Abstract
We attempted to replicate and add to our prior study of attempts to stop or reduce cannabis use among daily cannabis users trying to change on their own, by observing a larger sample and adding further clinically-relevant outcomes. Daily users (n = 193) who intended to stop or reduce sometime in the next 3 months called an Interactive Voice Response system each morning for 3 months to report on cannabis use, attempts to stop or reduce, withdrawal symptoms, etc., on the prior day. This study replicated our prior findings that a) cannabis users trying to change make many, and often rapid, transitions among use as usual, reduction and abstinence; b) reduction attempts are more common than abstinence attempts; c) quit and reduction attempts are short-lived and few participants achieve long-term abstinence; d) alcohol and drug use are not greater on abstinence days; and e) few users seek treatment. Novel findings included f) a greater number of days of abstinence or intentional reduction predicted a greater decline in cannabis dependence; g) most users do not prepare before their quit attempt; h) coping outcomes during abstinence predict increased duration of abstinence; i) tobacco use is less common on days of abstinence; and j) withdrawal symptoms occur even with short quit attempts. Replication tests in more generalizable samples and of longer duration are indicated. Further natural history studies are likely to provide information to help improve the content of psychological treatments for cannabis use.
Keywords: cannabis, cessation, marijuana, natural history, substance use disorder
Introduction
Cannabis is the most widely used illegal drug in the US (www.samhsa.gov/data/NSDUH). Although current treatments for cannabis dependence are efficacious, they are less than optimal (Budney, Vandrey, & Stanger, 2010). One likely reason for this is the lack of an adequate description of the process of successful and unsuccessful attempts to stop or reduce cannabis use (Klingemann et al., 2001). Although some studies have described attempts to quit cannabis among treatment seekers, as with other drugs, the large majority of attempts to change cannabis use do not involve treatment (Blanco et al., 2015) (Klingemann et al., 2001). Previous natural history studies have described how cannabis use changes over a lifetime (Kandel & Raveis, 1989; Swift, Hall, & Copeland, 2000; VonSydow et al., 2001; Aitken, DeSantis, Harford, & FeCaces, 2000; Ellingstad, Sobell, Sobell, Eickleberry, & Golden, 2006). Although informative, the large majority of participants in these studies were young, infrequent users, and these studies relied on retrospective recall over 3 – 6 month intervals.
Daily users of cannabis account for most of the harm, dependence, and treatment-seeking associated with cannabis use (Gordon A.J., Conley J.W, & Gordon J.M, 2013). Currently, there are about 5 million daily cannabis users in the US (www.samhsa.gov/nsduh). The prevalence of cannabis dependence (Stinson, Ruan, Pickering, & Grant, 2006; Compton, Grant, Colliver, Glantz, & Stinson, 2004) and the number of users seeking treatment (Office of Applied Statistics, 2007) have increased dramatically in recent years, and may increase even more with greater legalization of cannabis (Chu, 2014) and enhanced potency of cannabis (Downey & Verster, 2014) .
Prior studies of cannabis users trying to stop on their own have reported several findings. For example, the major reasons for attempting to stop were internal reasons (Ellingstad et al., 2006) and included self-image, self-control, health concerns, and self-efficacy (Chauchard, Levin, Copersino, Heishman, & Gorelick, 2013; Copersino et al., 2006b) as well as interpersonal relationship, legal, social acceptability concerns (Chauchard et al., 2013). Also, positive expectancies about cannabis use (Tyler Boden, McKay, Long, & Bonn-Miller, 2013), low physical activity (Irons, Babson, Bergeria, & Bonn-Miller, 2014), post-traumatic stress disorder(Bonn-Miller et al., 2015), and poor sleep (Babson, Tyler Boden, & Bonn-Miller, 2013; Babson, Tyler Boden, Harris, Stickle, & Bonn-Miller, 2013) predicted worse outcomes but delay discounting does not (Heinz, Peters, Boden, & Bonn-Miller, 2013). Rates of remission among dependent cannabis users (almost all of whom were self-quitters) was greater than for those with other drug dependencies (Calabria et al., 2010). The major strategies used for self-quitting were changing the environment, seeking help and seeking social support (Budney, Radonovich, Higgins, & Wong, 1998). Finally, abstinence increased withdrawal symptoms and increased use of other drugs (Copersino et al., 2006a; Copersino et al., 2006b; Boyd et al., 2005). Almost all of these studies relied on retrospective recall, sometimes of events that occur several years earlier. Although such studies are useful initial tests, retrospective recall of drug use behaviors and reasons for stopping drug use are often inaccurate due to memory and demand biases (Shiffman et al., 1997; Hughes, Naud, Fingar, Callas, & Solomon, 2015) and thus prospective tests are needed.
Only two prospective studies of self-quitting among heavy cannabis users have been published. One study focused on post-attempt behaviors and found that withdrawal symptoms, negative affect, and peer use were associated with relapse (Buckner, Zvolensky, & Ecker, 2013). In our earlier study (Hughes, Peters, Callas, Budney, & Livingston, 2008), 19 daily cannabis users who planned to quit or reduce in the next month reported cannabis use via daily phone calls over a one-month period. Our major finding was that users made multiple, often rapid, transitions among use as usual, reduction and abstinence.
The current study was a replication test of our prior study with a larger sample, a longer duration of monitoring, and inclusion of other clinically-relevant outcomes. These included: a) incidence and duration of attempts to stop or reduce cannabis; b) goals of attempts to change; c) amount of planning and coping during quit attempts; d) incidence of treatment-seeking; e) baseline predictors of attempts to change; f) ability of reduction to predict later quit attempts; g) impact of abstinence or reduction on cannabis problems or dependence; and h) occurrence of withdrawal symptoms and changes in other drug use during cannabis abstinence. Determining these outcomes is likely to be of help in developing treatments. For example, if most heavy users want to reduce rather than quit, and if reducing leads to future abstinence or to reduced cannabis problems, this would suggest reduction should be an acceptable goal and treatments focused on reduction should be developed. Also, if abstinence from cannabis increases alcohol or tobacco use, treatments will need to include interventions to prevent this.
Methods
Study Design
We recruited daily cannabis users who planned to quit or reduce to join a 6-month prospective, non-treatment study. Participation was via phone, mail, and internet. Participants initially completed a survey on their “usual” use pattern and then called an Interactive Voice Response (IVR) system each morning for 3 months to report the prior day’s cannabis use, as well as intentional and non-intentional attempts to reduce or abstain from cannabis, withdrawal symptoms, and alcohol/tobacco/drug use. Participants also completed a 6-month follow-up survey to determine long term abstinence rates.
Prior analysis of this study described cannabis use on days that participants were not trying to change (Hughes JR et al., 2014a) and which cues prospectively predicted attempts to stop or reduce cannabis use (Hughes et al., 2015). All participants provided verbal consent. The University of Vermont Committees on the Human Research approved the study. We registered the study at www.clinicaltrials.com (NCT01039415).
