Abstract
Coronary artery ectasia (CAE) often represents a coronary angiography finding casually detected or following the occurrence of an acute coronary syndrome. The pathogenetic role of cocaine abuse in the genesis of CAE is still little known and very few data are available in literature. We describe a case of a 31-year-old male cocaine user admitted to our department for typical acute chest pain. Coronary angiography showed diffuse coronary ectasia with slow flows and without hemodynamically significant stenosis. An increasing of matrix metalloproteinases values and a reduction of their tissue inhibitors was showed both during hospitalization and at one month after discharge. This case report emphasizes the close relationship between cocaine abuse, CAE and acute coronary syndromes in patients without hemodynamically significant coronary stenosis. As reported by Satran et al, cocaine abuse should be considered an important risk factor for CAE and these patients appear to be at increased risk of angina and acute myocardial infarct. Further studies that can strengthen this hypothesis would be useful to deepen and better analyze this interesting association.
Keywords: Coronary artery ectasia, Acute coronary syndromes, Cocaine abuse, Matrix metalloproteinases, Inflammation
Core tip: The pathogenetic role of cocaine abuse in the genesis of coronary artery ectasia (CAE) is still little known and very few data are available in literature. This case report emphasizes the close relationship between cocaine abuse, CAE and acute coronary syndromes in patients without hemodynamically significant coronary stenosis. As reported by Satran et al, cocaine abuse should be considered an important risk factor for CAE and appears to be another potential mechanism of acute coronary syndromes in cocaine users. Further studies that can strengthen this hypothesis would be useful to deepen and better analyze this interesting association.
INTRODUCTION
Coronary artery ectasia (CAE) is a dilation of coronary arteries angiographically defined if the diameter of the artery is at least 1.5 times greater than that of the intact adjacent vascular segment.
Common causes include atherosclerosis, systemic inflammatory disease, systemic vasculitis, genetic connective tissue disorders (Marfan and Ehler-Danlos syndrome) and cocaine abuse.
CAE may have a variable clinical presentation and often represents a coronary angiography finding casually detected or following the occurrence of an atypical chest pain or an acute coronary syndrome. The mechanisms that determine the abnormal dilatation of the vascular lumen are still poorly understood and particularly the overexpression of matrix metalloproteinases (MMPs) has been associated with an excessive expansive arterial remodeling[1].
CASE REPORT
A 31-year-old caucasian man, cocaine user without other cardiovascular risk factors, was admitted to our department for typical acute chest pain started while he was climbing stairs.
At cardiac examination we found a 1/6 Levine systolic murmur at the precordium and blood pressure was 180/90 mmHg. The ECG showed a sinus rhythm with 91 bpm, ST segment depression with T negative waves from V2 to V5 and a corrected QT interval of 493 msec (Figure 1).
Figure 1.
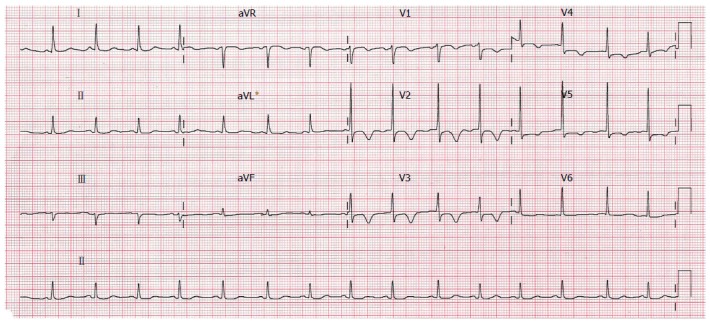
Electrocardiogram at the admission.
Leukocytosis with increasing of inflammatory markers (C-reactive protein 3.2 mg/dL) and positive Troponin I (0.3 ng/mL) were present. Transthoracic echocardiogram showed left ventricular concentric hypertrophy, ejection fraction of 60%, low mitral regurgitation and altered relaxation mitral inflow pattern.
