Abstract
Purpose
To evaluate conjunctival epithelial neoplastic lesions in a 7-year period.
Materials and methods
The data of all primary cases of conjunctival neoplasia diagnosed in the Pathology Department of Farabi Eye Hospital were analyzed.
Results
The patient group consisted of 179 (65.3%) males and 95 (34.6%) females, with an age range of 14–90 years and a mean age of 57.9 years. The most common primary conjunctival epithelial neoplastic lesion was invasive squamous cell carcinoma (SCC) (40.8%), followed by dysplasia (17%), papilloma (16.4%), In situ SCC (16%), actinic keratosis (7.3%), basal cell carcinoma (0.7%), xeroderma pigmentosum (0.7%), and mucoepidermoid carcinoma (0.3%). Of 274 lesions, 47 (17.1%) were benign, 159 (58%) were malignant, and 68 (24.8%) were precancerous. Compared to the results of a previous study of this center (1990–2004), the incidence of precancerous lesions has slightly increased whereas the incidence of SCC has decreased (22.1% vs. 24.8% and 59% vs. 40.8%, respectively).
Conclusion
SCC is the most common conjunctival epithelial neoplasm in this study, and its prevalence in males is nearly two times higher than in females. The high percentage of squamous cell carcinoma can likely be attributed to elevated sun exposure and ultraviolet light in Iran.
Keywords: Conjunctival epithelial neoplasm, Squamous cell carcinoma, Papilloma
Introduction
Squamous cell carcinoma of the conjunctiva (SCCC) is a rare cancer of the ocular surface with an incidence rate that varies geographically from 0.02 per 100,000 in high latitude areas to 3.5 per 100,000 at low latitudes.1, 2 Ocular surface squamous neoplasias (OSSN), a recent term ranging from “precancerous” lesions to invasive carcinoma, comprises a wide spectrum of dysplastic alterations of the squamous epithelium of the eye surface, including conjunctival intraepithelial neoplasia (CIN), carcinoma in situ (CIS), and SCCC.1, 3 Among the general population in the United States, using data from the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute, the risk of SCCC was higher in males and in whites and was correlated exposure to ultraviolet radiation.1 The etiology of the conjunctival cancers appears to be multifactorial; several etiologic factors have been identified including smoking, sun-exposure, latitude, history of pterygium, and both human immunodeficiency virus (HIV) and Human papilloma virus (HPV) infection. However, the reports on HPV and conjunctival neoplasms are controversial.4 OSSN grows in a flat superficial leukoplakia, velvety or papilliform, gelatinous nodular, or diffuse in an invasive fashion. These tumors may present as localized and slowly growing lesions and have sometimes been associated with pinguecula and pterygia.5, 6, 7 In elderly patients, the tumor may be initially diagnosed as a chronic unilateral conjunctivitis or scleritis, and as chalazion if arising from the bulbar conjunctiva.6
In the present study, we enrolled all conjunctival epithelial tumors in Farabi Eye Hospital (Tehran, Iran) over a 7-year period and evaluated the etiologic factors and clinical and pathologic features of the most malignant tumor, SCCC.
Patients and methods
In this retrospective seven-year cross-sectional study (2006–2012), 274 patients with conjunctival epithelial tumors were enrolled through the pathology files of Farabi Eye Hospital in Tehran, Iran. The tumors were classified as benign, precancerous, and malignant. Conjunctival intraepithelial neoplasia (CIN) encompasses dysplasia and actinic keratosis that were considered precancerous lesions of the conjunctiva. Demographic data with tumor location and presentation were also obtained from all patient׳s medical records. A survey was prepared inquiring if patients were exposed to the sun more or less than 180 days per year over the last 10 years. An age and gender matched control group (50 patients) with lesion-free, normal conjunctival biopsies (mean age: 64.3, age p-value: 0.4, sex p-value: 0.63) were selected from the archive of the Pathology Department of Farabi Eye Hospital.