Inclusion Criteria and Recruitment
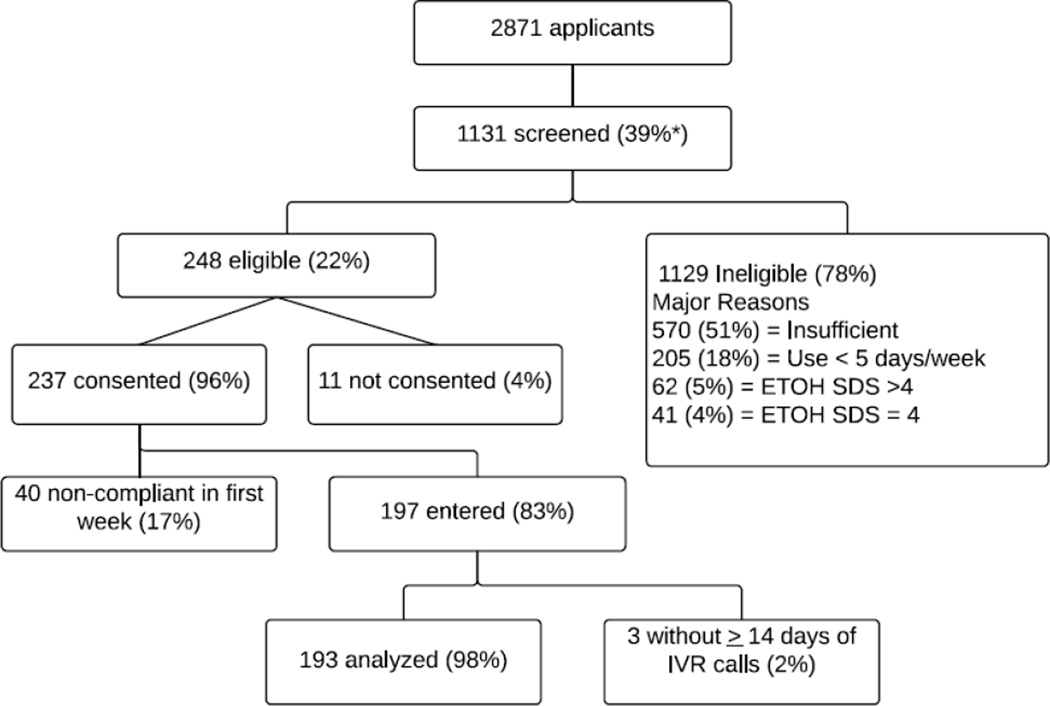
Participant flow is outlined in Figure 1. Major inclusion criteria were a) ≥ 18 years old; b) using cannabis on at least 5 days/week; c) scored < 3 on the Severity of Dependence Scales (SDS) (Swift, Copeland, & Hall, 1998) for dependence on alcohol and non-cannabis illicit drugs; d) stated probably or definitely intended to reduce or stop cannabis use at some point in the next 3 months(to increase the likelihood of observing quit and reduction attempts); e) had no pending legal actions; and f) were fluent in English. We excluded participants who did not reliably complete IVR calls in the first week, and we only used data from participants who provided ≥ 14 days of IVR data. We excluded one participant who entered residential treatment for cannabis during the study. The resultant 193 participants were recruited from throughout the US between 1/1/2010 and 3/1/2012 by notices on on-line bulletin boards (e.g., www.craigslist.org) (30% of those enrolled), internet ads (23%), participant referrals (16%), flyers (8%), bus ads (3%), and newspaper ads (2%). We based our target sample size of 200 to achieve a sufficient accuracy of the incidence rates of various events. We chose a sample of 200 because it would produce a 95% confidence interval of 7% or less, depending on the incidence rate (Fleiss, 2003).
Figure 1.
Participant Flow Chart. All percents are of those in the preceding box.
Sample Characteristics
The mean (sd) age of participants was 32 (11). Half the participants were men (53%), and half were employed (50%). Many were minorities (41%). Few were married (15%), and most had more than a high school education (72%). At study entry, participants stated they usually used cannabis on a median of 6 days/week, and on the days they used, averaged a median of 4 (3, 5) times/day. Participants typically used cannabis via water-pipes (60%) joints (52%), blunts (49%), bongs (36%), or vaporizers (7%). Use of synthetic cannabis substitutes (e.g. K2 or spice) was rare (4%). Our prior publication provides more details about how much of use was from joints, blunts, etc. (Hughes JR et al., 2014a).
The median age of onset of regular cannabis use was 16. Most (75%) met criteria for DSM- 5 Cannabis Use Disorder using a self-report version of the DSM checklist (Hudziak et al., 1993). The mean rating of addiction to cannabis was 6.5 (sd = 2.7) on a 0–10 scale (0 = not at all addicted, 10 = very addicted) (Hughes, Keely, Fagerstrom, & Callas, 2005). The median number of problems on the Marijuana Problems Scale (Stephens, Roffman, & Curtin, 2000) was 7 (3,13) out of a possible 18 problems. Upon study entry, half (51%) of participants were current cigarette smokers (39% daily and 13% nondaily smokers); a quarter (23%) were former smokers, and a quarter (26%) were never smokers. Few (16%) met criteria for problem or binge drinking (http://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking) in the last 3 months. Few (15%) had used a non-cannabis illegal drug in the last 3 months. For comparisons, we obtained mean demographic and cannabis use descriptors of daily cannabis users in a) the National Survey of Drug Use and Health (www.nsduhweb.rti.org), b) treatment seekers from the Treatment Episodes Data Set (www.dasis.samhsa.gov), c) a study of users ambivalent about quitting (Stephens et al., 2004), and d) research volunteers from the largest prior randomized controlled trial on cannabis treatment of users committed to quitting (Marijuana Treatment Project Research Group, 2004). Our sample appears more similar to the population-based samples and ambivalent users than to treatment seekers.
Procedures
Participants completed a baseline survey of demographics, and history of cannabis and other drug use either via the internet or paper form. They then called the IVR system by phone each morning (to minimize intoxication effects) to report cannabis use for the prior day. The IVR has participants respond to phone questions by using the phone keypad (Corkrey & Parkinson, 2002). IVR has many of the assets of computer-assisted telephone interviewing; e.g., automatic skips, branching options, prohibition of illogical responses and outliers, standardized questioning, and direct data entry. Drug use outcomes are more validly reported in IVR compared to phone interviews, computer assessments, written questionnaires or in-person interviews (Aquilino, 1992; Kobak et al., 1997). Daily reporting via IVR appears to produce little reactivity (Hufford, Shields, Shiffman, Paty, & Balabanis, 2002) (Hughes et al., 2013; Helzer, Badger, Rose, Mongeon, & Searles, 2002). Questions in the IVR were similar to those we developed in qualitative studies. Although no formal psychometric testing of these measures was done, we did find these measures produced sensitive and reliable results in a prior study of cannabis self-quitters(Hughes JR et al., 2014b; Hughes JR et al., 2014c). To quantify use, the IVR asked about times of use where a time of use could be long or short but had to be separated from the previous time of use by at least one hour. We chose “times” of use because the largest studies of daily cannabis users (e.g., the Marijuana Treatment Project) (Stephens, Babor, Kadden, & Miller, 2002) suggests this is a valid measure.
