Abstract
Ambulatory blood pressure monitoring offers the ability to collect blood pressure readings several times an hour across a 24-hour period. Ambulatory blood pressure monitoring facilitates the identification of white-coat hypertension, the phenomenon whereby certain individuals who are not on antihypertensive medication show elevated blood pressure in a clinical setting but show non-elevated blood pressure averages when assessed by ambulatory blood pressure monitoring. Additionally, readings can be segmented into time windows of particular interest, e.g., mean daytime and nighttime values. During sleep, blood pressure typically decreases, or dips, such that mean sleep blood pressure is lower than mean awake blood pressure. A non-dipping pattern and nocturnal hypertension are strongly associated with increased cardiovascular morbidity and mortality. Approximately 70% of individuals dip ≥10% at night, while 30% have non-dipping patterns, when blood pressure remains similar to daytime average, or occasionally rises above daytime average. The various blood pressure categorizations afforded by ambulatory blood pressure monitoring are valuable for clinical management of high blood pressure since they increase accuracy for diagnosis and the prediction of cardiovascular risk.
Keywords: high blood pressure, ambulatory blood pressure monitoring, white-coat hypertension, masked hypertension, nocturnal blood pressure
INTRODUCTION
High blood pressure is currently the greatest threat to the global burden of disease.1–3 Hypertension continues to be the most common diagnosis in adult primary care practice as well as the most salient cardiovascular disease risk factor. Recent figures published by the American Heart Association's Statistics Committee and Stroke Statistics Subcommittee, based on 2007–2010 data, revealed that 33% of adults ≥ 20 years of age in the United States have hypertension, i.e., almost 80 million people (the prevalence is similar for both sexes).4 Fortunately, antihypertensive treatment substantially reduces the risk of heart failure, myocardial infarction, and stroke.5
Blood pressure measurements are essential for clinicians in the diagnosis and treatment of hypertension.6 Choosing the most informative blood pressure assessment methodology is therefore a topic of fundamental importance. Pickering and colleagues7 observed that "Any clinical measurement of blood pressure may be regarded as a surrogate measure for the "true" blood pressure of the patient, which may be defined as the mean level over prolonged periods." Compared with the traditional method of taking a small number of readings in a clinical setting, ambulatory blood pressure monitoring offers the ability to collect blood pressure readings several times an hour across a 24-hour period. These readings can be aggregated to yield 24-hour means and also grouped into time windows (e.g., mean daytime and nighttime values). The various blood pressure categorizations facilitated by ambulatory blood pressure monitoring are valuable for clinical management of high blood pressure since they increase accuracy for diagnosis and the prediction of cardiovascular risk.8 Several recent guidelines discuss the employment of ambulatory blood pressure monitoring in clinical practice (Table 1).9–16
TABLE.
Guidelines/Consensus Documents/Position Papers/Scientific Statements from Professional Societies related to Ambulatory Blood Pressure Monitoring
| Authors (Date of Publication) |
Title |
|---|---|
| NICE (2011)9 | Hypertension: clinical management of primary hypertension in adults. |
| National Heart Foundation and High Blood Pressure Research Council of Australia Ambulatory Blood Pressure Monitoring Consensus Committee (2011)10 |
Ambulatory blood pressure monitoring |
| Campbell and Hemmelgarn (2012)11 |
New recommendations for the use of ambulatory blood pressure monitoring in the diagnosis of hypertension. |
| JCS Joint Working Group (2012)12 |
Guidelines for the clinical use of 24 hour ambulatory blood pressure monitoring (ABPM) (JCS 2010). |
| Hermida et al (2013)13 |
2013 ambulatory blood pressure monitoring recommendations for the diagnosis of adult hypertension, assessment of cardiovascular and other hypertension-associated risk, and attainment of therapeutic goals. |
| O'Brien et al (2013)14 |
European Society of Hypertension position paper on ambulatory blood pressure monitoring. |
| Flynn et al (2014)15 | Ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. |
| Parati et al (2014)16 | European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. [NOTE: This paper is from the same Working Group as the O'Brien et al14 paper, and represents "an updated schematic summary of the most important aspects related to the use of ABPM in daily practice."16] |
Abbreviations: ESH, European Society of Hypertension. JCS, Japanese Circulation Society. NICE, National Institute for Health and Care Excellence.
Given the rapidly expanding and diverse literature on ambulatory blood pressure monitoring, this paper provides a narrative review of the underlying rationale for its employment in clinical practice, its strengths and limitations, and the directions it may take in clinical practice in the coming years.