Statistical analysis
The results are expressed as mean ± SD. Statistical analysis was performed using SPSS version 16.0.1 (SPSS Inc., Chicago, IL, U.S.A.). The statistical differences between proportions were determined by χ2 analysis. Numerical data were evaluated using analysis of variance, followed by Tukey׳s post hoc test. P value < 0.05 was considered significant.
Results
Demographic data
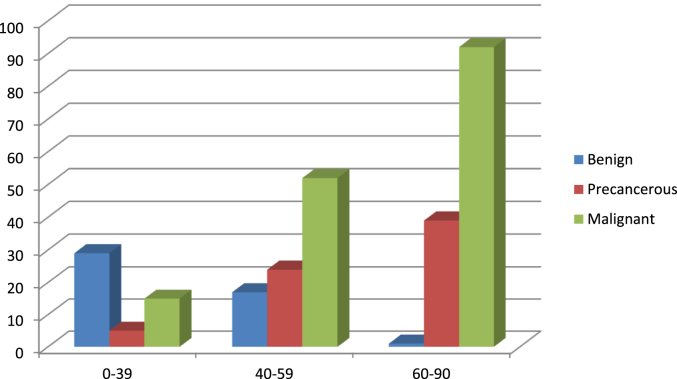
Among all conjunctival specimens which were addressed to the pathology department of Farabi Eye Hospital between 2006 to 2012, 274 patients (171 male and 103 female with a mean age of 57.9 years ranged from 14 to 90 years) were enrolled in this cross-sectional study. The mean age of the patients with malignant tumors was 62.1 years (range, 16–90 years), and the majority of patients were in their eighties (48 cases, 30.2%). About half of the conjunctival epithelial tumors (48.2%) were manifested in ages over 60 years. Among 274 tumors, 159 (58%) were malignant, 68 (24.8%) were precancerous, and 47 (17.1%) were benign. There was no association between gender and the type of the lesions (p > 0.05). Age stratification and frequency of benign, precancerous, and malignant epithelial tumors of the conjunctiva are denoted in Fig. 1. Compared to a previous study8 from this center conducted during 1990–2004, the incidence of precancerous conjunctival lesions slightly increased (22.1%–24.8%) whereas the incidence of SCC decreased (59%–40.8%). Characteristics of the tumors in comparison to the control group and previous studies are summarized in Table 1, Table 2.
Fig. 1.
Age stratification and frequency of 247 conjunctival epithelial neoplasms.
Table 1.
Characteristic of 274 conjunctival epithelial tumors in comparison to control group in Farabi Eye Hospital, Tehran, Iran.
| Characteristic | N (%) | Benign | IENa | Malignant | Control group |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 171 (62.4) | 28 | 45 | 98 | 29 |
| Female | 103 (37.6) | 19 | 23 | 61 | 21 |
| Sun-exposure (days/year) | |||||
| <180 | 133 (48.5) | 32 | 41 | 60 | 20 |
| >180 | 141 (51.5) | 15 | 27 | 99 | 30 |
IEN, intraepithelial neoplasia.
Table 2.
Pathology classification in 274 conjunctival epithelial tumors in Farabi Eye Hospital, Tehran, Iran.
| Histopathologic classification | M/F | This study (%) 2006–2012 |
Previous study (%)a 1990–2004 |
|---|---|---|---|
| Benign | 28/19 | 47 (17.1) | 35 (18.4) |
| Papilloma | 26/19 | 45 (16.4) | 35 (18.4) |
| XP | 2/0 | 2 (0.7) | – |
| IEN | 45/23 | 68 (24.8) | 42 (22.1) |
| Dysplasia | 33/15 | 48 (17.5) | 25 (13.2) |
| Actinic keratosis | 12/8 | 20 (7.3) | 17 (8.9) |
| Malignant | 98/61 | 159 (58) | 113 (59.5) |
| Invasive SCC | 69/43 | 112 (40.8) | 112 (59) |
| In situ SCC | 27/17 | 44 (16) | – |
| BCC | 1/1 | 2 (0.7) | – |
| MEC | 1/0 | 1 (0.3) | 1 (0.5) |
| Total | 171/103 | 274 (100) | 190 (100) |
BCC, basal cell carcinoma; IEN, intraepithelial neoplasia; MEC, mucoepidermoid carcinoma, SCC, squamous cell carcinoma; XP, Xeroderma pigmentosum.
