Abstract
Study Objectives:
Rapid eye movement (REM) sleep behavior disorder (RBD) is a parasomnia characterized by impaired motor inhibition during REM sleep, and dream-enacting behavior. RBD is especially associated with α-synucleinopathies, such as Parkinson disease (PD). Follow-up studies have shown that patients with idiopathic RBD (iRBD) have an increased risk of developing an α-synucleinopathy in later life. Although abundant studies have shown that degeneration of the nigrostriatal dopaminergic system is associated with daytime motor function in Parkinson disease, only few studies have investigated the relation between this system and electromyographic (EMG) activity during sleep. The objective of this study was to investigate the relationship between the nigrostriatal dopamine system and muscle activity during sleep in iRBD and PD.
Methods:
10 iRBD patients, 10 PD patients with PD, 10 PD patients without RBD, and 10 healthy controls were included and assessed with (123)I-N-omega-fluoropropyl-2-beta-carboxymethoxy-3beta-(4-iodophenyl) nortropane ((123)I-FP-CIT) Single-photon emission computed tomography (SPECT) scanning (123I-FP-CIT SPECT), neurological examination, and polysomnography.
Results:
iRBD patients and PD patients with RBD had increased EMG-activity compared to healthy controls. 123I-FP-CIT uptake in the putamen-region was highest in controls, followed by iRBD patients, and lowest in PD patients. In iRBD patients, EMG-activity in the mentalis muscle was correlated to 123I-FP-CIT uptake in the putamen. In PD patients, EMG-activity was correlated to anti-Parkinson medication.
Conclusions:
Our results support the hypothesis that increased EMG-activity during REM sleep is at least partly linked to the nigrostriatal dopamine system in iRBD, and with dopamine function in PD.
Citation:
Zoetmulder M, Nikolic M, Biernat H, Korbo L, Friberg L, Jennum P. Increased motor activity during rem sleep is linked with dopamine function in idiopathic REM sleep behavior disorder and Parkinson disease. J Clin Sleep Med 2016;12(6):895–903.
Keywords: idiopathic REM sleep behavior disorder, Parkinson disease, EMG, dopamine transporters, SPECT
INTRODUCTION
REM sleep behavior disorder (RBD) is a parasomnia characterized by REM sleep without atonia, dream enactment behavior, and vivid (and/or) violent dreams. Longitudinal studies have shown that patients with idiopathic RBD (iRBD) have an increased risk for developing an α-synucleinopathy, such as Parkinson disease (PD).1,2 The high proportion of iRBD patients developing PD may indicate a link between nigrostriatal degeneration and increased night-time motor activity. It is increasingly recognized that the dopaminergic system is associated with sleep-wake disturbances.3,4 Previous studies have shown that basal ganglia structures, such as the substantia nigra pars reticulata and the internal segment of the globus pallidus, have caudal connections to regions that modulate REM sleep atonia.5 Imaging studies in iRBD patients have shown microstructural changes in substantia nigra,6 reduced volume of the putamen,7 as well as reduced density of the striatal dopamine transporter, which decreases in the course of disease progression.8 In addition monkeys treated sub-chronic with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine hydrochloride (MPTP), a neurotoxin which specifically targets dopaminergic neurons of the substantia nigra pars compacta via uptake by the dopamine transporter, show an increase in the number of sleep epochs with high-amplitude EMG bouts during REM sleep compared to control animals.9 The high selectivity of MPTP to dopaminergic neurons suggests that the presence of REM sleep without atonia might reflect the early involvement of dopaminergic neurotransmission on medullary and/or pontine REM sleep-related structures. Only few studies have investigated the role of dopaminergic nigrostriatal denervation in relation to motor activity during REM sleep, and none during NREM sleep.10,11 We conducted a study using 123I-FP-CIT SPECT in patients with iRBD, PD with RBD, PD without RBD, and healthy controls to determine whether increased muscle activity during REM and NREM sleep is associated with an abnormality of the presynaptic dopamine transporters.
BRIEF SUMMARY
Current Knowledge/Study Rationale: The pathophysiology of RBD in PD is unclear. Although degeneration of the nigrostriatal dopaminergic system is characteristic for daytime motor function in PD, only few studies have investigated this system in motor function, atonia, during sleep. This study investigated the relation between the nigrostriatal dopamine system and EMG-activity during sleep in iRBD and PD.
Study Impact: We show in this study that increased EMG-activity during REM/NREM sleep is at least partly linked to the dopaminergic system in iRBD and PD. However, further studies are needed to elucidate possible mechanisms and pathways.
METHODS
Subjects
We included 10 iRBD patients, 10 PD patients with RBD, 10 PD patients without RBD, and 10 healthy. IRBD patients were diagnosed according to the International Classification of Sleep Disorders, 2nd Edition (ICSD-2), and PD patients were diagnosed according to the UK Parkinson Disease Society Brain Bank criteria. Sleep was scored according to the American Academy of Sleep Medicine (AASM) 2007 criteria. All participants had their history taken and were assessed with the Stiasny-Kolster RBD-scale,12 Beck Depression Inventory (BDI),13 and the non-motor symptom scale (NMSS).14 The diagnosis of RBD was based on the ICSD-2. The polysomnography (PSG) results for all participants were evaluated for the diagnosis RBD or no-RBD by a specialist in sleep medicine, who was blinded to diagnosis and other clinical variables of the patients. Exclusion criteria for patients and controls were: (1) a history of psychiatric disorder, (2) other neurological disorders, (3) epilepsy, (4) abuse of alcohol and drugs, (5) family history of mental illness in first-degree relatives, (6) head trauma, and (7) a history of a relevant clinical sleep disorder (apart from RBD), as sleepwalking, confusional arousals, night terrors, narcolepsy, or untreated sleep-disordered breathing, as shown by PSG recording. A further exclusion criteria for healthy controls was a score ≥ 5 on the RBD screening questionnaire.12 Patients with iRBD and controls had no current (or past) use of any central nervous system medication. PD patients were treated with anti-Parkinson medication, but they did not receive treatment with clonazepam, melatonin, antidepressants, or antipsychotics. We calculated the Levodopa equivalence dose (LED) according to recommendations by Tomlinson et al.15 All participants underwent polysomnography, 123I-FPCIT SPECT, physical and neurological examinations, and routine blood analysis. SPECT-scans were performed within 18 months before or after the PSG. Demographic information and medication status are shown in Table 1. All patients were included after they had given oral and written informed consent. The study was approved by the local ethical committee (reference code: H-A-2007-0120).
