Abstract
Hepatocellular carcinoma (HCC) is the most often primary cancer of the liver and is one if the leading cause of cancer-related death worldwide. The incidence of HCC has geographic distribution with the highest levels in countries with developing economies. Patients with hepatocellular carcinoma have poor prognosis despite the achievements in surgery techniques and other therapeutic procedures and it is a reason why continuous attention should be paid to this issue.
This article provides an overview of this disease based on an extensive review of relevant literature. The article summarizes the current risk factors, diagnosis, staging and the management of HCC.
Keywords: hepatocellular carcinoma, risk factors, diagnosis, management, review article
Introduction
Liver cancer is the fifth most common cancer in men and the seventh in women [1]. World-wide incidence is between 250,000 and 1,000,000 new cases per year with a male-female ratio of about 4 or 5:1 [2]. Hepatocellular carcinoma (HCC) is the most often primary cancer of the liver, accounting from 85% till 90% of all primary liver cancers [3]. Its occurrence reaches a peak at approximately 70 years of age with a rarely occurrence before the age of 40 years. Major risk factors for HCC include chronic alcohol consumption, hepatitis B, hepatitis C and non-alcoholic fatty liver disease [3]. Other, less common causes are Wilson’s disease, hereditary hemochromatosis, alpha1-antitrypsin deficiency, primary biliary cirrhosis and autoimmune hepatitis [4, 5]. The incidence of HCC in different regions of the world varies due to the incidence of the risk factors. Such countries are China, sub-Saharan Africa, Hong Kong and Taiwan with more than 15 cases per 100,000 populations per year [6]. Any agent leading to chronic hepatic injury and eventually cirrhosis has been associated with HCC. Although multiple etiologic factors are responsible for HCC, it has been made a significant progress in these past years in the understanding of the molecular mechanisms and the pathogenesis of this disease. This article provides an overview of this disease based on our extensive review of relevant literature. We will summarize the current risk factors, diagnosis, staging and the management of HCC.
Global variation of the incidence of HCC is in relation with the complex etiology of the neoplasm and the literature data depends on the evaluated region and population, time in which the studies are done or the used methodologies.
Relevant information can be provided by GLOBALCAN database maintained by the International Agency for Research on Cancer (Figure 1, 2) [7, 8].
Figure 1.
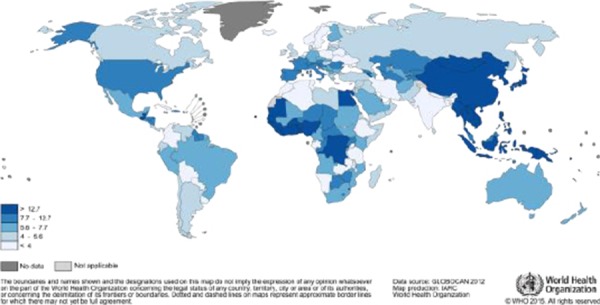
Estimated Liver Cancer Incidence Worldwide in 2012: Men (http://globocan.iarc.fr/old/FactSheets/cancers/liver-new.asp)
Figure 2.
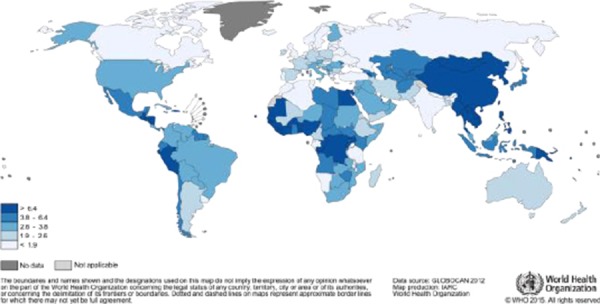
Estimated Liver Cancer Incidence Worldwide in 2012: Women (http://globocan.iarc.fr/old/FactSheets/cancers/liver-new.asp)
Risk factors
Almost 50% of all cases of HCC are associated with HBV infection and 25% are associated with HCV [9]. HBV is double-stranded DNA-containing virus that is able to integrate its DNA into the hepatic cells, act as a mutagenic agent and cause secondary chromosomal rearrangement and increasing genomic instability [10]. This is the reason why the risk of HCC development is 100-fold higher for patients who are infected with HBV in comparison with those who are not infected [11].