Ref:8.
Clinical data
The most frequent clinical findings and symptoms among malignant tumors were gelatinous mass (41.5%), followed by leukoplakia (24.5%), nodular mass (21.4%), pigmented lesions (8.2%), chronic conjunctivitis (3.1%), and blurred vision (1.3%). Among 274 patients, 126 (45.9%) of the lesions were on the bulbar conjunctiva, 122 (44.5%) on the limbal conjunctiva, 22 (8%) on the palpebral conjunctiva, and 4 (1.4%) on the fornix. Limbal and bulbar conjunctivas were the most frequent sites for benign and malignant tumors, respectively. No statistically significant difference was found among different anatomic sites in benign and malignant tumors (Table 3).
Table 3.
Anatomic sites in benign, precancerous, and malignant epithelial tumors of the conjunctiva.
| Anatomic site | Benign tumors | IEN | Malignant tumors | Total |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | |
| BC | 18 (38.3) | 32 (47) | 76 (47.8) | 126 (45.9) |
| LC | 23 (49) | 29 (42.6) | 70 (44) | 122 (44.5) |
| PC | 5 (10.6) | 7 (10.2) | 10 (6.3) | 22 (8) |
| F | 1 (2.1) | 0 (0) | 3 (1.9) | 4 (1.4) |
| Total | 47 (17.1) | 68 (24.8) | 159 (58) | 274 (100) |
BC, bulbar conjunctiva; F, fornix; IEN, intraepithelial neoplasia; LC, limbal conjunctiva; PC, palpebral conjunctiva.
Etiology and associated conditions
To define the etiologic effect of UV light on conjunctival epithelial tumors, we compared 50 age- and gender-matched control patients in the matter of the sun-exposure days per year with a cut-off point of 180 days/year. Our data revealed a significant association between the duration of sun exposure and the lesions with more than 180 days/year exposed to sun were more likely to be malignant than lesions with less than 180 days/year (p < 0.001). Malignant tumors had a significant association with sun exposure of more than 180 days/year in comparison to benign tumors (p < 0.001). Precancerous lesions had been also exposed to sun light more than 180 days/year (Table 1). Intraepithelial neoplasia including dysplasia and actinic keratosis were accompanied with malignant tumors, in which 107 (67.3%) cases of malignant tumors were associated with them. History of actinic changes and pterygium was present in 101 (63.5%) of malignant tumors.
Discussion
In our study, malignant epithelial tumors of the conjunctiva were more common than benign tumors, which may be due to the fact that Farabi Eye Hospital is a referral center for eye diseases, and more complicated cases are referred to this center. At the same time, this is a large series of benign, precancerous, and malignant epithelial tumors of the conjunctiva in Iran. In our previous report, it was suggested to consider patient age as a predictive factor of malignancy while evaluating conjunctival neoplasms.8 Compared to previous study in this center, the incidence of precancerous lesions, such as dysplasia and actinic keratosis, increased whereas the incidence of SCCC decreased. This fact may be a result of earlier detection and better management of patients in this center.