FUNDAMENTALS OF AMBULATORY BLOOD PRESSURE MONITORING
As noted in the Introduction, ambulatory blood pressure monitoring generates much more information than the single (typically daytime) 'snapshot in time' reading yielded by clinic measurement by providing a profile of blood pressure behavior over a 24-hour (or longer17) period, and, therefore, how blood pressure throughout this period can be beneficially influenced by antihypertensive therapy. The challenges, limitations, and questionable veracity of (office) blood pressure measurement have been extensively discussed.7,18,19 It is now well documented that ambulatory blood pressure monitoring provides superior prediction of cardiovascular outcomes, as discussed shortly.
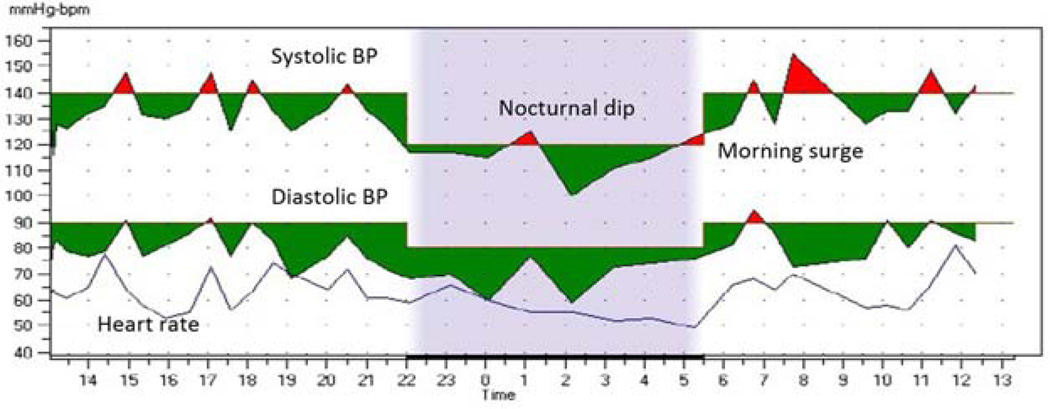
As well as facilitating blood pressure assessment aggregated over the entire 24-hour period, ambulatory blood pressure monitoring also allows more fine-tuned assessments during specific windows of this time cycle. The circadian cycle can be divided into various periods: assessments at different times permit evaluation of circadian variation in blood pressure (see Figure). Nighttime blood pressure is one of the most important measures of this circadian variation. Normally during sleep, blood pressure decreases ('dips') such that sleep average blood pressure is lower than average awake blood pressure. The 'normal' dip is considered 10%–20%. Individuals who dip <10% are said be nondippers. Nocturnal hypertension and non-dipping pattern are strongly associated with increased cardiovascular morbidity and mortality. Around 70% of individuals show reduced blood pressure at night (i.e., show dipping ≥10%), and about 30% have non-dipping patterns, when blood pressure remains similar to daytime average, or occasionally rises above daytime average (reverse dippers). Other important parameters of blood pressure assessment facilitated by ambulatory blood pressure monitoring are the morning surge, when blood pressure increases rapidly from nighttime levels to daytime levels, and blood pressure variability.
FIGURE. Graph of 24-Hour Ambulatory Blood Pressure Monitoring Data.
The shaded portion indicates the sleep period. This patient had 8 measurements recorded during sleep and 29 measurements while awake. The overall average is 130/79 mm Hg. Awake average is 134/82 mm Hg, and sleep average is 115/70 mm Hg, for a nocturnal systolic BP dip of 14%.
