Abstract
Although there is substantial literature documenting the challenges of pediatric sickle cell disease (SCD) for children and their parents, there is limited research identifying how parents prioritize their needs and use their social networks to manage information regarding their child’s SCD in terms of physical and mental health. We examined parents’ perceived needs regarding child health issues as they relate to SCD; who and what sources of information are utilized by parents regarding SCD; the frequency with which they consult these resources; and the level at which they trust them. Parents in this study reported that mothers, physicians, the Internet, and books were key sources of support, guidance, and counsel regarding the health needs of children with SCD. These three sources were rated high in importance, trust, frequency of contact, and perceived supportiveness toward mental and physical health needs.
Keywords: pediatric sickle cell disease, social networks, parents, child health needs
Introduction
Sickle cell disease (SCD) is a genetic disorder occurring in about 1 in 500 African American births in the United States1. Pediatric SCD contributes to multiple challenges in physical and mental health. As a result of SCD, children experience physical symptoms ranging from fever, anemia, and pain (musculoskeletal and abdominal) to stroke, acute chest syndrome, and restrictive lung disease among many other acute and chronic physical manifestations2. For children with a chronic illness, the potential for developing mental health disorders, including depression and anxiety is high3–5. (In the case of SCD, children may experience stigma and shame because of the disease, feel a lack of support from peers without SCD, and develop overwhelming stress and anxiety about the uncertainty associated with the disease and the impact that unanticipated pain and illness have on daily living and personal development)6–9.
Pediatric SCD also places many complex demands on parents/caregivers. Parents of children with SCD report that the disease greatly impacts them personally and within their families including through disruptions friendships, family activities, regular routines, and relationships10. The same appears to hold true for other chronic conditions11. Parents of children with SCD report being drained and facing distress especially during chronic phases of the illness or during pain episodes10,12–14. Social support is seen as an effective coping mechanism for parents of a child with SCD15 and can serve as a buffer during especially stressful disease-related events16. Social support in this case is viewed from a sociological perspective to include the relational aspects of the social network (i.e., groups, community, family ties).17
In the U.S., SCD primarily affects African Americans, and therefore the social and cultural context of the target population must be considered. African American children in the U.S. are likely to live in families with lower income and in poverty18 and to have limited access to traditional health and mental health resources, including a medical care home19. It has also been established that African American families tend to place emphasis on the extended familial networks,20–23 particularly when there is a chronically ill child in the family24,25. Although kinship support is culturally and socially meaningful for African-American families, this support is often necessary to balance the emotional and logistical demands of chronic illness management10. Despite the fact that parents of children with SCD may rely on their extended kin for support, feelings may not always be reciprocated. For example, in one study, parents of children with SCD perceived a decline in supportive kin after the child’s SCD diagnosis26. Further, some caregivers of children with SCD have reported increased isolation27.
Although there is substantial literature documenting the challenges of pediatric SCD for children and their parents, there is limited research identifying how parents prioritize their needs and use their social networks to manage information regarding their child’s SCD in terms of physical and mental health.
Such research can assist health providers not only in understanding how the social network is structured in terms of social support and resources related to SCD, but also in transmitting accurate information about SCD to important members of the network. This could improve provider communication with families, particularly so-called hard-to-reach families and those who may communicate about their child’s health via non-traditional channels (e.g., with other families, with pastors, via the Internet). Ultimately, understanding families’ broader networking could reduce health disparities in terms of health care access by providing information and interventions through multiple channels not just at the doctor’s office/clinic. This study identifies the needs of parents regarding the physical and mental health of their children and gives important information about social relationships in terms of the structure/mapping of social networks, the support received from others, the quality and quantity of social interactions, and feelings of isolation and loneliness. All of these social relationship factors play essential roles in parental health and well-being,28 which affects the health and well-being of their children with SCD15.
One way to measure social and community relationships and support is to map the important relationships between people and their social networks. The techniques of Social Network Analysis offer the possibility of new insights into the structure of relationships for parents of children with SCD. Specifically, social network analysis can portray in a single map both the type of relationships parents have around their children’s SCD and the people/organizations within the community with whom parents relate regarding their child’s SCD.
The purpose of this study is to understand more thoroughly the social support network of parents of children with SCD in one Midwestern city (that is, to understand to whom or what sources these parents turn for guidance and support and the corresponding quantity and quality of this support network). The following research questions were examined: 1) What needs regarding child health issues as it relates to SCD do parents perceive? and 2) Whom and what sources of information do parents consult regarding SCD; what is the frequency with which they consult them; and how much do they trust them?
Methods
Participants
Sixty parents of children with SCD completed questionnaires. All parents were African American and lived in the targeted large Midwestern city and its surrounding metropolitan area.
Measures
Parents of children with SCD were asked to complete two questionnaires during an Annual Sickle Cell Research and Education Day event)29. The first questionnaire, created by investigators, included demographic questions such as parent age, gender, highest grade completed, household income level, relationship to child with SCD, number of children they care for with SCD, and the children’s ages. The questionnaire also contained five open-ended questions about the parents’ perception of child health needs (e.g., What are the most important needs you have regarding your child’s health? What is your largest physical/mental/spiritual health need for your child? What would help you to improve the overall health of your child?).
