Abstract
Until recently, estimation of β-amyloid plaque density as a key element for identifying Alzheimer's disease (AD) pathology as the cause of cognitive impairment was only possible at autopsy. Now with amyloid-positron emission tomography (amyloid-PET) neuroimaging, this AD hallmark can be detected antemortem. Practitioners and patients need to better understand potential diagnostic benefits and limitations of amyloid-PET and the complex practical, ethical, and social implications surrounding this new technology. To complement the practical considerations, Eli Lilly and Company sponsored a Bioethics Advisory Board to discuss ethical issues that might arise from clinical use of amyloid-PET neuroimaging with patients being evaluated for causes of cognitive decline. To best address the multifaceted issues associated with amyloid-PET neuroimaging, we recommend this technology be used only by experienced imaging and treating physicians in appropriately selected patients and only in the context of a comprehensive clinical evaluation with adequate explanations before and after the scan.
Keywords: Alzheimer's disease, Mild cognitive impairment, Bioethics in neurology, Positron emission tomography, Diagnostic use, Dementia, Biomarkers, Amyloid-β
1. Introduction
Amyloid-β positron emission tomography (hereafter termed amyloid-PET) neuroimaging has been a useful tool in Alzheimer's disease (AD) research [1], [2], [3] and as a technique for subject enrichment in AD clinical trials to ensure that only those with underlying β-amyloid plaque pathology are enrolled [4]. The recent clinical availability of amyloid-PET now allows physicians to estimate the density of β-amyloid plaques during life, rather than postmortem, and to assess whether significant amyloid-β burden (moderate-to-frequent neuritic plaques needed to meet pathologic criteria for intermediate or high likelihood that AD pathology is the cause of dementia) is present. However, although amyloid-PET accurately detects the presence of β-amyloid plaques, the scan by itself captures only one core element of AD pathology (neuritic plaques but not neurofibrillary tangles). For example, patients with amyloid-β pathology often have other neuropathologies such as Lewy bodies or cerebrovascular disease, and interpretation may be further complicated by factors such as depression and cognitive impairment due to medications. As amyloid-PET enters into clinical use, it is important that practitioners and patients understand the potential diagnostic benefits and limitations of amyloid-PET. Furthermore, they need to recognize the complex practical, ethical, and social implications surrounding this new technology.
To complement the practical considerations, Eli Lilly and Company (Lilly) sponsored a multidisciplinary Bioethics Advisory Board to consider bioethical issues that might arise when using amyloid-PET as an adjunctive diagnostic tool to clinically evaluate patients with cognitive impairment. Our intent was not to propose evidence-based guidelines for clinical use of amyloid-PET because these were already being developed and subsequently published by the joint efforts of the Society of Nuclear Medicine and Molecular Imaging (SNMMI) and the Alzheimer's Association (AA) [5], [6]. Instead, we considered whether clinical use might have unexpected implications within and beyond interactions between doctors and patients and their families.
Academic experts in dementia, PET neuroimaging, bioethics, and a representative from a United States-based caregiver advocacy group discussed issues with Lilly and Avid Radiopharmaceuticals staff. Topics included ethical issues related to the diagnosis, management, and practical life concerns faced by patients, caregivers, and physicians/health care professionals. After the advisory board meeting, a subgroup of attendees collaborated to refine the concepts discussed and to write this report. In addition to a description of pertinent ethical issues, we will also present case study examples that illustrate application of bioethical principles for decision-making with individual patients and clinical situations. Finally, we provide practical recommendations for clinicians to consider when discussing the use of amyloid-PET with patients and their families.
2. Background
AD is the most common cause of gradually progressive cognitive and functional decline in older persons and accounts for 60%–80% of all dementias [7], [8]. Clinical diagnosis of AD has been primarily made by assessing progressive decline in cognitive abilities and ruling out other common causes for cognitive impairment [9], [10], [11]. Thus, clinical information was used to infer the presence of AD pathology. Understandably, this inference was not always accurate and neuropathologic examination has remained the “gold standard.” Recently, studies have assessed the accuracy of clinical diagnostic methods for possible or probable AD compared with neuropathology at autopsy. One study reported that the sensitivity of clinical AD diagnoses ranged from 70.9% to 87.3% and specificity ranged from 44.3% to 70.8% versus pathology, depending on the levels of certainty for either clinical or neuropathologic criteria [12]. Difficulty in achieving accurate clinical diagnoses of AD may arise because common dementing diseases, such as vascular dementia, dementia with Lewy bodies, frontotemporal dementia and others, share many symptoms with dementia due to AD and frequently coexist with AD pathology [13], [14]. It is not surprising in these circumstances that postmortem studies find that the accuracy of clinical diagnosis of cognitive disorders can range widely depending on the population studied, the intensity of evaluation, and the skill of the clinician [12], [14], [15], [16].
Furthermore, the National Institute on Aging (NIA)-Reagan neuropathologic criteria for AD classified findings as indicating low, intermediate, or high likelihood that the pathology caused the dementia, explicitly recognizing that β-amyloid plaques and neurofibrillary tangles alone did not always closely correlate with clinical symptoms [17].
Clinical diagnostic criteria for AD were revised in 2011 to incorporate new advances including biomarkers and to help physicians better define the full spectrum of AD [11], [18]. The NIA-Alzheimer's Association Task Force guidelines define the diagnostic phases of AD to include an asymptomatic phase, a “mild cognitive impairment” predementia phase, and the full expression of deficits in an AD dementia phase. According to these guidelines, a clinical diagnosis of possible or probable AD can be made with or without biomarker evidence, but biomarker results are considered to increase the level of diagnostic certainty. For the first time, the criteria incorporated biomarker results to define “dementia unlikely due to AD” when biomarkers of AD pathology were negative [11], [18].
