Abstract
Purpose
To report a case of Idiopathic retinal vasculitis, arteriolar macroaneurysms, and neuroretinitis (IRVAN). syndrome in a young female.
Case report
A 21-year-old woman presented with unilateral visual acuity (VA) loss. Ophthalmological examination disclosed unilateral optic disc swelling, star-shaped macular exudation, multiple aneurysms surrounded by perivascular exudation, retinal vasculitis, and mild vitreous reaction. The left eye examination was entirely normal. Clinical and paraclinical findings were compatible with IRVAN syndrome criteria. The patient was treated with a short course of oral steroid, a trans-septal triamcinolone acetonide injection, selective laser photocoagulation in peripheral non-perfusion areas, and intravitreal bevacizumab. In spite of primary good response, after each treatment cessation, VA dropped with increasing central macular thickness (CMT), but response to intravitreal triamcinolone (4 mg/0.1 cc) was permanent and good.
Conclusion
IRVAN syndrome can have unilateral presentation. All treatment options were temporary except intravitreal steroid injection in our case. The effect of steroid in IRVAN will need further evaluation.
Keywords: Idiopathic reinal vasculitis, aneurysms, and neuroretinitis syndrome; IRVAN retina; Unilateral
Introduction
Idiopathic retinal vasculitis, arteriolar macroaneurysms, and neuroretinitis (IRVAN) is a rare clinical entity that is usually seen bilaterally in a young healthy female without any systemic disease.1 The most complications of the disease are because of exudation, which is caused by the macroaneurysms, more common on the larger retinal arterioles and pre-retinal neovascularization secondary to vasoproliferative complications because of peripheral capillary non-perfusion.1, 2 The suggested treatments are laser photocoagulation, surgery, transscleral cryotherapy, steroids therapy, and administration of monoclonal antibodies such as ranibizumab and infliximab.3, 4 The diagnosis of disease is based on a combination of clinical features. Three major criteria (retinal vasculitis, aneurysmal dilations at arterial bifurcations, and neuroretinitis) and three minor criteria (peripheral capillary non-perfusion, retinal neovascularization, and macular exudation) have been defined for the diagnosis of the syndrome.3 Few cases of unilateral IRVAN syndrome have been reported in literature, and in other reports, it have started bilaterally or unilaterally with some delay in involving the other eye.3, 4, 5, 6, 7, 8 Herein, we report clinical features, disease progression, and effects of treatment in a case of unilateral IRVAN syndrome with typical findings.
Case report
A 21-year-old woman presented to our clinic with unilateral visual acuity (VA) loss in her right eye gradually since several months earlier. VA at presentation was 3/10 in the right eye and 10/10 in her left eye. Anterior segment examination was unremarkable, and intraocular pressure was within normal limits. There were only few anterior vitreous cells in slit lamp examination in her right eye. Posterior segment findings in her right eye included unilateral optic disc swelling, star-shaped macular exudation, multiple aneurysms surrounded by perivascular exudation, retinal vasculitis, and mild vitreous reaction. The left eye examination was entirely normal. Familial history was negative.
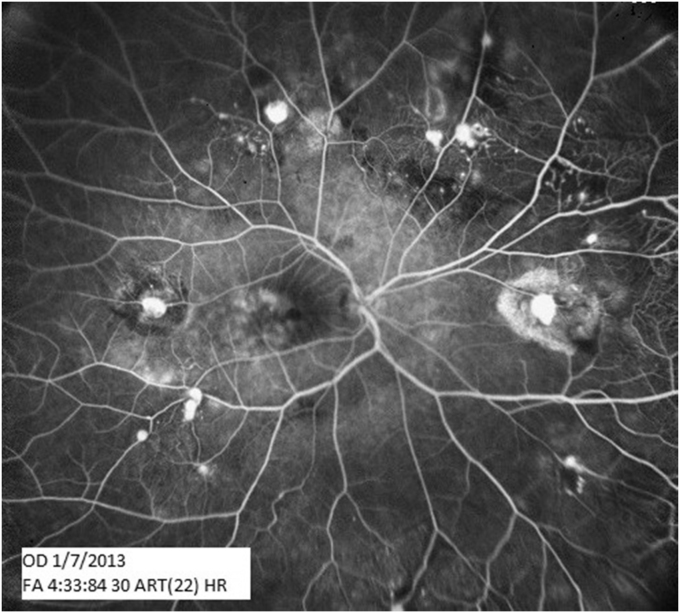
Fluorescein angiography showed anuerysmal dilations and hyperfluorescence of the vessels walls and leakage of the optic disc in the late phases in the right eye and macroaneurysm along the arterioles with late staining and significant capillary non-perfusion area with neovascular sheeting nearby. Neuroretinitis was diagnosed by blurred disc margin and late staining of the optic nerve head and retinal vasculitis (Fig. 1).