For the persistence of typical chest pain and the high pretest probability of coronary artery disease (CAD) due to cocaine abuse, we choose an invasive diagnostic approach. Percutaneous coronary angiography (performed with 6F diagnostic catheters and right femoral artery access) showed diffuse coronary ectasia without hemodynamically significant stenosis and coronary slow flow with Timi Frame Count score of 2 and a myocardial blush grade 2 (Figure 2). For left coronary artery contrast was injected with a flow rate of 4 mL/s and a volume of 8 mL; for right coronary artery contrast was injected with a flow rate of 3 mL/s and a volume of 6 mL.
Figure 2.
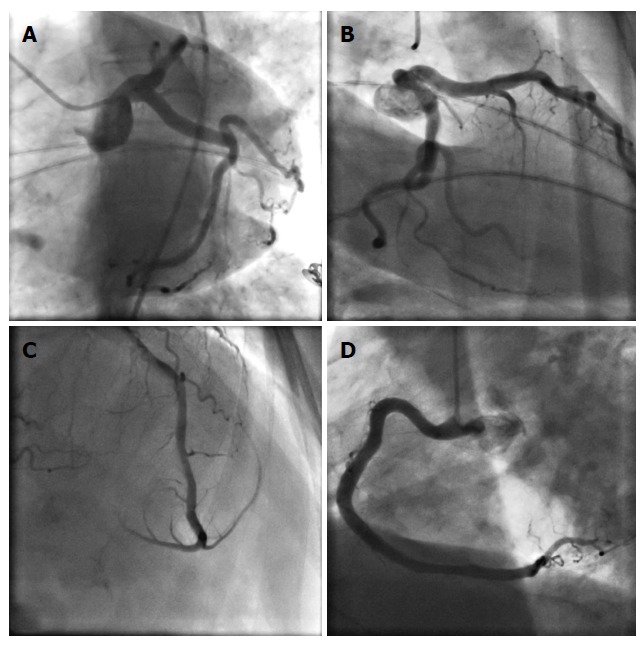
Coronary angiography performed with 6F diagnostic catheters showing ectasia of left anterior descending artery and circumflex coronary artery with maximum diameter of 5.8 mm (A and B), ectasia of medio-distal tract of left anterior descending artery (C), ectasia of right coronary artery with a maximum diameter of 5.6 mm (D).
To exclude a possible role of a coronary spasm in the genesis of the acute coronary syndrome, an hyperventilation testing and an intracoronary injection of acetylcholine (with incremental doses of 20 and 50 μg into the right coronary artery and of 20, 50, and 100 μg into the left coronary artery over 20 s and with at least a 3-min interval between injections) were performed and were negative. Furthermore, to exclude a thrombophilic diathesis, a thrombophilia testing was also performed and was negative.
For the presence of diffuse CAE MMPs plasma concentrations (MMP-2 and MMP-9) and their tissue inhibitors (TIMP-1 and TIMP-2) were also quantified.
An increasing of MMPs values and a reduction of their tissue inhibitors was showed both during hospitalization (MMP-2: 538.9 ng/mL, normal plasma values 125 ± 30 ng/mL; MMP-9: 53.5 ng/mL, normal plasma values 18 ± 6 ng/mL; TIMP-1: 39.2 ng/mL, normal plasma values 356 ± 110 ng/mL; TIMP-2: 26.3 ng/mL, normal plasma values 105 ± 12 ng/mL) and both at one month after discharge (MMP-2: 492.3 ng/mL, MMP-9: 51.7 ng/mL, TIMP-1: 40.5 ng/mL, TIMP-2: 29.1 ng/mL). Because during acute phenomena these values would be physiologically altered, a double assessment was carried out to ensure that values were not affected by the acute event.
Patient was subjected to pharmacological treatment with acetylsalicylic acid, ACE inhibitors, beta-blockers, spironolactone, and statins. Others possible causes of persistent elevated levels of MMP have not been observed one month after discharge.