The clinical diagnosis of AD is primarily based on patient history, physical examination, cognitive assessment, laboratory tests, and neuroimaging to identify other possible causes or contributors to cognitive impairment [19]. However, there is a paradigm shift in the field of cognitive impairment evaluation moving away from a symptom-only diagnosis to a biomarker-aided diagnosis. AD biomarkers are grouped into two major categories as follows: (1) pathology-specific biomarkers of amyloid-beta accumulation, which are abnormal tracer retention on amyloid-PET or low cerebrospinal fluid (CSF) amyloid-β1–42 levels, with elevated CSF tau (both total and phosphorylated tau) and (2) nonspecific neuroimaging biomarkers of neuronal degeneration or injury, which are decreased fluorodeoxyglucose uptake on PET in a specific topographic pattern involving temporoparietal and posterior cingulate cortex, and hippocampal atrophy on structural magnetic resonance imaging [20]. Each of these biomarker tests has different strengths and weaknesses regarding their utility as adjunctive diagnostic tests in clinical settings when a patient is evaluated for suspected AD [21]. Additionally, there are important differences with respect to insurance coverage and reimbursement for the different biomarkers.
The 2014 International Working Group guidelines revision suggests that neurodegeneration biomarkers not be considered specific to AD for making a diagnosis in the manner that amyloid-PET and CSF are used [22]. We focus on potential issues relating to the use of amyloid-PET in clinical settings, although some of the principles apply to the clinical use of other biomarkers.
3. Current state of AD diagnosis in clinical practice
Currently, primary care physicians are often the first to learn of a cognitive complaint and perform the initial assessment of a patient's cognitive decline. The complexity associated with differential diagnosis of cognitive impairment and AD, in particular, can be difficult for many primary care physicians who are not specialists in dementia care. Postmortem neuropathology studies indicate that even dementia experts often have difficulty in making an accurate clinical diagnosis of AD [12], [23].
The growing epidemic of AD is becoming more widely appreciated. However, in medical practice, there is reluctance among primary care practitioners to specify the cause of dementia or discuss an Alzheimer's diagnosis with patients and their families [24], [25], [26]. Reasons for this reluctance may include a lack of effective treatment options, the physician's lack of confidence in diagnosing the cause of cognitive impairment (particularly early in the course of the disease when symptoms are mild), and concern about upsetting the patient or family [25], [27]. This often leads to a delay in determining the specific cause and initiating treatment, or referral to a specialist, including proactive patient and family education and support [28]. Skepticism about the ability to accurately determine the cause of cognitive impairment often leads to skepticism about the value of treatment.
4. Current state of amyloid-PET neuroimaging
Amyloid-β deposition is most often seen in the context of cognitive impairment due to AD, but may also be comorbid with other neurologic conditions (e.g., cerebrovascular disease, cerebral amyloid-β angiopathy or dementia with Lewy bodies) that may be additive to the AD pathology or even responsible for the patients' cognitive impairment [13], [29]. Amyloid-β pathology can also be present in clinically normal older individuals [30]. Evidence is mounting to suggest amyloid-β–positive clinically normal individuals may have subtle cognitive impairments and may be more likely to decline than amyloid-β–negative individuals. However, not all clinically normal amyloid-β–positive individuals experience meaningful cognitive decline. Thus far, only a small percentage have been followed to the development of dementia, and it is not clear how to predict which individuals will decline or whether other pathologic changes must occur to place a subject on the path to dementia. Long-term follow-up from clinical studies is needed to understand the role of amyloid-β pathology in asymptomatic persons [31], [32], [33], [34].
Therefore, although studies suggest that amyloid-PET accurately detects the presence of β-amyloid plaques, an important limitation of this technique is that it does not differentiate among the different conditions with which this neuropathology is associated. It simply informs about the density of β-amyloid neuritic plaques, which must be interpreted in the context of the individual patient's symptom profile and entire evaluation for cause(s) of cognitive impairment [5], [6]. Acknowledging that AD is the most prevalent cause for dementia in older persons, it will be a top consideration in the differential diagnosis with a positive amyloid-PET scan result. However, this prevalence should not preempt a thorough and broader search for comorbid etiologies, especially for those that might be reversible or have a different prognosis and treatment, such as dementia caused by drugs, alcohol, hormone or vitamin imbalances, or depression. However, a negative amyloid-PET scan excludes amyloid-β pathology with high confidence.
The US Food and Drug Administration has approved three F18 amyloid-PET radiotracers for clinical use [35], [36], [37]. Because of a high level of patient and professional interest [38], amyloid-PET has the potential to be widely used despite constraints related to insurance coverage, cost, and local availability from regional radiopharmaceutical manufacturing networks. At the same time, there is widespread misunderstanding among the public and many clinicians about the risks of developing cognitive impairment, methods used to diagnose cognitive impairment, different causes of dementia, and available treatment options. Therefore, physicians with knowledge and experience incorporating amyloid-PET results into the evaluation and care of those with dementing disease are perhaps in the best position to use this new technology appropriately during these introductory years.
Currently, approved drug treatments for AD dementia can alter the symptoms and the clinical course that patients experience, but no proven treatments halt the progression of AD or delay or prevent the onset of AD [39]. In the absence of any disease pathology–modifying therapies, results of amyloid-PET can nonetheless provide critical information regarding the presence or absence and regional patterns of β-amyloid plaque pathology. This information may, in turn, influence treatment choice. For example, if amyloid-PET does not demonstrate significant β-amyloid plaque pathology, such that AD can be confidently excluded as a cause of cognitive impairment, AD-directed drug treatment could be discontinued and treatment directed to likely non-AD causes. Alternatively, if β-amyloid plaque pathology can be confirmed, use of AD drug treatment is justified, and common AD complications can be identified earlier and managed more appropriately.
5. Ethical decision points when using amyloid-PET neuroimaging
Bioethical principles should provide guidance for clinical use, recognizing that these considerations may need to be refined in the future as we learn more about the disease and its prognosis and develop more efficacious treatment options.
5.1. Value of knowing the cause of cognitive impairment
Before ordering amyloid-PET, physicians, patients, and care partners should understand the value of knowing amyloid-β status, whether positive or negative. Patients and families value an accurate diagnosis and knowing they are receiving care that includes state-of-the-art assessment procedures. A prospective study [25] found that patients often showed reduced levels of anxiety after diagnosis of a dementing condition. In another study, patients complained that their primary care providers often failed to accurately evaluate dementia and dismissed early symptoms, attributing them to “just aging” [40]. Some caregivers thought the dementia evaluation was not thorough enough or the diagnosis was based on incomplete information [40]. Caregivers who were provided more information about the cause of a loved one's impairment experienced significantly lower levels of depression, were more likely to have realistic expectations of their dependents' abilities, and felt more competent and confident as caregivers [25], [26].