The IVR first asked whether participants were abstinent or had reduced. Days of abstinence could represent a successful quit or reduction attempt (e.g. reducing number of days of use), or an unintentional abstinence (e.g. due to unavailability of cannabis). Similarly days of reduction could represent a failed quit attempt, gradual reduction prior to quitting), or a reduction attempt (e.g., reducing times of use/day), or unintentional reduction. To clarify this, we defined four change states. A quit attempt was a day of abstinence in which the participant stated he/she was trying “to stop and never use again, “or to stop and not use for as long as possible.” Intentional reduction was a day or more in which participants stated they “used less than usual” and were “trying to reduce or stop.” In contrast, an unintentional abstinence or an unintentional reduction episode was a day of abstinence or reduction that was due to “preparing for a drug test,” “no money,” “no marijuana was available,” “around people who object to my use of marijuana” or “some other reason.”
The IVR also asked about the number of standard alcoholic drinks consumed, number of tobacco cigarettes smoked, and use of non-cannabis illegal drug (yes/no). Binge drinking was defined as ≥ 5 drinks in a day for men and ≥ 4 drinks for women (http://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking). The IVR also asked users to rate their level of six symptoms consistent with cannabis withdrawal: anger, craving, hunger, insomnia, nervousness and sadness from 0 = not at all to 5= a lot. These symptoms consistently increase across studies of abstinence among self-quitters(Del Boca & Darkes, 2003). The IVR asked participant to rate intoxication on a scale previously shown to be related to amount of cannabis use(Hughes JR et al., 2014a) and asked ““how high you were” from 0 = not at all to 6 = “very high.” Alcohol, tobacco and illegal drug use, and withdrawal symptoms, were asked on both days of use and days of abstinence. If the participant made a quit attempt, the IVR asked whether they told others they were trying to reduce or quit, asked others for advice on quitting/reducing, discarded cannabis paraphernalia, avoided being around cannabis users, or talked to a counselor. In case participants missed a day or two of reporting, a weekly IVR asked about days of abstinence and attempts to stop using that did not last a day during the last week.
More lengthy scales were completed via paper or a website at baseline and 3 months (end of IVR period). They included the Severity of Dependence Scale (SDS) for Cannabis, the DSM Checklist for Cannabis Use Disorder, the Marijuana Problems Scale and a Motivation Ladder. The SDS has high internal, test-retest validity, and criterion validity as well as empirical cut-points (Pointek, Kraus, & Klempova, 2008) (Swift et al., 1998). The DSM Checklist determined if participants endorsed ≥ 2 of the 11 DSM-5 Substance Use Disorder criteria. Similar versions of the Checklist have adequate reliability and validity (Hudziak et al., 1993). The Marijuana Problems Scale evaluated negative social, occupational, physical, and personal consequences associated with cannabis use in the past 90 days (Stephens et al., 2000) and has excellent reliability (Buckner, Keough, & Schmidt, 2007). The Motivation Ladder has scores from 0 = do not intend to quit or reduce marijuana in the next 3 months to 10 = definitely intend to quit in the next 3 months. Although this ladder has not been tested with cannabis users, it appears to be reliable and a strong predictor of quit attempts among tobacco smokers (Hughes JR et al., 2014c). The 6-month surveys only asked participants about the number of days of abstinence and whether they had received treatment for cannabis use. Participants were reimbursed $2 for daily IVR completion plus a $10 bonus if they completed all IVR calls in a week. They received $7 for completion of each mailed or web-based survey. The total maximum compensation was $363.
Data Analysis
So that each participant would provide the same amount of data, descriptive summary statistics were calculated by first averaging within participants, and then averaging across participants. Most of the outcomes had skewed distributions; thus, we often report medians and 25th/75th percentiles. If there was a gap of ≤ 3 days of missing data and participants stated they were abstinent all week on the weekly IVR, we imputed abstinence during those days; otherwise, missing was assumed to represent usual cannabis use. Questions about within-subject changes were evaluated with multilevel models (Hox 2002) with the study participants treated as the second level using a random intercept and unstructured covariance matrix. This approach is appropriate when there are a large number of repeated measures and when there are varying number of records per participant. F statistics were reported for these analyses. In addition, Cox regression for multilevel survival analysis (UCLA Statistical Consulting Group, 2015) was used to examine duration of attempts. The analyses used SAS version 9.4 (SAS Institute, Cary, NC). We did not use other longitudinal statistics such as growth curves and GEE because our focus was not on describing trends over time, but rather on the seven specific clinical questions outline in the Introduction. For testing those questions, multilevel models provided the ability to examine both within and between participant trends. We did not correct for multiple testing because many statisticians believe such corrections are inappropriate when analyses are considered exploratory, such as ours(Feise, 2002; Perneger, 1998).
Results
Compliance
Participants provided IVR data on a median of 96% (81%–100%) of days. Few (11%) participants dropped out during the study. The median day on which these participants dropped out was day 48 (25–59). Men were more likely to drop out during the 3 month IVR period; 68% vs 44%; x2 =4.6, p=0.03.
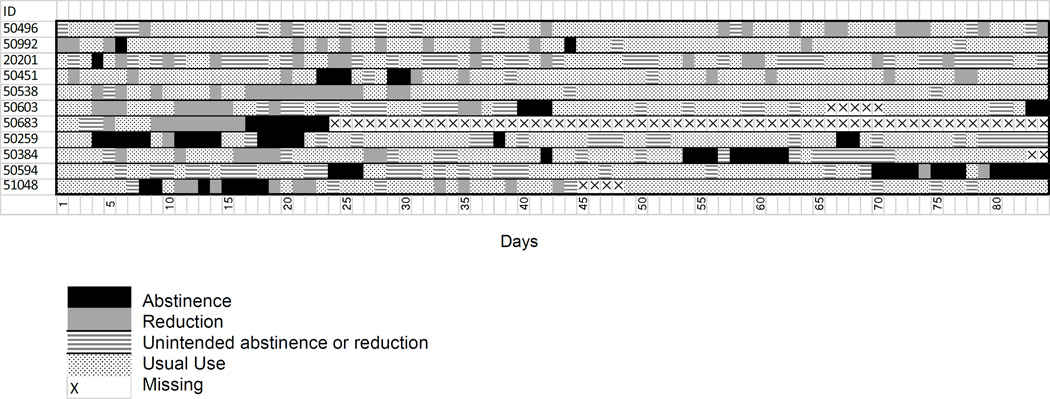
Attempts to Change
Participants made multiple, and often rapid, transitions among usual use, abstinence and reduction states. Across the 84 days of IVR reporting, the median number of within-participant transitions among these three states was 22 (12, 31). In lieu of presenting raw data for all 191 participants, Figure 2 provides examples of the patterns of change. This figure provides results of “average” participants; i.e. the 11 participants nearest the median number of days of abstinence or reduction during the study. This figure illustrates not only the large number of transitions, but also the large variability in change patterns across participants. Since these participants are near the median, about half of the participants will have more, and half fewer, transitions than these exemplar participants.