Ocular surface squamous neoplasia is more common in countries with high exposure to sunlight. In line of this fact, the interpalpebral zone, the part of the conjunctiva heavily exposed to the ultraviolet light is the most prevalent site of the malignancy.6, 9, 10, 11 Malignant epithelial tumors are more common in men than in women because men spend more time outdoors and are exposed to sunlight more. However, in a study in Zimbabwe, 70% of the patients with OSSN were female due to their involvement in agriculture and harvesting in farms, which led to high sun exposure.12
Regarding exposure time, malignant tumors in our presentation had a significant association with the sun exposure being more than 180 days/year in comparison to benign tumors (p-value < 0.001). Precancerous lesions are also correlated with sun exposure of more than 180 days/year, devoid of significant association. Actinic changes/pterygium and conjunctival intraepithelial neoplasia (CIN), which were present in 63.5% and 67.3% of squamous carcinoma, respectively, may be attributed to the intensity and duration of sunlight exposure in our country. This strong association confirms the role of direct sun-exposure in etiology of actinic changes and epithelial neoplasia of the conjunctiva. Other studies have also confirmed that OSSN is associated with pinguecula, pterygium, and CIN.5, 6, 7, 13, 14, 15 Usually, these lesions arise within interpalpebral fissure, mostly at the limbus, although they may be found in any part of the conjunctiva and cornea.3
Recently, human papilloma virus (HPV), mainly type 16, has been detected in tissue specimens of OSSN. Our previous study on 50 cases of SCCC showed that HPV is strongly associated with SCCC in comparison to all normal conjunctival biopsy specimens.16 Ateenyi-Agaba et al.׳s study supports the hypothesis that cutaneous, but not mucosal subtypes of HPV, may be involved in the etiology of this rare malignancy and its precursor lesions.17, 18, 19 There are marked variations in the reported HPV prevalence rates in conjunctival carcinoma, ranging from 0% to 100%.20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30 Whereas some studies have reported highest incidence of HPV, 21, 24 others have shown no evidence of HPV infection in OSSN lesions.20, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34 These discrepancies show the more important role of UV exposure in OSSN development than HPV infection.35, 36
In conclusion, the high percentage of squamous cell carcinoma can likely be attributed to geographical latitude and greater sun exposure. The characterization of precancerous lesions in this study emphasizes their potential to transform into malignant lesions and the need for sufficient early management and follow-up. The incidence of precancerous lesions and SCC compared to a previous study increased and decreased, respectively, suggesting earlier detection and better management of OSSN in this eye center.
Acknowledgment
This study was supported by a grant from the Deputy for Research of Tehran University of Medical Sciences, Tehran, Iran (Grant 20915).
Footnotes
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Alves L.F., Fernandes B.F., Burnier J.V. Incidence of epithelial lesions of the conjunctiva in a review of 12,102 specimens in Canada (Quebec) Arq Bras Oftalmol. 2011 Jan–Feb;74:21–23. doi: 10.1590/s0004-27492011000100005. [DOI] [PubMed] [Google Scholar]
- 2.Emmanuel B., Ruder E., Lin S.W. Incidence of squamous-cell carcinoma of the conjunctiva and other eye cancers in the NIH-AARP Diet and Health Study. Ecancermedicalscience. 2012;6:254. doi: 10.3332/ecancer.2012.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pe׳er J. Ocular surface squamous neoplasia. Ophthalmol Clin North Am. 2005 Mar;18:1–13. doi: 10.1016/j.ohc.2004.08.001. vii. review. [DOI] [PubMed] [Google Scholar]