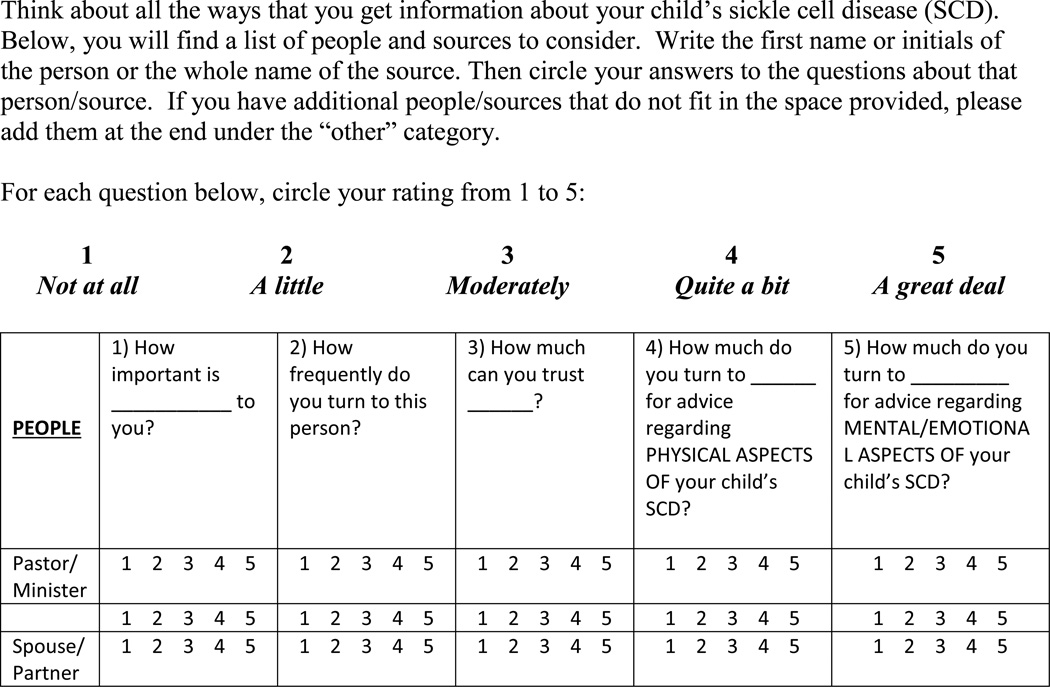
Second, parents responded to a network questionnaire that is a modification of the Norbeck Social Support Questionnaire (NSSQ).30. The modified NSSQ assessed quantity (number and frequency of contacts) and quality (perceived supportiveness) of parents’ social support networks regarding their children’s SCD. Participants were asked to indicate characteristics of support for possible network members or sources. Ten people (e.g., pastor, spouse, mother, physician) and four sources (Internet, television, books, support groups) were listed and participants could add any other people or sources not listed. Following each possible network member of source were five questions including length of time known, frequency of contact, trust in and importance of the relationship, and perceived supportiveness toward physical and mental health of their child (see Figure 1). The original NSSQ has high test-retest reliability (.85 to .92) and excellent internal consistency (alphas above .85)31. Predictive validity has also been established with the original NSSQ in a sample of low-income minority women31. The current modification of the NSSQ has not been used in other studies but is similar in design and concept to the original, and we would not expect our modifications to alter the psychometric properties of the instrument. In fact, our modifications add specificity to the questions about the particular social network applicable to parents who have children with SCD. We believe this enhances the face validity of the measure for the purpose of this study.
Figure 1.
Network Questionnaire example questions from modified NSSQ
Procedure
As stated previously, parents of children with SCD were recruited as part of an Annual Sickle Cell Research and Education Day. During the event, the project was verbally explained to parents and they were given a consent form which outlined the study, the risks, benefits, alternatives, confidentiality, compensation, who to contact, and that the study was voluntary. Parents received $20 as compensation for their time. Because the information collected was de-identified, this study was exempted by the Institutional Review Board.
Data
The data collected on the network questionnaire included: 1) the respondent; 2) the resource they rated (e.g., pastor, physician, spouse); and 3) the characteristics of the resource (e.g., importance, trust, frequency of contact, and perceived supportiveness toward physical and mental health). Respondents rated the characteristics of the resources on a 5 point scale (see Figure 1 for an example of the questionnaire). Upon examination of the raw data, it became obvious that respondents perceived the relationship between resource and characteristic as dichotomous. In other words, there was either no relation (or little relation) between the resource and characteristic as perceived by the parent, or the relation was rated high. Therefore, we chose to dichotomize the ratings, and coded all values of 4 and 5 as indicative of a relation and all other values as 0. This resulted in a binary matrix for each respondent of resources by characteristics. Since we were interested in mapping the relationships of resources and the characteristics of the different resources, we summed the data for each parent into a single contingency table of resources and characteristics which was used in subsequent analyses (see Table 1). Dichotomizing the values has the effect of reducing the variance in the data and, as a result, risks that the nuance will be missed. The risk was an acceptable compromise for understanding the network in this case since respondents did not use the full range of the scale presented.
Table 1.
Contingency Table of Resources and Characteristics
| Frequency | Importance | Mental | Physical | Trust | |
|---|---|---|---|---|---|
| Pastor | 1 | 7 | 4 | 2 | 6 |
| Spouse | 17 | 18 | 13 | 12 | 15 |
| Mother | 19 | 22 | 19 | 16 | 21 |
| Father | 6 | 10 | 6 | 5 | 7 |
| Sister | 3 | 3 | 2 | 2 | 2 |
| Other family | 12 | 15 | 11 | 11 | 13 |
| Daughter | 3 | 3 | 3 | 3 | 3 |
| Grandmother | 2 | 2 | 2 | 2 | 2 |
| Neighbor | 2 | 2 | 2 | 2 | 2 |
| Friend | 6 | 12 | 8 | 9 | 12 |
| Co-worker | 3 | 5 | 4 | 5 | 6 |
| Physician | 22 | 27 | 18 | 24 | 25 |
| Nurse | 4 | 4 | 4 | 4 | 4 |
| Counselor | 3 | 5 | 5 | 3 | 5 |
| TV | 3 | 4 | 1 | 0 | 2 |
| Books | 7 | 13 | 7 | 10 | 14 |
| Internet | 11 | 12 | 8 | 9 | 10 |
| Support group | 8 | 8 | 7 | 7 | 8 |
| Other | 6 | 7 | 6 | 7 | 8 |
Values in the cells of the table are frequencies representing the number of parents (N=60) that indicated that they would utilize a specific resource (e.g., pastor physician) to meet a specific characteristics (e.g., trust, importance, mental health support).