By documenting the absence or presence of neuropathology, an amyloid-PET scan may provide valuable knowledge to both patients and family members. Importantly, as with any diagnostic test, users of this technology will need to understand that there will always be the possibility for false-positive, false-negative, or indeterminate results (e.g., due to acquisition or interpretation errors). However, a negative amyloid-PET scan is inconsistent with a neuropathologic diagnosis of AD, thus reducing the likelihood that the patient's cognitive impairment is due to AD and suggesting the need for further diagnostic efforts. Additionally, in patients suspected of having dementia or mild cognitive impairment due to AD, there is emerging evidence that a negative amyloid-PET scan indicates lower probability of clinically significant cognitive deterioration for at least the next 36 months [30], [41], [42], [43]. Alternatively, a positive amyloid-PET scan may increase a clinician's confidence in diagnosing AD [44], [45].
A confident and specific diagnosis also helps patients and families cope with the inherent difficulty of life-altering decisions and changes in lifestyle, as well as the uncertainty of future needs [25], [46]. In some circumstances, the patient may not wish to know the diagnosis or cannot appreciate its meaning [47]. However, even in this situation, family members may want to know the cause of impairment to aid their own understanding and planning [48]. Providing patients and family members the opportunity to make informed autonomous plans and decisions is consistent with the ethical principle of respect for persons, but the limitations of the test and the possible benefits and harms of “knowing” must be explained clearly and in advance.
The value of knowing the cause of cognitive impairment also extends to health professionals. One ethical dilemma for health professionals is balancing a patient's (and caregiver's) right to know the cause of cognitive impairment (and thus the provider's obligation to disclose a diagnosis) with a provider's wish to withhold certain information for fear this information may harm the patient. Anticipated harms could include anxiety, depression or ill-advised decisions based on unwarranted assumptions. When a provider withholds information in an attempt to protect a patient's emotional wellbeing, this is known as “benevolent deception.” Benevolent deception is more common in some societal traditions than others. Sometimes family members even request such deception.
The decision of whether to disclose a diagnosis of AD may be influenced by how comfortable, or certain, the physician is in the diagnosis. Identifying the presence or absence of amyloid-β pathology provides additional information that is likely to enhance their confidence in the accuracy of a diagnosis [44], [45]. The AA has established a recommendation on disclosing an AD diagnosis to an individual: “Except in unusual circumstances, physicians and the care team should disclose the diagnosis to the individual with Alzheimer's disease because of the individual's moral and legal right to know.” However, patients and families who express a direct desire “not to know” would likely not be good candidates for amyloid-PET, although the implications of uncertainty on patient care and future planning should be discussed.
Health care providers have an ethical responsibility to provide support for patients and their care partners [49]. Amyloid-PET results are likely to affect how the diagnosis and treatment recommendations are communicated and carried out [44]. Low levels of physician confidence can be unintentionally conveyed to family members and affect their willingness to act on recommendations. Confidence in the accuracy of diagnosis and the value of treatments are strongly linked to patient adherence [50]. Although a positive amyloid-PET result may indeed improve the diagnostic confidence for an AD diagnosis, and thus help with the ethical tension of whether or when to communicate a diagnosis of AD, the context of communicating a positive scan result by the treating physician needs to be individualized for a given patient and care partner [19].
5.2. Patient selection for amyloid-PET scan
Proper patient selection is fundamental before conducting any diagnostic test from ethical, legal, financial, and clinical perspectives. Recently, the AA and the SNMMI convened the Amyloid Imaging Task Force to provide guidance on appropriate patient selection to dementia care practitioners, patients, and caregivers [5], [6]. Appropriate use criteria (AUC) were proposed to define the patients and clinical circumstances in which amyloid-PET could be used but also described situations where the use of amyloid-PET would be considered inappropriate at this time [5], [6]. According to the AUC, amyloid-PET is appropriately used by dementia experts “when there is evidence of a cognitive complaint with objectively confirmed impairment; when AD is a possible diagnosis, but that diagnosis is uncertain after a comprehensive evaluation by an expert; and when knowledge of amyloid-β pathology is likely to increase diagnostic certainty and alter patient management” [5], [6].
The AUC working group recommended that amyloid-PET is inappropriate when used for patients meeting core clinical criteria for probable AD with typical age of onset (indicating entirely typical symptoms and examination and thus little reason for uncertainty); to determine dementia severity, based solely on family history of dementia or presence of the ε4 allele of apolipoprotein E (APOE); for patients with a cognitive complaint that is unconfirmed on clinical examination; in lieu of genotyping for suspected autosomal carriers; in asymptomatic individuals; and for nonmedical use (e.g., legal, insurance coverage or employment screening) [5], [6].
The potential for overuse and misuse of amyloid-PET is an ethical concern. The desire by both physicians and patients for a definitive test that explains the cause of symptoms is strong. Yet, if unnecessary testing is done, it could divert health care spending from providing interventions that are more useful for a particular patient. From the clinical perspective, over-reliance on amyloid-PET scan findings during clinical care is of particular concern. Clinicians who are not dementia specialists may be tempted to seek simple definitive tests and might prefer obtaining an amyloid-PET scan to completing a comprehensive clinical evaluation or even making a referral to a dementia specialist, especially given the pressure to see more patients in less time [51]. Evaluation of cognitive problems requires a substantial time commitment and complex decision making. A broad array of conditions must be considered, and identifying a dementing disease can uncover medical and social issues that are not easily addressed (e.g., social stigma resulting from a diagnosis). Therefore, it would be inappropriate for amyloid-PET to be performed outside of the context of a full clinical evaluation.