- 4.Peralta R., Valdivia A., Estañ̆ol P. Low frequency of human papillomavirus infection in conjunctival squamous cell carcinoma of Mexican patients. Infect Agent Cancer. 2011;18:24. doi: 10.1186/1750-9378-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ni C., Searl S.S., Kriegstein H.J., Wu B.F. Epibulbar carcinoma. Int Ophthalmol Clin. 1982;22:1–33. doi: 10.1097/00004397-198202230-00005. [DOI] [PubMed] [Google Scholar]
- 6.Tunc M., Char D.H., Crawford B. Intraepithelial and invasive squamous cell carcinoma of the conjunctiva: analysis of 60 cases. Br J Ophthalmol. 1999;83:98–103. doi: 10.1136/bjo.83.1.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee G.A., Hirst L.W. Ocular surface squamous neoplasia. Surv Ophthalmol. 1995;39:429–450. doi: 10.1016/s0039-6257(05)80054-2. [DOI] [PubMed] [Google Scholar]
- 8.Amoli F.A., Heidari A.B. Survey of 447 patients with conjunctival neoplastic lesions in Farabi Eye Hospital, Tehran, Iran. Ophthalmic Epidemiol. 2006;13:275–279. doi: 10.1080/09286580600801036. [DOI] [PubMed] [Google Scholar]
- 9.McDonnell J.M., McDonnell P.J., Mounts P. Demonstration of papillomavirus capsid Pe׳er 8 antigen in human conjunctival neoplasia. Arch Ophthalmol. 1986;104:1801–1805. doi: 10.1001/archopht.1986.01050240075043. [DOI] [PubMed] [Google Scholar]
- 10.Guech-Ongey M., Engels E.A., Goedert J.J. Elevated risk for squamous cell carcinoma of the conjunctiva among adults with AIDS in the United States. Int J Cancer. 2008;122:2590–2593. doi: 10.1002/ijc.23384. [DOI] [PubMed] [Google Scholar]
- 11.Lee G.A., Hirst L.W. Incidence of ocular surface dysplasia in metropolitan Brisbane. A ten year survey. Arch Ophthalmol. 1992;110:525–527. doi: 10.1001/archopht.1992.01080160103042. [DOI] [PubMed] [Google Scholar]
- 12.Pola E.C., Masanganise R., Rusakaniko S. The trend of ocular surface squamous neoplasia among ocular surface tumour biopsies submitted for histology from Sekuru Kaguvi Eye Unit, Harare between 1996 and 2000. Cent Afr J Med. 2003;49:1–4. [PubMed] [Google Scholar]
- 13.Degrassi M., Piantanida A., Nucci P. Unexpected histological findings in pterygium. Optom Vis Sci. 1993;70:1058–1060. doi: 10.1097/00006324-199312000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Clear A.S., Chirambo M.C., Hutt M.S. Solar keratosis, pterygium, and squamous cell carcino-ma of the conjunctiva in Malawi. Br J Ophthalmol. 1979;63:102–109. doi: 10.1136/bjo.63.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seregard S., Kock E. Squamous spindle cell carcinoma of the conjunctiva: fatal outcome of pterygium-like lesion. Acta Ophthalmol Scand. 1995;73:464–466. doi: 10.1111/j.1600-0420.1995.tb00311.x. [DOI] [PubMed] [Google Scholar]
- 16.Asadi-Amoli F., Heidari A.B., Jahanzad I. Detection of human papillomavirus in squamous cell carcinoma of conjunctiva by nested PCR: a case control study in Iran. Acta Med Iran. 2011;49:707–714. [PubMed] [Google Scholar]
- 17.Ateenyi-Agaba C., Franceschi S., Wabwire-Mangen F. Human papillomavirus infection and squamous cell carcinoma of the conjunctiva. Br J Cancer. 2010;102:262–267. doi: 10.1038/sj.bjc.6605466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ateenyi-Agaba C., Weiderpass E., Smet A. Epidermodysplasia verruciformis human papillomavirus types and carcinoma of the conjunctiva: a pilot study. Br J Cancer. 2004;90:1772–1779. doi: 10.1038/sj.bjc.6601743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Koning M.N., Waddell K., Magyezi J. Genital and cutaneous human papillomavirus (HPV) types in relation to conjunctival squamouscell neoplasia: a case – control study in Uganda. Infect Agent Cancer. 2008;3:12. doi: 10.1186/1750-9378-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McDonnell J.M., Mayr A.J., Martin W.J. DNA of human papillomavirus type 16 in dysplastic and malignant lesions of the conjunctiva and cornea. N Engl J Med. 1989;320:1442–1446. doi: 10.1056/NEJM198906013202202. [DOI] [PubMed] [Google Scholar]