Major cause of HCC in Europe, Japan, Latin America and the United States is cirrhosis caused by hepatitis C virus infection and the annual incidence ranges from 2% to 8% [9, 10]. Generally HCV-infected patients have 17 fold higher risk of developing HCC than uninfected [11-13]. HCV is an RNA-containing virus, unable to integrate into the host genome and therefore causes HCC by various indirect mechanisms such as alterations in apoptotic pathways and tumor formation [5, 14].
Obesity and diabetes mellitus have been correlated with increased risk of HCC [15, 16]. These patients have twice higher chance of developing HCC compared to those who are not obese and do not have diabetes [17]. Alcohol is another important risk factor for developing HCC with increasing as levels of alcohol intake rise [16]. Chronic consumption of alcohol from 40 to 60 grams of alcohol on a daily bases are highly associated with HCC [18]. Aflatoxin is a mycotoxin produced by Aspergillus flavus and related fungus that contaminates stored foods such as rice, corn, soybeans, and peanuts. In some regions of the world, especially in Asia and Africa, it is major risk factors of HCC [19]. Chronic exposure to aflatoxin is highly associated with HCC due to damaging the DNA of hepatic cells and causing mutation of the p53 tumor suppressor gene [20]. Mutations of other genes and chromosome aberrations are described in HCC also. Point mutation of the c-KRAS gene and co-amplification of the cyclin D1 gene are rare and are detected in 3% and 11% of HCCs respectively. Mutations of beta-catenin gene are detected in 26-41% of HCCs. Frequent allelic losses are reported at loci 1p, 4q, 5q, 8p, 11p, 13q, 16p, 16q and 17p and loss of heterozygosity (LOH) is reported on chromosome 16. Reduction of expression of p21WAF/CIP1 (universal CDK inhibitor), P16 protein loss, high level expression of transforming growth factor-beta (TGF-beta), high expression of DNA metiltransferase (DNMT1) mRNA are found in significant percentage of HCCs.
There is increased risk of developing HCC in several rare inherited disorders: glycogen storage disease, alpha-1-antitrypsin deficiency, metal storage disease and chronic cholestatic syndromes [21].
Diagnosis
In many patients, HCC is asymptomatic and when symptoms occur they are usually related to those of chronic liver disease such as yellowing of the skin and eyes, pain in the right upper abdominal side, swelling of the abdomen, weakness, weight loss, fever [19, 22]. Over the past decades more asymptomatic patient are being diagnosed as a result of the active surveillance and the increased awareness of HCC in high risk patients, especially in those with cirrhosis. Screening for HCC in these patients is recommended every six months [1] and most used tools are serum levels of alpha-fetoprotein (AFP) and ultrasound [22]. Also the role of the serum level of AFP not always correlate with the tumor growth and it has been showed that is less useful than previously tough [23]. Generally values over 400 ng/mL can confirm the diagnosis in 20% of HCC patients [19]. The diagnosis of HCC can be made by history, physical examination and using noninvasive imaging methods such as ultrasound, MRI and CT scan. Suspicious lesion in the liver detected by ultrasound usually requires additional imaging methods to confirm the diagnosis and to detect additional, smaller, lesions that previously were not seen. Specificity and sensitivity of the ultrasound depends on the size of the tumor, ability to detect tumors 3-5cm in diameter is 80-95% and 60-80% of tumors <1cm in diameter [5, 24]. Standard noninvasive diagnostic methods for diagnosing HCC are dynamic multiphasic multidetector-row CT (MDCT) and magnetic resonance imaging (MRI) [25]. Typical finding for HCC in contrast enhanced CT is arterial phase enhancement followed by loss of enhancement (washout) in the portal venous and delayed phases [26]. This image finding has a sensitivity of 90% and specificity of 95% for diagnosing HCC [26, 27]. Nodules less that 1 cm are difficult to assess and usually image-guided biopsy should be considered for these lesions [28]. This also should be done for focal hepatic masses with atypical imaging features or discrepant findings on CT and MRI, or for lesions detected in the absence of cirrhosis [1]. A negative result from the biopsy does not rule out malignancy and continuous surveillance and ultrasound check up is needed in intervals from 3 till 6 months until they grow in size or change their echo pattern [29].
