Intensive care management
The goal in management of an acute burn is to limit the extent of the systemic insult. Intensive care management should not be seen as rescue for failed initial treatment but as a preventive measure in patients at high risk of organ failure. Intensive care units have the resources for improved monitoring and expertise in managing acute physiological changes. Intensive care management should not, however, become an obstacle to early aggressive surgical excision of the burn wound, which is associated with improved outcome.
Figure 1.
Patient with burns in intensive care unit. Note the bilateral slings raising the burnt hands, air fluidised mattress, warm air heater, haemofiltration, and ventilator
Airway burns
The term “inhalational injury” has been used to describe the aspiration of toxic products of combustion, but also more generally any pulmonary insult associated with a burn injury. Patients with cutaneous burns are two to three times more likely to die if they also have lower airway burns. Death may be a direct result of lung injury but is usually due to the systemic consequences of such injury. It may be impossible to distinguish lung injury caused at the time of the burn directly to the lungs by a burn from injury due to the systemic consequences of the burn.Q
Table 1.
Warning signs of airway burns
| Suspect airway burn if: |
| • Burns occurred in an enclosed space |
| • Stridor, hoarseness, or cough |
| • Burns to face, lips, mouth, pharynx, or nasal mucosa |
| • Soot in sputum, nose, or mouth |
| • Dyspnoea, decreased level of consciousness, or confusion |
| • Hypoxaemia (low pulse oximetry saturation or arterial oxygen tension) or increased carbon monoxide levels (>2%) |
| Onset of symptoms may be delayed |
Diagnosis of lower airway burns is largely based on the patient's history and clinical examination. Clinicians should have a high index of suspicion of airway burns in patients with one or more of the warning signs. Special investigations will support clinical suspicion. However, severity of injury or prediction of outcome is not aided by additional tests.
The pathophysiology of airway burns is highly variable, depending on the environment of the burn and the incomplete products of combustion. The clinical manifestations are often delayed for the first few hours but are usually apparent by 24 hours. Airway debris—including secretions, mucosal slough, and smoke residue—can seriously compromise pulmonary function.
There is no specific treatment for airway burns other than ensuring adequate oxygenation and minimising iatrogenic lung insult. Prophylactic corticosteroids or antibiotics have no role in treatment.
Table 2.
Mechanisms of pulmonary insult after lower airway burns
| • Mucosal inflammation | • Ciliary paralysis |
| • Mucosal burn | • Reduced surfactant |
| • Bronchorrhoea | • Obstruction by debris |
| • Bronchospasm | • Systemic inflammatory response |
Control of the airway, by endotracheal intubation, is essential before transporting any patient with suspected airway burn. Rapid fluid administration, with inevitable formation of oedema, may lead to life threatening airway compromise if control of the airway is delayed. Endotracheal intubation before oedema formation is far safer and simpler. Oxygen (100%) should be given until the risk of carbon monoxide toxicity has been excluded, since high concentrations of oxygen will clear carbon monoxide from the body more rapidly than atmospheric concentrations. Importantly, carbon monoxide toxicity may result in a falsely elevated pulse oximetry saturation.
Airway burns are associated with a substantially increased requirement for fluid resuscitation. Reducing the fluid volume administered, to avoid fluid accumulation in the lung, results in a worse outcome. Invasive monitoring may be required to guide fluid administration, especially with failure to respond to increasing volumes of fluid. Adequate oxygen delivery to all the tissues of the body is essential to prevent multi-organ failure.
Figure 2.