Both hardware and software considerations are important for successful and optimally informative implementation of ambulatory blood pressure monitoring. First, monitors should be validated according to internationally accepted protocols. The International Protocol of the European Society of Hypertension20,21 is now the protocol that is used most commonly for the independent validation of devices.22 Second, while it is essential that appropriate hardware be utilized, it is equally, and arguably more, important that appropriately informative software be employed.23
Several papers provide informative summaries of ambulatory blood pressure monitoring techniques.7,23–25 Considerably more detailed discussion can be found in the European Society of Hypertension's 2013 position paper on ambulatory blood pressure monitoring.14
PREDICTION OF CLINICAL OUTCOMES
In a seminal study, Perloff and colleagues26 examined follow-up data for more than 1,000 hypertensive individuals who had initially been evaluated with both office measurements and ambulatory blood pressure monitoring: both sexes were equally represented. The mean (±SD) initial office blood pressures were 161.2±22.6/100.7±12.1 mm Hg, and the mean ambulatory blood pressures were 145.6±22.3/91.5±13.7 mm Hg. Ambulatory blood pressure monitoring was found to be an independent prognostic indicator when assessing the overall risk profile of individual patients: those patients whose ambulatory blood pressure monitoring values were higher than predicted via regression analysis from their office blood pressure measurements (systolic blood pressure ≥ 10 mmHg higher or diastolic blood pressure ≥ 6 mmHg higher) had statistically significantly higher cumulative mortality and morbidity over 10 years than those whose ambulatory blood pressure monitoring values were lower than predicted (systolic blood pressure ≥ 10 mmHg lower or diastolic blood pressure ≥ 6 mmHg lower). These findings extended research by the same group demonstrating that among patients with similar office blood pressure measurements, those with relatively higher ambulatory blood pressure monitoring values had a greater prevalence of target-organ damage, including retinopathy and left ventricular hypertrophy. Ambulatory blood pressure monitoring was therefore considered superior to traditional office blood pressure measurements in this regard.26Across the subsequent three decades, other data have supported these authors' assertion of ambulatory blood pressure monitoring's superiority in predicting various outcomes.
Mancia and colleagues27 provided longitudinally controlled evidence across 12 months that ambulatory blood pressure monitoring better predicted antihypertensive treatment-induced regression of left ventricular hypertrophy than did clinic blood pressure. Verdecchia and colleagues28 provided extended discussions of the clinical applicability of results from longitudinal studies.
CLINICAL PRACTICE
Ambulatory blood pressure monitoring may be differentially useful in clinical practice according to whether or not an individual patient is being treated for hypertension.28 For untreated patients who have a clinical diagnosis of high blood pressure based on office readings, ambulatory blood pressure monitoring can categorize individuals at various levels of cardiovascular risk that would not be possible on the basis of the office readings alone: these risks may be low (the patient is demonstrating white-coat hypertension: see discussion shortly) or high (the patient is demonstrated sustained hypertension). Such determination of risk is a key factor in the clinical decision to commence antihypertensive treatment.29 For patients who have started antihypertensive treatment, ambulatory blood pressure monitoring facilitates individual tailoring of treatment regimens, which can be particularly helpful in cases of apparent drug resistance, excessive variability in multiple clinical readings, symptoms of hypotension despite apparently normal clinic blood pressure readings, and marked discrepancies between in-office and out-of-office blood pressure readings.28
While noting these strengths of ambulatory blood pressure monitoring, it should be made clear that we are not recommending broad ambulatory blood pressure monitoring should completely replace clinic blood pressure assessments.
White-coat Hypertension
White-coat hypertension is the phenomenon whereby certain individuals who are not on antihypertensive medication show elevated blood pressure in a clinical setting but show a non-elevated blood pressure average when assessed by ambulatory blood pressure monitoring:30 it occurs in 15%–30% of individuals with elevated office blood pressure readings.31 White-coat hypertension is more frequent in various categories of patients, including older adults, women, nonsmokers, and individuals without evidence of target organ damage.31 The misdiagnosis of white-coat hypertension as true hypertension has various undesirable consequences, including patients unnecessarily taking chronic medications, at considerable expense, with potentially seriously debilitating side effects.31, 32 Based on the finding that ambulatory blood pressure monitoring was the most cost-effective strategy for the diagnosis of hypertension because it avoids unnecessary treatment of white-coat hypertension,32 United Kingdom guidelines now recommend ambulatory blood pressure monitoring for all patients before diagnosing hypertension.9 The identification of occurrences of white-coat hypertension via ambulatory blood pressure monitoring therefore has considerable benefits at both the individual patient and the public health levels.
Consider the following case study. Mrs. Smith (pseudonym) is a 45 year-old, generally healthy woman who presents to clinic as a new patient for a “routine checkup.” Except for an elevated clinic blood pressure that was 152/92 mm Hg at check-in when taken by the medical assistant and 150/95 mm Hg when taken manually by the physician, the physical exam is unremarkable. The patient reports that, in the past, she has taken her blood pressure using her mother’s home blood pressure monitor, and her values are “always below 140/90 [mm Hg].” Mrs. Smith asks you about whether she needs further evaluation or treatment. In this case, performing ambulatory blood pressure monitoring to exclude white-coat hypertension before commencing antihypertensive treatment would be advantageous.