Fig. 1.
Wide field FAG of the right eye shows hyperfluorescence of the vessel walls in the late phases and macroaneurysm along the arterioles with late staining and significant capillary non-perfusion area with neovascular sheeting nearby in the right eye.
An extensive medical evaluation was performed including a chest X-ray, complete blood cell count (CBC diff), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), urinalysis, Venereal Disease Research Laboratory test (VDRL), fluorescent treponemal antibody absorption test (FTA-ABS), purified protein derivate (PPD test), C3, C4, anti-neutrophil cytoplasmic antibody (C-ANCA, P-ANCA), rheumatoid factor, human immunodeficiency virus, antinuclear antibody, angiotensin converting enzyme, and serum lysozyme. Systemic evaluation and laboratory work-up did not suggest any systemic abnormality. Rheumatologic and neurologic consultation disclosed no evidence of systemic vasculitis. Anterior chamber PCR results were negative for cytomegalovirus (CMV), tuberculosis (TB), herpes simplex virus (HSV), and varicella zoster virus (VZV) infections.
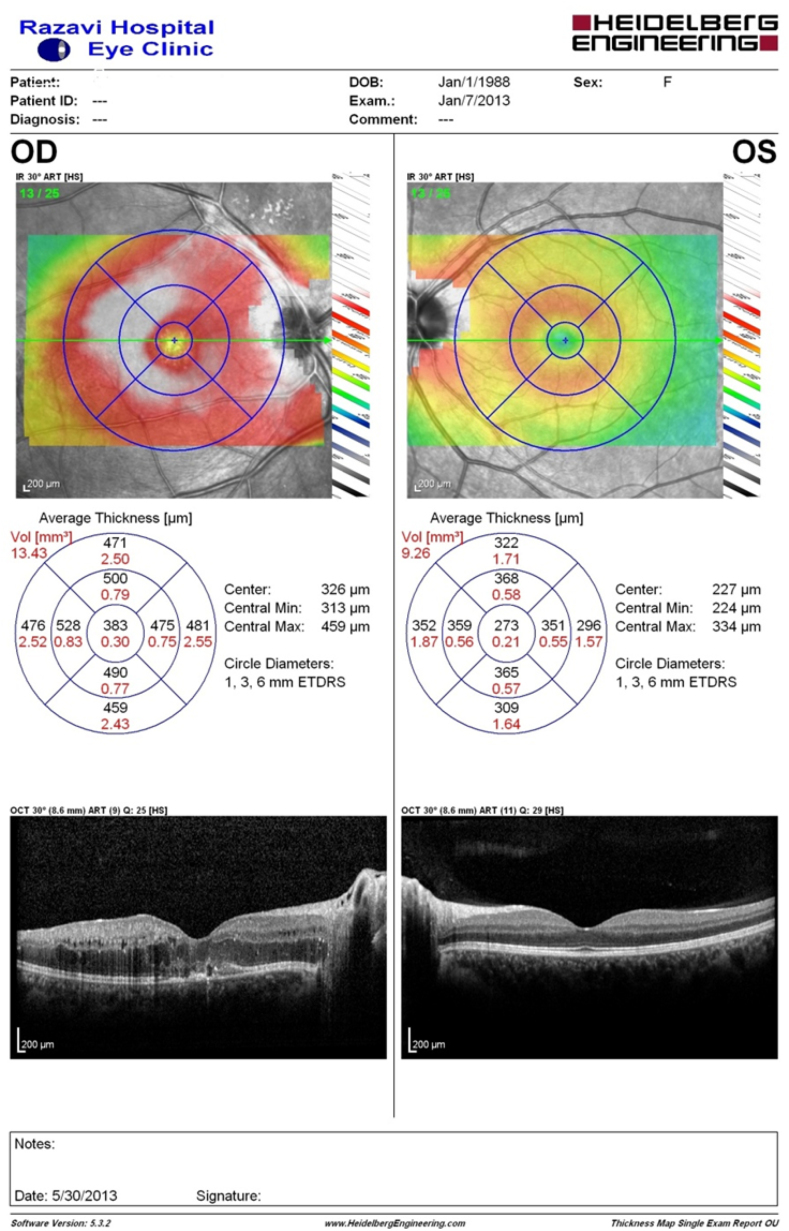
Eye-tracked spectral-domain optical coherence tomography (SD-OCT Heidelberg) was done from the posterior pole of both eyes. There was diffuse retinal thickening at the posterior pole, most severe at the level of the outer nuclear layer with schisis cavities and cystoid spaces and hyper-reflective excrescences in the outer retina with decay of the outer components (Fig. 2).