Data Analysis
To uncover network structures and interrelationships, data in the contingency table were analyzed using the method of social network analysis32. To create a network map, data were analyzed using correspondence analysis33 in order to position the resources and characteristics in a two-dimensional map. Correspondence analysis calculates x,y coordinates for each element of the columns in a contingency table.34 Ucinet software35 was used to quantify characteristics of the network. Data from Ucinet was entered into NetDraw software36 to provide visual displays of the network of relationships.
Qualitative data analysis was used with open-ended questions. Following a standard qualitative research procedure based on grounded theory, three members of the research team independently reviewed the answers to open-ended questions and distilled the answers into a manageable number of themes37. The final themes were checked by the research team for clarification, consensus and validation.
Results
Demographics of participants
Eight-eight percent were mothers of children with SCD; 32% of the parents had completed some college. The mean age of respondents was 35.9 years (SD=8.1). Household income levels (before taxes) varied: 25% reported under $10,000; 12% $10,000–$19,999; 17% $20,000–$29,999; 13% $30,000–$39,999, 5% $40,000–$49,999; 10% $50,000–$74,999 and 13% above $74,999. The mean age of the children as 10 years and the vast majority of parents (80%) indicated that they cared for only one child with SCD. See Table 2 for details on demographic characteristics.
Table 2.
Demographic Information About Respondents and Their Children
| Variable | N | Percent |
|---|---|---|
| Respondents | ||
| Respondents’ Relation to Child | 53 | 88 |
| Mother | 2 | 3 |
| Grandmother | 2 | 3 |
| Aunt | 1 | 2 |
| Father | 1 | 2 |
| Stepfather | 1 | 2 |
| Sister | ||
| Age of Respondent | ||
| 18–19 years | 2 | 3 |
| 24–30 years | 12 | 20 |
| 31–40 years | 29 | 48 |
| 41–50 years | 13 | 22 |
| 51–70 years | 2 | 3 |
| Missing | 2 | 3 |
| Respondent’ Highest Level of Education | ||
| Junior High | 3 | 5 |
| Partial High School | 11 | 18 |
| High School Graduate or GED | 8 | 13 |
| Some College | 19 | 32 |
| College Graduate | 13 | 22 |
| Graduate School/Professional Degree | 5 | 8 |
| Missing | 1 | 2 |
| Household Income (before taxes) | ||
| Under 10K | 15 | 25 |
| 10K–$19,999 | 7 | 12 |
| 20K–29K | 10 | 17 |
| 30K–39K | 8 | 13 |
| 40K–49K | 3 | 5 |
| 50K–$74,999 | 6 | 10 |
| Above $74,999 | 8 | 13 |
| Missing | 3 | 5 |
| Number of Children with Sickle Cell Disease | ||
| 1 child | 48 | 80 |
| 2 children | 12 | 20 |
| Children’s Ages | ||
| Child 1 | ||
| Age 1–5 years | 6 | 10 |
| Age 6–10 years | 16 | 27 |
| Age 11–15 years | 23 | 38 |
| Age 16–20 years | 10 | 17 |
| Missing | 5 | 8 |
| Child 2 | ||
| No Second Child | 48 | 80 |
| Age 1–5 years | 3 | 5 |
| Age 6–10 years | 5 | 8 |
| Age 11–15 years | 4 | 7 |
| Age 16–20 years | 0 | 0 |
| Missing | 0 | 0 |
Themes from open-ended questions
In terms of physical health needs for their children, parents indicated that medication-related issues were their greatest need followed by leg pain and staying healthy in general. Regarding mental health needs for their children, fitting in/peer group socialization and the child staying focused were the most common responses. For spiritual health needs for their children, knowing God and praying were the most frequent reported needs. Although parents in this study named many topics that they would like to learn more about, the most common were healthy lifestyle habits (such as eating and sleep and pain management). See Table 3 for the top five health topics prioritized by parents. Parents indicated anticipated resources for each aspect of their child’s health—health care providers for physical health (75%) and mental health (45%) and ministers/priests for spiritual health (42%). Interestingly, parents reported family/relatives as the secondary resource for each area of child health needs—physical health (21%); mental health (37%); and spiritual health (40%).
Table 3.
