Abstract
Background
Multiple sclerosis (MS) is the most common neurological autoimmune disease, characterized by multifocal areas of inflammatory demyelination within the central nervous system. It has been hypothesized that the stimulation of the immune system by viral infections is the leading cause of MS among susceptible individuals.
Objectives
The aim of this study was to investigate the prevalence of the varicella zoster virus (VZV) in patients with relapsing-remitting multiple sclerosis.
Patients and Methods
Plasma and peripheral blood mononuclear cells (PBMCs) collected from MS patients (n = 82) and controls (n = 89) were screened for the presence of anti-VZV antibodies and VZV DNA by the ELISA and PCR methods. DNA was extracted from all samples, and VZV infection was examined by the PCR technique. Statistical analysis was used to investigate the frequency of the virus in MS patients and a healthy control group.
Results
Of all the MS patients, 78 (95.1%) and 21 (25.6%) were positive for anti-VZV and VZV DNA, respectively. Statistical analysis of the PCR results showed a significant correlation between the abundance of VZV and MS disease (P < 0.001). However, there was no significant correlation between the abundance of anti-VZV antibodies and MS disease by the ELISA method.
Conclusions
These results support the hypothesis that VZV may contribute to MS in establishing a systemic infection process and inducing an immune response.
Keywords: Multiple Sclerosis, Varicella Zoster Virus, Relapsing-Remitting Multiple Sclerosis
1. Background
Multiple sclerosis (MS), a degenerative chronic disease of the central nervous system, is characterized by small demyelination in the brain and myeloid cord. Several clinical studies have confirmed the contribution of viral or microbial infections in the development of MS (1). In addition, several human pathogenic viruses have been implicated as potential candidates in the pathogenesis of MS. Some studies have indicated that, according to the clinical presentations and the histopathological properties of MS lesions, a viral infection could be responsible for MS (2, 3).
Herpesviruses are a large family of DNA viruses, which are responsible for several autoimmune diseases, including systemic lupus erythematosus, MS and rheumatoid arthritis (4, 5). Herpesviruses remain within the nervous system of their hosts for decades, producing periodic inactivations (2). Some herpesviruses are neurotrophic, especially those from the subgroup of α-herpes viruses, such as herpes simplex virus (HSV) and varicella zoster virus (VZV) (2, 6). Varicella (chickenpox) is highly contagious and is a common epidemic disease of childhood. Most cases occur in children younger than 10 years old. In temperate climates, VZV infection is much more common in winter and spring than in summer. Zoster (shingles) occurs sporadically, mainly in adults and without seasonal distribution (5).
Although several herpesviruses have been involved as participants in the pathology of MS, the most often cited by current studies are human herpes virus 6 (HHV-6) and Epstein Barr virus (EBV) (7, 8). Epidemiological studies from geographical regions where the incidence of MS has enhanced in recent decades, have pointed out a high prevalence of VZV in the clinical history of MS patients. In addition, laboratory examinations have found a high viral load of VZV DNA in leucocytes and cerebrospinal fluid (CSF) of MS patients, limited to the transient stage of MS relapse, followed by the disappearance of VZV during alleviation (2). Although VZV has been suggested as a possible participant in the etiopathogenesis of MS (9, 10), the results of several epidemiological investigations have failed to support this link. Previous studies have indicated that there is inadequate document to confirm the correlation of MS with VZV infections (11).
2. Objectives
Varicella zoster virus infection is a controversial risk factor in the medical history of MS patients. Therefore, the present study aimed to investigate the presence of VZV in patients with MS.
3. Patients and Methods
3.1. Patients
Eighty-two blood samples from MS patients (23 males and 59 females) and 89 blood samples from healthy individuals (control group) were collected based on age and gender in four different cities in the north of Iran (Rasht, Ramsar, Tonkabon and Chalus). The samples were transferred to the laboratory of genetics research at Islamic Azad university, Tonekabon branch. Patients were diagnosed according to the McDonald et al. criteria (12). MS patients had no history of diabetes, allergy, or other autoimmune diseases, and all patients received treatment, except 10 that were considered ‘drug naive’. The study protocol was approved by the local ethics committee and confirmed by the ethical guidelines of Islamic Azad university, Tonekabon branch, Iran.
3.2. Sample Collection
Five mL of peripheral blood from MS patients and healthy group were treated with EDTA and then centrifuged. The serum samples were stored at -80°C until enzyme-linked immunosorbent assay (ELISA).