Figure 2.
Use status of “average” participants; i.e., the 11 participants nearest the median number of days of abstinence or reduction for the entire sample. Black = day of intentional abstinence (i.e., quit attempt), gray = day of intentional reduction, dotted = day of usual use (including unintentional abstinence or reduction), X = day with missing data.
Quit Attempts
About half (46%) of participants made a quit attempt at some point in the study. At the end of the 3 month IVR monitoring period, 10% of participants had been abstinent for the prior 7 days; i.e. point prevalent abstinent, and 5% had been abstinent for the prior month; i.e. sustained abstinent. Determining the average duration of a quit attempt requires defining when a quit attempt begins and ends. For example, suppose a cannabis user was abstinent for 2 days, used for 2 days, and then was abstinent again. Whether this represents one or two quit attempts depends on the definition of the duration of a quit attempt. One possibility is to define a quit attempt to last until a “lapse” (i.e. any use) occurs. Using this definition, among those who made a quit attempt, the median number of quit attempts was relatively large, but the duration of a quit attempt was small (Table 1). With tobacco quit attempts, a quit attempt is usually defined to last until a “relapse” occurs, where a relapse is defined as 7 consecutive days of use (Hughes et al., 2003). If we use this definition, the median number of attempts is small, and the median duration of attempts is relatively long (Table 1).
Table 1.
Number and duration of quit attempts using two definitions of duration of a quit attempt
| Quit attempt ends with first lapse n = 402 |
Quit attempt ends with 7 days of continuous use n = 148 |
|
|---|---|---|
| Median number of attempts | 3 (2, 6)* | 1 (1, 2) |
| Median duration of attempts (days) | 2 (1, 6) | 9 (2, 40) |
(25th, 75th percentiles)
In the multilevel analysis, the incidence of quit attempts (i.e. intentional abstinence) declined over time (F = 17.8, p < .0001). For example, the incidence of a new quit attempt in the first week of the study was 19% and in the last week was 5%. Among users who tried to quit and failed during the first month, 61% tried to quit again in the second or third month, and their median time between failing and a second attempt was 27 days. Those who made a quit attempt and failed in the first month had a greater, not lesser, chance of making a quit attempt in the second or third month than those who did not make a quit attempt in the first month (72% vs 19%, OR = 11.0, p < .0001). In addition, when those who attempted and failed in the first month then made a quit attempt in the second or third month, the duration of their second attempt was no different from those who had not tried in the first month but then tried in the second or third month (Wald chi-square = 0.11, p = .74).
When a quit attempt occurred, the IVR asked if participants engaged in any of the following five activities during the quit attempt: asking for advice, avoiding other users, getting rid of cannabis, talking to a counselor, or telling others about the quit attempt. In most quit attempts (69%), one or more of these occurred. In the multilevel analysis, engaging in at least one of these behaviors during the quit attempt predicted a greater duration of the quit attempt (medians = 15 days vs 5 days, chi-square = 10.1, p =.002). The only individual behavior to predict duration of abstinence, independent of the other behaviors, was telling someone that they were trying to stop or reduce during the quit attempt (15 days if they did so vs 6 days if they did not; Wald Chi-Square = 6.9, p =.0009)
Among the baseline variables, the occurrence of DSM Cannabis Use Disorder predicted a decreased probability of a quit attempt (OR = 0.80; 95% CI = 0.72, 0.90, p = .0001). Age, sex, minority status, marital status, education, employment, age of onset of cannabis use, alcohol use and tobacco use did not predict a quit attempt. Among the participants who made a quit attempt, none of the baseline variables predicted the duration of abstinence on their longest quit attempt during the study.
Ten participants sought treatment during the study (6% of those who intentionally tried to stop or reduce during the IVR period). Nine sought outpatient treatment. The one participant who entered residential treatment was excluded from the analyses.
Intentional Reduction
Most (85%) participants made an intentional reduction attempt during the study. Overall, reduction attempts occurred on 18% of study days. Few (5%) intentional reduction attempts lasted more than a week. To examine the validity of reports of use of less cannabis, we compared the number of times of cannabis use on days in which participants reported reduced use with that on days they reported usual use. In the multilevel analysis, use was lower on days of reduced use (2.0 vs 3.3, multilevel regression F = 2284, p < .0001). On days of reduced use, the intoxication rating was 3.2 (on 0–6 scale) vs 4.0 on days of usual use (F = 812, p < .0001).
Among the participants who did not make a quit attempt in the first month, those who had more days of reduction in the first month were more likely to make a quit attempt in the second or third month than those who did not reduce (OR = 3.6, 95% CI = 1.4, 9.3, p =.01). For example, 29% of those with 5+ days of reduction in first month made a quit attempt vs 10% of those with 0–4 days of reduction in the first month.
Changes in Withdrawal Symptoms and Tobacco, Alcohol and Drug Use During Days of Abstinence
To examine withdrawal effects we compared symptoms on days of usual use vs days of abstinence (either intentional or unintentional). In the multilevel analysis, ratings of sadness, nervousness, anger, and sleep problems were greater on days of abstinence (all F values > 28, all p values < .001), but these effects were small (increases of 0.1 – 0.2 on a 4-point scale). Ratings of craving and hunger were lower during abstinence (decrease of 0.3 units, both F values > 137, both p values < .0001).
Among the 100 occasional or daily tobacco smokers at study entry, 5% quit smoking tobacco during the study (i.e., did not smoke on the last 7 days of the study). Four (9%) of the former tobacco smokers and one (2%) of the never smokers were smoking regularly at the end of the study (i.e. smoked at least once per week for the last 4 weeks of the study).
Among the 82 regular (i.e. weekly) alcohol users at study entry, the median number of drinks/day (1.3 vs 1.7, F = 11.3, p< .001) and the incidence of binge drinking (4.4% vs 6.6%, F = 6.2, p = .01) was less on abstinent days than on days of usual use. Among those who used alcohol weekly at baseline, 4 particpants (6%) did not use any alcohol in the last month of the IVR period. Among those who, at baseline, stated they never used alcohol, one (3%) was using alcohol weekly by the end of the study but was drinking few (median = 2) beverages/week. Among those who reported illegal drug use in the 30 days prior to study entry (n= 29), use of illegal drugs was uncommon (6% of days) and did not differ between abstinent and usual use days.