Treatment
Tumor staging has an essential role in guiding and making decision for further treatment. There are many systems to use in patients with HCC, but today most effective and most used is the Barcelona Clinic Liver Cancer (BCLC) classification [30] (Figure 3).
Figure 3.
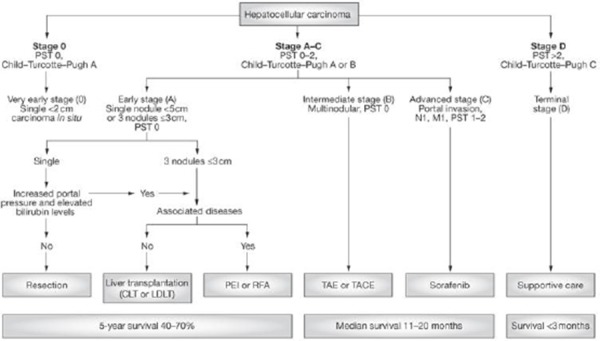
Barcelona Clinic Liver Cancer (BCLC) classification. *PST – Performance Status Test.
Performance status scale is developed by the Eastern Cooperative Oncology Group (ECOG) is included in BCLC system and is used to evaluate the progression of diseases (Figure 4).
Figure 4.
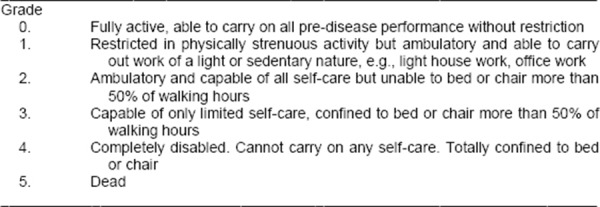
Performance status.
Child-Turcotte-Pugh score which is also included in BCLC is used to assess the prognosis of chronic liver disease (Figure 5).
Figure 5.
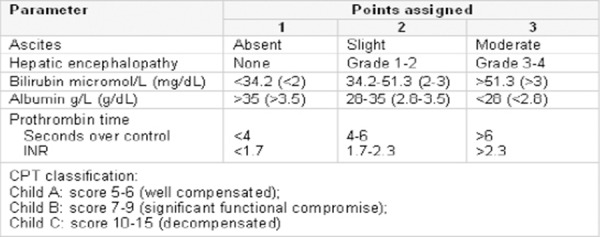
Child-Turcotte-Pugh score.
Using the BCLC system can help the doctor classify the patients with early-stage HCC, who may benefit from curative therapies and the patients with advanced-stage disease who would need palliative treatment. Sadly majority of patients present with advanced HCC at the time of diagnosis and are not candidate for curative therapies. Depending of the stage of the disease there are several therapeutic choices: surgical resection, percutaneous ethanol injection (PEI), radiofrequency ablation (RFA), transarterial chemoembolization (TACE) and radio-embolization [31].