3.3. VZV‑Specific Antibody Response
A serological marker for VZV was performed on the stored serum samples from MS patients and the healthy group. Serum from patients with MS and 89 healthy control subjects was searched for the IgG antibody to VZV antigens by ELISA (EUROIMMUN anti-Varicella-Zoster-Virus IgG-ELISA, Germany).
3.4. DNA Extraction
Peripheral blood mononuclear cells (PBMCs) were separated from fresh whole blood by Ficoll density gradient centrifugation (Sigma, Germany), re-suspended in RPMI (Sigma, Germany), and stored in liquid nitrogen for future use. VZV DNA was extracted from the PBMC samples using an extraction kit (Qiagen, Germany), according to the manufacturer’s instructions. The purity of the extracted DNA was confirmed based on the absorbance of the extracted DNA at 260 nm and 280 nm wavelengths by biophotometer (Eppendorf, Germany). The samples were stored in a -80°C freezer for future tests.
3.5. Human Beta-Globin Gene Amplification
The human beta-globin gene was used as an internal control in order to confirm the accuracy of DNA extraction. The following primers, produced by TAG Copenhagen (Denmark), were used to amplify the human beta-globin gene: beta-globin-forward: 5’-TCCAACATCAACATCTTGG T-3’ and beta-globin-Reverse: 5’-TCCCCCAAATTCTAAGCAGA-3’ (13). Each reaction mixture contained 10 μL of primer taq premix (2X), 1 μL of 10 pmol of forward and reverse PCR primers, 3 μL of distilled water and 5 μL of DNA template. PCR amplification conditions on a thermocycler (Biorad-Germany) were as follows: 95°C for 5 minutes, followed by 35 cycles of 95°C for 45 seconds, 54°C for 30 seconds and 72°C for 30 seconds, with a final extension at 72°C for 5 minutes. An aliquot of all PCR products was run on a 1.5% (w/v) agarose gel with a 100 bp DNA ladder.
3.6. Polymerase Chain Reaction for the Detection of Varicella Zoster Virus
Specific primers, produced by TAG Copenhagen (Denmark), were used to amplify the VZV genes. The sequences of forward and reverse primers were 5’- ATGTCCGTACAACATCAACT-3’ and 5’-CGATTTTCCAAGAGAGACGC-3', respectively (13). Each reaction mixture contained 10 μL of primer taq premix (2X), 1 μL of 10 pmol of forward and reverse PCR primers, 3 μL of distilled water and 5 μL of DNA template. The negative control tube contained the same PCR reagents as mentioned above, but 5 μL of water was used instead of DNA template. The PCR amplification conditions on a thermocycler (Biorad-Germany) were as follows: 95°C for 5 minutes, followed by 40 cycles of 94°C for 45 seconds, 54.5°C for 40 seconds and 72°C for 35 seconds, with a final extension at 72°C for 10 minutes. An aliquot of all PCR products was run on a 1.5% (w/v) agarose gel with a 100 bp DNA ladder (Fermentas-Russia) and electrophoresed at 75 V for 40 minutes. The bands were visualized by ethidium bromide staining and photographed after UV treatment by a transilluminator (UV doc, England).
3.7. Statistical Analysis
The Statistical Program for the Social Sciences (SPSS-16, SPSS Inc., Chicago, Illinois, USA) was used for statistical analysis. Continuous variables were expressed as the mean ± standard deviation (SD) or median and were compared using the independent t-test. Categorical variables were expressed as percentages, and differences between groups were judged for significance using the Chi-square test or Fisher’s exact test. P values < 0.05 were considered significant.
4. Results
The demographic and clinical features of MS patients and healthy controls are given in Table 1. In this study, 171 blood samples were examined, among which 82 samples belonged to the patient group and 89 samples belonged to the control group. The blood samples from the patient group were collected based on factors such as age, gender, geographical area, history of viral infection, genetics, medications and disease duration. To describe the sample features, first, the collected data were summarized and concluded by descriptive statistics index, then, all the results from observing the selected samples were generalized to the society.