3- Month (End of Study) and 6-Month Surveys
Most participants (84%) completed the survey that occurred at the end of IVR call period. Among the 75% who continued to use cannabis daily at that point, perceived difficulty in quitting decreased (3.1 vs 2.9 on 4-point scale, t = 3.0, p <.003) as did number of problems from marijuana use (6.4 vs 5.2, t = 3.5, p = .0007) and number of DSM criteria (4.3 vs 3.4, t = −4.2, p =.001). Motivation to stop cannabis did not change from baseline to 3-month follow-up
Among those who were still using cannabis at 3 months, a greater percent of days of intentional reduction during the 3 months period prospectively predicted a greater decline in the number of DSM 5 criteria (t= −2.8, p = .006) and a greater reduction in the number of cannabis problems (t= −2.7, p = .01). A greater percent of days of intentional abstinence also predicted a greater reduction in DSM criteria (t = − 2.6, p=.006) but did not predict a greater reduction in problems. Neither the amount of reduction nor abstinence predicted increase in motivation or decrease in perceived difficulty of quitting.
Six-month drop-outs were more likely to be male (60% vs 42%) , younger (27 vs 32 years old) and non-minority users (24% vs 46%) and had an earlier age of onset of use (15 vs 16)( all p’s ≤ 0.03). At 6 month follow-up, 8% of participants had not used cannabis in the last month.
Discussion
This study replicates our prior findings (Hughes et al., 2008) that a) cannabis users trying to change make many, and often rapid, transitions among use as usual, reduction and abstinence states; b) reduction attempts are more common than abstinence attempts; c) quit and reduction attempts are short-lived and few participants achieve long-term abstinence; d) use of alcohol and illicit drugs does not significantly increase with abstinence; and e) few seek treatment. In addition, novel findings of the study are that f) most users did not prepare ahead of time before their quit attempt; g) tobacco use and alcohol use were less common on days of cannabis abstinence than on days of cannabis use; h) symptoms of withdrawal occurred even with short quit attempts; i) abstinence and reduction predicted decreases in cannabis dependence; and j) planning activities during the quit attempt predicted greater abstinence.
One liability of the current study is the lack of biological validation of self-reports. Although we know of no studies of the validity of self-reports among cannabis users in non-treatment settings, studies of alcohol (Del Boca & Darkes, 2003) and tobacco (SRNT Subcommittee on Biochemical Verification, 2002) users in these settings suggest self-report is accurate. In addition, the large majority of our participants had no phone contact with study staff during the study, thereby decreasing experimenter demand. Another possible liability is that the repeated measurement was reactive; i.e., decreased cannabis use. Although we know of no test of this among cannabis users, most studies using IVR (Helzer et al., 2002) or Ecological Momentary Assessments (Shiffman, 2009) have failed to find reactivity with alcohol and tobacco users. Finally, we sampled only daily cannabis users who were intending to quit or reduce at some point in the next 3 months. We know of no data to estimate what proportion of daily cannabis users this represents. The major assets of the study are a) the inclusion of a large sample of non-treatment seeking, daily, cannabis users; b) the collection of prospective, daily data on attempts to change; and c) high compliance.
This study found that most cannabis users make multiple attempts to stop or reduce and such attempts continue over time. Many studies of cannabis abstinence or reduction focus on a single attempt to stop or reduce cannabis use, and many do not follow participants after they relapse. In the current study and in almost all prior studies, the large majority of attempts to change cannabis fail (Moore & Budney, 2003) (Calabria et al., 2010). However, failed quit attempts predicted an increased, not decreased, probability of later quit attempts. Thus, a failed quit or reduction attempt is a marker of increased, not decreased, interest in changing. These results suggest researchers should focus not just on the outcome of the initial attempt to change, but also on continued attempts to change that occur after a lapse or relapse. Similarly, our findings suggest clinicians and clients might best view change as a process that will usually require failed attempts and, thus, treatment may need to be ongoing to encompass several attempts to change.
Although abstinence attempts continued throughout the 3-month study, the incidence of new quit attempts decreased over time. This result is consistent with empirical evidence from the “Strength Model” of motivation (Hagger, Wood, & Stiff, 2010) and the concept of “cessation fatigue” (Liu, Li, Lanza, Vasilenko, & Piper, 2013), both of which posit individuals have a finite amount of “energy” for self-regulation and predict that repeated failures should result in less motivation. On the other hand, in our study those who tried to quit and failed early on during the IVR period were more, not less, likely to make later quit attempts than those who did not try to quit.
Whether a goal of reduction only (i.e. not in preparation for abstinence) should be accepted as a primary treatment goal among cannabis users is debatable (Lozano, Stephens, & Roffman, 2006). Reduction attempts were more common than abstinence attempts in our self-changers. However, even over the 3 months of the study, most users attempted both abstinence and reduction, suggesting goal is a state, not trait, phenomena. During the IVR period, a greater amount of reduction predicted less problems and less dependence and a greater probability of a later quit attempt. This would suggest reduction may be an acceptable goal. On the other hand greater reduction did not predict increases in motivation to quit or decreases in perceived difficulty in quitting. Clearly, more empirical research on reduction as a goal of treatment is warranted.
Similar to the results of epidemiological studies (Blanco et al., 2015), we found that seeking treatment is uncommon. In the current study, activities during a quit influenced abstinence. Although we know of no test of the efficacy of pre- vs. post-quit attempt activities in cannabis cessation, several studies on tobacco self-quitters have found that preparatory actions such as telling someone that one is trying to change (Cobb, Niaura, Donaldson, & Graham, 2014) (Hughes JR et al., 2014c), and post-cessation actions such as coping behaviors (Fiore et al., 2008) predict abstinence. However, an experimental comparison of pre- vs. post-quit attempt actions in tobacco users found post-quit but not pre-quit actions predicted long-term abstinence (Borland, Balmford, & Swift, 2015).
Similar to our prior study (Hughes et al., 2008), almost all attempts to stop or reduce cannabis lasted less than a week, and many did not last more than one day. We do not know of other studies of how quickly cannabis users trying to quit on their own relapse. However, the steep relapse observed in this study is similar to that of self-quitting in tobacco smokers (Hughes, Keely, & Naud, 2004). This rapid relapse rate suggests “front-loaded” treatment with multiple contacts in the first week of a quit attempt (Garvey et al., 2012) should be considered.