First option for patients who have optimal profile according to BCLC staging system should be resection [32]. Surgical resection is the choice of treatment for patients with single nodules, no underlying cirrhosis and good liver function [33]. Treatment with PEI and RFA are optimal treatment option for patients with small tumours who are not candidates for surgical resection or liver transplantation [26]. Treatment with radiofrequency ablation demonstrated that complete ablation of lesions smaller than 2 cm is possible in more than 90% of cases, with a local recurrence rate of less than 1% [32, 34]. Survival rates after this treatment is 100% at first year and 98% at second year [1]. Standard treatment for the patients with intermediate-stage HCC is TACE. Patients with compensated liver function (Child B up to 8 points), with large single nodule (< 5 cm) or multifocal HCC without evidence of vascular invasion or extra hepatic spread are considered candidates for TACE [33]. Also TACE plays an important role in the palliative treatment and it is a standard choice of treatment in patients with asymptomatic multinodular disease [35]. The prognosis of patients with HCC is poor in symptomatic patients in whom five-year survival rate is reported to be less than 5%. It is very poor in patients with AFP levels greater than 100ng/ml at the time of diagnosis, portal vein thrombosis and presence of p53 mutation. Long –term survival is reported only in patients with small, asymptomatic HCC (Table 1).
Table 1.
Estimated Incidence, Mortality and Prevalence of liver cancer Worldwide in 2012. Estimated numbers (thousands) http://globocan.iarc.fr/old/FactSheets/cancers/liver-new.asp
| Men | Women | Both sexes | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Cases | Deaths | 5-year prev. | Cases | Deaths | 5-year prev. | Cases | Deaths | 5-year prev. | |
| World | 554 | 521 | 453 | 228 | 224 | 180 | 782 | 746 | 633 |
| More developed regions | 92 | 80 | 112 | 42 | 43 | 51 | 134 | 123 | 164 |
| Less developed regions | 462 | 441 | 341 | 186 | 182 | 129 | 648 | 622 | 469 |
| WHO Africa region (AFRO) | 25 | 24 | 17 | 14 | 13 | 9 | 39 | 37 | 26 |
| WHO Americas region (PAHO) | 40 | 35 | 35 | 23 | 23 | 18 | 63 | 58 | 53 |
| WHO East Mediterranean region (EMRO) | 20 | 19 | 12 | 10 | 9 | 6 | 29 | 28 | 18 |
| WHO Europe region (EURO) | 47 | 44 | 42 | 23 | 25 | 20 | 71 | 69 | 61 |
| WHO South-East Asia region (SEARO) | 55 | 52 | 33 | 25 | 24 | 15 | 80 | 77 | 48 |
| WHO Western Pacific region (WPRO) | 368 | 347 | 314 | 133 | 129 | 112 | 501 | 477 | 426 |
| IARC membership (24 countries) | 120 | 104 | 135 | 56 | 55 | 60 | 176 | 159 | 195 |
| United States of America | 23 | 17 | 21 | 8 | 7 | 7 | 30 | 24 | 27 |
| China | 293 | 282 | 220 | 101 | 101 | 71 | 395 | 383 | 291 |
| India | 17 | 17 | 8 | 10 | 10 | 5 | 27 | 27 | 13 |
| European Union (EU-28) | 36 | 32 | 33 | 16 | 17 | 14 | 52 | 48 | 47 |
The development of new drugs and types of therapy can improve the outcome of patients with hepatocellular carcinoma, but the key factor in management of HCC is still making a diagnosis in the very-early stages of disease and continuously surveillance of the patients with a high risk of HCC [1, 36, 37].