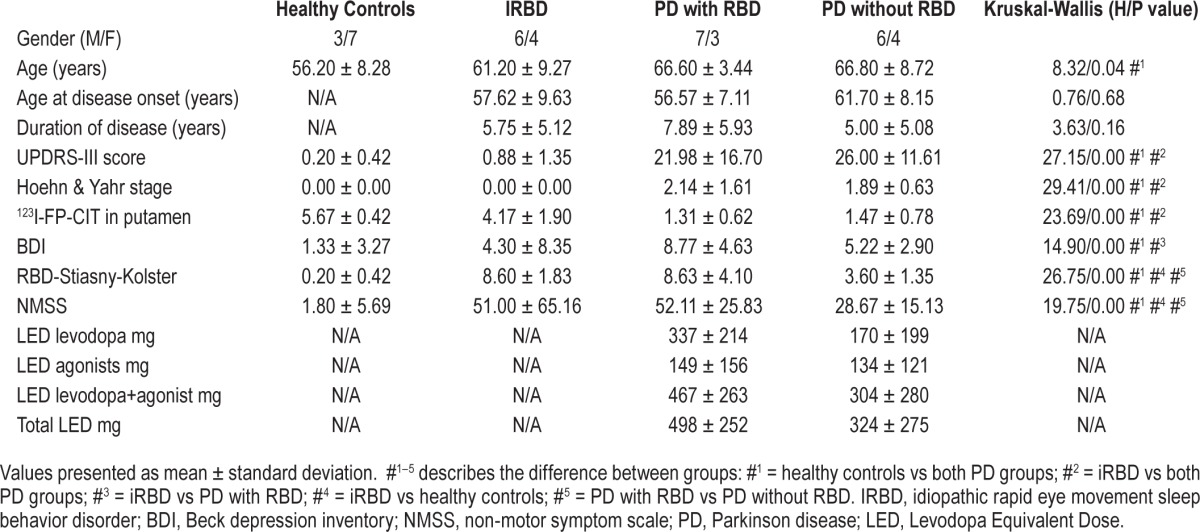
Table 1.
Demographic and clinical data.
Polysomnography
All subjects underwent one night of PSG, which were scored in accordance to AASM 2007 criteria.16 All recordings included at least 6 leads of EEG (F3-A2, F4-A1, C3-A2, C4-A1, O1-A2, O2-A1), surface EMG recordings from the mentalis and bilateral anterior tibialis, ECG and vertical and horizontal EOG. Impedances were kept < 10 kΩ. Respiration was monitored using a nasal cannula and with thoracic and abdominal strain gauges, whereas blood oxygen saturation was continuously recorded by cutaneous finger pulse oximetry. The apnea-hypopnea index (AHI) was defined as the average number of apneas and hypopneas per hour of sleep. Patients were excluded when they had an AHI > 5. Two iRBD patients were originally diagnosed with concomitant sleep apnea and were re-assessed with PSG with continuous positive airway pressure (CPAP). When reassessed with CPAP the AHI dropped below 5, but their excessive motor activity during REM sleep persisted. None of the controls or PD patients included in the study had diagnosed sleep apnea. The onset of REM sleep was based on the occur-rence of the first REM, as REM sleep in RBD cannot be scored on the basis of chin EMG. PLMS were scored according to AASM 2007 criteria.
Detection and Analysis of EMG Activity
The signals were recorded with the standard EEG system (Nervus, Nicolet) and exported to EMG viewer via the EDF file format. EMG-viewer is an analysis tool, based on MATLAB, developed in-house. The sampling frequency was 256 Hz. Surface EMG recordings were made from the mentalis muscle and bilateral from the anterior tibialis. The EMG activity was analyzed in the channels at an amplitude scale of 30 microvolt/cm and time scale of 30 s/screen on a 24-inch LCD screen. A band pass filter with 3 dB cut frequencies at 10 Hz and 100 Hz and a 50 Hz Notch filter was used for the EMG signals to reduce artefacts and noise. In addition, we used a 2nd-order low-pass Butterworth IIR filter with a 3 dB cut frequency at 20 Hz.
Signal segments with a length of 5 s including artifacts and increase in EMG activity due to respiratory-related arousals or events were excluded from further EMG-analysis. For easier discrimination between muscle activity and baseline the EMG signal was rectified and low pass filtered (rlpEMG). The baseline was estimated separately for each sleep segment by dividing the rlpEMG signal into 5-s intervals and finding the intervals with the lowest activity calculated as the lowest root mean square (RMS) value. A detection threshold of 4 times the estimated baseline was used to detect motor activity. Muscle activity was defined as: a duration > 0.1 s, an amplitude exceeding 4 times the root mean square, based on the lowest 5-s baseline in a given consecutive sleep stage following the hypnogram. The end of each EMG-burst was defined as an identifiable return below threshold (less than 4 RMS cutoff line) for longer than 250 ms.
In all groups each EMG channel, the chin and tibialis muscle, was scored separately according to the hypnogram derived from the original sleep-assessment. In PD patients we analyzed EMG-activity of the tibialis muscle in the most affected body-side, contralateral to the most affected hemisphere, e.g., the hemisphere with the most reduced putamen function measured with 123I-FP-CIT brain SPECT scans. Therefore, EMG activity of only one leg per patient was included for statistical analysis. In PD patients with RBD 4 of the 10 patients had lowest uptake in the left putamen, while in PD patients without RBD 9 of 10 patients had lowest uptake in the left putamen.
In iRBD patients we observed significant asymmetries between left and right putamen (p < 0.001), with less 123I-FP-CIT uptake in the left putamen. Therefore, in the iRBD group only EMG activity from the right tibialis muscle was included for statistical analysis. EMG activity in the right tibialis muscle of iRBD patients was then compared to EMG activity in the right tibialis muscle of healthy controls. With regard to iRBD 8 of 10 patients had lowest uptake in the left putamen, while 9 out of 10 healthy controls had lowest uptake in the left putamen.