All of the DSM 5 cannabis withdrawal symptoms we tested changed as expected on abstinence days even though many attempts were short-lived. Our study adds to the several studies that have validated symptoms of cannabis withdrawal (Del Boca & Darkes, 2003), by adding an externally valid test of these symptoms. Although we have labeled these as withdrawal symptoms, due to the short duration of abstinence periods in our study we could not verify the classic transitory pattern of symptoms and thus cannot rule out that these symptoms represent the simple offset of the direct effects of cannabis(Hughes, 1991). Our study did find that craving decreased, not increased, with abstinence. Interestingly, craving failed to increase in about half of the prior cannabis abstinence studies (Allsop et al., 2012), and this also often occurred in tobacco abstinence studies (Shiffman, West, & Gilbert, 2004).
Six prior studies have found increases, decreases and no change in alcohol and tobacco use during cannabis abstinence (Allsop et al., 2014). In the most rigorous study of non-treatment seekers, alcohol substantially increased (+8 standard drinks/week) as did tobacco use (+2 cigs/day) during abstinence (Allsop et al., 2014). In contrast, the current study found a decrease in alcohol and illicit drug use on days of cannabis abstinence and slightly less tobacco use. Our findings may differ from this prior study because periods of abstinence in our study were very short. Also, we excluded dependent alcohol users. Finally perhaps, initially alcohol and drug use declines but then increases with longer duration of abstinence.
Only 8% of those trying to quit cannabis were abstinent at 6-month follow-up. We could not locate a prospective study of the incidence of long-term abstinence among cannabis users who try to stop on their own; however, the 8% success rate in this study is almost identical to that for tobacco self-quitters (Hughes et al., 2004).
In summary, the current results with cannabis users trying to change are very similar to those of our prior study of daily cannabis users (Hughes et al., 2008) and our prior studies of tobacco smokers using the same methodology (Hughes JR et al., 2014c; Peters & Hughes, 2009; Hughes et al., 2013). Specifically, heavy cannabis users trying to change make multiple, unplanned and short-lived attempts to change and even short periods of cannabis abstinence precipitate withdrawal symptoms but do not appear to increase alcohol and tobacco use. Since many of those who try to change fail and quickly try again, we believe future research and treatment should focus on helping with a series of attempts to change, not just one. Also, reduction was a common goal in our study and predicted a greater probability of a quit attempt and a decrease in problems or dependence. Given this, further studies on reduction as a treatment goal are needed.
Acknowledgements
We thank Emily Casey, Ginger Cloud, Miki Dash, Tonya Ferraro, Matthew MacKinnon, Sharon Muellers, Adam Rhodes-Rogan, and Beth Walsh for their help in the conduct of the study.
Role of funding source: This study was funded by grant 1 R01 DA-025089 from the US National Institute on Drug Abuse. The funding source had no role in the collection, analysis and interpretation of the data; in the writing of the report, and in the decision to submit the study for publication.
Footnotes
Conflict of Interest: none
Contributors: JH and AB designed and obtained funding for the study. JH and JF conducted the study. PC and SN undertook the statistical analyses. JH wrote the first draft of the manuscript. All authors helped interpret the study results and write the paper.
Reference List
- Aitken SS, DeSantis J, Harford TC, FeCaces M. Marijuana use among adults. A longitudinal study of current and former users. Journal of Substance Abuse. 2000;12:213–226. doi: 10.1016/s0899-3289(00)00051-1. [DOI] [PubMed] [Google Scholar]
- Allsop DJ, Dunlop AJ, Sadler C, Rivas GR, McGregor IS, Copeland J. Changes in cigarette and alcohol use during cannabis abstinence. Drug and Alcohol Dependence. 2014;138:54–60. doi: 10.1016/j.drugalcdep.2014.01.022. [DOI] [PubMed] [Google Scholar]
- Allsop D, Copeland J, Norberg MM, Fu S, Molnar A, Lewis J, et al. Quantifying the clinical significance of cannabis withdrawal. PLoS One. 2012;7:e44864. doi: 10.1371/journal.pone.0044864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aquilino WS. Telephone versus face-to-face interviewing for household drug use surveys. International Journal of Addiction. 1992;27:71–91. doi: 10.3109/10826089109063463. [DOI] [PubMed] [Google Scholar]
- Babson KA, Tyler Boden M, Bonn-Miller MO. The impact of perceived sleep quality and sleep efficiency/duration on cannabis use. Addictive Behaviors. 2013;38(11):2707–2713. doi: 10.1016/j.addbeh.2013.06.012. [DOI] [PubMed] [Google Scholar]
- Babson KA, Tyler Boden M, Harris AH, Stickle TR, Bonn-Miller MO. Poor sleep quality as a risk factor for lapse following a cannabis quit attempt. Journal of Substance AbuseTreatment. 2013;44:438–443. doi: 10.1016/j.jsat.2012.08.224. [DOI] [PubMed] [Google Scholar]
- Blanco C, Iza M, Fernandez-Rodriguez JM, Baca-Garcia E, Wang S, Olfson M. Probability and predictors of treatment-seeking for substance use disorders in the U.S. Drug and Alcohol Dependence. 2015;149:136–144. doi: 10.1016/j.drugalcdep.2015.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller MO, Moos RH, Boden MT, Long WR, Kimerling R, Trafton JA. The influence of posttraumatic stress disorder on cannabis quit success. American Journal of Drug and Alcohol Abuse. 2015;41(4):339–344. doi: 10.3109/00952990.2015.1043209. [DOI] [PubMed] [Google Scholar]
- Borland R, Balmford J, Swift E. Effects of encouraging rapid implementation and/or structured planning of quit attempts on smoking cessation outcomes: A randomized controlled trial. Annals of Behavioral Medicine, Epub ahead of print. 2015 doi: 10.1007/s12160-015-9706-3. [DOI] [PubMed] [Google Scholar]
- Boyd SJ, Tashkin DP, Huestis MA, Heishman SJ, Dermand JC, Simmons MS, et al. Strategies for quitting among non-treatment-seeking marijuana smokers. American Journal on Addictions. 2005;14:35–42. doi: 10.1080/10550490590899835. [DOI] [PubMed] [Google Scholar]