Parents’ Prioritized Health Topics
| Health Topics | Percentage of Parents Indicating Topic of Interest |
|---|---|
| healthy lifestyle habits (e.g., eating, vitamins, sleep, etc.) | 33% |
| pain management | 22% |
| medication-related—either specific medicines (e.g., Hydroxyurea, Ex-Jade, Penicillin) or issues with medication (e.g., coverage, trying different medicines) | 20% |
| sickle cell disease in general | 15% |
| social needs related to having a chronic illness (e.g., transportation, school support, available resources, bills, health care access) | 10% |
Visualizing the Social Network
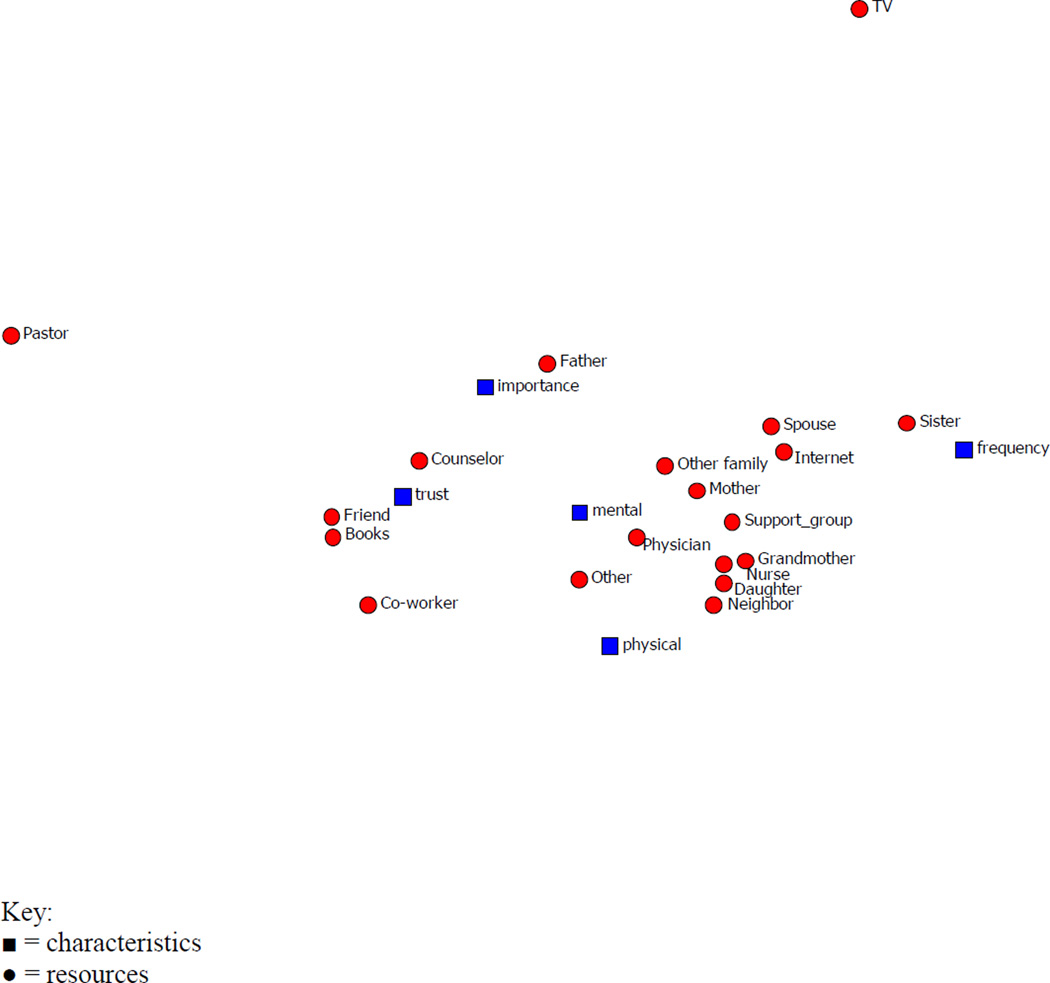
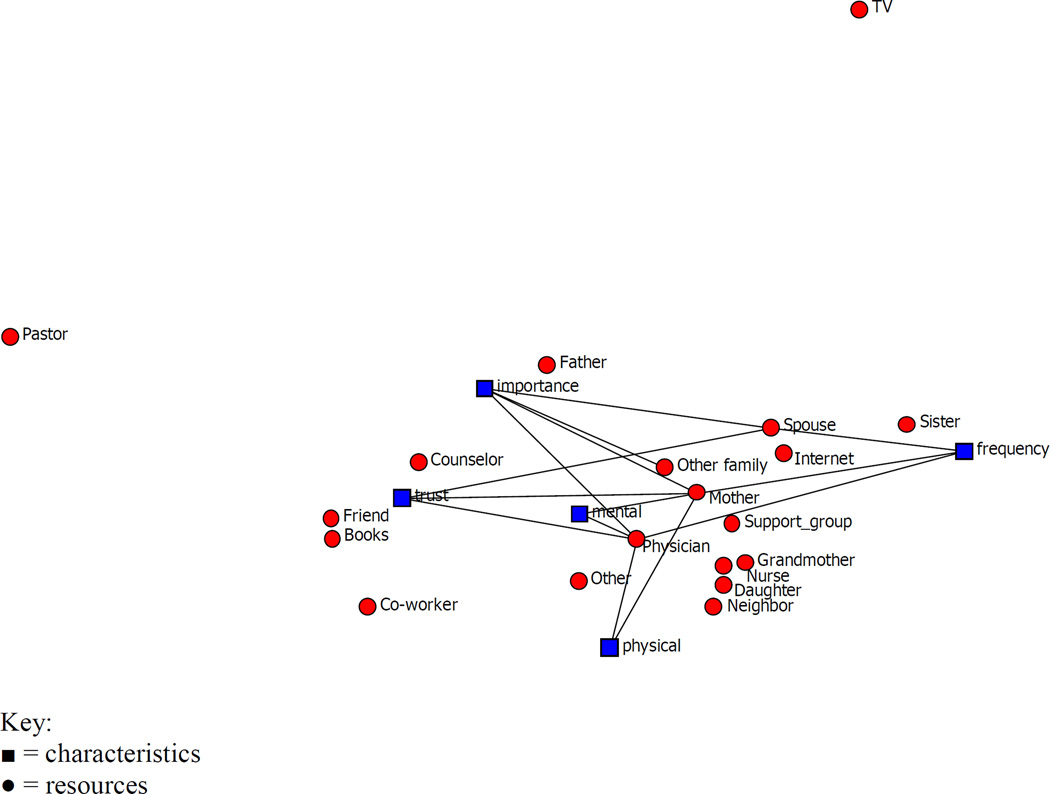
Figure 2 displays the results of the correspondence analysis for the contingency table and shows the position of points for both resources and characteristics. The variance accounted for in this two-dimensional solution from the correspondence analysis was 84.2% Output from the analysis (see Figure 2) positions resources that are similar to each other closer together and the resources that are dissimilar further apart; characteristics can be viewed in the same way. We added the frequency data to the coordinates to portray the network further and this allowed us to interactively portray the links between resources and characteristics. For example, setting the frequency of interactions to a value equal to or greater than 15 connects all the resources and characteristics where the number of times a parent indicated a relationship was greater or equal to 15. At a value of 15, this represents almost half of the respondents. The map is sparse, that is, there are few lines. The lines that are present suggest these resources and characteristics were strongly connected, that is, almost half of the respondents indicated a relationship. Showing relations at this level (N=>15) provides insight into the central traits of this network. Specifically, mother, physician, other family members, and spouse are central supportive figures in the network. Further, the physician and mother connect to all characteristics whereas spouse connects only to importance and frequency (See Figure 3).