After scoring of the EMG activity, all separate REM periods were added into one total REM sleep stage. We repeated this procedure for the NREM sleep stage, resulting in a total NREM sleep stage, adding all N1, N2 and N3. Then the percentage of time with increased EMG activity in REM and NREM sleep was measured.
Periodic leg movements were scored in REM and NREM sleep according to AASM 2007 criteria.16 PLMS were distinguished from phasic EMG activity by their characteristic periodic appearance, and they were excluded from quantitative analysis.
123I-FP-CIT Brain SPECT
123I-FP-CIT brain SPECT scans were carried out with a Prism 3000XP (Picker/Phillips) triple-headed gamma camera equipped with low energy, ultra-high-resolution fan-beam collimators. SPECT scans were performed according to guidelines.17 The SPECT-scanning started exactly 3 hours after patients had received an intravenous injection of 185 MBq 123I-FP-CIT, when a steady state of tracer concentration in the striatum was obtained. For details on the SPECT protocol, please see previous study.18 Dopamine transporter SPECT scans were analysed with an automatic 3D quantification tool (Exini DAT, EXINI Diagnostics AB, Lund, Sweden). The quantification module automatically calculates specific uptake in: striatum, putamen, and nucleus caudatus for the patient's brain images. The cerebral cortex has been delineated as background region. This article focussed on the uptake in the putamen region, as this part of the striatum has been associated with motor function.
Statistical Analysis
Kruskal-Wallis analysis of variance was used to evaluate group differences. Post hoc analyses were conducted using the Mann-Whitney U test. Correlations between 123I-FP-CIT up-take and percentage EMG activity during REM and NREM were evaluated using Kendall tau. Furthermore, the sleep parameters duration of REM sleep and total sleep time was analysed with ANCOVA with age and H&Y when appropriate. The Statistical Package for the Social Sciences (SPSS version 17.0) was used for statistical analyses. Results are reported as the mean ± SD unless otherwise stated. P values ≤ 0.05 were considered statistically significant.
RESULTS
Data on clinical characteristics and of the patient groups are presented in Table 1.
Kruskal-Wallis analysis of variance showed significant difference between groups in age (H = 8.32, p = 0.040), UPDRS (H = 27.15, p < 0.001), H&Y score (H = 29.41, p < 0.001), BDI (H = 14.90, p = 0.002), RBD Stiasny-Kolster (H = 26.75, p < 0.001), and the NMSS (H = 19.75, p < 0.001). Post hoc analysis showed that healthy controls were significantly younger than PD patients with RBD (U = 12.50, Z = −2.853, p = 0.004) and PD patients without RBD (U = 20.50, Z = −2.004, p = 0.045). As expected UPDRS scores were significantly lower in healthy controls compared to both PD patients with RBD (U = 0.00, Z = −3.823, p < 0.001) and PD patients without RBD (U = 0.00, Z = −3.723, p < 0.001), and also lower in iRBD patients compared to both PD patients with RBD (U = 0.00, Z = −3.499, p < 0.001) and PD patients without RBD (U = 0.00, Z = −3.398, p < 0.001). Furthermore, H&Y scores were significantly lower in healthy controls compared to both PD patients with RBD (U = 5.00, Z = −3.640, p < 0.001) and PD patients without RBD (U = 0.00, Z = −3.907, p < 0.001), and lower in iRBD patients compared to both PD patients with RBD (U = 5.00, Z = −3.640, p < 0.001) and PD patients without RBD (U = 0.00, Z = −3.907, p < 0.001). Moreover, PD patients with RBD had significantly higher BDI scores than iRBD patients (U = 18.00, Z = −2.241, p = 0.025) and healthy controls (U = 5.00, Z = −3.203, p = 0.001), and the group PD without RBD scored higher on BDI than healthy controls (U = 17.00, Z = −2.087, p = 0.037). The scores on the RBD Stiasny-Kolster scale were significantly lower in healthy controls compared to both PD patients with RBD (U = 6.00, Z = −3.231, p = 0.001) and PD patients without RBD (U = 0.00, Z = −3.839, p < 0.001). As expected, iRBD patients scored much higher on this scale than healthy controls (U = 0.00, Z = −3.926, p < 0.001) and PD without RBD (U = 1.00, Z = −3.634, p < 0.001), and PD patients with RBD had higher scores than PD without RBD (U = 9.00, Z = −2.617, p = 0.009). The NMSS scores were lower in healthy controls compared to both PD patients with RBD (U = 0.00, Z = −3.586, p < 0.001) and PD patients with -out RBD (U = 2.00, Z = −3.607, p < 0.001). Moreover, iRBD patients scored significantly higher on the NMSS than healthy controls (U = 10.50, Z = −3.193, p = 0.001), whereas PD patients with RBD scored significantly higher on the NMSS than PD patients without RBD (U = 4.50, Z = −2.520. p = 0.012) and healthy controls (U = 6.00, Z = −3.231, p = 0.001).
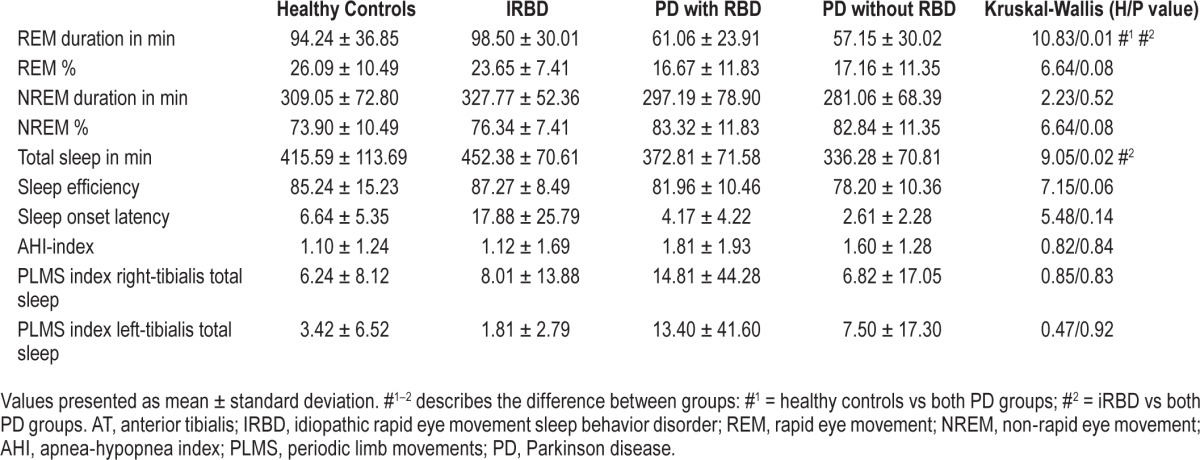
Group Comparisons with Regard to PSG Data
The sleep parameters for the groups are presented in Table 2. We found group differences for the sleep parameters “REM duration in min” (H = 10.83, p = 0.013) and “Total sleep in min” (H = 9.05, p = 0.029). Post hoc tests showed that iRBD patients had significantly more REM sleep than PD patients with RBD (U = 18.00, Z = −2.420, p = 0.016) and PD patients without RBD (U = 14.00, Z = −2.533, p = 0.011). In addition, healthy controls had more REM sleep than both PD-groups (healthy vs PD with RBD: U = 22.00, Z = −2.117, p = 0.034; healthy vs PD without RBD: U = 20.00, Z = −2.043, p = 0.041). IRBD patients had more total sleep time compared to both PD-groups (iRBD vs PD with RBD: U = 16.00, Z = −2.368, p = 0.018; iRBD vs PD without RBD: U = 12.00, Z = −2.694, p = 0.007). The sleep parameters did not differ between the two PD groups and were similar between healthy controls and iRBD patients.