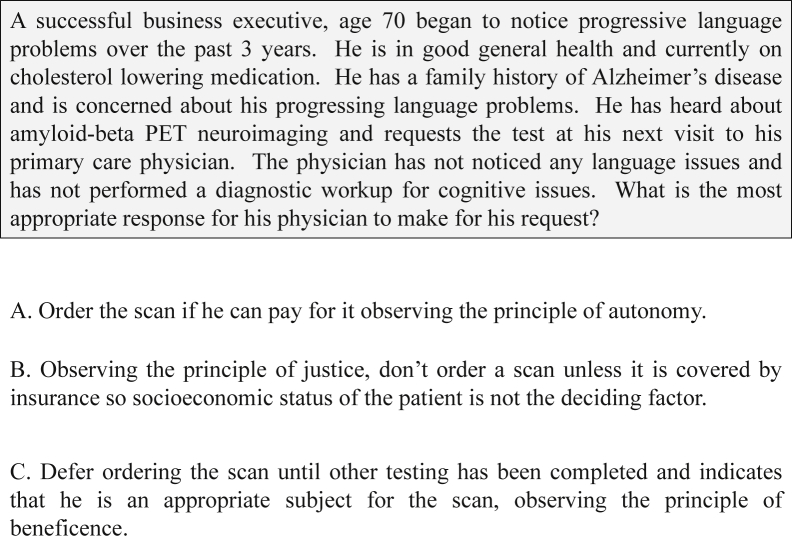
Further pressures might come from patients and families themselves, demanding that amyloid-PET be performed, possibly when it is not medically indicated or when symptoms are not present. For example, first-degree relatives of patients diagnosed with AD may request to be tested with amyloid-PET [52]. Fig. 1 depicts a hypothetical case in which a physician must decide the appropriate steps to take when faced with a patient who has had a history of progressive language problems and requests a scan. In this scenario, the physician needs to decide if the patient is an appropriate subject for amyloid-PET. As recommended by the AUC, before a decision regarding amyloid-PET, a standard work-up for causes of this patient's symptoms should be completed to establish the potential for AD in the differential diagnosis and to exclude other causes of the patient's language complaint. This may include more detailed language and cognitive testing to confirm the presence and type of language deficit, as well as recommended laboratory and imaging tests if indicated. It is recommended to defer ordering amyloid-PET pending the completion of other testing and only if knowledge of amyloid-β pathology will likely increase diagnostic certainty, observing the principle of beneficence.
Fig. 1.
A hypothetical case regarding ethical decisions physicians may face when selecting appropriate patients for amyloid-PET. The authors recommend approach option C. Abbreviation: PET, positron emission tomography.
There are also potential issues to consider regarding the underuse or omission of amyloid-PET. Some patients with cognitive impairment may be misdiagnosed and, either because of misplaced confidence in clinical methods or failure to consider all potential causes, may not be judged candidates for amyloid-PET [53]. In such situations, the potential benefit of correcting diagnostic errors with amyloid-PET would fail to be realized. Additionally, some patients with high cognitive reserve may tolerate significantly greater amyloid-β burden with fewer symptoms than those with low cognitive reserve, but when they develop dementia, they decline more rapidly [54]. In some instances, these patients may be regarded as “worried well” at an initial evaluation and not be considered for amyloid-PET. Then they and their families would lose the advantages associated with obtaining an early and accurate explanation for their complaint. Whether to consider the use of amyloid-PET in situations such as these will have to be made on a case-by-case basis considering the full context of the clinical circumstances.
In clinical practice, patient demands may be difficult to resist. Nevertheless, ethical principles indicate that relief of an asymptomatic individual's curiosity or anxiety is not sufficient to justify obtaining a scan, both because of the ethical principle of distributive justice (i.e., misuse of social resources) and because the clinical implications of an amyloid-PET result for an asymptomatic patient are not yet known (i.e., the precautionary principle) and may lead to drawing false conclusions. The ethical principle of beneficence requires that physicians not undertake interventions, if the risks outweigh their benefits. With further research, this risk-benefit ratio could change, particularly if current clinical trials involving individuals with preclinical AD are successful. At this time, there is insufficient research evidence that asymptomatic persons should be scanned, except in a research study.
5.3. Consequences of amyloid-PET results
Another concern is how, or will, the results of amyloid-PET change the approach to the care and education of the patient? If patients and families engage in reductionist thinking regarding amyloid results, they may attach greater importance to a brain PET scan result than is warranted. On the other hand, a scan could provide sufficient evidence to motivate patients and family members to accept the diagnosis from the physician and to make environmental changes if needed.
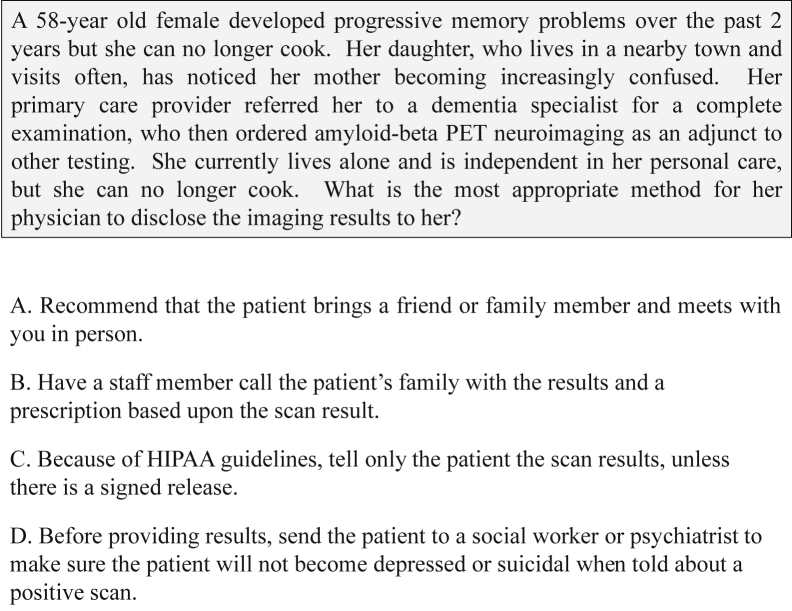
How should physicians explain what a positive or negative scan might mean to patients, especially given the limited longitudinal and prospective amyloid-PET data that are currently available? Simply telling patients and families about the results of the scan without providing further explanation or support could unnecessarily cause distress or misunderstanding. This is particularly important for patients with neuropsychological deficits in memory and language, which may make it difficult for some individuals to understand, recall, or discuss the information with their family or friends. Fig. 2 depicts a hypothetical case in which a physician must decide the best approach to report amyloid-PET results for an individual patient. It is the recommendation of the authors that in this situation a family member should be included when disclosing the scan results. Furthermore, recent qualitative research using mock amyloid-PET scan results found that despite a variety of emotional responses, care partners easily understood the scan result and its prognostic implications and most cognitively impaired patients had at least limited understanding. All wanted quick access to further management by their physicians [47].