DISCUSSION
Cocaine is an alkaloid extracted from the leaf of the Erythroxylon coca bush which blocks the presynaptic reuptake of epinephrine, norepinephrine and dopamine, thereby increasing their postsynaptic concentrations and improving sympathetic activity. Cocaine's principal effects on the cardiovascular system are mediated via alpha-adrenergic stimulation with increase in the determinants of myocardial oxygen demand (increasing of heart rate and systemic arterial pressure) and with a concomitant decrease in myocardial oxygen supply caused by vasoconstriction of the epicardial coronary arteries.
Cocaine induced chest pain is a common presentation in emergency departments and premature coronary atherosclerosis with obstructive coronary artery disease often has been seen in young cocaine abusers. Focal occlusive vasospasm, diffuse coronary vasoconstriction, endothelial dysfunction and coronary thrombosis may be responsible for cocaine induced myocardial infarct in patients with normal coronary arteries and cocaine use is also associated with an activation of platelets, leading to increased platelet adhesiveness and aggregation that play a major role in the development of coronary thrombi[2].
Patients with a history of cocaine abuse have also an increased prevalence of CAE. Potential mechanisms that play a major role in the development of CAE may include direct vascular smooth muscle cells apoptosis with media damage, enhanced monocyte migration and endothelium adhesion with hypersecretion of inflammatory cytokines and MMP overexpression with enzymatic degradation and hyalinization of the extracellular matrix. All this effects may cause “chronic vascular stress” (vascular inflammation, arterial remodeling and coronary ectasia) resulting in coronary slow flow and thrombosis[1].
Su et al[3] have demonstrated that cerebral vascular smooth muscle cells can undergo rapid apoptosis in response to cocaine in a concentration-dependent manner, moreover Fiala et al[4] have shown that cocaine in vitro increases the expression of endothelial adhesion molecules, intercellular adhesion molecule-1, vascular cell adhesion molecules-1 and platelet/endothelial cell adhesion molecule-1. Moreover, both in vitro and in vivo, cocaine increases rolling white blood cell flux, leukocyte-endothelium adhesion and mononuclear cells activation with hypersecretion of inflammatory cytokines and overexpression of MMPs with consequent coronary arterial remodeling and ectasia[3,4].
In Demopoulos et al[5] study, history of acute myocardial infarct was reported among 39% of patients with CAE but without CAD and for the authors the presence of ectasic vascular segments would lead to a slow blood flow with greater likelihood of intracoronary thrombosis. In an interesting study Satran et al[6] have demonstrated as patients with a history of cocaine abuse have an increased prevalence of CAE. These patients appear also to be at increased risk of acute myocardial infarct (nearly half the patients in the cocaine group had a history of acute MI despite an average age of 43 years). Therefore CAE appears to be another potential mechanism of acute coronary syndromes in cocaine users[6].
It is known that CAE can be also caused by long lasting hypertension, but it is also known that the cocaine abuse may determines CAE[6]. In our case the patient did not reported to suffer from hypertension and his young age and lack of familiarity for hypertension does not support the hypothesis that CAE may be secondary to a possible hypertension. Moreover to exclude this hypothesis and on the basis of the echocardiography view of concentric hypertrophy we also investigated possible causes of secondary hypertension but all the exams resulted negative. No others conditions (except cocaine abuse) were present to exclude other causes of CAE.
The pathogenetic role of cocaine abuse in the genesis of CAE is still little known and very few data are available in literature. As demonstrated by Satran et al[6], cocaine abuse should be considered an important risk factor for CAE and furthermore these patients appear to be at increased risk of acute coronary syndromes even without hemodynamically significant coronary stenosis.
This case emphasizes the close relationship between cocaine abuse, CAE and acute coronary syndromes in patients without coronary stenosis but, being only a case report, it is not possible to draw conclusions about this association, although often in our clinical practice we see more and more cases like this. Further studies that can strengthen this hypothesis would be useful to deepen and better analyze this interesting association.
COMMENTS
Case characteristics
The authors describe a case of a 31-year-old male cocaine user and without other cardiovascular risk factors, admitted to the authors’ department for typical acute chest pain.
Clinical diagnosis
At cardiac examination the authors found a 1/6 Levine systolic murmur at the precordium, blood pressure was 180/90 mmHg and the electrocardiogram showed sinus rhythm, ST segment depression with T negative waves from V2 to V5.