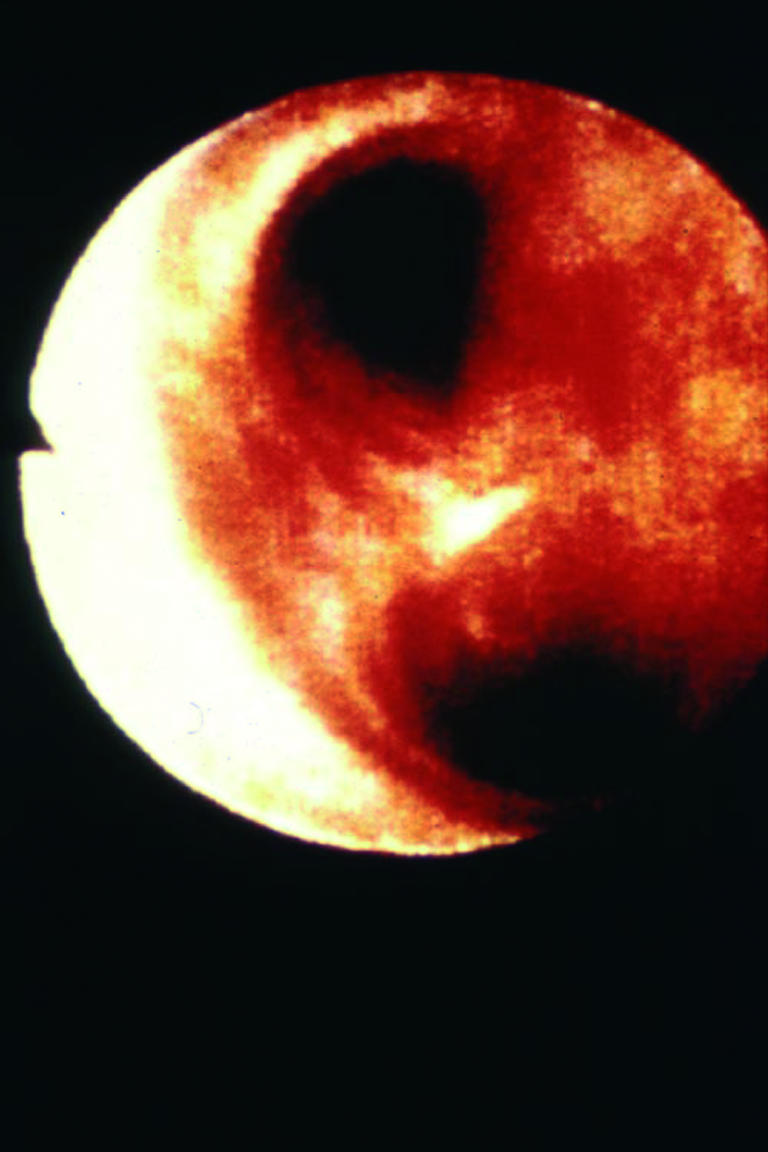
Bronchoscopy image showing mucosal inflammation
Aggressive airway toilet is essential. Diluted heparin and acetyl cystine nebulisation may be helpful. Early surgical debridement, enteral feeding, mobilisation of the patient, and early extubation are desirable. Antibiotics should be reserved for established infections and guided by regular microbiological surveillance.
Table 3.
Airway burns—key clinical points
| • Restricting fluids increases mortality |
| • If in doubt, intubate |
| • Give 100% oxygen until carbon monoxide toxicity excluded |
| • Ventilatory strategies to avoid lung injury (low volume or pressure) |
| • Aggressive airway toilet |
| • Early surgical debridement of wounds |
| • Early enteral feeding |
Several ventilatory strategies have been proposed to improve outcome following airway burns. Adequate systemic oxygenation and minimising further alveolar injury is the primary clinical objective. Prolonging survival will permit spontaneous lung recovery.
Intensive monitoring—The intensive care environment facilitates rapid, graded response to physiological disturbance. Frequent reassessment, based on a range of clinical and monitored parameters, should guide treatment. Fluid administration should not be guided by calculated fluid requirements alone. Failure to respond to treatment should trigger an escalation in the invasiveness of the monitoring.
Table 4.
Possible ventilatory strategies for patients with airway burns
| • Low volume ventilation |
| • Permissive hypercapnia |
| • High frequency percussive ventilation |
| • Nitric oxide |
| • Surfactant replacement |
| • Partial liquid ventilation (experimental) |
| • Extracorporeal membrane oxygenation (limited application) |
Heart failure
Myocardial dysfunction is a potential consequence of major burn injury. It has been attributed to a circulating myocardial depressant factor, primarily causing myocardial diastolic dysfunction. It may also be caused by myocardial oedema.
Administration of an inotropic agent is preferable to overloading a failing myocardium with large volumes of fluid. However, the inotropic drug can produce vasoconstriction in the burn wound, reducing the viability of critically injured tissue. Inotropic drugs should not be used until adequate fluid resuscitation has been ensured (usually by invasive monitoring). Inotropic drugs that do not produce vasoconstriction (such as dopexamine or dobutamine) will preserve wound viability, providing they do not produce unacceptable hypotension.
Table 5.