Table 2.
Polysomnographic data.
Comparison of EMG Activity (%) in REM and NREM Sleep Stages between Patient Groups
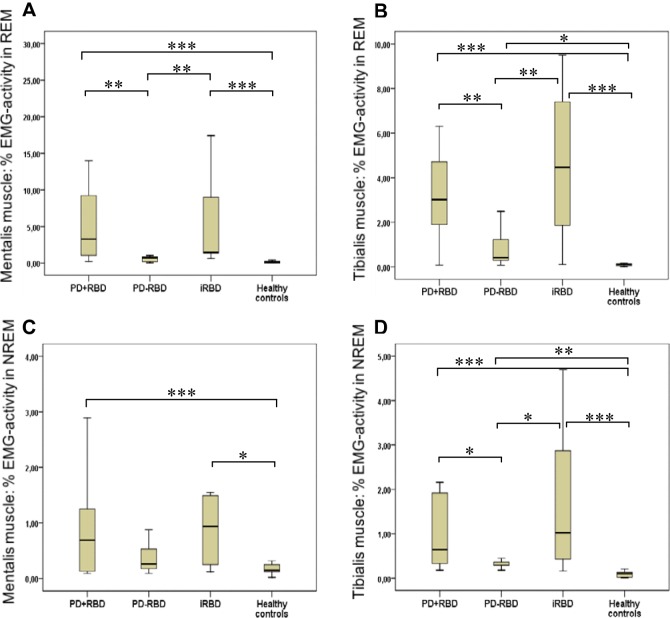
Then we evaluated whether the percentage of EMG-activity during REM and NREM sleep differed between groups. Kruskal-Wallis analysis of variance showed significant group differences between percentage of EMG-activity during REM sleep for mentalis muscle (H = 19.87, p < 0.001) and tibialis muscle (H = 20.33, p < 0.001). Group differences were also found during NREM sleep for tibialis muscle (H = 21.38, p < 0.001), with a trend for mentalis muscle (H = 7.09, p = 0.069). Post hoc analyses between groups are presented in Figure 1.
Figure 1. % EMG-activity during REM and NREM sleep between groups.
PD+RBD means PD with RBD; PD-RBD means PD without RBD. *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001. IRBD, idiopathic rapid eye movement sleep behavior disorder; REM, rapid eye movement; NREM, non-rapid eye movement; PD, Parkinson disease.
Comparison of 123I-FP-CIT Uptake between Patient Groups
In iRBD patients we observed significant asymmetries between left and right putamen (p < 0.001), with less 123I-FP-CIT uptake in the left putamen. We did not observe differences in uptake between hemispheres in healthy controls. Therefore, we compared 123I-FP-CIT uptake in the left putamen between iRBD patients and healthy controls. In PD patients we looked at the hemisphere (putamen-region) contralateral to the most affected body-side, which we denoted the dominant hemisphere. Afterwards, we compared 123I-FP-CIT uptake between patient-groups (H = 23.69, p < 0.001), and found that iRBD patients had significant lower 123I-FP-CIT uptake in the left putamen (U = 24.00, Z = −1.965, p = 0.049) compared to healthy controls. As expected, iRBD patients had significant higher 123I-FP-CIT uptake than PD patients with RBD (U = 10.00, Z = −3.024, p = 0.002) and without RBD (U = 12.00, Z = −2.694, p = 0.007). We did not find differences in 123I-FP-CIT uptake between PD patients with and without RBD, see Table 1.
Relation between 123I-FP-CIT Uptake and EMG Activity during REM and NREM in iRBD
Subsequently, we evaluated the relationship between 123I-FPCIT uptake in the left putamen and the percentage of EMG activity during REM and NREM sleep in iRBD. During REM sleep, we found significant and inverse correlations between 123I-FP-CIT uptake in the left putamen and the percentage of EMG activity in the mentalis muscle (r = −0.556, p = 0.019), but not with EMG-activity in the right tibialis muscle (r = −0.056, p = 0.417). In NREM sleep, we found trends toward significant inverse correlations between 123I-FP-CIT binding in the left putamen and EMG activity in the mentalis muscle (r = −0.389, p = 0.072) and right tibialis muscle (r = −0.333, p = 0.090).
Relation between 123I-FP-CIT Uptake and EMG Activity in PD with and without RBD
In PD patients with or without RBD the correlations between 123I-FP-CIT uptake in the putamen region and EMG activity in mentalis and tibialis muscle during REM sleep were nonsignificant. During NREM sleep, we found significant inverse correlations between 123I-FP-CIT binding in the putamen and EMG-activity in the mentalis muscle (r = −0.611, p = 0.011) and tibialis muscle (r = −0.611, p = 0.011) in PD patients with RBD. In addition, the EMG-activity in the tibialis muscle was inversely correlated with 123I-FP-CIT binding in the putamen (r = −0.530, p = 0.027) in PD patients without RBD. No significant correlations were found between 123I-FP-CIT uptake for mentalis muscle.