- Buckner J, Keough ME, Schmidt NB. Problematic alcohol and cannabis use among young adults: The roles of depression and discomfort and distress tolerance. Addictive Behaviors. 2007;32(9):1957–1963. doi: 10.1016/j.addbeh.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner J, Zvolensky M, Ecker A. Cannabis use during a voluntary quit attempt: an analysis from ecological momentary assessment. Drug and Alcohol Dependence. 2013;132:610–616. doi: 10.1016/j.drugalcdep.2013.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney AJ, Radonovich KJ, Higgins ST, Wong CJ. Adults seeking treatment for marijuana dependence: A comparison with cocaine-dependent treatment seekers. Experimental and Clinical Psychopharmacology. 1998;6(4):419–426. doi: 10.1037//1064-1297.6.4.419. [DOI] [PubMed] [Google Scholar]
- Budney A, Vandrey R, Stanger C. Pharmacological and psychosocial interventions for cannabis use disorders. Revista Brasileira de Psyquiatria. 2010;32:S46–S55. [PMC free article] [PubMed] [Google Scholar]
- Calabria B, Degenhardt L, Brieglib C, Vos T, Hall W, Lynskey M, et al. Systematic review of prospective studies investigating “remission” from amphetamine, cannabis, cocaine or opioid dependence. Addictive Behaviors. 2010;35:741–749. doi: 10.1016/j.addbeh.2010.03.019. [DOI] [PubMed] [Google Scholar]
- Chauchard E, Levin K, Copersino ML, Heishman SJ, Gorelick DA. Motivations to quit cannabis use in an adult non-treatment sample: Are they related to relapse? Addictive Behaviors. 2013;38:2422–2427. doi: 10.1016/j.addbeh.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu YL. The effects of medical marijuana laws on illegal marijuana use. Journal of Heatlh Economics. 2014;38:43–61. doi: 10.1016/j.jhealeco.2014.07.003. [DOI] [PubMed] [Google Scholar]
- Cobb CO, Niaura R, Donaldson EA, Graham AL. Quit now? Quit soon? Quit when you’re ready? Insights about target quit dates for smoking cessation from an online quit date tool. J.Med.Internet Res. 2014;16(2):e55. doi: 10.2196/jmir.3086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States. 1991–1992 and 2001–2002. Journal of the American Medical Association. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- Copersino ML, Boyd SJ, Tashkin DP, Huestis MA, Heishman SJ, Dermand JC, et al. Cannabis withdrawal among non-treatment-seeking adults cannabis users. The American Journal on Addictions. 2006a;15:8–14. doi: 10.1080/10550490500418997. [DOI] [PubMed] [Google Scholar]
- Copersino ML, Boyd SJ, Tashkin DP, Huestis MA, Heishman SJ, Dermand JC, et al. Quitting among non-treatment-seeking marijuana users: Reasons and changes in other substance use. Am Jl Addiction. 2006b;15:297–302. doi: 10.1080/10550490600754341. [DOI] [PubMed] [Google Scholar]
- Corkrey R, Parkinson L. Interactive Voice Response: Review of studies 1989–2000. Behavior Research Methods, Instruments & Computers. 2002;34:342–353. doi: 10.3758/bf03195462. [DOI] [PubMed] [Google Scholar]
- Del Boca F, Darkes J. The validity of self reports of alcohol consumption: State of the science and challenges for research. Addiction. 2003;98:S1–S12. doi: 10.1046/j.1359-6357.2003.00586.x. [DOI] [PubMed] [Google Scholar]
- Downey LA, Verster JC. Cannabis concerns: Increased potency, availability and synthetic analogues. Current Drug Abuse Review. 2014;7:67–68. doi: 10.2174/1874473708666150113165140. [DOI] [PubMed] [Google Scholar]
- Ellingstad TP, Sobell LC, Sobell MB, Eickleberry L, Golden CJ. Self-change: A pathway to cannabis abuse resolution. Addictive Behaviors. 2006;31:519–530. doi: 10.1016/j.addbeh.2005.05.033. [DOI] [PubMed] [Google Scholar]
- Feise R. Do multiple outcome measures require p-value adjustment? BMC Medical Research Methodology, 2. 2002 doi: 10.1186/1471-2288-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore M, Jaen C, Baker T, Bailey W, Benowitz N, Curry S, et al. Treating Tobacco Use and Dependence: Clinical Practice Guideline. Washington, DC: US Public Health and Human Services; 2008. [Google Scholar]
- Fleiss J. Statistical Methods for Rates and Proportions. 3rd. Hoboken, NJ: Wiley-Interscience; 2003. [Google Scholar]
- Garvey A, Kalman D, Hoskinson R, Jr, Kinnunen T, Wadler B, Thomson C, et al. Front-loaded versus weekly counseling for treatment of tobacco addiction. Nicotine & Tobacco Research. 2012;14:578–585. doi: 10.1093/ntr/ntr256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon AJ, Conley JW, Gordon JM. Medical consequences of marijuana use: A review of current literature. Current Psychiatry Reports. 2013;15:419. doi: 10.1007/s11920-013-0419-7. [DOI] [PubMed] [Google Scholar]
- Hagger M, Wood C, Stiff C. Ego depletion and the strength model of self-control: A meta-analysis. Psychological Bulletin. 2010;136(4):495–525. doi: 10.1037/a0019486. [DOI] [PubMed] [Google Scholar]
- Heinz A, Peters E, Boden M, Bonn-Miller M. A comprehensive examination of delay discounting in a clinical sample of cannabis-dependent military veterans making a self-guided quit attempt. Experimental Clinical Psychopharmacology. 2013;21:55–65. doi: 10.1037/a0031192. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Badger GJ, Rose GL, Mongeon JA, Searles JS. Decline in alcohol consumption during two years of daily reporting. Journal of Studies on Alcohol. 2002;63:551–558. doi: 10.15288/jsa.2002.63.551. [DOI] [PubMed] [Google Scholar]
- Hudziak JJ, Helzer JE, Wetzel MW, Kessel KB, McGee B, Janca A, et al. The use of the DSM-III-R checklist for initial diagnostic assessments. Comprehensive Psychiatry. 1993;34:375–383. doi: 10.1016/0010-440x(93)90061-8. [DOI] [PubMed] [Google Scholar]
- Hufford MR, Shields AL, Shiffman S, Paty J, Balabanis M. Reactivity to ecological momentary assessment: An example using undergraduate problem drinkers. Psychology of Addictive Behaviors. 2002;16:205–211. [PubMed] [Google Scholar]
- Hughes JR, Fingar J, Budney A, Naud S, Helzer JE, Callas P. Marijuana use and intoxication among daily users: An intensive longitudinal study. Addictive Behaviors. 2014a;39(10):1464–1470. doi: 10.1016/j.addbeh.2014.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Solomon LJ, Naud S, Fingar J, Helzer JE, Callas P. Natural history of attempts to stop smoking. NicotineTobacco Research. 2014b doi: 10.1093/ntr/ntu052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Solomon LJ, Naud S, Fingar J, Helzer JE, Callas P. Natural history of attempts to stop smoking. Nicotine & Tobacco Research. 2014c;16:1190–1198. doi: 10.1093/ntr/ntu052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99:29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Fagerstrom K-O, Callas PW. Intentions to quit smoking change over short periods of time. Addictive Behaviors. 2005;30:653–662. doi: 10.1016/j.addbeh.2004.08.011. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Naud S, Fingar J, Callas P, Solomon L. Do environmental cues prompt attempts to stop smoking? A prospective natural history study. Drug and Alcohol Dependence. 2015;154:146–151. doi: 10.1016/j.drugalcdep.2015.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR. Distinguishing withdrawal relief and direct effects of smoking. Psychopharmacology. 1991;104:409–410. doi: 10.1007/BF02246044. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely J, Niaura R, Ossip-Klein D, Richmond R, Swan G. Measures of abstinence in clinical trials: Issues and recommendations. Nicotine & Tobacco Research. 2003;5:13–25. [PubMed] [Google Scholar]