Table 1. Demographic Characteristics and VZV Frequency in RRMS Patients and Healthy Control Groupa.
| Variable | RRMS (n = 82) | Healthy (n = 89) | P Value |
|---|---|---|---|
| Gender | 0.194 | ||
| Male | 23 (28) | 34 (38.2) | |
| Female | 59 (72) | 55 (61.8) | |
| Age, y | 36.9 ± 9.30 | 34.32 ± 10.56 | 0.096 |
| Disease onset age | 27.46 ± 7.9 | NA | |
| Disease definite recognition age | 30.04 ± 9.53 | NA | |
| Family history | |||
| Yes | 15 (18.3) | NA | |
| No | 65 (79.3) | NA | |
| Unavailable | 2 (2.4) | NA | |
| VZV antibody | 0.539 | ||
| Positive | 78 (95.1) | 82 (92.1) | |
| Negative | 4 (4.9) | 7 (7.9) | |
| VZV PCR | < 0.001 | ||
| Positive | 21 (25.6) | 3 (3.4) | |
| Negative | 61 (74.4) | 86 (96.6) |
aValues are expressed as mean ± SD or No. (%).
The sex ratio of the MS group was 2.56:1, and a similar age distribution was observed between female (median 34 years; range 19 - 70) and male (median 39 years; range 18 - 54) patients. For the healthy individuals, the sex ratio was 1.61:1, and the age distribution was similar between female (median 31 years; range 15 - 58) and male (median 34 years; range 10 - 35) patients. There was no significant difference between the controls and the MS patients (P value = 0.194). Fifteen (18.3%) patients had a familial history of MS.
The standard PCR technique was used to identify the DNA of the virus. The amplified fragments of the human beta-globin gene and viral DNA were 122 bp and 267 bp, respectively (Figures 1 and 2).
Figure 1. Beta-Globin Amplification Products Analyses in a 1.5% Agarose Gel.

Lane M, ladder; Lanes 1 and 2, human beta-globin gene; and Lane 3, negative control.
Figure 2. VZV Amplification Products Analyses in a 1.5% Agarose Gel.
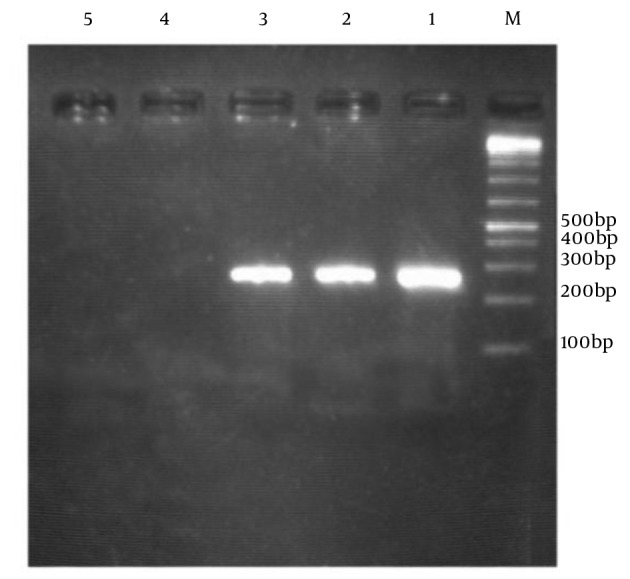
Lane M, ladder; Lane 1, positive control; Lanes 2 and 3, viral DNA (+); Lane 4, viral DNA (-); and Lane 5, negative control.
4.1. Detection of VZV Specific IgG Antibody
Of all participants in this study, 160 (93.56%) were positive for anti-VZV. Seventy-eight (95.1%) and 82 (92.1%) were positive for anti-VZV in MS patients and the healthy control group, respectively. Statistical analysis showed that there was no significant relationship between the frequency of anti-VZV antibodies in the MS patients and the healthy individuals (P = 0.539). In addition, no significant differences were found between gender, drug receives status, age, and the type of drug treatment in the MS patients (P = 0.325, 0.071 and 0.693, respectively).
4.2. PCR Finding
Varicella zoster virus DNA detection in MS patients and the healthy control group was performed in the PBMCs. As shown in Table 2, of all the participants, 24 (14%) were positive for VZV DNA. Furthermore, 21 (25.6%) and 3 (3.4%) were positive for VZV DNA in MS patients and the healthy control group, respectively (Table 3). We found that the presence of VZV DNA was significantly different in both groups (P = 0.001). No significant differences were found between MS patients based on gender, drug receives status, age, and the type of drug treatment (P = 0.874, 0.625 and 0.797, respectively).