- 21.Lauer S.A., Malter J.S., Meier J.R. Human papillomavirus type 18 in conjunctival intraepithelial neoplasia. Am J Ophthalmol. 1990;110:23–27. doi: 10.1016/s0002-9394(14)76932-6. [DOI] [PubMed] [Google Scholar]
- 22.McDonnell J.M., Wagner D., Ng S.T. Human papillomavirus type 16 DNA in ocular and cervical swabs of women with genital tract condylomata. Am J Ophthalmol. 1991;112:61–66. doi: 10.1016/s0002-9394(14)76214-2. [DOI] [PubMed] [Google Scholar]
- 23.Odrich M.G., Jakobiec F.A., Lancaster W.D. A spectrum of bilateral squamous conjunctival tumors associated with human papillomavirus type 16. Ophthalmology. 1991;98:628–635. doi: 10.1016/s0161-6420(91)32218-8. [DOI] [PubMed] [Google Scholar]
- 24.Tuppurainen K., Raninen A., Kosunen O. Squamous cell carcinoma of the conjunctiva. Failure to demonstrate HPV DNA by in situ hybridization and polymerase chain reaction. Acta Ophthalmol (Copenh) 1992;70:248–254. doi: 10.1111/j.1755-3768.1992.tb04132.x. [DOI] [PubMed] [Google Scholar]
- 25.McDonnell J.M., McDonnell P.J., Sun Y.Y. Human papillomavirus DNA in tissues and ocular surface swabs of patients with conjunctival epithelial neo-plasia. Invest Ophthalmol Vis Sci. 1992;33:184–189. [PubMed] [Google Scholar]
- 26.Saegusa M., Takano Y., Hashimura M. HPV type 16 in conjunctival and junctional papilloma, dysplasia, and squamous cell carcinoma. J Clin Pathol. 1995;48:1106–1110. doi: 10.1136/jcp.48.12.1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lewallen S., Shroyer K.R., Keyser R.B. Aggressive conjunctival squamous cell carcinoma in three young Africans. Arch Ophthalmol. 1996;114:215–218. doi: 10.1001/archopht.1996.01100130209021. [DOI] [PubMed] [Google Scholar]
- 28.Nakamura Y., Mashima Y., Kameyama K. Detection of human papillomavirus infection in squamous tumors of conjunctiva and lacrimal sac by immunohistochemistry, in situ hybridisation, and polymerase chain reaction. Br J Ophthalmol. 1997;81:308–313. doi: 10.1136/bjo.81.4.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tabrizi S.N., McCurrach F.E., Drewe R.H. Human papillomavirus in corneal and conjunctival carcinoma. Aust N Z J Ophthalmol. 1997;25:211–215. doi: 10.1111/j.1442-9071.1997.tb01394.x. [DOI] [PubMed] [Google Scholar]
- 30.Karcioglu Z.A., Issa T.M. Human papilloma virus in neoplastic and non-neoplastic conditions of the external eye. Br J Ophthalmol. 1997;81:595–598. doi: 10.1136/bjo.81.7.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McDonnell P.J., McDonnell J.M., Kessis T. Detection of human papillomavirus type 6/11 DNA in conjunctival papillomas by in situ hybridization with radioactive probes. Hum Pathol. 1987;18:1115–1119. doi: 10.1016/s0046-8177(87)80378-7. [DOI] [PubMed] [Google Scholar]
- 32.Dushku N., Hatcher S.L., Albert D.M., Reid T.W. p53 expression and relation to human papillomavirus infection in pingueculae, pterygia, and limbal tumors. Arch Ophthalmol. 1999;117:1593–1599. doi: 10.1001/archopht.117.12.1593. [DOI] [PubMed] [Google Scholar]
- 33.Toth J., Karcioglu Z.A., Moshfeghi A.A. The relationship between human papillomavirus and p53 gene in conjunctival squamous cell carcinoma. Cornea. 2000;19:159–162. doi: 10.1097/00003226-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Waddell K., Magyezi J., Boursarghin L. Antibodies against human papillomavirus type 16 (HPV-16) and conjunctival squamous cell neoplasia in Uganda. Br J Cancer. 2003;88:2002–2003. doi: 10.1038/sj.bjc.6600950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eng H.L., Lin T.M., Chen S.Y. Failure to detect human papillomavirus DNA in malignant epithelial neoplasia of conjunctiva by polymerase chain reaction. Am J Clin Pathol. 2002;117:429–436. doi: 10.1309/RVUP-QMU3-5X6W-3CQ1. [DOI] [PubMed] [Google Scholar]
- 36.Verma V., Shen D., Sieving P.C. The role of infectious agents in the etiology of ocular adnexal neoplasia. Surv Ophthalmol. 2008;53:312–331. doi: 10.1016/j.survophthal.2008.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]