Figure 2.
Network Map of Resources and Characteristics
Figure 3.
Network Map of Resources and Characteristics with Links =>15 Parents
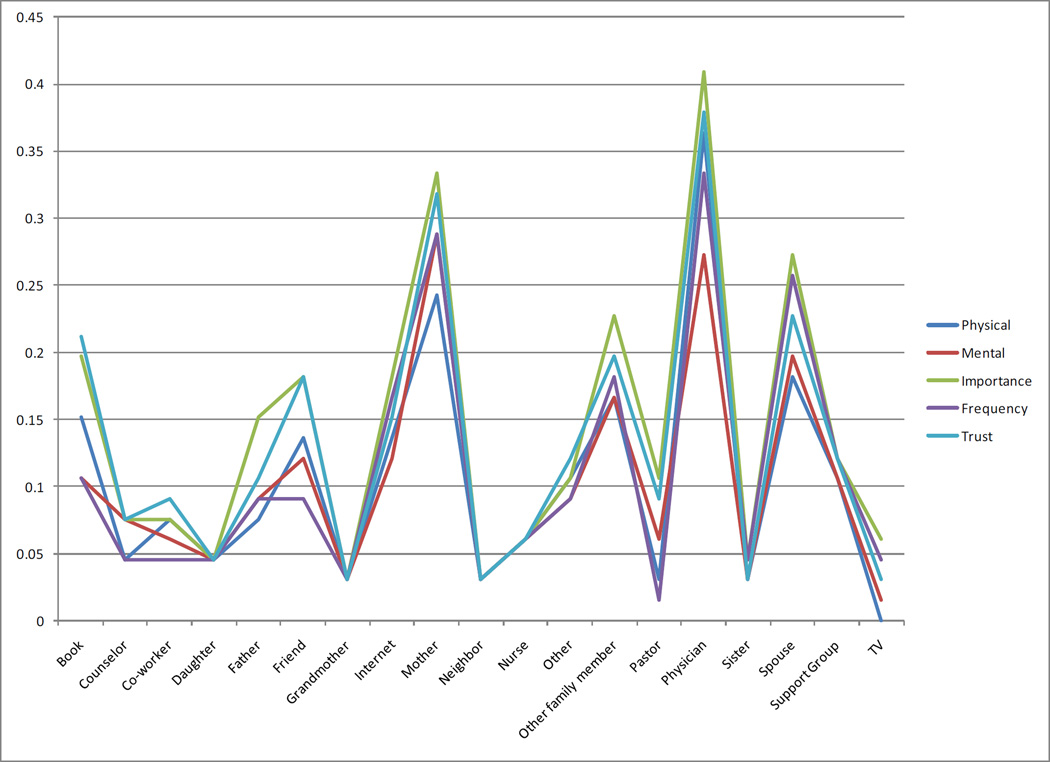
Quantifying the Social Network
In addition to visual inspection, the degree centrality of all resources was calculated for each characteristic. Degree centrality in social network terms is a measure of network activity in terms of the number of connections--in our case, between resources and characteristics38. Characteristics with a large number of connections would have a high value for centrality; conversely, characteristics with fewer connections would have a low value. While the number of connections can be portrayed, as in Figure 3, calculating centrality quantifies and makes visual inspection more precise. The analysis assessed centrality for each characteristic. The responses for each person were summed for each characteristic resulting in a respondent by resource contingency table for each characteristic. This allowed us to examine whether centrality changes based on whether a respondent was considering trust, importance, or some other characteristic. Figure 4 illustrates the degree centrality of the network for resources by each of the five characteristics. This means that resources that are high on degree centrality will likely be used regardless of whether the concern is trust in the resource, importance of the resource, the content of the resource (e.g., physical information) or something else. For example, as resource, physician is high regardless of the issue and past is low regardless of the issue.
Figure 4.
Degree Centrality for each resource within a characteristic.
Discussion
Parents of children with SCD provided information about their perceived needs relating to SCD and about where they go for information regarding their child’s illness. In general, parents of children with SCD in this study indicated a desire to learn more and know more regarding all aspects of their child’s SCD. Although health topics are of particular interest to parents (e.g., medications), there was wide variability in answers across parents.