Fig. 2.
A hypothetical case regarding ethical decisions physicians may face when disclosing amyloid-PET results. The authors recommend approach option A. Abbreviations: PET, positron emission tomography; HIPPA, Health Insurance Portability and Accountability Act of 1996.
When test results are disclosed, practitioners should draw on best practices in health education and risk communication to clearly convey information and provide appropriate resources to assist coping and promote continued care [55]. Often referral to AA local offices can provide additional information and support in addition to an existing national 24/7 helpline. Results from a recent cross-sectional study in patients who had a diagnosis of mild dementia due to AD underscore the importance of truly comprehending the diagnosis from a patient perspective. This understanding may facilitate the patient's ability to deal with issues of loss and to make positive life changes via available coping strategies [56].
There has been considerable research on patient and family reactions to genotyping of APOE, where the ε4 allele is a known genetic risk factor for AD. The Risk Evaluation and Education for Alzheimer's Disease (REVEAL) study of the psychological and behavioral impact of APOE testing of asymptomatic first-degree relatives of AD patients may provide a model [57], although there are also important differences between these tests [58]. In a symptomatic patient, risk for AD onset is not a concern. Instead, by providing tangible, visual evidence about pathologic status, a positive or negative amyloid-PET scan is difficult to refute. Inability to deny the presence of significant pathology and sustain alternative explanations such as “just normal aging” in the face of such evidence could be devastating to some patients and family members and justifies supportive care in delivering results. In this regard, amyloid-PET has more in common with diagnostic genetic testing for Huntington's disease or spinocerebellar atrophy.
5.4. Considerations for society
The earlier the cause of dementia is determined, the more options will be available to the patient for making life choices. However, the results of amyloid-PET scans could also have adverse social consequences. How will society handle the disclosure of amyloid-β neuroimaging results? Will a positive amyloid-PET scan result be considered a preexisting condition such that medical insurance benefits are subsequently denied? How will scan results affect a patient's ability to obtain long-term care or disability insurance, maintain employability, maintain driving privileges, or retain legal competency? These questions illustrate the potential risk that early diagnosis can pose to patients if societal safeguards are not put in place. Appropriate rules or laws need to be created protecting patients and families who receive amyloid-PET scans from discrimination or abuse. Measures enacted to provide legal protections for patients obtaining genetic testing are a useful model that could be applied for this purpose.
The use of limited health care resources must also be considered. As new technology is often expensive, access could be limited in a cost-constrained environment, at a time when scan results could be particularly beneficial. Conversely, inappropriate expenditures on scanning could reduce the resources available for other health care needs, including important patient and family education and support that are often given a low priority in our health care system. Could differences in medical insurance coverage and reimbursement by payers create regional or financially based disparities in which only those who can afford to pay for the scan out of their pocket, or those fortunate enough to have more comprehensive coverage, are able to benefit from the scan?
These issues are not unique to amyloid-PET imaging but are related to the whole process and consequence of diagnosing a dementing disease. Solutions to these issues will require an evolution in thinking and action by the government, payers, and health care providers.
6. Recommendations from the bioethics advisory board
As a novel technology, amyloid-PET will evoke new practical and bioethical challenges as its clinical use expands. Societal and personal expectations will be slow to adjust to our better understanding of AD, necessitating education and leadership from the medical community. We propose the following recommendations:
-
1.
Physician education: Physicians caring for patients with cognitive complaints need to become familiar with the SNMMI/AA AUC to ensure that amyloid-PET scans are used appropriately [5], [6]. Without proper education on how to interpret test results and counsel patients and family members, physicians would see patient expectations and hopes mismatched with the information that the scan can provide. Amyloid-PET may help physicians provide more specific and consistent advice to patients if results allow more accurate and confident diagnosis of the cognitive impairment. However, in some situations communicating the uncertainties regarding the meaning of amyloid-PET may present new challenges, particularly in early stage disease.
-
2.
Patient education: Clinicians have an ethical duty to provide education and support for patients and their families as part of their duty to care. Table 1 presents a proposed pretest/posttest model for patient education and results disclosure. Patients, families, and caregivers need to be counseled before receiving amyloid-PET about the implications of a positive or negative result, as well as possible impact on psychosocial issues, including implications for family members. Discussion should include possible actions (e.g., obtaining long-term care insurance) to be taken before undergoing an extensive diagnostic workup. At the postscan disclosure visit, physicians should ensure patients and caregivers have a good understanding of the test results, the implications on receiving a diagnosis for their condition, and their future treatment options.
-
3.
Comprehensive clinical evaluation: Amyloid-PET should be considered only as an adjunctive diagnostic test within a comprehensive clinical evaluation of patients presenting with objectively documented cognitive decline, consistent with the AUC. This should include a full medical history; interview with a knowledgeable informant; review of possible medication adverse effects; medical, psychiatric, and neurologic examination; assessment of cognition and function; laboratory assessments; and structural brain imaging where indicated.
-
4.
Dementia specialist training and experience: Dementia specialist physicians who order amyloid-PET and integrate imaging results with other relevant clinical evidence should have appropriate training and experience in evaluating cognitive complaints. Compassion and support are needed while performing a dignified and respectful diagnosis and including the patient in discussions and management decisions.
-
5.
Imaging specialist training and experience: Imaging specialist physicians who oversee the technical performance and interpretation of amyloid-PET should have appropriate training and experience to ensure the accurate image acquisition, data processing, and scan interpretation to minimize the potential for errors.
Table 1.