White-coat Effect in Resistant Hypertension
A white-coat effect can also occur in patients with treated hypertension, and is particularly relevant to the evaluation of patients with possible resistant hypertension. Many patients appear to have resistant hypertension based on their office blood pressure measurements but actually have controlled blood pressure when assessed by ambulatory blood pressure monitoring. In one study of over 600 patients with uncontrolled office blood pressure (i.e., >140 mmHg systolic blood pressure or >90 mmHg diastolic blood pressure), nearly 40% of those on one or two medications and almost 30% of those on three medications had controlled blood pressure on ambulatory blood pressure monitoring.33 In a Spanish study of over 8,200 patients with resistant hypertension, 38% were attributed to white-coat effect based on ambulatory blood pressure monitoring.34 Thus, ambulatory blood pressure monitoring is indicated for patients suspected of having resistant hypertension before increasing doses of current medications or adding additional blood pressure-lowering medication. See White et al35 for more detailed discussion of the use of ambulatory blood pressure monitoring in the diagnosis and treatment of resistant hypertension.
Masked Hypertension
Masked hypertension is the phenomenon whereby certain individuals who are not on antihypertensive medication show non-elevated blood pressure in a clinical setting but show high blood pressure when out of the office, typically assessed by ambulatory blood pressure monitoring: approximately 15–30% of adults with non-elevated office blood pressure have masked hypertension.36 Since masked hypertension is associated with increased risks of cardiovascular morbidity and mortality, clinic readings may therefore underestimate an individual's cardiovascular risk.7 For example, left ventricular mass index and carotid plaque are similar between people with masked hypertension and those with sustained hypertension.37,38 A meta-analysis of 7 studies including a total of 11,502 participants followed over 8 years showed a two-fold higher incidence of cardiovascular disease events (HR = 2.00; 95% CI 1.58–2.52) in people with masked hypertension compared with those with normal blood pressure (i.e., normal clinic blood pressure and normal ambulatory blood pressure monitoring averages).39
Antihypertensive treatment may be warranted in patients with masked hypertension, but there are currently no randomized trials that have evaluated this strategy, and the best method to identify people with masked hypertension has not been established. There is a substantial diagnostic overlap between prehypertension and masked hypertension. In one study, 83.8% of participants with masked hypertension had prehypertension and 34.1% of participants with prehypertension had masked hypertension: the prevalence of masked hypertension was only 3.9% in participants with normal clinic blood pressure (<120/80 mm Hg).40 Evidence-based guidelines for detecting, evaluating, and managing masked hypertension are needed.
LIMITATIONS OF AMBULATORY BLOOD PRESSURE MONITORING
The limitations of ambulatory blood pressure monitoring include potential discomfort during nighttime periods, the reluctance of some patients to undergo ambulatory blood pressure monitoring especially for repeat measurement, occasionally not being able to detect genuine artefactual measurements, and the limited available of ambulatory blood pressure monitoring in general practice.16 Reimbursement issues are a considerable contributor to ambulatory blood pressure monitoring's limited availability in some regions, including the United States, where the only currently reimbursable indication from Medicare is suspected white-coat hypertension: private insurers have more indications, but these vary from carrier to carrier. Many countries outside the United States do not provide any reimbursement.16
However, while it is true that the cost of ambulatory blood pressure monitoring equipment will likely be more expensive than a simple cuff blood pressure measurement in the short term, it may be more cost effective in the long term because of the avoidance of multiple clinic visits during which cuff blood pressure readings would be obtained and the cost savings from not treating patients who do not actually need antihypertensive medication since white-coat hypertension was ruled out by early ambulatory blood pressure monitoring. As previously noted, this rationale, discussed by Lovibond et al,32 formed the basis of the United Kingdom's 2011 guidelines for the clinical management of primary hypertension in adults.9 Cost-effectiveness and reimbursement issues concerning ambulatory blood pressure monitoring in the United States have certainly been discussed in the literature,41–44 and evidence of cost-effectiveness reported. However, reimbursement is still a difficult issue. As Bloch and Basile44 observed, "Even if we believe that routine use of [ambulatory blood pressure monitoring] will better secure the diagnosis of hypertension and save money in the long-run, there is simply no group that is appropriately incentivized to make the needed short-term investment required to make it practical in our system." It is nonetheless hoped that, over time, changes in reimbursement structures may facilitate the wider use of ambulatory blood pressure monitoring.