- Hughes J, Peters E, Callas P, Budney A, Livingston A. Attempts to stop or reduce marijuana use in non-treatment seekers: A pilot study. Drug and Alcohol Dependence. 2008;97:180–184. doi: 10.1016/j.drugalcdep.2008.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes J, Solomon L, Fingar J, Naud S, Helzer J, Callas P. The natural history of efforts to stop smoking: A prospective cohort study. Drug and Alcohol Dependence. 2013;128:171–174. doi: 10.1016/j.drugalcdep.2012.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irons JG, Babson KA, Bergeria CL, Bonn-Miller MO. Physical activity and cannabis cessation. The American Journal on Addictions. 2014;23:485–492. doi: 10.1111/j.1521-0391.2014.12135.x. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Raveis VH. Cessation of illicit drug use in young adulthood. Archives of General Psychiatry. 1989;46:109–116. doi: 10.1001/archpsyc.1989.01810020011003. [DOI] [PubMed] [Google Scholar]
- Klingemann H, Sobell L, Barker J, Blomqvist J, Cloud W, Ellinstad T, et al. Promoting Self-Change from Problem Substance Use: Practical Implications for Policy, Prevention and Treatment. Dordrecht, Netherlands: Kluwer Academic Publications; 2001. [Google Scholar]
- Kobak KA, Taylor LvH, Dottl SL, Greist JH, Jefferson JW, Burroughs D, et al. A computer-administered telephone interview to identify mental disorders. Journal of the American Medical Association. 1997;278:905–910. [PubMed] [Google Scholar]
- Liu X, Li R, Lanza ST, Vasilenko SA, Piper M. Understanding the role of cessation fatigue in the smoking cessation. Drug and Alcohol Dependence. 2013;133:548–555. doi: 10.1016/j.drugalcdep.2013.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozano BE, Stephens RS, Roffman RA. Abstinence and moderate use goals in the treatment of marijuana dependence. Addiction. 2006;101:1589–1597. doi: 10.1111/j.1360-0443.2006.01609.x. [DOI] [PubMed] [Google Scholar]
- Marijuana Treatment Project Research Group. Brief treatments for cannabis dependence: Findings from a randomized multi-site trial. Journal of Consulting and Clinical Psychology. 2004;72:455–466. doi: 10.1037/0022-006X.72.3.455. [DOI] [PubMed] [Google Scholar]
- Moore BA, Budney AJ. Relapse in outpatient treatment for marijuana dependence. Journal of Substance Abuse Treatment. 2003;25:85–89. doi: 10.1016/s0740-5472(03)00083-7. [DOI] [PubMed] [Google Scholar]
- Office of Applied Statistics. Treatment Episode Data Set (TEDS) 2007 www.oas.samhsa.gov/teds.
- Perneger TV. What’s wrong with Bonferroni adjustments. British Medical Journal. 1998;316:1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters E, Hughes J. The day-to-day process of stopping or reducing smoking: A prospective study of self-changers. Nicotine & Tobacco Research. 2009;11:1083–1092. doi: 10.1093/ntr/ntp105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pointek d, Kraus L, Klempova D. Short scales to assess cannabis-related problems: A review of psychometric properties. Substance Abuse Treatment, Prevention, and Policy. 2008;3:1–10. doi: 10.1186/1747-597X-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S. Ecological momentary assessment (EMA) in studies of substance use. Psychological Assessment. 2009;21:486–497. doi: 10.1037/a0017074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Hufford M, Hickcox M, Paty JA, Gnys M, Kassel JD. Remember that? A comparison of real-time versus retrospective recall of smoking lapses. Journal of Consulting and Clinical Psychology. 1997;65(2):292–300. doi: 10.1037/0022-006x.65.2.292.a. [DOI] [PubMed] [Google Scholar]
- Shiffman S, West RJ, Gilbert DG. Recommendation for the assessment of tobacco craving and withdrawal in smoking cessation trials. Nicotine & Tobacco Research. 2004;6:599–614. doi: 10.1080/14622200410001734067. [DOI] [PubMed] [Google Scholar]
- SRNT Subcommittee on Biochemical Verification. Biochemical verification of tobacco use and cessation. Nicotine & Tobacco Research. 2002;4:149–159. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- Stephens RS, Babor TF, Kadden R, Miller M. The Marijuana Treatment Project: Rationale, design and participant characteristics. Addiction. 2002;97:109–124. doi: 10.1046/j.1360-0443.97.s01.6.x. [DOI] [PubMed] [Google Scholar]
- Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology. 2000;68(5):898–908. [PubMed] [Google Scholar]
- Stephens R, Roffman R, Fearer S, Williams C, Picciano J, Burke R. The Marijuana Check-up: Reaching users who are ambivalent about change. Addiction. 2004;99:1323–1332. doi: 10.1111/j.1360-0443.2004.00832.x. [DOI] [PubMed] [Google Scholar]
- Stinson FS, Ruan WJ, Pickering R, Grant BF. Cannabis use disorders in the USA: Prevalence, correlates and co-morbidity. Psychological Medicine. 2006;36:1447–1460. doi: 10.1017/S0033291706008361. [DOI] [PubMed] [Google Scholar]
- Swift W, Copeland J, Hall W. Choosing a diagnostic cut-off for cannabis dependence. Addiction. 1998;93:1681–1692. doi: 10.1046/j.1360-0443.1998.931116816.x. [DOI] [PubMed] [Google Scholar]
- Swift W, Hall W, Copeland J. One year follow-up of cannabis dependence among long-term users in Syndey, Australia. Drug and Alcohol Dependence. 2000;59:309–318. doi: 10.1016/s0376-8716(99)00131-3. [DOI] [PubMed] [Google Scholar]
- Tyler Boden M, McKay JR, Long WR, Bonn-Miller MO. The effects of cannabis use expectancies on self-initiated cannabis cessation. Addiction. 2013;108:1649–1657. doi: 10.1111/add.12233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UCLA Statistical Consulting Group. SAS FAQ: How can I model repeated events survival analysis in proc phreg? 2015 Retrieved from http://www.ats.ucla.edu/stat/sas/faq/survival_repeated_events.html.
- VonSydow K, Lieb R, Pfister H, Hofler M, Sonntag H, Wittchen HU. The natural course of cannabis use, abuse and dependence over four years: A. 2001 doi: 10.1016/s0376-8716(01)00137-5. [DOI] [PubMed] [Google Scholar]