Relation between EMG Activity and Levodopa Equivalent Dose (LED) in PD with and without RBD
To evaluate the relation between EMG activity and dopaminergic treatment, we analysed the association between EMG-activity and LED in PD patients with and without RBD, during REM and NREM sleep.
In PD patients with RBD, we found that EMG activity during REM sleep in the tibialis muscle was significantly and inversely correlated to treatment with dopamine agonists alone (r = −0.582, p = 0.011), with combined levodopa and dopamine agonist treatment (r = −0.598, p = 0.009), and total LED (r = −0.704, p = 0.004). A multiple regression analysis was performed to evaluate the relation between EMG activity during REM sleep in the tibialis muscle and factors suspected to influence this activity. The variables included in the model were age, REM sleep duration, and treatment with dopamine agonists alone, with combined levodopa and dopamine agonist treatment, and total LED. The variables disease duration, UPDRS and H&Y were not correlated with EMG activity in the tibialis muscle during REM sleep. The final linear regression model using the stepwise exclusion method showed that total LED was the only explaining variable (Beta = −0.842; p = 0.004). The overall model fit (R2) was 0.709. These results suggest that dopamine may be linked to the percentage of EMG-activity during REM sleep.
In PD patients without RBD, we found significant and inverse correlations between treatment with dopamine agonists and EMG activity during REM sleep in the mentalis muscle (r = −0.551, p = 0.022) and the tibialis muscle (r = −0.530, p = 0.028). The correlations between dopaminergic treatment and EMG-activity during NREM were all nonsignificant.
DISCUSSION
In this study we investigated the relation between increased nighttime motor activity during REM and NREM sleep and the midbrain dopaminergic system in patients with iRBD and PD. As expected, the iRBD patients and PD patients with RBD had higher EMG activity during REM sleep in mentalis muscle and tibialis muscle than PD patients without RBD and healthy controls. In addition, iRBD patients also showed increased EMG activity during NREM sleep in the mentalis muscle and tibialis muscle compared to healthy controls and PD patients without RBD. A similar pattern was seen for PD patients with RBD, who had significantly increased EMG activity in the tibialis muscle during NREM sleep compared to PD patients without RBD. Most studies on RBD have mainly focused on measuring EMG activity during REM sleep,19–21 and to our knowledge no other studies have addressed EMG activity during NREM sleep in patients with iRBD and Parkinson disease. The increase of EMG activity during both REM and NREM sleep may suggest a general instability of mechanisms regulating atonia, although most pronounced during REM sleep.
Furthermore, iRBD patients had significantly lower 123I-FPCIT uptake in the left putamen compared to healthy controls, and higher uptake compared to both PD groups. This is in line with previous studies showing a reduction in 123I-FP-CIT up-take in the striatum in iRBD and PD with disease progression.8 We analyzed the relation between EMG-activity during REM sleep and 123I-FP-CIT uptake in iRBD patients, and found a significant and inverse correlation between EMG activity in the mentalis muscle and 123I-FP-CIT binding in the putamen. These results are in agreement with a study by Eisensehr et al., who found that a decreased density of the dopamine transporter in the striatum was associated with increased EMG activity during REM sleep in iRBD.10
These findings are also in agreement with a study in a marmoset model of PD, which showed that monkeys treated with MPTP had an increased number of sleep epochs with high-amplitude EMG bouts during REM sleep relative to control animals. These monkeys showed a slight increase in phasic activity and an increase in tonic activity as a percentage of total REM sleep.9 Similarly, increased muscle tone during nighttime has also been reported in the macaque treated with MPTP. This increase in muscle tone was characterized by the occurrence of high-amplitude EMG bouts during both REM and NREM sleep.22 The high selectivity of MPTP to midbrain dopaminergic neurons23 suggests that the presence of REM sleep without atonia might reflect the early involvement of dopaminergic neurotransmission on pontine and medullary REM sleep-related structures.24
The extent to which the nigrostriatal dopaminergic system contributes to the regulation of REM sleep and RBD needs to be confirmed in more extensive studies. In our study PD patients with and without RBD did not differ with regard to 123I-FP-CIT binding in the putamen, and no relation was found between 123I-FP-CIT binding and EMG-activity during REM sleep in both groups. These results would suggest that the nigrostriatal dopaminergic dysfunction in PD does not play a prominent role in EMG activity seen during REM sleep. However, these findings do not disconfirm a possible role for dopa-mine in RBD. Subsequently, we analyzed possible effects of dopaminergic treatment on EMG activity during REM sleep. In PD patients with RBD we found significant and inverse correlations between EMG activity in the tibialis muscle and treatment with dopamine agonists alone, combined treatment with levodopa and dopamine agonists, and most pronounced with total LED. In PD patients without RBD, we also found significant inverse correlations between treatment with dopa-mine agonists and EMG activity during REM sleep in the mentalis muscle and the tibialis muscle. These results suggest that dopaminergic medication may have an effect on EMG activity during REM sleep. According to the Best Practice Guide for the Treatment of REM Sleep Behavior Disorder (RBD),25 there are limited data on dopaminergic treatment effects of RBD.26–28 Therefore, the extent to which dopamine plays a role in sleep and RBD needs to be investigated in future studies.