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.El-Serag HB. Hepatocellular Carcinoma. N Engl J Med. 2011;365:1118–27. doi: 10.1056/NEJMra1001683. http://dx.doi.org/10.1056/NEJMra1001683 . PMid:21992124. [DOI] [PubMed] [Google Scholar]
- 2.Simonetti RG, Liberati A, Angiolini C, Pagliaro L. Treatment of hepatocellular carcinoma: A systematic review of randomized controlled trials. Annals of Oncology. 1997;8:117–136. doi: 10.1023/a:1008285123736. http://dx.doi.org/10.1023/A:1008285123736 . PMid:9093719. [DOI] [PubMed] [Google Scholar]
- 3.El-Serag HB, Rudolph KL. Hepatocellular Carcinoma: Epidemiology and Molecular Carcinogenesis. Gastroenterology. 2007;132:2557–2576. doi: 10.1053/j.gastro.2007.04.061. http://dx.doi.org/10.1053/j.gastro.2007.04.061 . PMid:17570226. [DOI] [PubMed] [Google Scholar]
- 4.Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: Part I. Diagnosis and evaluation. Am Fam Physician. 2006;74:756–762. PMid:16970019. [PubMed] [Google Scholar]
- 5.Sanyal AJ, Yoon SK, Lencioni R. The Etiology of Hepatocellular Carcinoma and Consequences for Treatment. The Oncologist. 2010;15(suppl 4):14–22. doi: 10.1634/theoncologist.2010-S4-14. http://dx.doi.org/10.1634/theoncologist.2010-S4-14 . PMid:21115577. [DOI] [PubMed] [Google Scholar]
- 6.Munoz N, Bosch X. Epidemiology of hepatocellular carcinoma. In: Okuda K, Ishak KG, editors. Neoplasms of the Liver. Tokyo: Springer; 1989. p. 3. [Google Scholar]
- 7.Venook AP, Papandreou C, Furuse J, Ladrón de Guevara L. The Incidence and Epidemiology of Hepatocellular Carcinoma: A Global and Regional Perspective The Oncologist. 2010;15:5–13. doi: 10.1634/theoncologist.2010-S4-05. [DOI] [PubMed] [Google Scholar]
- 8.Parkin DM, Bray F, Ferlay J, et al. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. http://dx.doi.org/10.3322/canjclin.55.2.74 . PMid:15761078. [DOI] [PubMed] [Google Scholar]
- 9.Gurtsevitch VE. Human oncogenic viruses: Hepatitis B and hepatitis C viruses and their role in hepatocarcinogenesis. Biochemistry (Mosc) 2008;73:504–513. doi: 10.1134/s0006297908050039. http://dx.doi.org/10.1134/S0006297908050039 . [DOI] [PubMed] [Google Scholar]
- 10.Szabó E, Páska C, Kaposi Novák P, et al. Similarities and differences in hepatitis B and C virus induced hepatocarcinogenesis. Pathol Oncol Res. 2004;10:5–11. doi: 10.1007/BF02893401. http://dx.doi.org/10.1007/BF02893401 . PMid:15029254. [DOI] [PubMed] [Google Scholar]
- 11.Alan D, Herbst BA, Reddy KR. Risk Factors for Hepatocellular Carcinoma. Clinical Liver Disease. 2012;1(6) doi: 10.1002/cld.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferenci P, Fried M, Labrecque D, Bruix J, Sherman M, Omata M, et al. World Gastroenterology Organisation guideline. Hepatocellular carcinoma (HCC): a global perspective. J Gastrointestin Liver Dis. 2010;19:311–317. http://dx.doi.org/10.1097/mcg.0b013e3181d46ef2 . [PubMed] [Google Scholar]
- 13.Donato F, Tagger A, Gelatti U, et al. Alcohol and hepatocellular carcinoma: The effect of lifetime intake and hepatitis virus infections in men and women. Am J Epidemiol. 2002;155:323–331. doi: 10.1093/aje/155.4.323. http://dx.doi.org/10.1093/aje/155.4.323 . PMid:11836196. [DOI] [PubMed] [Google Scholar]