End points to guide fluid administration
| • Vital signs (blood pressure, heart rate, capillary refill) |
| • Urine output |
| • Peripheral perfusion (temperature gradient) |
| • Gastric mucosal pH |
| • Serum lactate or base deficit |
| • Central venous pressure or pulmonary capillary wedge pressure |
| • Cardiac output—oxygen delivery and consumption |
Kidney failure
Early renal failure after burn injury is usually due to delayed or inadequate fluid resuscitation, but it may also result from substantial muscle break down or haemolysis. Delayed renal failure is usually the consequence of sepsis and is often associated with other organ failure.
A reduced urine output, despite adequate fluid administration, is usually the first sign of acute renal failure. This will be followed by a rise in serum creatinine and urea concentrations. Early renal support (haemodialysis or haemodiafiltration) will control serum electrolytes and accommodate the large volumes of nutritional supplementation required in a major burn.
Cerebral failure
Hypoxic cerebral insults and closed head injuries are not uncommonly associated with burn injuries. Fluid administration for the burn injury will increase cerebral oedema and intracranial pressure. Monitoring intracranial pressure may help in minimising the adverse effects of trying to achieve two contradictory treatment goals.
Figure 3.
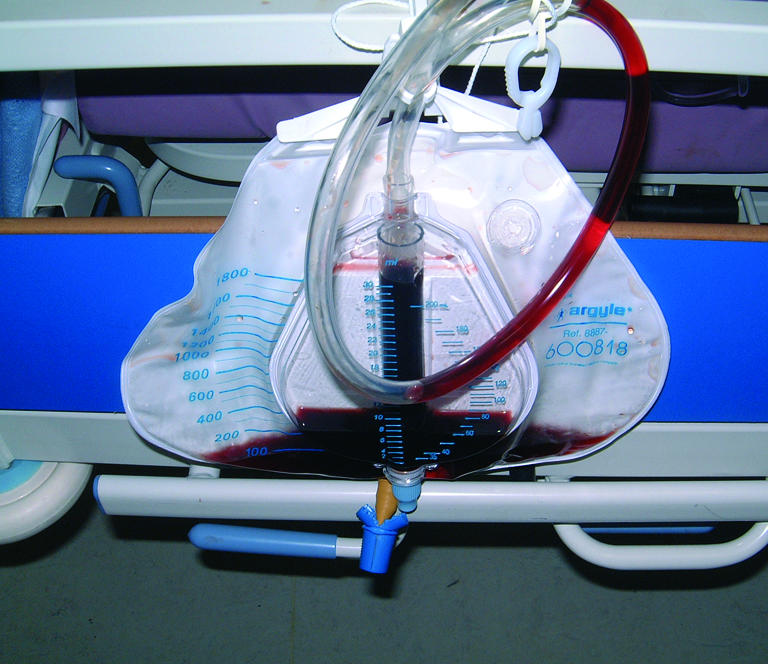
Myoglobinuria in patient after receiving high tension electrical burns
Nutrition
Burn injury is associated with a considerable hypermetabolic response, mediated by the systemic response to the burn and related to the extent of the burn injury. The hypermetabolism may result in a resting energy expenditure increase in excesses of 100% of basal metabolic rate. Even small burns can be associated with hyperpyrexia directly due to hypermetabolism.
Only limited success has been achieved in reducing the hypermetabolic state, which may persist for many months. Close attention to nutritional needs is critical to prevent protein breakdown, decreased wound healing, immune suppression, and an increase in infective complications.
Table 6.
Management of the hypermetabolic response
| • Reduce heat loss—environmental conditioning |
| • Excision and closure of burn wound |
| • Early enteral feeding |
| • Recognition and treatment of infection |
Energy requirements are proportional to the size of the burn and should be met by enteral nutrition, and this should be established as soon as possible after the burn injury. Total parenteral nutrition is associated with immunosuppression, an increase in infective complications, and reduced survival. Glutamine, arginine, and omega 3 fatty acid supplementation may improve immunity and gut function.
Table 7.