Not all hypertension guidelines contain information on the use of ambulatory blood pressure monitoring, which may lead physicians who tend to rely on a particular guideline that does not contain this information to believe that ambulatory blood pressure monitoring is not of importance in their clinical practice. Such guidelines include the recent report from the JNC 8 panelists,45 who noted in the Supplemental Information available on-line that their report does not comment on ambulatory blood pressure monitoring because it was not used in the randomized controlled trials used in their evidence review, and "conducting a separate evidence-based review to look at this issue was beyond the scope" of their report.46
Potential Solutions
While the large majority of patients with hypertension are managed in primary care settings, primary care doctors may be able to refer their patients to an external service, including specialist clinics and pharmacy-based services.16
The European Society of Hypertension has established accredited Centres of Excellence in hypertension,47 and the American Society of Hypertension has designated certain centers as Hypertension Centers that are well-placed to assist patients with difficult-to-treat hypertension and their health care providers.48 These initiatives "can ensure the application of [ambulatory blood pressure monitoring] in many patients with complex hypertension."14
One study conducted in Ireland to explore additional ways to increase accessibility to ambulatory blood pressure monitoring compared data from patients attending primary care sites with those attending pharmacies between 2007 and 2013.49 The blood pressure characteristics of patients with ambulatory blood pressure recorded in pharmacies were similar to those recorded in primary care practice settings, supporting the feasibility of performing ambulatory blood pressure monitoring in pharmacies, thus increasing availability of the technique to the large hypertensive population.
With regard to educating primary care physicians about ambulatory blood pressure monitoring and clinical practice guidelines related to its employment, greater outreach and educational activities by hypertension professional societies may be helpful. This could be done via targeted Editorials in the societies' journals and also by increased educational opportunities at their annual meetings.
FUTURE DIRECTIONS
The practice of pharmacological chronotherapy may increase in coming years given increasing interest in this approach. Chronotherapy involves "the timing of hypertension medications to endogenous circadian rhythm determinants of the 24-h [blood pressure] pattern."50 It is now known that there are clinically meaningful treatment-time differences in responses (both therapeutically beneficial responses and adverse effects) to drugs in multiple classes: for example, calcium channel blockers are more effective when taken at bedtime than in the morning. Increasing attention is being paid to the importance of reducing sleep-time blood pressure, since mean sleep-time blood pressure is the most significant prognostic marker of cardiovascular morbidity and mortality.51 One study included over 3,000 participants during a median follow-up period of more than 5 years,51 and reported that progressive decrease in sleep-time blood pressure was the most significant predictor of event-free survival. The most beneficial time for a patient to take antihypertensive medication, perhaps evening time rather than first thing in the morning, can be determined by ambulatory blood pressure monitoring.
CONCLUSION
The technique of ambulatory blood pressure monitoring is important in the diagnosis and management of hypertension. It enables white-coat hypertension to be ruled out, thus precluding patients who do not need interventions at that time from being prescribed such intervention, while also identifying those individuals who should commence antihypertensive therapy. It also facilitates the assessment of blood pressure during sleep-time: a non-dipping pattern and nocturnal hypertension are strongly associated with increased cardiovascular morbidity and mortality. The various blood pressure categorizations afforded by ambulatory blood pressure monitoring are valuable for clinical management of high blood pressure since they increase accuracy for diagnosis and the prediction of cardiovascular risk.
Clinical Significance.
Ambulatory blood pressure monitoring allows BP readings to be taken across a 24-hour period.
Several guidelines exist for the use of ambulatory blood pressure monitoring in clinical practice.
Using ambulatory blood pressure monitoring to rule out white-coat hypertension prevents patients from being prescribed unnecessary antihypertensive medications.
Ambulatory blood pressure monitoring also allows measurement of nocturnal BP, an increasingly important prognostic parameter for cardiovascular disease risk.
Acknowledgments
All authors had a significant role in the conceptualization and writing of this manuscript. There are no funding sources to declare. Dr Turner has declared that he is an employee of Quintiles, a pharmaceutical services company: he does not own any stock in the company. No specific products of any kind are named in the manuscript. Dr. Viera has declared that he has served on the Medical Advisory Board for Suntech Medical, and has received grant funding from the National Heart Lung and Blood Institute to study ambulatory blood pressure monitoring. Dr Shimbo has declared that he has received grant funding from the National Heart Lung and Blood Institute to study ambulatory blood pressure monitoring.