Table 2. Frequency of VZV DNA Infection in Patients With MSa.
| Variable | VZV Positive (n = 21) | VZV Negative (n = 61) | P Value |
|---|---|---|---|
| Gender | 0.951 | ||
| Male | 6 (28.6) | 17 (27.9) | |
| Female | 15 (71.4) | 44 (72.1) | |
| Age, y | 36.22 ± 8.711 | 37.15 ± 9.58 | 0.693 |
| Family history | 0.548 | ||
| Yes | 5 (23.8) | 10 (16.4) | |
| No | 16 (76.2) | 49 (80.3) | |
| Unavailable | 0 | 2 (3.3) |
aValues are expressed as mean ± SD or No. (%).
Table 3. Frequency of VZV DNA Infection Healthy Control Groupa.
| Variable | VZV Positive | VZV Negative | P Value |
|---|---|---|---|
| Gender | 0.555 | ||
| Male | 2 (66.7) | 32 (37.1) | |
| Female | 1 (33.3) | 54 (62.9) | |
| Age, y | 32 ± 5.14 | 34.46 ± 10.8 | 0.615 |
aValues are expressed as mean ± SD or No. (%).
5. Discussion
Multiple sclerosis is a chronic inflammatory demyelinating disease of the central nervous system. Genetic and environmental factors jointly determine the susceptibility of developing MS (14, 15). Nowadays, researchers claim that many viruses, such as measles, VZV and EBV, are involved in the development of MS. These viruses can have long-term survival in the body (16). The present study investigated the prevalence of VZV in MS patients and healthy controls. In our study, 21 (25.%6) of patients with relapsing-remitting MS (RRMS) had VZV DNA, which was significantly higher than the control group. In addition, 78 (95.1%) of patients had specific antibodies against VZV.
The findings of our study suggest the effective role of viral infection in the pathology of MS disease. However, some studies, such as Franciotta et al. have reported no significant relationship between VZV and MS disease (17). Franciotta et al. screened the DNA of human herpesviridae in the serum and CSF of MS patients. The DNA of HSV, VZV, CMV, EBV and HHV-6 were examined in serum and CSF samples in 54 MS patients by the PCR method. All serum and CSF samples were negative in terms of the existence of herpesvirus DNA, but one sample of CSF in MS patients was positive in terms of the presence of EBV DNA. The findings of this study did not support the role of herpesviruses in the pathogenesis of MS (17). However, recent studies have been conducted because of the observation that the incidence of MS in Mexico was increasing, from a very rare disease in the 1970s to a common disease nowadays. This was observed by the progressive incidence distribution of new reports in neurological units throughout the country (18, 19). In addition, a nationwide population-based study in Taiwan showed that the incidence of MS could be correlated with herpes zoster activation. Kang et al. observed a significantly higher risk factor for MS within a 1-year follow-up period of VZV attack, compared with the control group (20).
The present study showed that there is a meaningful relationship between the frequency of VZV in MS patients and the control group, using the PCR method. As with the epidemiology of MS, the epidemiology of VZV is significantly different in various temperate and tropical regions, and its gradient prevalence decreases from north to south. VZV is common in temperate regions in childhood, while in tropical and subtropical regions it occurs later in life and affects less than 50% of the general population (21). As the north of Iran belongs to the temperate region, the risk of VZV in childhood and the high levels of VZV-specific antibodies appear reasonable (22).
In our study, viral DNA from VZV was found in PBMCs from patients with MS, who were possibly in the acute relapse phase at the time of the study. According to this supposition, the presence of VZV DNA only during the initial weeks of clinical aggravation could be similar to the characteristic diseases affected by VZV. Viral DNA can be detected in PBMCs only during the primary days of the acute phase (23).
Consistent with our study, other groups have found a significant relationship between human herpesviruses and MS disease (24-28). Sanders et al. analyzed active and inactive plaque textures in MS disease and a control group by the PCR method. They concluded that HSV, HHV-6, and VZV were more prevalent in MS cases compared to the control group (24). Based on our study and recent evidence, we propose that VZV is significantly associated with MS disease (2, 20, 29).