Neuropathological studies have reported that the degenerative process in the PD brain starts in the medulla, advances to the pons, and subsequently targets the midbrain.29 As REM atonia is mediated by nuclei in the medulla24 it is suggested that RBD reflects involvement of non-dopaminergic pontine and medullary structures. However, these structures are closely connected to the midbrain dopaminergic pathways, and may therefore be affected by an imbalance of dopamine levels.30 The retrorubral nucleus (RRN, also called A8) is an area with dopamine-containing neurons that forms a bridge between the substantia nigra (A9) and ventral tegmental area (A10).31 The RRN projects to the pontine inhibitory area32 as well as to the pedunculopontine nucleus,33 and stimulation of the RRN produces bilateral suppression of muscle tone.30 Both the RRN and its dopamine transporter-positive fibers in the brainstem (pedunculopontine and cuneiform nucleus) is severely affected by MPTP.23,33 Furthermore, Takakusaki et al. showed that the excessive GABAergic output from the basal ganglia to the PPN in patients with PD may induce sleep disturbances, including a reduction of REM sleep periods and REM sleep behavioral disorders as REM without atonia.5 Studies in MPTP-treated rats, cats, and monkeys have also reported a role for dopaminergic neurons in the substantia nigra in the regulation of REM sleep,3,4,34,35 In addition, dopamine D2-receptor immunoreactivity has been found in brainstem structures involved in REM sleep without atonia, including subcoeruleus, lateral paragigantocellular, nucleus raphe magnus, gigantocellular nucleus pars alpha, ventral gigantocellular nucleus, and raphe obscurus.33,36
We found significant inverse correlations between 123I-FPCIT uptake and non-periodic EMG activity in the mentalis and tibialis muscle in PD patients with RBD during NREM sleep. In addition, in PD patients without RBD 123I-FP-CIT uptake was also inversely correlated to EMG activity in the tibialis muscle. This may suggest that the nigrostriatal dopaminergic system may be involved in EMG activity during NREM sleep. The involvement of the dopaminergic system in periodic limb movements is well known,37 and reduced striatal 123I-beta-CIT binding has been associated with an increased number of PLMS in PD.38 However, this system may also be involved in nonperiodic motor activity during NREM.
Furthermore, iRBD patients and PD patients with RBD scored significantly higher on the NMSS, and therefore reported a higher prevalence of more non-motor symptoms than the healthy controls and PD patients without RBD. Previous studies have shown that iRBD is associated with an increased prevalence of non-motor symptoms, and that RBD is a signifi-cant predictor of increased non-motor symptoms in PD.39,40 The non-motor symptoms include autonomic dysfunction, depressive symptoms, sleep disturbances, and fatigue.41 Although these non-motor symptoms may occur in the premotor stage of PD, this does not necessarily preclude an involvement of dopaminergic degeneration in the development of non-motor symptoms. For instance, the dorsal motor nucleus of vagus, a medullary autonomic nucleus, and a structure very early affected in the course of Parkinson disease, shows a wide distribution of dopamine D1 and D2 receptors in the cholinergic and catecholaminergic neurons in the DMV of rats.42
A baseline was calculated separately for each consecutive sleep stage to control for possible differences in muscle tone during the sleep period. Previous studies have shown that the mean tonic level of mentalis muscle is significantly decreased in REM sleep compared to NREM sleep.43,44 Within NREM episodes the tonic EMG level seems to vary systematically, as the EMG level decreases during the first NREM episode, while the EMG level in other NREM episodes show an increasing trend.43,44 As such, our method deviate from previous studies measuring EMG activity only during REM sleep.19–21 Mont-plaisir et al. established cutoff values for EMG activity during REM sleep for a diagnosis of RBD ≥ 30% for tonic activity or ≥ 15% for phasic activity. These authors used 20-s epochs for scoring tonic activity and 2-s mini-epochs for phasic activity. The threshold for counting motor activity was two times baseline or 10πV.45 A study by Frauscher et al. concluded that the most sensitive method for discriminating iRBD patients from healthy controls was to include “any” muscle activity in the EMG analysis.42 These authors used 30-s epochs for tonic activity and 3-s mini epochs for phasic activity. In our method we did not distinguish between phasic and tonic activity, but included “any” type of EMG activity. However, we did not use 30-s epochs and 3-s epochs. In our study, EMG activity was scored when the duration was > 0.1 s and the amplitude exceeded 4 times the root mean square. Furthermore, the end of each EMG burst was defined as an identifiable return below threshold (< 4 RMS cutoff line) for longer than 250 ms, a parameter which was also applied in the study by Frauscher et al.46
Our methods have some limitations. Manual scoring is time consuming and therefore development of an automatic algorithm for the use of scoring EMG activity during the entire sleep period would be recommended. In addition, we did not evaluate the sensitivity of the baseline before scoring and analyzing the EMG activity. Our group has recently published a study with the aim of finding the most sensitive baseline for measuring EMG activity during REM sleep.47 However, such a baseline should also be developed when analyzing the whole sleep period, taking into account possible changes in muscular tone across the sleep stages.
In summary, the present study shows that increased EMG activity during REM sleep may be linked with degeneration of the midbrain dopaminergic system in iRBD and possibly to dopaminergic treatment in Parkinson disease. Dopaminergic receptors are scattered throughout the brainstem and are observed both in structures mediating REM atonia36 and in the dorsal vagal nucleus,42 one of the first structures affected in the brain in Parkinson disease.29 Although this suggests that dopamine may play a role in the preclinical PD disease stage, the possible involvement of dopamine in REM atonia needs to be addressed in further studies.
DISCLOSURE STATEMENT
The study is supported by the Lundbeck Foundation, the National Foundation for Parkinson's Disease and the Toyota Foundation. These foundations had no role in the study design, the collection, analysis and interpretation of data, the writing of the report, or the decision to submit the paper for publication. The authors have indicated no financial conflicts of interest. The work was performed at Bispebjerg Hospital, Copenhagen, Denmark, Glostrup Hospital, Copenhagen, Denmark, and Bispebjerg University Hospital, Copenhagen, Denmark.