Differential diagnosis
Cocaine induced chest pain is a common presentation in emergency departments and premature coronary atherosclerosis with obstructive coronary artery disease, focal occlusive vasospasm, diffuse coronary vasoconstriction and coronary artery ectasia (CAE) are clinical conditions to be excluded in these patients.
Laboratory diagnosis
Leukocytosis, increasing of inflammatory markers and positive Troponin I were present; furthermore thrombophilia testing was negative and an increasing of matrix metalloproteinase (MMP) values with a reduction of their tissue inhibitors was showed both during hospitalization and at one month after discharge.
Imaging diagnosis
Coronary angiography showed diffuse coronary ectasia with slow flows and without hemodynamically significant coronary stenosis.
Treatment
Patient was subjected to pharmacological treatment with acetylsalicylic acid, ACE inhibitors, beta-blockers, spironolactone, and statins.
Related reports
A double assessment of MMP values and of their tissue inhibitors was carried out both during hospitalization and at one month after discharge to ensure that values were not affected by the acute event, furthermore others possible causes of persistent elevated levels of MMP have not been observed after discharge.
Experiences and lessons
Cocaine abuse should be considered an important risk factor for CAE and appears to be another potential mechanism of acute coronary syndromes in cocaine users; anyway further studies that can strengthen this hypothesis would be useful to deepen and better analyze this interesting association.
Peer-review
The authors reported the acute coronary syndrome accompanied with CAE in a young male cocaine user. This case report is interesting.
Footnotes
Institutional review board statement: Interventional Cardiology, “P.Giaccone” University Hospital of Palermo Institutional Review Board.
Informed consent statement: All involved persons gave their informed prior to study inclusion.
Conflict-of-interest statement: No conflict of interest.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: January 3, 2016
First decision: February 2, 2016
Article in press: March 9, 2016
P- Reviewer: den Uil CA, Falconi M, Teragawa H S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
References
- 1.Dendramis G, Paleologo C, Lo Presti A, Piraino D, Lo Greco V, Grassedonio E, La Grutta L, Midiri M, Assennato P, Novo S. [Coronary artery ectasia: etiopathogenesis, diagnosis and treatment] G Ital Cardiol (Rome) 2014;15:161–169. doi: 10.1714/1463.16165. [DOI] [PubMed] [Google Scholar]
- 2.Lange RA, Hillis LD. Cardiovascular complications of cocaine use. N Engl J Med. 2001;345:351–358. doi: 10.1056/NEJM200108023450507. [DOI] [PubMed] [Google Scholar]
- 3.Su J, Li J, Li W, Altura BT, Altura BM. Cocaine induces apoptosis in cerebral vascular muscle cells: potential roles in strokes and brain damage. Eur J Pharmacol. 2003;482:61–66. doi: 10.1016/j.ejphar.2003.09.056. [DOI] [PubMed] [Google Scholar]
- 4.Fiala M, Gan XH, Zhang L, House SD, Newton T, Graves MC, Shapshak P, Stins M, Kim KS, Witte M, et al. Cocaine enhances monocyte migration across the blood-brain barrier. Cocaine’s connection to AIDS dementia and vasculitis? Adv Exp Med Biol. 1998;437:199–205. doi: 10.1007/978-1-4615-5347-2_22. [DOI] [PubMed] [Google Scholar]
- 5.Demopoulos VP, Olympios CD, Fakiolas CN, Pissimissis EG, Economides NM, Adamopoulou E, Foussas SG, Cokkinos DV. The natural history of aneurysmal coronary artery disease. Heart. 1997;78:136–141. doi: 10.1136/hrt.78.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Satran A, Bart BA, Henry CR, Murad MB, Talukdar S, Satran D, Henry TD. Increased prevalence of coronary artery aneurysms among cocaine users. Circulation. 2005;111:2424–2429. doi: 10.1161/01.CIR.0000165121.50527.DE. [DOI] [PubMed] [Google Scholar]