None.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Horton R. GBD 2010: Understanding disease, injury, and risk. Lancet. 2013;380:2053–2054. doi: 10.1016/S0140-6736(12)62133-3. [DOI] [PubMed] [Google Scholar]
- 2.Das P, Samarasekera U. The story of GBD 2010: a "super-human" effort. Lancet. 2013;380:2067–2070. doi: 10.1016/s0140-6736(12)62174-6. [DOI] [PubMed] [Google Scholar]
- 3.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Go AS, Mozaffarian D, Roger VL, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart and stroke statistics--- 2014 update. A report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Winter KH, Tuttle LA, Viera AJ. Hypertension. Prim Care. 2013;40:179–194. doi: 10.1016/j.pop.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 6.Turner JR, Hoofwijk TJ. Clinical trials in new drug development. J Clin Hypertens (Greenwich) 2013;15:306–309. doi: 10.1111/jch.12085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pickering T, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N Eng J Med. 2006;354:2368–2374. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- 8.Krakoff LR. Ambulatory blood pressure improves prediction of cardiovascular risk: implications for better antihypertensive management. Curr Atheroscler Rep. 2013;15:317. doi: 10.1007/s11883-013-0317-9. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence. Clinical Guideline 127. [Accessed 20th June 2014];Hypertension: clinical management of primary hypertension in adults. 2011 Aug; Available at http://guidance.nice.org.uk/CG127/Guidance. [Google Scholar]
- 10.National Heart Foundation and High Blood Pressure Research Council of Australia Ambulatory Blood Pressure Monitoring Consensus Committee. Ambulatory blood pressure monitoring. Aust Fam Physician. 2011;40:877–880. [PubMed] [Google Scholar]
- 11.Campbell NR, Hemmelgarn BR. New recommendations for the use of ambulatory blood pressure monitoring in the diagnosis of hypertension. CMAJ. 2012;184:633–634. doi: 10.1503/cmaj.110501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Japanese Circulation Society Joint Working Group. Guidelines for the clinical use of 24 hour ambulatory blood pressure monitoring (ABPM) (JCS 2010): Digest version. Circ J. 2012;76:508–519. doi: 10.1253/circj.cj-88-0020. [DOI] [PubMed] [Google Scholar]
- 13.International Society for Chronobiology; American Association of Medical Chronobiology and Chronotherapeutics; Spanish Society of Applied Chronobiology, Chronotherapy, and Vascular Risk; Spanish Society of Atherosclerosis; Romanian Society of Internal Medicine. Hermida RC, Smolensky MH, Ayala DE, Portaluppi F. 2013 ambulatory blood pressure monitoring recommendations for the diagnosis of adult hypertension, assessment of cardiovascular and other hypertension-associated risk, and attainment of therapeutic goals. Chronobiol Int. 2013;30:355–410. doi: 10.3109/07420528.2013.750490. [DOI] [PubMed] [Google Scholar]
- 14.O'Brien E, Parati G, Stergiou G, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–1768. doi: 10.1097/HJH.0b013e328363e964. [Erratum: J Hypertens. 2013;31:2467] [DOI] [PubMed] [Google Scholar]
- 15.Flynn JT, Daniels SR, Hayman LL, et al. on behalf of the American Heart Association Atherosclerosis, Hypertension and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young. Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension. 2014;63:1116–1135. doi: 10.1161/HYP.0000000000000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parati G, Stergiou G, O'Brien E, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014 May 30; doi: 10.1097/HJH.0000000000000221. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Liu W, Ye H, Tang B, et al. Comparison of 44-hour and fixed 24-hour ambulatory blood pressure monitoring in dialysis patients. J Clin Hypertens (Greenwich) 2014;16:63–69. doi: 10.1111/jch.12217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ray GM, Nawarskas JJ, Anderson JR. Blood pressure monitoring technique impacts hypertension treatment. J Gen Intern. Med. 2012;27:623–629. doi: 10.1007/s11606-011-1937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Powers BJ, Olsen MK, Smith VA, Woolson RF, Bosworth HB, Oddone EZ. Measuring blood pressure for decision making and quality reporting: where and how many measures? Ann Intern. Med. 2011;154:781–788. W-289–W-290. doi: 10.7326/0003-4819-154-12-201106210-00005. [DOI] [PubMed] [Google Scholar]