Fig. 2.
Macular OCT of left eye shows increased retinal thickening at the posterior pole, with schisis cavities and cystoid spaces and hyper-reflective excrescences in the outer retina with decay of the outer components.
According to all of clinical and paraclinical findings, the first diagnosis of IRVAN syndrome was made in this case. Our patient had all of the three major (retinal vasculitis, aneurysmal dilations at arterial bifurcations, and neuroretinitis) and 3 minor (peripheral capillary non-perfusion, retinal neovascularization, and macular exudation) criteria of disease in her right eye.
The patient was treated with a short course of oral steroid therapy, a trans-septal triamcinolone acetonide injection, and selective laser photocoagulation in peripheral non-perfusion areas. After treatment, the visual acuity increased from 3/10 to 5/10, and central macular thickness (CMT) decreased during the six-month follow-up. However, after treatment cessation, VA dropped with increasing central macular thickness (CMT). Intravitreal triamcinolone (4 mg/0.1 cc) was tried after poor response to the primary treatment options, and this time, the response to treatment was permanent and acceptable after six-month follow-up. The VA remained 6/10, and the CMT remained normal in control OCTs.
Discussion
Herein, we reported a unilateral IRVAN syndrome in a young female. The diagnosis was based on the major and minor criteria of disease, and because of atypical presentation, we excluded other possible aetiologies by the means of paraclinical exams and anterior chamber PCR.
Chang et al described the biggest series of this syndrome as a condition that usually affects young, healthy females, and its major features are multiple aneurysmal dilatations of the retinal arteries, exudative retinopathy, diffuse staining of the optic disc, and non-perfusion of peripheral capillaries.2 All of their presented cases were bilateral or unilateral with secondary involvement of the other eye in a period of time.
Unilateral and atypical IRVAN syndrome have been reported in few case reports. Gedik et al in 2005 reported a case of IRVAN. Based on their presentation, the patient׳s age, the unilateral nature of her condition, and the hemorrhage from the aneurysms that they observed were not typical features of this disorder.6 Another unilateral IRVAN syndrome was reported by Norlina et al, in which oral steroid combined with a systemic immunosuppressant had no effect on the disease course. They concluded that the unilaterality and unresponsiveness to systemic immunosuppressant can differentiate IRVAN from systemic vasculitis although IRVAN is a bilateral disease in nature.8
There is another report of atypical IRVAN syndrome reported by Darly et al in which their patient demonstrated the three major criteria of IRVAN: retinal vasculitis, aneurysmal dilations at arterial bifurcations, and neuroretinitis. However, their patient differs from a typical patient with IRVAN in that he is male, is older than 50 years, and has a probable associated systemic disease although his presentation was also bilateral. Their report was the first reported case of a patient with both antiphospholipid syndrome and IRVAN.5
Nourinia et al reported a case of IRVAN syndrome associated with positive perinuclear antineutrophil cytoplasmic antibody (P-ANCA) which is an atypical association in this case.7
Samuel et al divided the disease course into five stages.3 Stage 1 is macroaneurysms, exudation, neuroretinitis, and retinal vasculitis. Stage 2 is capillary non-perfusion (angiographic evidence). Stage 3 shows posterior segment neovascularization of disc or elsewhere and/or vitreous hemorrhage. In stage 4, there is anterior segment neovascularization (rubeosis iridis), and stage 5 shows neovascular glaucoma. Accordingly, our patient shows stage 2 of the disease.