Recommended pretest/posttest model for patient education and disclosure of results
| Prescan | Postscan |
|---|---|
|
|
7. Conclusion
The availability of amyloid-PET for appropriate clinical use represents a major advance in the evaluation of patients with cognitive impairment when AD is a possible cause. We recommend amyloid-PET be used by experienced imaging and treating physicians in appropriately selected patients and only in the context of a comprehensive clinical evaluation with adequate explanations before and after the scan.
As with any new technology, additional efforts are needed to continue to define the diagnostic performance, clinical value, cost effectiveness, and ethical implications of the procedure in clinical practice. Toward this end, a recent case-control study has provided initial evidence that amyloid-PET results led to revision of clinical diagnoses and prevented the initiation of incorrect or suboptimal treatment for patients in an urban hospital setting [59]. Additional studies are needed to determine the impact amyloid-PET results may have on patients and family members. From such data, we will be better able to understand and minimize potential harms to patients, while optimizing the potential benefits of amyloid-PET.
Research in Context.
-
1.
Systematic review: Eli Lilly and Company sponsored a multidisciplinary Bioethics Advisory Board to discuss practical and bioethical issues that might arise from the widespread clinical use of amyloid-PET neuroimaging as an adjunctive diagnostic tool to clinically evaluate patients with cognitive impairment. These practical and bioethical issues are reported here.
-
2.
Interpretation: Our findings were not meant to add to evidence-based guidelines for clinical use of amyloid-PET which are already being developed by the joint efforts of the SNMMI and AA. Instead, we discussed whether clinical use might have unexpected implications within and beyond interactions between doctors and patients, as well as their families.
-
3.
Future directions: The practical and bioethical principles proposed in this manuscript provide guidance for clinical use, recognizing that these considerations may need to be refined in the future as we learn more about the disease and its prognosis and develop more efficacious treatment options.
Acknowledgments
The authors thank Dr. Helen Levretsky and Dr. Laura Dunn for their participation and input at the Bioethics Advisory Board meeting, Sharron Stewart for assistance in arranging and coordinating the meeting, Laura Ramsey (Eli Lilly and Company), and Shannon Gardell (inVentiv Health Clinical) for assistance with the article.
N.L.F. is funded by NIH grants AG24904 and AG044147.
Footnotes
Conflicts of interest: All advisors were compensated for their attendance and participation in the Florbetapir Bioethics Advisory Board meeting. However, no compensation was provided to advisors for preparation of this article. M.M.W., A.M.H., L.E.V.C., H.M.H., C.A.H., and L.B.T. are employees and stockholders of Eli Lilly and Company (Indianapolis, IN, USA). P.T.T. was an employee of Eli Lilly and Company at the time of this work. M.J.P. is an employee of Avid Radiopharmaceuticals, a wholly owned subsidiary of Eli Lilly and Company. A.S.F. has served as a consultant for Eli Lilly and Company, Avid Radiopharmaceutical, and Siemens diagnostics; functioned as a site investigator on Lilly, Avid, Astra Zeneca, Navidea, and GE-sponsored trials; and received investigator-initiated research funding from Avid Radiopharmaceuticals. At the time of the Bioethics Advisory Board meeting, A.S.F. served as an independent advisor and was not affiliated with Eli Lilly. He became an employee of Lilly on April 7th, 2014. N.L.F. has served as a consultant for GE Healthcare, Piramal, and Bristol-Myers Squibb; served on an ethics advisory board for Lilly USA; received travel expenses and/or honoraria for lectures or educational activities not funded by industry; received research support from Avid Radiopharmaceuticals, GE Healthcare, the Center for Health Improvement, Janssen Alzheimer Immunotherapy, Baxter Bioscience, Lilly, the Alzheimer's Disease Cooperative Study, and the Veteran's Administration; and is CEO and holds >5% ownership of ProActive Memory Services, Inc., a University start-up company that currently receives NIH STTR funds. M.M.Williams has served as a site investigator in trials sponsored by Eli Lilly and Company and Bristol Myers Squibb, and as a consultant for Lilly USA, LLC, and Centene. G.D.R. received speaking honoraria from GE Healthcare, served as a consultant for Eli Lilly on the Bioethics Advisory Board, and receives research support from Avid Radiopharmaceuticals. K.Q., J.L.L., M.W., J.S.R., and G.H. have nothing additional to disclose.