Causative agents of wound infection
| Bacteria |
| β haemolytic streptococci—Such as Streptococcus pyogenes. Cause acute cellulitis, and occasionally associated with toxic shock syndrome |
| Staphylococci—Such as methicillin resistant Staphylococcus aureus (MRSA). Cause abscesses and subeschar pus |
| Gram negative bacteria—Such as Pseudomonas aeruginosa, Acinetobacter baumanii, Proteus species. Mini epidemics seen in specialised centres secondary to antibiotic pressure |
| Fungi |
| Candida—Most common fungal isolate, act as surface colonisers but have low potential for invasion |
| Filamentous fungi—Such as Aspergillus, Fusarium, and phycomycetes. Can be aggressive invaders of subcutaneous tissues. Treatment must include debridement of infected tissue |
| Viruses |
| Herpes simples—Characterised by vesicular lesions |
Infection in burns patients
After the initial resuscitation, up to 75% of mortality in burns patients is related to infection. Preventing infection, recognising it when it occurs, and treating it successfully present considerable challenges. Infective pulmonary complications are now the commonest types of infection seen in burns patients, but infection is common in many other sites. Several factors contribute to the high frequency and severity of infection at multiple sites in burns patients:
Table 8.
Tube feeding in burns patients
| • In all patients with burns covering more than 20% of total body surface area |
| • Established during initial resuscitation |
| • Early enteral feeding improves success in establishing feeding |
| • Nasojejunal feeding will bypass gastric stasis |
Destruction of the skin or mucosal surface barrier allows microbial access
Presence of necrotic tissue and serosanguinous exudate provides a medium to support growth of microorganisms
Invasive monitoring provides portals for bacterial entry
Impaired immune function allows microbial proliferation.
Deciding whether infection is present can be difficult. Burns patients have an inflammatory state from the injury itself that can mimic infection. Extensive microbial colonisation of wounds makes interpretation of surface cultures difficult. Patients may have open wounds and repeated episodes of infection over weeks. Excessive use of antibiotics will encourage the appearance of resistant colonising organisms. A sensible approach is to limit antibiotic use to short courses of drugs with as narrow a spectrum of activity as is feasible.
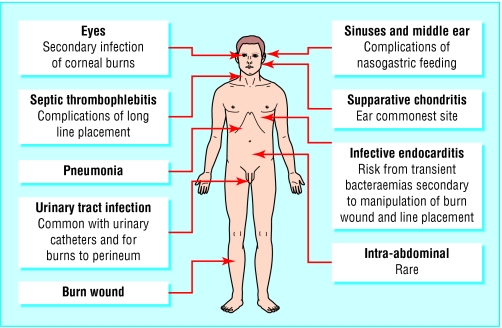
Figure 4.
Sites of potential infection in a burns patient
Pathogenesis
The burn injury destroys surface microbes except for Gram positive organisms located in the depths of the sweat glands or hair follicles. Without prophylactic use of topical antimicrobial agents, the wound becomes colonised with large numbers of Gram positive organisms within 48 hours. Gram negative bacteria appear from three to 21 days after the injury. Invasive fungal infection is seen later.
Figure 5.

Streptococcal cellulitis in a superficial burn wound
The microbiology reflects the hospital environment and varies from centre to centre. In general there has been a change in the main infective organisms over time from β haemolytic streptococci to resistant Gram negative organisms including pseudomonas, resistant Gram positive organisms, and fungi.
Figure 6.

Pseudomonal colonisation of a grafted burn wound on a thigh (note vivid green coloration of dressing)
Table 9.
Risk factors for pneumonia
| • Inhalational injury: |
| a) Destruction of respiratory epithelial barrier |
| b) Loss of ciliary function and impaired secretion clearance |
| c) Bronchospasm |
| d) Mucus and cellular plugging |
| • Intubation |
| • Circumferential, full thickness chest wall burns |
| Decreased chest wall compliance |
| • Immobility |
| • Uncontrolled wound sepsis |
| Can lead to secondary pneumonia from haematogenous spread of organisms from wound |
Preventing invasive wound infection
One aim of initial wound management is to prevent invasive infection. To this end, aggressive surgery and the use of topical antimicrobial agents are effective. Topical antimicrobial treatment slows wound colonisation and is of use early, before definitive surgery. A wide selection of agents are available: silver sulfadiazine is the most frequently used. Early closure of the burn wound by surgical techniques then lessens the surface area available for further microbial colonisation and subsequent infection.
Table 10.