As a rare retinal vascular condition, if IRVAN is left untreated, it may lead to severe bilateral visual loss. Because of the risk for sight-threatening complications, panretinal laser photocoagulation, corticosteroids, and vitrectomy have been used in an attempt to improve visual outcome, but most of these treatments have remained controversial. Early panretinal laser photocoagulation should be considered when angiographic evidence of widespread retinal non-perfusion is present and before (or shortly after) the development of neovascularization. The value of corticosteroids in controlling ischemic sequelae in IRVAN remains unproven.3
IRVAN syndrome is a diagnosis of exclusion, so we did an extensive evaluation to rule out other etiologies. This evaluation seems necessary especially in the atypical cases. For example, anterior chamber sampling for PCR may have a high rate of false negative results especially in the absence of AC reaction, but the positive results are valuable.
Samuel et al reviewed the clinical features, disease progression, and effects of treatment on idiopathic retinitis, vasculitis, aneurysms, and neuroretinitis. Treatments included panretinal laser photocoagulation, cryotherapy, vitrectomy surgery, and injection of periocular or intravitreal steroids, and a functional staging system is proposed to improve treatment paradigms.3
Response to the oral and topical steroid was temporary in our presented case in spite of intravitreal steroid injection. We followed the patient for two years for evaluation of any progression in the disease course and involvement of the other eye. No sign of involvement of the other eye was observed during this period of time. We think that this is enough to consider our patient as a case with unilateral IRVAN syndrome.
IRVAN syndrome can have unilateral presentation. Other aetiologies should be ruled out by the means of paraclinical examinations. Response to oral and topical steroid therapy and photocoagulation was temporary in our case in spite of intravitreal steroid injection.
Footnotes
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Kincaid J., Schatz H. Bilateral retinal arteritis with multiple aneurysmalvdilatations. Retina. 1983;3:171. doi: 10.1097/00006982-198300330-00005. [DOI] [PubMed] [Google Scholar]
- 2.Chang T.S., Aylward G.W., Davis J.L. Idiopathic retinal vasculitis, aneurysms, and neuro-retinitis: retinal vasculitis study. Ophthalmology. 1995;102:1089–1097. doi: 10.1016/s0161-6420(95)30907-4. [DOI] [PubMed] [Google Scholar]
- 3.Samuel M.A., Equi R.A., Chang T.S. vol. 114. 2007. pp. 1526–1529. (Idiopathic Retinitis, Vasculitis, Aneurysms, and Neuroretinitis (IRVAN): New Observations and a Proposed Staging System). [DOI] [PubMed] [Google Scholar]
- 4.Faghihi H., Seyed Safizadeh M., Faghihi S., Faghihi H. Idiopathic retinal vasculitis, aneurysm, neuroretinitis: a significant increase in visual acuity after treatment with one session of panretinal photocoagulation, retinopexy and three consecutive intravitreal bevacizumab (Avastin) injection. Iranian J Ophthalmol. 2012;24:65–71. [Google Scholar]
- 5.Daryl E., Kurz M.D., Robert C., Wang M.D., Paul A., Kurz M.D. Idiopathic retinal vasculitis, aneurysms, and neuroretinitis in a patient with antiphospholipid syndrome. Arch Ophthalmol. 2012;130:257–258. doi: 10.1001/archopthalmol.2011.1363. [DOI] [PubMed] [Google Scholar]
- 6.Gedik S., Yilmaz G., Akça S., Akova Y.A. An atypical case of idiopathic retinal vasculitis, aneurysms, and neuroretinitis (IRVAN) syndrome. Eye. 2005;19:469–471. doi: 10.1038/sj.eye.6701524. [DOI] [PubMed] [Google Scholar]
- 7.Nourinia R., Montahai T., Amoohashemi N., Hassanpour H., Soheilian M. Idiopathic retinal vasculitis, aneurysms and neuroretinitis syndrome associated with positive perinuclear antineutrophil cytoplasmic antibody. J Ophthalmic Vis Res. 2011;6:330–333. [PMC free article] [PubMed] [Google Scholar]
- 8.Norlina M, Mimiwati Z. IRVAN syndrome. Philipp J Ophthalmol ; 32:46–48.