References
- 1.Vandenberghe R., Van Laere K., Ivanoiu A., Salmon E., Bastin C., Triau E. 18F-flutemetamol amyloid imaging in Alzheimer disease and mild cognitive impairment: A phase 2 trial. Ann Neurol. 2010;68:319–329. doi: 10.1002/ana.22068. [DOI] [PubMed] [Google Scholar]
- 2.Clark C.M., Schneider J.A., Bedell B.J., Beach T.G., Bilker W.B., Mintun M.A. Use of florbetapir-PET for imaging beta-amyloid pathology. JAMA. 2011;305:275–283. doi: 10.1001/jama.2010.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barthel H., Gertz H.J., Dresel S., Peters O., Bartenstein P., Buerger K. Cerebral amyloid-β PET with florbetaben (18F) in patients with Alzheimer's disease and healthy controls: A multicentre phase 2 diagnostic study. Lancet Neurol. 2011;10:424–435. doi: 10.1016/S1474-4422(11)70077-1. [DOI] [PubMed] [Google Scholar]
- 4.Klunk W.E. Amyloid imaging as a biomarker for cerebral beta-amyloidosis and risk prediction for Alzheimer dementia. Neurobiol Aging. 2011;32(Suppl 1):S20–S36. doi: 10.1016/j.neurobiolaging.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson K.A., Minoshima S., Bohnen N.I., Donohoe K.J., Foster N.L., Herscovitch P. Appropriate use criteria for amyloid PET: A report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer's Association. Alzheimers Dement. 2013;54:476–490. doi: 10.1016/j.jalz.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson K.A., Minoshima S., Bohnen N.I., Donohoe K.J., Foster N.L., Herscovitch P. Update on appropriate use criteria for amyloid PET imaging: Dementia experts, mild cognitive impairment, and education. Amyloid Imaging Task Force of the Alzheimer's Association and Society of Nuclear Medicine and Molecular Imaging. Alzheimers Dement. 2013;9:e106–e109. doi: 10.1016/j.jalz.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Waldorff F.B., Buss D.V., Eckermann A., Rasmussen M.L., Keiding N., Rishøj S. Efficacy of psychosocial intervention in patients with mild Alzheimer's disease: The multicentre, rater blinded, randomised Danish Alzheimer Intervention Study (DAISY) BMJ. 2012;345:e4693. doi: 10.1136/bmj.e4693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thies W., Bleiler L., Alzheimer's Association 2013 Alzheimer's disease facts and figures. Alzheimers Dement. 2013;9:208–245. doi: 10.1016/j.jalz.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization . 2014. Classifications: International classification of diseases, 10th revision. Available at: http://www.who.int/classifications/icd/en/index.html. Accessed June 4, 2014. [Google Scholar]
- 10.American Psychiatric Association . American Psychiatric Association; Washington, DC: 2000. Diagnostic and statistical manual of mental disorders, Fifth Edition, Text Revision. [Google Scholar]
- 11.McKhann G.M., Knopman D.S., Chertkow H., Hyman B.T., Jack C.R., Jr., Kawas C.H. The diagnosis of dementia due to Alzheimer's disease: Recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:263–269. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beach T.G., Monsell S.E., Phillips L.E., Kukull W. Accuracy of the clinical diagnosis of Alzheimer disease at National Institute on Aging Alzheimer Disease Centers, 2005-2010. J Neuropathol Exp Neurol. 2012;71:266–273. doi: 10.1097/NEN.0b013e31824b211b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beach T.G., Sue L.I., Walker D.G., Sabbagh M.N., Serrano G., Dugger B.N. Striatal amyloid plaque density predicts Braak neurofibrillary stage and clinicopathological Alzheimer's disease: Implications for amyloid imaging. J Alzheimers Dis. 2012;28:869–876. doi: 10.3233/JAD-2011-111340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haneuse S., Larson E., Walker R., Montine T., Sonnen J. Neuropathology-based risk scoring for dementia diagnosis in the elderly. J Alzheimers Dis. 2009;17:875–885. doi: 10.3233/JAD-2009-1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knopman D.S., DeKosky S.T., Cummings J.L., Chui H., Corey-Bloom J., Relkin N. Practice parameter: Diagnosis of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:1143–1153. doi: 10.1212/wnl.56.9.1143. [DOI] [PubMed] [Google Scholar]
- 16.Gay B.E., Taylor K.I., Hohl U., Tolnay M., Staehelin H.B. The validity of clinical diagnoses of dementia in a group of consecutively autopsied memory clinic patients. J Nutr Health Aging. 2008;12:132–137. doi: 10.1007/BF02982566. [DOI] [PubMed] [Google Scholar]
- 17.Newell K.L., Hyman B.T., Growdon J.H., Hedley-Whyte E.T. Application of the National Institute on Aging (NIA)-Reagan Institute criteria for the neuropathological diagnosis of Alzheimer disease. J Neuropathol Exp Neurol. 1999;58:1147–1155. doi: 10.1097/00005072-199911000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Albert M.S., DeKosky S.T., Dickson D., Dubois B., Feldman H.H., Fox N.C. The diagnosis of mild cognitive impairment due to Alzheimer's disease: Recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:270–279. doi: 10.1016/j.jalz.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matthews B.R., Miller B.L. The behavioral neurology of dementia. Cambridge University Press; New York: 2009. Alzheimer's disease; pp. 56–73. [Google Scholar]
- 20.Jack C.R., Albert M.S., Knopman D.S., McKhann G.M., Sperling R.A., Carrillo M.C. Introduction to the recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:257–262. doi: 10.1016/j.jalz.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frisoni G.B., Bocchetta M., Chételat G., Rabinovici G.D., de Leon M.J., Kaye J. Imaging markers for Alzheimer disease: Which vs how. Neurology. 2013;81:487–500. doi: 10.1212/WNL.0b013e31829d86e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dubois B., Feldman H.H., Jacova C., Hampel H., Molinuevo J.L., Blennow K. Advancing research diagnostic criteria for Alzheimer's disease: The IWG-2 criteria. Lancet Neurol. 2014;13:614–629. doi: 10.1016/S1474-4422(14)70090-0. [DOI] [PubMed] [Google Scholar]
- 23.Hogervorst E., Barnetson L., Jobst K.A., Nagy Z., Combrinck M., Smith A.D. Diagnosing dementia: Interrater reliability assessment and accuracy of the NINCDS/ADRDA criteria versus CERAD histopathological criteria for Alzheimer's disease. Dement Geriatr Cogn Disord. 2000;11:107–113. doi: 10.1159/000017222. [DOI] [PubMed] [Google Scholar]
- 24.Johnson H., Bouman W.P., Pinner G. On telling the truth in Alzheimer's disease: A pilot study of current practice and attitudes. Int Psychogeriatr. 2000;12:221–229. doi: 10.1017/s1041610200006347. [DOI] [PubMed] [Google Scholar]