In other research studies comprising mostly African American samples, extended family networks are reported as an important resource in providing emotional, social, and logistical support to parents of chronically ill children.39–41 In this study, we found support for extended family networks as an important resource and also gained a more nuanced understanding of family support. Specifically, regarding social support, participants in this study indicated that mothers were a key source of support, guidance, and counsel regarding the health needs of children with SCD. Across respondents, the relationship with the mother was rated high in importance, trust, frequency of contact, and perceived supportiveness toward mental and physical health needs. This finding alone warrants further investigation because of the undue burden and stress that mothers may be experiencing as they care for children with SCD. It is strongly supported in the literature that mothers of children with chronic illness, compared with other family members, experience higher rates of depression, burn-out, psychological distress, and perceived burdens.42–45
From analysis of the frequencies with which various health care professionals are considered to meet their child’s health needs, participants reported that they are more likely to turn to physicians and less likely to rely on nurses. Across all characteristics of support, the physician was rated as a key source of support for meeting the health needs of the child with SCD. This finding was a bit surprising to us given that interactions with the actual physician don’t occur as frequently as interactions with other health professionals (such as nurses). However, this may reflect parents’ respect for positions of authority and a “doctor knows best” attitude. Additionally, the high ratings for physicians could be related to confusion about the roles of health professionals and who is the doctor. Several key studies highlight that patients often do not understand the role or duties of various health care providers, especially in large teaching centers where multiple handoffs are possible and in which various levels of physicians including attendings, residents, fellows, and medical students46,47. Although nurses may be generally respected by patients for their professional guidance and support, in our comprehensive and multidisciplinary clinic, it may be difficult to discern the nurse’s role in supporting physical and mental health independently of the physician, social worker, and psychologist.
Interestingly, the respondent’s spouse was seen as an important, trusting, and frequent source of support, but not rated as highly on perceived supportiveness for mental and physical health needs as the mother and physician. Other family members were seen as an important source of support but rated lower on other characteristics of support. This finding may reflect burn-out on the part of the spouse and other family members who are important in their familial role but viewed as less supportive of SCD-related needs.
We were surprised that the pastor and nurse were rated low for support, as spiritual coping has been identified as an important resource for African American parents of chronically ill children.48 Regarding the pastor, need for spiritual health needs was not listed separately as a health need on the social network questionnaire; the pastor may have been rated more highly if spiritual needs were explicitly included. Further, there are people who are spiritual and rely on their faith but who may not be a part of a church with a pastor.
Another interesting finding is that parents rated books and the Internet highly as sources of support for specific content (i.e., physical, mental health). Because parents are often hungry for knowledge about their child’s illness, and the Internet is increasingly accessible, parents may turn to these sources from home rather than waiting for clinic appointments to get information. Given the earlier findings about common topics of interest, there were a few topics that were mentioned more frequently but otherwise, parents have nuanced needs for information based on the specific manifestation of SCD in their child. Parents may then turn to books and the Internet to meet those particular needs since they are not likely to be covered at a general SCD education event. In addition, transportation and insurance have been cited as barriers to health care, and parents may turn to less expensive and more accessible sources of information in order to meet physical and mental health care needs.49,50
Overall, parents in this study reported looking for information from sources that are convenient, trusted, valued, and respected. Parents want to turn to someone they can trust, who is important, with whom they are in frequent contact, and someone who they perceive as supportive of both physical and mental health needs. Parents are not as likely to parcel out support characteristics and turn to someone just because they are important (e.g. family members who are important but whom they don’t trust).
These findings expand on past research that has suggested that the support systems of African American parents often include extended family members;39–41 less information has been reported previously about the perceived helpfulness of sources of support when families have a child with a chronic illness. Past research has suggested that African American parents of a child with a chronic illness have more limited support and resources form extended family members than those of European American parents. Communication about SCD is also important to social networks and family adjustment. Results of the current study suggest that parents of children with SCD are more likely to communicate about SCD with family, friends, and medical professionals whom they trust and respect.
The limitations of the study should be noted. Understanding differences in communication and reliance patterns, and hence multiple methods of communication, was not undertaken in this study but is important for future research. The study is limited by the fact that data came from participant self-report of reliance on social networks and did not include data from other sources of complementary data on health beliefs or a similar construct. This study also did not have the power to examine social networks in the context of disease severity and other medical and cultural variables (e.g. socioeconomic status). Finally, data were collected on a convenience sample of children with SCD. It is possible that patients not represented have fewer or less developed social networks preventing their ability to participate in SCD events and research.
A social network analysis may be a useful method for understanding influential social networks for parents of children with SCD. This study examined social networks in the context of parents’ health beliefs and practices. Information from this study will assist providers in targeting key members of the social network to provide them with information necessary to promote health awareness and empower positive health practices in patients with SCD. It is important to ensure that patients are getting accurate information to manage SCD through trusted and supporting relationships. Future studies are needed to examine the relationship between social networks, disease management, health, and quality of life outcomes.