Advantages and adverse effects of topical antimicrobials
| Silver sulfadiazine |
| • Water soluble cream |
| • Advantages—Broad spectrum, low toxicity, painless |
| • Adverse effects—Transient leucopenia, methaemoglobinaemia (rare) |
| Cerium nitrate-silver sulfadiazine |
| • Water soluble cream |
| • Advantages—Broad spectrum, may reduce or reverse immunosuppression after injury |
| • Adverse effects—As for silver sulfadiazine alone |
| Silver nitrate |
| • Solution soaked dressing |
| • Advantages—Broad spectrum, painless |
| • Adverse effects—Skin and dressing discoloration, electrolyte disturbance, methaemoglobinaemia (rare) |
| Mafenide |
| • Water soluble cream |
| • Advantages—Broad spectrum, penetrates burn eschar |
| • Adverse effects—Potent carbonic anhydrase inhibitor—osmotic diuresis and electrolyte imbalance, painful application |
Prophylactic use of systemic antibiotics is controversial. Most agree that prophylactic penicillin against group A streptococcal sepsis is not indicated, and broad spectrum antibiotics to cover wound manipulation are not required in patients with burns covering less than 40% of total body surface area.
Diagnosing invasive wound infection
Surface swabs and cultures cannot distinguish wound infection from colonisation. Wound biopsy, followed by histological examination and quantitative culture, is the definitive method. However, it is time consuming and expensive, making it impractical as a routine diagnostic technique. Diagnosis of infection therefore relies heavily on clinical parameters, with the aid of blood, surface, or tissue cultures to identify likely pathogens.
Table 11.
Signs of wound infection
| • Change in wound appearance: |
| a) Discoloration of surrounding skin |
| b) Offensive exudate |
| • Delayed healing |
| • Graft failure |
| • Conversion of partial thickness wound to full thickness |
Treatment
When invasive infection of a burn wound is suspected, empirical systemic antimicrobial treatment must be started. Topical treatment alone is not sufficient, as it does not effectively penetrate the eschar and damaged tissue. The choice of antibiotic depends on the predominant flora on the unit. This can be adjusted later depending on culture and sensitivity results of relevant specimens. Necrotic and heavily infected material must be removed by surgical excision.
Table 12.
Key points
| • Fluid resuscitation must be based on frequent reassessment. Formulas are only a guide |
| • Pulse oximetry readings may be normal in carbon monoxide toxicity |
| • Unnecessary intubation is preferable to systemic hypoxia |
| • Early enteral nutrition in major burns may improve survival |
| • Burn patients are at high risk of infection, and there are many sites for infective complications |
| • Antibiotics should be used wisely to limit emergence of multiresistant organisms: close liaison with a clinical microbiologist is crucial |
Infection control
Infection control measures help to minimise cross infection between patients and acquisition of nosocomial pathogens (such as MRSA or multiresistant Gram negative bacteria). Strict isolation of every patient is impractical, but universal precautions are an absolute necessity.
Mark Ansermino is paediatric anaesthesiologist, British Columbia's Children's Hospital, Vancouver, Canada. Carolyn Hemsley is specialist registrar in infectious diseases and microbiology, John Radcliffe Hospital, Oxford.
The ABC of burns is edited by Shehan Hettiaratchy, specialist registrar in plastic and reconstructive surgery, Pan-Thames Training Scheme, London; Remo Papini, consultant and clinical lead in burns, West Midlands Regional Burns Unit, Selly Oak University Hospital, Birmingham; and Peter Dziewulski, consultant burns and plastic surgeon, St Andrew's Centre for Plastic Surgery and Burns, Broomfield Hospital, Chelmsford. The series will be published as a book in the autumn.
Competing interests: See first article for series editors' details.
Further reading and resources
- • Still JM Jr, Law EJ. Primary excision of the burn wound. Clin Plast Surg 2000;27: 23-8 [PubMed] [Google Scholar]
- • Desai MH, Mlcak R, Richardson J, Nichols R, Herndon DN. Reduction in mortality in pediatric patients with inhalation injury with aerosolized heparin/N-acetylcystine [correction of acetylcystine] therapy. J Burn Care Rehabil 1998;19: 210-2 [DOI] [PubMed] [Google Scholar]
- • Pruitt BA, Mc Manus AT, Kim SH, Goodwin MD. Burn wound infections. World J Surg 1998;22: 135-45 [DOI] [PubMed] [Google Scholar]
- • Monafo WM, West MA. Current treatment recommendations for topical therapy. Drugs 1990;40: 364-73 [DOI] [PubMed] [Google Scholar]
- • Warren S, Burke JF. Infection of burn wounds: evaluation and management. Curr Clin Top Infect Dis 1991;11: 206-17 [PubMed] [Google Scholar]