Abstract
Formerly known as Nantucket fever, babesiosis is increasing in incidence across the Northeastern United States. Because of its emerging health risk globally, it is important to be aware of its various presenting manifestations. We present the case of a middle-aged man with haemolytic anaemia from Babesia microti infection.
Keywords: Babesia microti, babesiosis, haemolytic anaemia, immunocompetent, Ixodes scapularis tick
Case report
A 45-year-old man presented with a 3-week history of worsening dyspnoea on exertion and fatigue, as well as a dry cough prompting him to present to the emergency department. He reported experiencing subjective fevers and weight loss. He reported recent travel to the Midwest United States from New York City; however, he had not travelled internationally in several years. At presentation the patient was tachycardic and afebrile. Initial laboratory results revealed anaemia (haemoglobin 9.3 g/dL), elevated prothrombin time, hyperbilirubinemia and hepatitis.
The patient was admitted; follow-up laboratory studies revealed worsening anaemia (haemoglobin 7.2 g/dL) with elevated reticulocyte count, lactate dehydrogenase and haptoglobin as well as a negative direct Coombs test. A parasite smear looking for Plasmodium or Babesia parasites was performed and demonstrated the presence of intraerythrocytic ring forms (Fig. 1) suggestive of Babesia microti with an overall low parasite load of 1%. B. microti serologies showed an immunoglobulin M level greater than 1:320 with an immunoglobulin G level of 1:128. Serum for babesial DNA was positive. Investigation for concurrent infection with Ehrlichia chaffeensis, Anaplasma phagocytophilum and Borrelia burgdorferi was negative. He was treated with atovaquone and azithromycin, with improvements in symptoms and haemolytic anaemia.
Fig. 1.
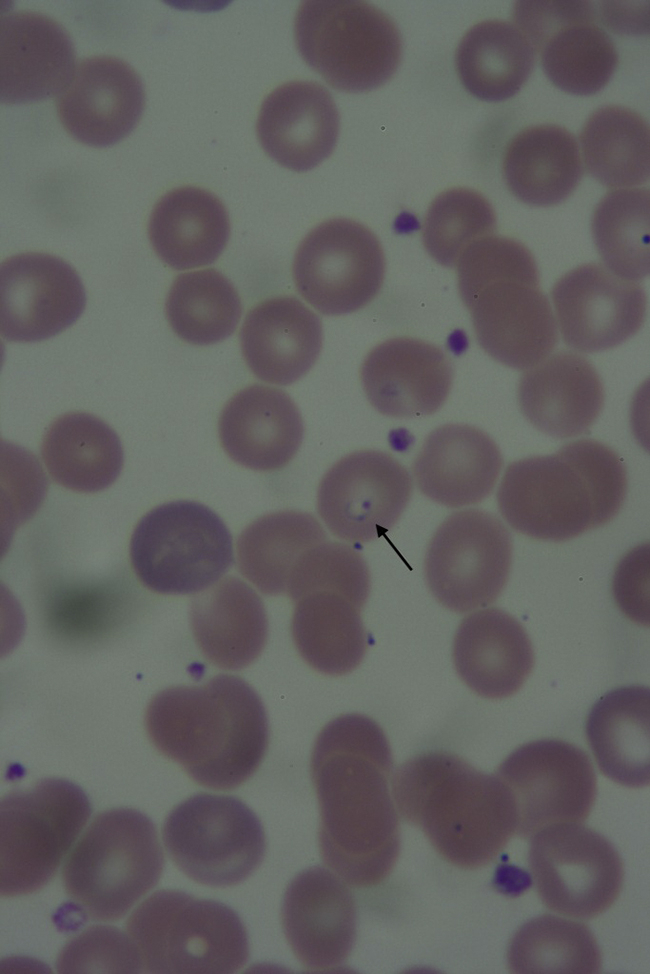
Parasite blood smear demonstrating presence of intraerythrocytic ring-form trophozoite (arrow).
Discussion
The intraerythrocytic protozoan species Babesia microti is the most common cause of human babesiosis in the United States and is a growing health concern [1]. Although it is mainly transmitted to humans through the Ixodes scapularis tick, it has also been reported by the US Food and Drug Administration to be the most common transfusion-transmitted pathogen [2]. It is endemic to the Northeast and upper Midwest regions of the United States [2].
Clinical manifestations of babesiosis range from an asymptomatic infection to fulminant and sometimes fatal disease. Common symptoms include fatigue, malaise, myalgia, fever and headache. Common laboratory abnormalities include a haemolytic anaemia, thrombocytopenia and elevated liver enzymes [1], [2].
Our patient's presentation was atypical for babesiosis. He required hospitalization despite his younger age and immunocompetent status. Fever is the most common symptom of babesiosis, with 85% of patients exhibiting a temperature greater than 38°C [1]. In 2011 the median age for hospitalized patients was 68 years [1]. Most patients with B. microti infections who require hospitalization are immunocompromised with malignancy, prior splenectomy or chronic heart, lung or liver disease [2].
A definitive diagnosis of babesiosis is made by visualization of the intraerythrocytic trophozoites or merozoites (with the classic finding of a Maltese cross tetrad) on thin blood smears with Giemsa or Wright staining, and must be clinically distinguished from Plasmodium falciparum [2]. Parasitemia on Giemsa-stained thin blood smears rarely exceeds 5% in immunocompetent hosts. The parasite level and the severity of the disease do not necessarily coincide [2], [3].
Treatment of babesiosis in the immunocompetent patient with mild to moderate disease typically involves a combination of atovaquone and azithromycin for 7 to 10 days [4]. Symptoms typically resolve within a day or two of initiating therapy, and complete clearance of the infection occurs within 3 months. Immunocompromised patients with severe disease may require partial or complete erythrocyte exchange transfusion [2], [5]. These patients may experience parasitemia for extended periods of time [2].
With babesial infections becoming more prevalent across America, it is important to be able to recognize all spectrums of the disease to prevent delays in diagnosis.
Conflict of interest
None declared.
Acknowledgement
We thank M. Lee, Department of Pathology, New York University Langone Medical Center, for providing us with the pathology images.
References
- 1.US Centers for Disease Control and Prevention Babesiosis surveillance—18 states, 2011. MMWR Morb Mortal Wkly Rep. 2012;61:505–509. [PubMed] [Google Scholar]
- 2.Vannier E., Krause P.J. Human babesiosis. N Engl J Med. 2012;366:2397–2407. doi: 10.1056/NEJMra1202018. [DOI] [PubMed] [Google Scholar]
- 3.Vannier E., Krause P.J. Update on babesiosis. Interdiscip Perspect Infect Dis. 2009;2009:984568. doi: 10.1155/2009/984568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krause P.J., Lepore T., Sikand V.K., Gadbaw J., Jr, Burke G., Telford S.R., 3rd Atovaquone and azithromycin for the treatment of babesiosis. N Engl J Med. 2000;343:1454–1458. doi: 10.1056/NEJM200011163432004. [DOI] [PubMed] [Google Scholar]
- 5.Jacoby G.A., Hunt J.V., Kosinski K.S., Demerjian Z.N., Huggins C., Etkind P. Treatment of transfusion-transmitted babesiosis by exchange transfusion. N Engl J Med. 1980;303:1098–1100. doi: 10.1056/NEJM198011063031906. [DOI] [PubMed] [Google Scholar]