References
- 1.Brousseau DC, Panepinto JA, Nimmer M, et al. The number of people with sickle-cell disease in the United States: national and state estimates. Am J Hermatol. 2010 Jan;85(1):77–78. doi: 10.1002/ajh.21570. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics/Section of Hemotology/Oncology Committee on Genetics. Health supervision for children with sickle cell disease. Pediatrics. 2002 Mar;109(3):526–535. doi: 10.1542/peds.109.3.526. [DOI] [PubMed] [Google Scholar]
- 3.Cruz I, Marciel KK, Quittner AL, et al. Anxiety and depression in cystic fibrosis. Semin Respir Crit Care Med. 2009 Oct;30(5):569–578. doi: 10.1055/s-0029-1238915. [DOI] [PubMed] [Google Scholar]
- 4.Ekinci O, Titus JB, Rodopman AA, et al. Depression and anxiety in children and adolescents with epilepsy: prevalence, risk factors, and treatment. Epilepsy Behav. 2009 Jan;14(1):8–18. doi: 10.1016/j.yebeh.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 5.Katon W, Lozano P, Russo J, et al. The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared with controls. J Adolesc Health. 2007 Nov;41(5):455–463. doi: 10.1016/j.jadohealth.2007.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barakat LP, Patterson CA, Daniel LC, et al. Quality of life among adolescents with sickle cell disease: mediation of pain by internalizing symptoms and parenting stress. Health Qual Life Outcomes. 2008;6:60. doi: 10.1186/1477-7525-6-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edwards CL, Scales MT, Loughlin C, et al. A brief review of the pathophysiology, associated pain, and psychosocial issues in sickle cell disease. Int J Behav Med. 2005;12(3):171–179. doi: 10.1207/s15327558ijbm1203_6. [DOI] [PubMed] [Google Scholar]
- 8.Hofmann M, de Montalembert M, Beauquier-Maccotta B, et al. Posttraumatic stress disorder in children affected by sickle-cell disease and their parents. Am J Hematol. 2007 Feb;82(2):171–172. doi: 10.1002/ajh.20722. [DOI] [PubMed] [Google Scholar]
- 9.Palermo TM. Impact of recurrent and chronic pain on child and family daily functioning: a critical review of the literature. J Dev Behav Pediatr. 2000 Feb;21(1):58–69. doi: 10.1097/00004703-200002000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell MJ, Lemanek K, Palermo TM, et al. Parent perspectives on pain management, coping, and family functioning in pediatric sickle cell disease. Clin Pediatr. 2007 May;46(4):311–319. doi: 10.1177/0009922806293985. [DOI] [PubMed] [Google Scholar]
- 11.Gannoni AF, Shute RH. Parental and child perspectives on adaptation to childhood chronic illness: a qualitative study. Clin Child Psychol Psychiatry. 2010 Jan;15(1):39–53. doi: 10.1177/1359104509338432. [DOI] [PubMed] [Google Scholar]
- 12.Chesler MA, Barbarin OA. Childhood cancer and the family: meeting the challenge of stress and support. New York, NY: Brunner/Mazel; 1987. [Google Scholar]
- 13.Gil KM, Wilson JJ, Edens JL, et al. Effects of cognitive coping skills training on coping strategies and experimental pain sensitivity in African American adults with sickle cell disease. Health Psychol. 1996 Jan;15(1):3–10. doi: 10.1037//0278-6133.15.1.3. [DOI] [PubMed] [Google Scholar]
- 14.Noll RB, Vannatta K, Koontz K, et al. Peer relationships and emotional well-being of youngsters with sickle cell disease. Child Dev. 1996 Apr;67(2):423–436. doi: 10.1111/j.1467-8624.1996.tb01743.x. [DOI] [PubMed] [Google Scholar]
- 15.Barbarin OA, Whitten CF, Bond S, et al. The social and cultural context of coping with sickle cell disease: III. Stress, coping tasks, family functioning and children’s adjustment. J Black Psychol. 1999 Aug;25(3):356–377. 1028 Social networks of parents of children with SCD. [Google Scholar]
- 16.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bulletin. 1985 Sep;98(2):310–357. [PubMed] [Google Scholar]
- 17.Wellman B, Wortley S. Different strokes from different folks: community ties and social support. Am J Sociol. 1990 Nov;96(3):558–588. [Google Scholar]
- 18.DeNavas-Walt C, Proctor BD, Smith JC. Current Population Reports: income, poverty, and health insurance coverage in the United States: 2007. Washington, DC: U.S. Census Bureau; 2008. pp. 60–235. Available at: http://www.census.gov/prod/2008pubs/p60–235.pdf. [Google Scholar]
- 19.Tucker CM. Expanding pediatric psychology beyond hospital walls to meet the health care needs of ethnic minority children. J Pediatric Psychol. 2002 Jun;27(4):315–323. doi: 10.1093/jpepsy/27.4.315. [DOI] [PubMed] [Google Scholar]
- 20.Garcia Coll C, Lamberty G, Jenkins R, et al. An integrative model for the study of developmental competencies in minority children. Child Dev. 1996 Oct;67(5):1891–1914. [PubMed] [Google Scholar]
- 21.Taylor RD. Risk and resilience in low-income African American families: moderating effects of kinship social support. Cultur Divers Ethnic Minor Psychol. 2010 Jul;16(3):344–351. doi: 10.1037/a0018675. [DOI] [PubMed] [Google Scholar]
- 22.Taylor RD, Casten R, Flickinger SM. Influence of kinship social support on the parenting experiences and psychosocial adjustment of African-American adolescents. Dev Psychol. 1993 Mar;29(2):382–388. [Google Scholar]
- 23.Wilson MN, Tolson TF. Familial support in the Black community. J Clin Child Psychol. 1990;19(4):347–355. [Google Scholar]
- 24.Dilworth-Anderson E. Family structure and intervention strategies: beyond empirical research. Annals New York Academy of Sciences. 1989;565:183–188. [Google Scholar]
- 25.Gallant MP. The influence of social support on chronic illness self-management: a review and directions for research. Health Educ Behav. 2003 Apr;30(2):170–195. doi: 10.1177/1090198102251030. [DOI] [PubMed] [Google Scholar]
- 26.Slaughter DT, Dilworth-Anderson P. Care of Black children with sickle cell disease: fathers, maternal support, and esteem. Fam Relations. 1988 Jul;37(3):281–287. [Google Scholar]