ABBREVIATIONS
- AASM
American Academy of Sleep Medicine
- AHI
apnea-hypopnea index
- BDI
Beck depression inventory
- CPAP
continuous positive airway pressure
- EMG
electromyography
- H&Y
Hoehn and Yahr score
- ICSD
International Classification of Sleep Disorders
- 123I-FP-CIT SPECT
(123)I-N-omega-fluoropropyl-2-beta-carboxymethoxy-3beta-(4-iodophenyl) nortropane ((123) I-FP-CIT) Single-photon emission computed tomography (SPECT) scanning
- iRBD
idiopathic rapid eye movement sleep behavior disorder
- LED
Levodopa equivalence dose
- MPTP
1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine hydrochloride
- NMSS
non motor symptom scale
- NREM
non rapid eye movements
- PD
Parkinson's disease
- PLMS
periodic limb movements
- PSG
polysomnography
- RBD
rapid eye movement sleep behavior disorder
- REM
rapid eye movement
- UPDRS
unified Parkinson's disease rating scale
REFERENCES
- 1.Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a parkinsonian disorder or dementia in 81% of older males initially diagnosed with idiopathic REM sleep behavior disorder (RBD): 16 year update on a previously reported series. Sleep Med. 2013;14:744–8. doi: 10.1016/j.sleep.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 2.Iranzo A, Fernandez-Arcos A, Tolosa E, et al. Neurodegenerative disorder risk in idiopathic REM sleep behavior disorder: study in 174 patients. PLoS One. 2014;9:e89741. doi: 10.1371/journal.pone.0089741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lima MM, Andersen ML, Reksidler AB, et al. The role of the substantia nigra pars compacta in regulating sleep patterns in rats. PLoS One. 2007;2:e513. doi: 10.1371/journal.pone.0000513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lima MM. Sleep disturbances in Parkinson's disease: the contribution of dopamine in REM sleep regulation. Sleep Med Rev. 2013;17:367–75. doi: 10.1016/j.smrv.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 5.Takakusaki K, Saitoh K, Harada H, et al. Evidence for a role of basal ganglia in the regulation of rapid eye movement sleep by electrical and chemical stimulation for the pedunculopontine tegmental nucleus and the substantia nigra pars reticulata in decerebrate cats. Neuroscience. 2004;124:207–20. doi: 10.1016/j.neuroscience.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 6.Unger MM, Belke M, Menzler K, et al. Diffusion tensor imaging in idiopathic REM sleep behavior disorder reveals microstructural changes in the brainstem, substantia nigra, olfactory region, and other brain regions. Sleep. 2010;33:767–73. doi: 10.1093/sleep/33.6.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ellmore TM, Hood AJ, Castriotta RJ, et al. Reduced volume of the putamen in REM sleep behavior disorder patients. Parkinsonism Relat Disord. 2010;16:645–9. doi: 10.1016/j.parkreldis.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 8.Iranzo A, Valldeoriola F, Lomena F, et al. Serial dopamine transporter imaging of nigrostriatal function in patients with idiopathic rapid-eye-movement sleep behaviour disorder: a prospective study. Lancet Neurol. 2011;10:797–805. doi: 10.1016/S1474-4422(11)70152-1. [DOI] [PubMed] [Google Scholar]
- 9.Verhave PS, Jongsma MJ, Van den Berg RM, et al. REM sleep behavior disorder in the marmoset MPTP model of early Parkinson disease. Sleep. 2011;34:1119–25. doi: 10.5665/SLEEP.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eisensehr I, Linke R, Tatsch K, et al. Increased muscle activity during rapid eye movement sleep correlates with decrease of striatal presynaptic dopamine transporters. IPT and IBZM SPECT imaging in subclinical and clinically manifest idiopathic REM sleep behavior disorder, Parkinson's disease, and controls. Sleep. 2003;26:507–12. doi: 10.1093/sleep/26.5.507. [DOI] [PubMed] [Google Scholar]
- 11.Kim YK, Yoon IY, Kim JM, et al. The implication of nigrostriatal dopaminergic degeneration in the pathogenesis of REM sleep behavior disorder. Eur J Neurol. 2010;17:487–92. doi: 10.1111/j.1468-1331.2009.02854.x. [DOI] [PubMed] [Google Scholar]
- 12.Stiasny-Kolster K, Mayer G, Schafer S, et al. The REM sleep behavior disorder screening questionnaire--a new diagnostic instrument. Mov Disord. 2007;22:2386–93. doi: 10.1002/mds.21740. [DOI] [PubMed] [Google Scholar]
- 13.Beck AT, WARD CH, MENDELSON M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 14.Chaudhuri KR, Martinez-Martin P, Brown RG, et al. The metric properties of a novel non-motor symptoms scale for Parkinson's disease: results from an international pilot study. Mov Disord. 2007;22:1901–11. doi: 10.1002/mds.21596. [DOI] [PubMed] [Google Scholar]
- 15.Tomlinson CL, Stowe R, Patel S, et al. Systematic review of levodopa dose equivalency reporting in Parkinson's disease. Mov Disord. 2010;25:2649–53. doi: 10.1002/mds.23429. [DOI] [PubMed] [Google Scholar]
- 16.Iber C, Ancoli-Israel S, Chesson AL, et al. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. [Google Scholar]
- 17.Darcourt J, Booij J, Tatsch K, et al. EANM procedure guidelines for brain neurotransmission SPECT using (123)I-labelled dopamine transporter ligands, version 2. Eur J Nucl Med Mol Imaging. 2010;37:443–50. doi: 10.1007/s00259-009-1267-x. [DOI] [PubMed] [Google Scholar]
- 18.Lokkegaard A, Werdelin LM, Regeur L, et al. Dopamine transporter imaging and the effects of deep brain stimulation in patients with Parkinson's disease. Eur J Nucl Med Mol Imaging. 2007;34:508–16. doi: 10.1007/s00259-006-0257-5. [DOI] [PubMed] [Google Scholar]
- 19.Frauscher B, Iranzo A, Hogl B, et al. Quantification of electromyographic activity during REM sleep in multiple muscles in REM sleep behavior disorder. Sleep. 2008;31:724–31. doi: 10.1093/sleep/31.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iranzo A, Frauscher B, Santos H, et al. Usefulness of the SINBAR electromyographic montage to detect the motor and vocal manifestations occurring in REM sleep behavior disorder. Sleep Med. 2011;12:284–8. doi: 10.1016/j.sleep.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 21.Mayer G, Kesper K, Ploch T, et al. Quantification of tonic and phasic muscle activity in REM sleep behavior disorder. J Clin Neurophysiol. 2008;25:48–55. doi: 10.1097/WNP.0b013e318162acd7. [DOI] [PubMed] [Google Scholar]