- 14.Sheikh MY, Choi J, Qadri I, et al. Hepatitis C virus infection: Molecular pathways to metabolic syndrome. Hepatology. 2008;47:2127–2133. doi: 10.1002/hep.22269. http://dx.doi.org/10.1002/hep.22269 . PMid:18446789. [DOI] [PubMed] [Google Scholar]
- 15.Polesel J, Zucchetto A, Montella M, Dal Maso L, Crispo A, La Vecchia C, et al. The impact of obesity and diabetes mellitus on the risk of hepatocellular carcinoma. Ann Oncol. 2009;20:353–357. doi: 10.1093/annonc/mdn565. http://dx.doi.org/10.1093/annonc/mdn565 . PMid:18723550. [DOI] [PubMed] [Google Scholar]
- 16.Ascha MS, Hanouneh IA, Lopez R, Abu-Rajab Tamini T, Feldstein AF, Zein NN. The Incidence and Risk Factors of Hepatocellular Carcinoma in Patients with Nonalcoholic Steatohepatitis. Hepatology. 2010;51(6):1972–8. doi: 10.1002/hep.23527. http://dx.doi.org/10.1002/hep.23527 . PMid:20209604. [DOI] [PubMed] [Google Scholar]
- 17.El-Serag HB, Hampel H, Javadi F. The association between diabetes and hepatocellular carcinoma: a systematic review of epidemiologic evidence. Clin Gastroenterol Hepatol. 2006;4:369–80. doi: 10.1016/j.cgh.2005.12.007. http://dx.doi.org/10.1016/j.cgh.2005.12.007 . PMid:16527702. [DOI] [PubMed] [Google Scholar]
- 18.Donato F, Tagger A, Gelatti U, et al. Alcohol and hepatocellular carcinoma: the effect of lifetime intake and hepatitis virus infections in men and women. Am J Epidemiol. 2002;155:323–31. doi: 10.1093/aje/155.4.323. http://dx.doi.org/10.1093/aje/155.4.323 . PMid:11836196. [DOI] [PubMed] [Google Scholar]
- 19.Raphael SW, Yangde Z, YuXiang C. Hepatocellular Carcinoma: Focus on Different Aspects of Management ISRN Oncology. 2012 doi: 10.5402/2012/421673. Article ID 421673: 12 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bressac B, Kew M, Wands J, Ozturk M. Selective G to T mutations of p53 gene in hepatocellular carcinoma from southern Africa. Nature. 1991;350:429. doi: 10.1038/350429a0. http://dx.doi.org/10.1038/350429a0 . PMid:1672732. [DOI] [PubMed] [Google Scholar]
- 21.Hirohashi S, Blum HE, Ishak KG, Deugnier Y, Kojiro M, Laurent Puig P, Wanless IR, Fischer HP, Theise ND, Sakamoto M, Tsukuma H. Hepatocellular carcinoma in World Health Organization Classification of Tumours Pathology and Genetics of Tumours of the Digestive System IARCPress Lyon. 2000 [Google Scholar]
- 22.El-Serag HB, Marrero JA, Rudolph L, Reddy KR. Diagnosis and treatment of hepatocellular carcinoma. Gastroenterology. 2008;134(6):1752–1763. doi: 10.1053/j.gastro.2008.02.090. http://dx.doi.org/10.1053/j.gastro.2008.02.090 . PMid:18471552. [DOI] [PubMed] [Google Scholar]
- 23.Somi MH. Hepatocellular Carcinoma. Hepatitis Monthly. 2005;5(3):65–76. [Google Scholar]
- 24.Ryder SD. British Society of Gastroenterology. Guidelines for the diagnosis and treatment of hepatocellular carcinoma (HCC) in adults. Gut. 2003;52(suppl 3):iii1–iii8. doi: 10.1136/gut.52.suppl_3.iii1. http://dx.doi.org/10.1136/gut.52.suppl_3.iii1 . PMid:12692148 PMCid:PMC1867754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bolog N, Andreisek G, Oancea I, Mangrau A. CT and MR imaging of hepatocellular carcinoma. Journal of Gastrointestinal and Liver Diseases. 2011;20(2):181–189. PMid:21725516. [PubMed] [Google Scholar]
- 26.Cabrera R, Nelson DR. Review article: the management of hepatocellular carcinoma. Aliment Pharmacol Ther. 2010;15;31(4):461–76. doi: 10.1111/j.1365-2036.2009.04200.x. [DOI] [PubMed] [Google Scholar]