Ordonez et al. studied the possible role of VZV in the pathology of MS disease. They showed that the presence of VZV in blood mononuclear cells is restricted to the MS clinical relapse period. This finding suggests that either latent VZV is activated during an MS relapse, or VZV plays an important role in the etiological pathogenesis of MS (26). Furthermore, Ordonez et al. studied advanced forms of MS and their association with VZV. They examined the presence of VZV DNA in the blood lymphoid and cerebro-spinal fluid (CSF) of 20 progressive MS patients by the PCR method. VZV DNA was observed in 65% of CSF samples and viral particles, such as VZV, were found in 30% of the cases (27). If VZV has an association with the etiopathology of MS, some moot points, related to population genetic predisposition and to the mechanisms of viral latency and reactivation of VZV, are engrossing subjects for future studies.
The present study analyzed the distribution of VZV in the blood samples of RRMS patients and a healthy control group. Our finding has been implicated as a major participant in the etiology of MS disease.
Acknowledgments
We thank the research council of Tonekabon branch, Islamic Azad university for supporting this project.
Footnotes
Authors’ Contribution:Study concept and design: Saeideh Najafi and Masood Ghane; statistical analysis: Saeideh Najafi and Mehdi Amiri; data interpretation: Saeideh Najafi and Shahrokh Yousefzadeh-Chabok; drafting of the manuscript: Saeideh Najafi.
References
- 1.Nylander A, Hafler DA. Multiple sclerosis. J Clin Invest. 2012;122(4):1180–8. doi: 10.1172/JCI58649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sotelo J, Corona T. Varicella zoster virus and relapsing remitting multiple sclerosis. Mult Scler Int. 2011;2011:214763. doi: 10.1155/2011/214763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bachmann S, Kesselring J. Multiple sclerosis and infectious childhood diseases. Neuroepidemiology. 1998;17(3):154–60. doi: 10.1159/000026167. [DOI] [PubMed] [Google Scholar]
- 4.Posnett DN. Herpesviruses and autoimmunity. Curr Opin Investig Drugs. 2008;9(5):505–14. [PubMed] [Google Scholar]
- 5.Brooks GF, Carroll KC, Butel JS, Morse SA. Jawetz, Melnick and Adelberg's Medical Microbiology: Lange Medical Books. New York City: McGraw-Hill; 2013. [Google Scholar]
- 6.Alvarez R, Cour I, Kanaan A, Benedicto M, Martin-Estefania C, Arroyo R, et al. [Detection of viral genomes of the Herpesviridae family in multiple sclerosis patients by means of the polymerase chain reaction (PCR)]. Enferm Infecc Microbiol Clin. 2000;18(5):223–8. [PubMed] [Google Scholar]
- 7.Gilden D. Infectious causes of multiple sclerosis. Lancet Neurol. 2005;4(3):195–202. doi: 10.1016/s1474-4422(05)70023-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lipton HL, Liang Z, Hertzler S, Son KN. A specific viral cause of multiple sclerosis: one virus, one disease. Ann Neurol. 2007;61(6):514–23. doi: 10.1002/ana.21116. [DOI] [PubMed] [Google Scholar]
- 9.Ahlgren C, Toren K, Oden A, Andersen O. A population-based case-control study on viral infections and vaccinations and subsequent multiple sclerosis risk. Eur J Epidemiol. 2009;24(9):541–52. doi: 10.1007/s10654-009-9367-2. [DOI] [PubMed] [Google Scholar]
- 10.Ross RT, Cheang M, Landry G, Klassen L, Doerksen K. Herpes zoster and multiple sclerosis. Canadian J Neurol Sci. 1999;26(1):29–32. [PubMed] [Google Scholar]
- 11.Marrie RA, Wolfson C. Multiple sclerosis and varicella zoster virus infection: a review. Epidemiol Infect. 2001;127(2):315–25. doi: 10.1017/s0950268801005891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol. 2001;50(1):121–7. doi: 10.1002/ana.1032. [DOI] [PubMed] [Google Scholar]
- 13.Zaravinos A, Bizakis J, Spandidos DA. Prevalence of human papilloma virus and human herpes virus types 1-7 in human nasal polyposis. J Med Virol. 2009;81(9):1613–9. doi: 10.1002/jmv.21534. [DOI] [PubMed] [Google Scholar]