- 22.Belaid H, Adrien J, Laffrat E, et al. Sleep disorders in Parkinsonian macaques: effects of L-dopa treatment and pedunculopontine nucleus lesion. J Neurosci. 2014;34:9124–33. doi: 10.1523/JNEUROSCI.0181-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.German DC, Manaye KF, Sonsalla PK, et al. Midbrain dopaminergic cell loss in Parkinson's disease and MPTP-induced parkinsonism: sparing of calbindin-D28k-containing cells. Ann N Y Acad Sci. 1992;648:42–62. doi: 10.1111/j.1749-6632.1992.tb24523.x. [DOI] [PubMed] [Google Scholar]
- 24.Luppi PH, Clement O, Fort P. Paradoxical (REM) sleep genesis by the brainstem is under hypothalamic control. Curr Opin Neurobiol. 2013;23:786–92. doi: 10.1016/j.conb.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 25.Aurora RN, Zak RS, Maganti RK, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD) J Clin Sleep Med. 2010;6:85–95. [PMC free article] [PubMed] [Google Scholar]
- 26.Sasai T, Matsuura M, Inoue Y. Factors associated with the effect of pramipexole on symptoms of idiopathic REM sleep behavior disorder. Parkinsonism Relat Disord. 2013;19:153–7. doi: 10.1016/j.parkreldis.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 27.Kumru H, Iranzo A, Carrasco E, et al. Lack of effects of pramipexole on REM sleep behavior disorder in Parkinson disease. Sleep. 2008;31:1418–21. [PMC free article] [PubMed] [Google Scholar]
- 28.Schmidt MH, Koshal VB, Schmidt HS. Use of pramipexole in REM sleep behavior disorder: results from a case series. Sleep Med. 2006;7:418–23. doi: 10.1016/j.sleep.2006.03.018. [DOI] [PubMed] [Google Scholar]
- 29.Braak H, Del TK, Rub U, et al. Staging of brain pathology related to sporadic Parkinson's disease. Neurobiol Aging. 2003;24:197–211. doi: 10.1016/s0197-4580(02)00065-9. [DOI] [PubMed] [Google Scholar]
- 30.Lai YY, Siegel JM. Muscle tone suppression and stepping produced by stimulation of midbrain and rostral pontine reticular formation. J Neurosci. 1990;10:2727–34. doi: 10.1523/JNEUROSCI.10-08-02727.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deutch AY, Goldstein M, Baldino F, Jr., et al. Telencephalic projections of the A8 dopamine cell group. Ann N Y Acad Sci. 1988;537:27–50. doi: 10.1111/j.1749-6632.1988.tb42095.x. [DOI] [PubMed] [Google Scholar]
- 32.Lai YY, Clements JR, Siegel JM. Glutamatergic and cholinergic projections to the pontine inhibitory area identified with horseradish peroxidase retrograde transport and immunohistochemistry. J Comp Neurol. 1993;336:321–30. doi: 10.1002/cne.903360302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rolland AS, Tande D, Herrero MT, et al. Evidence for a dopaminergic innervation of the pedunculopontine nucleus in monkeys, and its drastic reduction after MPTP intoxication. J Neurochem. 2009;110:1321–9. doi: 10.1111/j.1471-4159.2009.06220.x. [DOI] [PubMed] [Google Scholar]
- 34.Pungor K, Papp M, Kekesi K, et al. A novel effect of MPTP: the selective suppression of paradoxical sleep in cats. Brain Res. 1990;525:310–4. doi: 10.1016/0006-8993(90)90880-k. [DOI] [PubMed] [Google Scholar]
- 35.Almirall H, Pigarev I, de la Calzada MD, et al. Nocturnal sleep structure and temperature slope in MPTP treated monkeys. J Neural Transm. 1999;106:1125–34. doi: 10.1007/s007020050228. [DOI] [PubMed] [Google Scholar]
- 36.van Dijken H. The dopaminergic innervation of the brain stem and spinal cord: an anatomical study on the distribution of the neurotransmitter dopamine and its D2 receptor. Erasmus University Rotterdam. 2000. http://repub.eur.nl/pub/20986.
- 37.Karatas M. Restless legs syndrome and periodic limb movements during sleep: diagnosis and treatment. Neurologist. 2007;13:294–301. doi: 10.1097/NRL.0b013e3181422589. [DOI] [PubMed] [Google Scholar]
- 38.Happe S, Pirker W, Klosch G, et al. Periodic leg movements in patients with Parkinson's disease are associated with reduced striatal dopamine transporter binding. J Neurol. 2003;250:83–6. doi: 10.1007/s00415-003-0957-8. [DOI] [PubMed] [Google Scholar]
- 39.Neikrug AB, Avanzino JA, Liu L, et al. Parkinson's disease and REM sleep behavior disorder result in increased non-motor symptoms. Sleep Med. 2014;15:959–66. doi: 10.1016/j.sleep.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Howell MJ, Schenck CH. Rapid eye movement sleep behavior disorder and neurodegenerative disease. JAMA Neurol. 2015;72:707–12. doi: 10.1001/jamaneurol.2014.4563. [DOI] [PubMed] [Google Scholar]
- 41.Ferini-Strambi L, Oertel W, Dauvilliers Y, et al. Autonomic symptoms in idiopathic REM behavior disorder: a multicentre case-control study. J Neurol. 2014;261:1112–8. doi: 10.1007/s00415-014-7317-8. [DOI] [PubMed] [Google Scholar]
- 42.Cai QQ, Zheng LF, Fan RF, et al. Distribution of dopamine receptors D1- and D2-immunoreactive neurons in the dorsal motor nucleus of vagus in rats. Auton Neurosci. 2013;176:48–53. doi: 10.1016/j.autneu.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 43.Brunner DP, Dijk DJ, Borbely AA. A quantitative analysis of phasic and tonic submental EMG activity in human sleep. Physiol Behav. 1990;48:741–8. doi: 10.1016/0031-9384(90)90219-t. [DOI] [PubMed] [Google Scholar]
- 44.Bliwise D, Coleman R, Bergmann B, et al. Facial muscle tonus during REM and NREM sleep. Psychophysiology. 1974;11:497–508. doi: 10.1111/j.1469-8986.1974.tb00578.x. [DOI] [PubMed] [Google Scholar]
- 45.Montplaisir J, Gagnon JF, Fantini ML, et al. Polysomnographic diagnosis of idiopathic REM sleep behavior disorder. Mov Disord. 2010;25:2044–51. doi: 10.1002/mds.23257. [DOI] [PubMed] [Google Scholar]
- 46.Frauscher B, Iranzo A, Gaig C, et al. Normative EMG values during REM sleep for the diagnosis of REM sleep behavior disorder. Sleep. 2012;35:835–47. doi: 10.5665/sleep.1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Frandsen R, Nikolic M, Zoetmulder M, Kempfner L, Jennum P. Analysis of automated quantification of motor activity in REM sleep behaviour disorder. J Sleep Res. 2015;24:583–90. doi: 10.1111/jsr.12304. [DOI] [PubMed] [Google Scholar]