- 27.Marrero JA, Hussain HK, Nghiem HV, et al. Improving the prediction of hepatocellular carcinoma in cirrhotic patients with an arterially-enhancing liver mass. Liver Transpl. 2005;11:281–9. doi: 10.1002/lt.20357. http://dx.doi.org/10.1002/lt.20357 . PMid:15719410. [DOI] [PubMed] [Google Scholar]
- 28.Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–36. doi: 10.1002/hep.20933. http://dx.doi.org/10.1002/hep.20933 . PMid:16250051. [DOI] [PubMed] [Google Scholar]
- 29.Hepatocellular Carcinoma: Novel Molecular Targets in Carcinogenesis for Future Therapies. Bertino G, Demma S, Ardiri A, Proiti M, Gruttadauria S, Toro A, Malaguarnera G, Bertino N, Malaguarnera M, Malaguarnera M, Di Carlo I. BioMed Research International. 2014 doi: 10.1155/2014/203693. Article ID 203693: 15 pages. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 30.Pons F, Varela M, Llovet MJ. Staging systems in hepatocellular carcinoma. HPB (Oxford) 2005;7(1):35–41. doi: 10.1080/13651820410024058. http://dx.doi.org/10.1080/13651820410024058 . PMid:18333159 PMCid:PMC2023920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.European Association For The Study Of The Liver, European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908–943. doi: 10.1016/j.jhep.2011.12.001. http://dx.doi.org/10.1016/j.jhep.2011.12.001 . PMid:22424438. [DOI] [PubMed] [Google Scholar]
- 32.Bruix J, Shereman M. Management of hepatocellular carcinoma: An update. Hepatology. 2011;53(3):1020–1022. doi: 10.1002/hep.24199. http://dx.doi.org/10.1002/hep.24199 . PMid:21374666 PMCid:PMC3084991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Raza A, Sood GK. Hepatocellular carcinoma review: Current treatment, and evidence-based medicine. World J Gastroenterol. 2014;20(15):4115–4127. doi: 10.3748/wjg.v20.i15.4115. http://dx.doi.org/10.3748/wjg.v20.i15.4115 . PMid:24764650 PMCid:PMC3989948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Livraghi T, Meloni F, Di Stasi M, Rolle E, Solbiati L, Tinelli C, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: Is resection still the treatment of choice? Hepatology. 2008;47:82–89. doi: 10.1002/hep.21933. http://dx.doi.org/10.1002/hep.21933 . PMid:18008357. [DOI] [PubMed] [Google Scholar]
- 35.Wang P, Sheng L, Mang G, Wang H, Huang X, Yan X, Yang X, Pei R. Association of transarterial chemoembolization with survival in patients with unresectable hepatocellular carcinoma. Mol Clin Oncol. 2014;2(2):203–206. doi: 10.3892/mco.2014.239. PMid:24649333 PMCid:PMC3917780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Greten T F, Papendorf F, Bleck J S, Kirchhoff T, Wohlberedt T, Kubicka S, Klempnauer J, Galanskiand M, Manns M P. Survival rate in patients with hepatocellular carcinoma: a retrospective analysis of 389 patients. BJC. 2005;92:1862–1868. doi: 10.1038/sj.bjc.6602590. http://dx.doi.org/10.1038/sj.bjc.6602590 . PMid:15870713 PMCid:PMC2361778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hirohashi S, Blum HE, Ishak KG, Deugnier Y, Kojiro M, Laurent Puig P, Wanless IR, Fischer HP, Theise ND, Sakamoto M, Tsukuma H. Hepatocellular carcinoma in World Health Organization Classification of Tumours Pathology and Genetics of Tumours of the Digestive System. Lyon: IARC Press; 2000. [Google Scholar]