- 14.McFarlin DE, McFarland HF. Multiple sclerosis (first of two parts). N Engl J Med. 1982;307(19):1183–8. doi: 10.1056/NEJM198211043071905. [DOI] [PubMed] [Google Scholar]
- 15.De Jager PL, Jia X, Wang J, de Bakker PI, Ottoboni L, Aggarwal NT, et al. Meta-analysis of genome scans and replication identify CD6, IRF8 and TNFRSF1A as new multiple sclerosis susceptibility loci. Nat Genet. 2009;41(7):776–82. doi: 10.1038/ng.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kakalacheva K, Munz C, Lunemann JD. Viral triggers of multiple sclerosis. Biochim Biophys Acta. 2011;1812(2):132–40. doi: 10.1016/j.bbadis.2010.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Franciotta D, Bestetti A, Sala S, Perucca P, Jarius S, Price RW, et al. Broad screening for human herpesviridae DNA in multiple sclerosis cerebrospinal fluid and serum. Acta Neurol Belg. 2009;109(4):277–82. [PubMed] [Google Scholar]
- 18.Gonzalez O, Sotelo J. Is the frequency of multiple sclerosis increasing in Mexico? J Neurol Neurosurg Psychiatr. 1995;59(5):528–30. doi: 10.1136/jnnp.59.5.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Corona T, Roman GC. Multiple sclerosis in Latin America. Neuroepidemiology. 2006;26(1):1–3. doi: 10.1159/000089230. [DOI] [PubMed] [Google Scholar]
- 20.Kang JH, Sheu JJ, Kao S, Lin HC. Increased risk of multiple sclerosis following herpes zoster: a nationwide, population-based study. J Infect Dis. 2011;204(2):188–92. doi: 10.1093/infdis/jir239. [DOI] [PubMed] [Google Scholar]
- 21.Longfield JN, Winn RE, Gibson RL, Juchau SV, Hoffman PV. Varicella outbreaks in Army recruits from Puerto Rico. Varicella susceptibility in a population from the tropics. Arch Intern Med. 1990;150(5):970–3. [PubMed] [Google Scholar]
- 22.Weller TH. Varicella and herpes zoster. Changing concepts of the natural history, control, and importance of a not-so-benign virus. N Engl J Med. 1983;309(23):1434–40. doi: 10.1056/NEJM198312083092306. [DOI] [PubMed] [Google Scholar]
- 23.Gilden DH, Kleinschmidt-DeMasters BK, LaGuardia JJ, Mahalingam R, Cohrs RJ. Neurologic complications of the reactivation of varicella-zoster virus. N Engl J Med. 2000;342(9):635–45. doi: 10.1056/NEJM200003023420906. [DOI] [PubMed] [Google Scholar]
- 24.Sanders VJ, Felisan S, Waddell A, Tourtellotte WW. Detection of herpesviridae in postmortem multiple sclerosis brain tissue and controls by polymerase chain reaction. J Neurovirol. 1996;2(4):249–58. doi: 10.3109/13550289609146888. [DOI] [PubMed] [Google Scholar]
- 25.Wandinger K, Jabs W, Siekhaus A, Bubel S, Trillenberg P, Wagner H, et al. Association between clinical disease activity and Epstein-Barr virus reactivation in MS. Neurology. 2000;55(2):178–84. doi: 10.1212/wnl.55.2.178. [DOI] [PubMed] [Google Scholar]
- 26.Ordonez G, Pineda B, Garcia-Navarrete R, Sotelo J. Brief presence of varicella-zoster vral DNA in mononuclear cells during relapses of multiple sclerosis. Arch Neurol. 2004;61(4):529–32. doi: 10.1001/archneur.61.4.529. [DOI] [PubMed] [Google Scholar]
- 27.Ordonez G, Martinez-Palomo A, Corona T, Pineda B, Flores-Rivera J, Gonzalez A, et al. Varicella zoster virus in progressive forms of multiple sclerosis. Clin Neurol Neurosurg. 2010;112(8):653–7. doi: 10.1016/j.clineuro.2010.04.018. [DOI] [PubMed] [Google Scholar]
- 28.Djelilovic-Vranic J, Alajbegovic A. Role of early viral infections in development of multiple sclerosis. Med arch. 2012;66(3 Suppl 1):37–40. doi: 10.5455/medarh.2012.66.s37-s40. [DOI] [PubMed] [Google Scholar]
- 29.Mikaeloff Y, Caridade G, Suissa S, Tardieu M, Kidsep Study Group Clinically observed chickenpox and the risk of childhood-onset multiple sclerosis. Am J Epidemiol. 2009;169(10):1260–6. doi: 10.1093/aje/kwp039. [DOI] [PubMed] [Google Scholar]