- 20.O’Brien E, Pickering T, Asmar R, et al. on behalf of the Working Group on Blood Pressure Monitoring of the European Society of Hypertension. International protocol for validation of blood pressure measuring devices in adults. Blood Press Monit. 2002;7:3–17. doi: 10.1097/00126097-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 21.O’Brien E, Atkins N, Stergiou G, et al. on behalf of the Working Group on Blood Pressure Monitoring of the European Society of Hypertension. European Society of Hypertension International Protocol for the Validation of Blood Pressure Measuring Devices in Adults. 2010 Revision. Blood Press Monit. 2010;15:23–38. doi: 10.1097/MBP.0b013e3283360e98. [DOI] [PubMed] [Google Scholar]
- 22.Stergiou G, Karpettas N, Atkins N, O’Brien E. European Society of Hypertension International Protocol for the validation of blood pressure monitors: A critical review of its application and rationale for revision. Blood Press Monit. 2010;15:39–48. doi: 10.1097/MBP.0b013e3283360eaf. [DOI] [PubMed] [Google Scholar]
- 23.O'Brien E. First Thomas Pickering Memorial Lecture: ambulatory blood pressure measurement is essential for the management of hypertension. J Clin Hypertens (Greenwich) 2012;14:836–847. doi: 10.1111/j.1751-7176.2012.00698.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giles TD, Black HR, Messerli F, White WB. Ambulatory blood pressure monitoring should be included in the National Health and Nutritional Examination Survey (NHANES) J Am Soc Hypertens. 2012;6:364–366. doi: 10.1016/j.jash.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 25.Campbell P, Ghuman N, Wakefield D, Wolfson L, White WB. Long-term reproducibility of ambulatory blood pressure is superior to office blood pressure in the very elderly. J Hum Hypertens. 2010;24:749–754. doi: 10.1038/jhh.2010.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perloff D, Sokolow M, Cowan R. The prognostic value of ambulatory blood pressures. JAMA. 1983;249:2792–2798. [PubMed] [Google Scholar]
- 27.Mancia G, Zanchetti A, Agabiti-Rosei E, et al. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment-induced regression of left ventricular hypertrophy. Circulation. 1997;95:1464–1470. doi: 10.1161/01.cir.95.6.1464. [Erratum, Circulation 1997;96:1065.] [DOI] [PubMed] [Google Scholar]
- 28.Verdecchia P, Angeli F, Cavallini C. Ambulatory blood pressure for cardiovascular risk stratification. Circulation. 2007;115:2091–2093. doi: 10.1161/CIRCULATIONAHA.107.697086. [DOI] [PubMed] [Google Scholar]
- 29.Verdecchia P, Angeli F. How can we use the results of ambulatory blood pressure monitoring in clinical practice? Hypertension. 2005;46:25–26. doi: 10.1161/01.HYP.0000170139.90918.50. [DOI] [PubMed] [Google Scholar]
- 30.Pickering TG, James GD, Boddie C, et al. How common is white coat hypertension? JAMA. 1988;259:225–228. [PubMed] [Google Scholar]
- 31.Franklin SS, Thijs L, Hansen TW, et al. White-coat hypertension: new insights from recent studies. Hypertension. 2013;62:982–987. doi: 10.1161/HYPERTENSIONAHA.113.01275. [DOI] [PubMed] [Google Scholar]
- 32.Lovibond K, Jowett S, Barton P, et al. Cost-effectiveness of options for the diagnosis of high blood pressure in primary care: a modelling study. Lancet. 2011;378:1219–1230. doi: 10.1016/S0140-6736(11)61184-7. [Erratum: Lancet. 2011;378:1218] [DOI] [PubMed] [Google Scholar]
- 33.Brown MA, Buddle ML, Martin A. Is resistant hypertension really resistant? Am J Hypertens. 2001;14:1263–1269. doi: 10.1016/s0895-7061(01)02193-8. [DOI] [PubMed] [Google Scholar]
- 34.de la Sierra A, Segura J, Banegas JR, et al. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension. 2011;57:898–902. doi: 10.1161/HYPERTENSIONAHA.110.168948. [DOI] [PubMed] [Google Scholar]