- 27.Whitten CF, Fischoff J. Psychosocial effects of sickle cell disease. Arch lntern Med. 1974;133:681–689. [PubMed] [Google Scholar]
- 28.Cohen S. Social relationships and health. Am Psychol. 2004 Nov;59(8):676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- 29.Hines J, Mitchell M, Crosby L, et al. Engaging patients with sickle cell disease and their families in disease education, research, and community awareness. J Prev Interv Comm. 2011 doi: 10.1080/10852352.2011.576976. (In press.) [DOI] [PubMed] [Google Scholar]
- 30.Norbeck JS, Lindsey AM, Carrieri VL. The development of an instrument to measure social support. Nurs Res. 1981 Sep-Oct;30(5):264–269. [PubMed] [Google Scholar]
- 31.Norbeck JS, Anderson NJ. Psychosocial predictors of pregnancy outcomes in lowincome Black, Hispanic, and White women. Nurs Res. 1989 Jul-Aug;38(4):204–209. [PubMed] [Google Scholar]
- 32.Cross RL, Parker A, Borgatti SP. A birds-eye view: using social network analysis to improve knowledge creation and sharing. Knowledge Directions. 2000;2(1):48–61. Available at: http://www.analytictech.com/borgatti/papers/cross,%20parker%20and%20borgatti%20–%20A_birds_eye_view.pdf. [Google Scholar]
- 33.Roberts JM., Jr Correspondence analysis of two-mode network data. Social Networks. 2000 May;22(1):65–72. Available at: http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6VD1-40963CR-4&_user=139596&_coverDate=05%2F31%2F2000&_rdoc=1&_fmt=high&_orig=gateway&_origin=gateway&_sort=d&_docanchor=&view=c&_searchStrId=1757753873&_rerunOrigin=google&_acct=C000011518&_version=1&_urlVersion=0&_userid=139596&md5=05c66c975903647f748fae890290dc74&searchtype=a. Vaughn, McLinden, Jacquez, Crosby, Slater, and Mitchell 1029. [Google Scholar]
- 34.SPSS, Inc. SPSS for Windows, Rel. 16.0.1 [computer program] Chicago, IL: SPSS, Inc.; 2007. [Google Scholar]
- 35.Analytic Technologies. Ucinet 6 for windows: software for social network analysis. Lexington, KY: Analytic Technologies; 2002. [Google Scholar]
- 36.Analytic Technologies. NetDraw: graph visualization software, version 2.087. Lexington, KY: Analytic Technologies; 2002. [Google Scholar]
- 37.Strauss AL, Corbin JM. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park, CA: Sage Publications; 1990. [Google Scholar]
- 38.Borgatti SP, Everett MG. Network analysis of 2-mode data. Social Networks. 1997;19(3):243–269. [Google Scholar]
- 39.Hanline MF, Daley SE. Family coping strategies and strengths in Hispanic, African-American, and Caucasian families of young children. Topics in Early Childhood Special Education. 1992 Fall;12(3):351–366. [Google Scholar]
- 40.Holder B, Turner-Musa J, Kimmel PL, et al. Engagement of African American families in research on chronic illness: a multisystem recruitment approach. Fam Process. 1998 Summer;37(2):127–151. doi: 10.1111/j.1545-5300.1998.00127.x. [DOI] [PubMed] [Google Scholar]
- 41.Sterling YM, Peterson J, Weekes DP. African-American families with chronically ill children: oversights and insights. J Pediatr Nurs. 1997;12(5):292–300. doi: 10.1016/S0882-5963(97)80047-4. [DOI] [PubMed] [Google Scholar]
- 42.Calderón C, Gómez-López L, Martinez-Costa C, et al. Feeling of burden, psychological distress, and anxiety among primary caregivers of children with home enteral nutrition. J Pediatr Psychol. 2011 Mar;36(2):188–196. doi: 10.1093/jpepsy/jsq069. [DOI] [PubMed] [Google Scholar]
- 43.Coffey JS. Parenting a child with chronic illness: a metasynthesis. Pediatr Nurs. 2006 Jan-Feb;32(1):51–59. [PubMed] [Google Scholar]
- 44.Tew K, Landreth GL, Joiner KD, et al. Filial therapy with parents of chronically ill children. In: Baggerly JN, Ray DC, Bratton SC, editors. Child-centered play therapy research: the evidence base for effective practice. Hoboken, NJ: Wiley; 2010. Apr, pp. 295–309. [Google Scholar]
- 45.Wiedebusch S, Konrad M, Foppe H, et al. Health-related quality of life, psychosocial strains, and coping in parents of children with chronic renal failure. Pediatr Nephrol. 2010 Aug;25(8):1477–1485. doi: 10.1007/s00467-010-1540-z. [DOI] [PubMed] [Google Scholar]
- 46.Gonzalez del Rey JA. Masters in Education Thesis. Cincinnati, OH: University of Cincinnati; 2006. Can an educational video improve parental understanding of physician trainee roles in the pediatric emergency department? [Google Scholar]
- 47.Santen SA, Rotter TS, Hemphill RR. Patients do not know the level of training of their doctors because doctors do not tell them. J Gen Intern Med. 2008 May;23(5):607–610. doi: 10.1007/s11606-007-0472-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Allen D, Marshall ES. Spirituality as a coping resource for African American parents of chronically ill children. MCN Am J Matern Child Nurs. 2010 Jul-Aug;35(4):232–237. doi: 10.1097/NMC.0b013e3181de3f76. [DOI] [PubMed] [Google Scholar]
- 49.Eysenbach G, Jadad AR. Evidence-based patient choice and consumer health informatics in the internet age. J Med Internet Res. 2001 Apr-Jun;3(2):E19. doi: 10.2196/jmir.3.2.e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McMullan M. Patients using the internet to obtain health information: how this affects the patient-health professional relationship. Patient Educ Couns. 2006 Oct;63(1–2):24–28. doi: 10.1016/j.pec.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 51.Lee EJ, Parker V, DuBose L, et al. Demands and resources: parents of school-age children with asthma. J Pediatr Nurs. 2006 Dec;21(6):425–433. doi: 10.1016/j.pedn.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 52.Graff JC, Hankins JS, Hardy BT, et al. Exploring parent-sibling communication in families of children with sickle cell disease. Issues Compr Pediatr Nurs. 2010 Jan;33(2):101–123. doi: 10.3109/01460861003663987. [DOI] [PMC free article] [PubMed] [Google Scholar]