrinkles of papilledema are structural manifestations of stress and strain induced by the intracranial pressure on the optic nerve head and load bearing structures (sclera, lamina cribrosa) . The development of a specific type fold in each case is the product of a complex interaction between structural geometry, tissue material properties and loading force conditions.5
Supplementary Material
Acknowledgments
This report is supported in part by U10 EY017281-01A1, U10 EY017387-01A1, 3U10EY017281-01A1S1
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Trial registration: clinicaltrials.gov identifier: NCT01003639
Financial Disclosures: none
Bibliography
- 1.Paton L, Holmes G. The pathology of papilloedema: a histological study of sixty eyes. Brain. 1911;33:389–432. [Google Scholar]
- 2.Lepore FE. Toward a definition of papilledema: a historical review, 1851-1911. Surg Neurol. 1982;17:178–80. doi: 10.1016/0090-3019(82)90270-1. [DOI] [PubMed] [Google Scholar]
- 3.Paton L. Papilledema and optic neuritis: A retrospect. Archives of Ophthalmology. 1936;15:1–20. [Google Scholar]
- 4.OCT Substudy Committee for the NORDIC Idiopathic Intracranial Hypertension Study Group Baseline OCT measurements in the idiopathic intracranial hypertension treatment trial, part I: quality control, comparisons, and variability. Invest Ophthalmol Vis Sci. 2014;55:8180–8. doi: 10.1167/iovs.14-14960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sibony PA, Kupersmith MJ, Feldon SE, et al. Retinal and Choroidal Folds in Papilledema. Invest Ophthalmol Vis Sci. 2015;56:5670–80. doi: 10.1167/iovs.15-17459. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.