- 35.White WB, Turner JR, Sica D, et al. Detection, evaluation, and treatment of severe and resistant hypertension: proceedings from an American Society of Hypertension Interactive Forum held in Bethesda, Maryland, USA, October 10th 2013. [accepted June 2014];J Am Soc Hypertens. doi: 10.1016/j.jash.2014.06.005. in press [Note to Editor/Reviewers: publication of this paper is being expedited, likely into the September 2014 issue.] [DOI] [PubMed] [Google Scholar]
- 36.Peacock J, Diaz KM, Viera AJ, et al. Unmasking masked hypertension: prevalence, clinical implications, diagnosis, correlates and future directions. J Hum Hypertens. 2014 Feb 27; doi: 10.1038/jhh.2014.9. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu JE, Roman MJ, Pini R, Schwartz JE, Pickering TG, Devereux RB. Cardiac and arterial target organ damage in adults with elevated ambulatory and normal office blood pressure. Ann Intern Med. 1999;13:564–572. doi: 10.7326/0003-4819-131-8-199910190-00003. [DOI] [PubMed] [Google Scholar]
- 38.Sega R, Trocino G, Lanzarotti A, Carugo S, Cesana G, Schiavina R, et al. Alterations of cardiac structure in patients with isolated office, ambulatory, or home hypertension: Data from the general population (Pressione Arteriose Monitorate E Loro Associazioni [PAMELA] Study) Circulation. 2001;104:1385–1392. doi: 10.1161/hc3701.096100. [DOI] [PubMed] [Google Scholar]
- 39.Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007;25:2193–2198. doi: 10.1097/HJH.0b013e3282ef6185. [DOI] [PubMed] [Google Scholar]
- 40.Shimbo D, Newman JD, Schwartz JE. Masked hypertension and prehypertension: diagnostic overlap and interrelationships with left ventricular mass: the Masked Hypertension Study. Am J Hypertens. 2012;25:664–671. doi: 10.1038/ajh.2012.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Krakoff LR. Cost-effectiveness of ambulatory blood pressure: a reanalysis. Hypertension. 2006;47:29–34. doi: 10.1161/01.HYP.0000197195.84725.66. [DOI] [PubMed] [Google Scholar]
- 42.Swartz SJ, Srivaths PR, Croix B, Feig DI. Cost-effectiveness of ambulatory blood pressure monitoring in the initial evaluation of hypertension in children. Pediatrics. 2008;122:1177–1181. doi: 10.1542/peds.2007-3432. [DOI] [PubMed] [Google Scholar]
- 43.Wang YC, Koval AM, Nakamura M, et al. Cost-effectiveness of secondary screening modalities for hypertension. Blood Press Monit. 2013;18:1–7. doi: 10.1097/MBP.0b013e32835d0fd3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bloch MJ, Basile JN. New British guidelines mandate ambulatory blood pressure monitoring to diagnose hypertension in all patients: not ready for prime time in the United States. J Clin Hypertens (Greenwich) 2011;13:785–786. doi: 10.1111/j.1751-7176.2011.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 46.Supplement to 2014 Evidence-based guideline for the management of high blood pressure in adults: report by the panel appointed to the Eighth Joint National Committee (JNC 8) [Accessed 1st June, 2014]; doi: 10.1001/jama.2013.284427. Available at http://jama.jamanetwork.com/article.aspx?articleid=1791497#ArticleInformation. [DOI] [PubMed] [Google Scholar]
- 47.ESH Hypertension Excellence Centres: a new strategy to combat an old foe. Blood Press. 2007;16:276–277. doi: 10.1080/08037050701549896. [DOI] [PubMed] [Google Scholar]
- 48.White WB, Kostis JB. Leadership message. American Society of Hypertension-designated centers of excellence: a new initiative. J Clin Hypertens (Greenwich) 2011;13:391–392. doi: 10.1111/j.1751-7176.2011.00466.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.James K, Dolan E, O'Brien E. Making ambulatory blood pressure monitoring accessible in pharmacies. Blood Press Monit. 2014;19:134–139. doi: 10.1097/MBP.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 50.Hermida RC, Ayala DE, Fernández JR, et al. Administration-time differences in effects of hypertension medications on ambulatory blood pressure regulation. Chronobiol. Int. 2013;30:280–314. doi: 10.3109/07420528.2012.709448. [DOI] [PubMed] [Google Scholar]
- 51.Hermida RC, Ayala DE, Mojón A, Fernández JR. Decreasing sleep-time blood pressure determined by ambulatory monitoring reduces cardiovascular risk. J Am Coll Cardiol. 2011;58:1165–1173. doi: 10.1016/j.jacc.2011.04.043. [DOI] [PubMed] [Google Scholar]