- 25.Carpenter B.D., Xiong C., Porensky E.K., Lee M.M., Brown P.J., Coats M. Reaction to a dementia diagnosis in individuals with Alzheimer's disease and mild cognitive impairment. J Am Geriatr Soc. 2008;56:405–412. doi: 10.1111/j.1532-5415.2007.01600.x. [DOI] [PubMed] [Google Scholar]
- 26.Lecouturier J., Bamford C., Hughes J.C., Francis J.J., Foy R., Johnston M. Appropriate disclosure of a diagnosis of dementia: Identifying the key behaviours of “best practice”. BMC Health Serv Res. 2008;8:95. doi: 10.1186/1472-6963-8-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bradford A., Kunik M.E., Schulz P., Williams S.P., Singh H. Missed and delayed diagnosis of dementia in primary care prevalence and contributing factors. Alzheimer Dis Assoc Disord. 2009;23:306–314. doi: 10.1097/WAD.0b013e3181a6bebc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grossberg G.T., Christensen D.D., Griffith P.A., Kerwin D.R., Hunt G., Hall E.J. The art of sharing the diagnosis and management of Alzheimer's disease with patients and caregivers: Recommendations of an expert consensus panel. Prim Care Companion J Clin Psychiatry. 2010;12 doi: 10.4088/PCC.09cs00833oli. PCC.09cs00833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schneider J.A., Bennett D.A. Where vascular meets neurodegenerative disease. Stroke. 2010;41(10 Suppl):S144–S146. doi: 10.1161/STROKEAHA.110.598326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Villemagne V.L., Burnham S., Bourgeat P., Brown B., Ellis K.A., Salvado O., Australian Imaging Biomarkers and Lifestyle (AIBL) Research Group Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer's disease: A prospective cohort study. Lancet Neurol. 2013;12:357–367. doi: 10.1016/S1474-4422(13)70044-9. [DOI] [PubMed] [Google Scholar]
- 31.Mintun M.A., Larossa G.N., Sheline Y.I., Dence C.S., Lee S.Y., Mach R.H. [11C]PIB in a nondemented population: Potential antecedent marker of Alzheimer disease. Neurology. 2006;67:446–452. doi: 10.1212/01.wnl.0000228230.26044.a4. [DOI] [PubMed] [Google Scholar]
- 32.Mormino E.C., Kluth J.T., Madison C.M., Rabinovici G.D., Baker S.L., Miller B.L. Episodic memory loss is related to hippocampal-mediated beta-amyloid deposition in elderly subjects. Brain. 2009;132(Pt 5):1310–1323. doi: 10.1093/brain/awn320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pike K.E., Savage G., Villemagne V.L., Ng S., Moss S.A., Maruff P. Beta-amyloid imaging and memory in non-demented individuals: Evidence for preclinical Alzheimer's disease. Brain. 2007;130(Pt11):2837–2844. doi: 10.1093/brain/awm238. [DOI] [PubMed] [Google Scholar]
- 34.Villemagne V.L., Pike K.E., Chetelat G., Ellis K.A., Mulligan R.S., Bourgeat P. Longitudinal assessment of beta-amyloid and cognition in aging and Alzheimer disease. Ann Neurol. 2011;69:181–192. doi: 10.1002/ana.22248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Highlights of prescribing information: Amyvid (florbetapir F 18 injection) for intravenous use. 2014. Available at: http://pi.lilly.com/us/amyvid-uspi.pdf. Accessed June 4, 2014. [Google Scholar]
- 36.Vizamyl (flutemetamol F 18 injection): Highlights of prescribing information. 2013. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/203137s002lbl.pdf. Accessed June 4, 2014. [Google Scholar]
- 37.Highlights of prescribing information. Neuraceq (florbetaben F 18 injection), for intravenous use. 2013. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/204677s000lbl.pdf. Accessed June 4, 2014. [Google Scholar]
- 38.Klein E.P., Kaye J. Dementia specialists and early adoption. J Alzheimers Dis. 2013;33:445–450. doi: 10.3233/JAD-2012-121216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fagan A.M. CSF biomarkers of Alzheimer's disease: Impact on disease concept, diagnosis, and clinical trial design. Adv Geriatr. 2014;2014:14. Article ID 302712. [Google Scholar]
- 40.Hinton L., Franz C., Friend J. Pathways to dementia diagnosis: Evidence for cross-ethnic differences. Alzheimer Dis Assoc Disord. 2004;18:134–144. doi: 10.1097/01.wad.0000127444.23312.ff. [DOI] [PubMed] [Google Scholar]
- 41.Doraiswamy P.M., Sperling R.A., Johnson K., Reiman E.M., Wong T.Z., Sabbagh M.N., AV45-A11 Study Group Florbetapir F 18 amyloid PET and 36-month cognitive decline: A prospective multicenter study. Mol Psychiatry. 2014;19:1044–1051. doi: 10.1038/mp.2014.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Landau S.M., Mintun M.A., Joshi A.D., Koeppe R.A., Petersen R.C., Aisen P.S., Alzheimer's Disease Neuroimaging Initiative Amyloid deposition, hypometabolism, and longitudinal cognitive decline. Ann Neurol. 2012;72:578–586. doi: 10.1002/ana.23650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kawas C.H., Greenia D.E., Bullain S.S., Clark C.M., Pontecorvo M.J., Joshi A.D. Amyloid imaging and cognitive decline in nondemented oldest-old: The 90+ study. Alzheimers Dement. 2013;9:199–203. doi: 10.1016/j.jalz.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grundman M., Pontecorvo M., Salloway S.P., Doraiswamy P.M., Fleisher A.S., Sadowsky C.H., AV45-A17 Study Group Potential impact of amyloid imaging on diagnosis and intended management in patients with progressive cognitive decline. Alzheimer Dis Assoc Disord. 2013;27:4–15. doi: 10.1097/WAD.0b013e318279d02a. [DOI] [PubMed] [Google Scholar]
- 45.Ossenkoeple R., Prins N.D., Pijnenburg Y.A., Lemstra A.W., van der Flier W.M., Adriaanse S.F. Impact of molecular imaging on the diagnostic process in a memory clinic. Alzheimers Dement. 2013;9:414–421. doi: 10.1016/j.jalz.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 46.Connell C.M., Roberts J.S., McLaughlin S.J., Carpenter B.D. Black and white adult family members' attitudes toward a dementia diagnosis. J Am Geriatr Soc. 2009;57:1562–1568. doi: 10.1111/j.1532-5415.2009.02395.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Witte M.M., Barnes J., Lingler J., Agronin M., Hochstetler H., Healey K. Testing the use of standardized scripts for disclosing “hypothetical/mock” amyloid PET scan results to nondemented cognitively-impaired patients and their care partners. Alzheimers Dement. 2013;9(Suppl):P131–P132. [Google Scholar]
- 48.Karnieli-Miller O., Werner P., Aharon-Peretz J., Sinoff G., Eidelman S. Expectations, experiences, and tensions in the memory clinic: The process of diagnosis disclosure of dementia within a triad. Int Psychogeriatr. 2012;24:1756–1770. doi: 10.1017/S1041610212000841. [DOI] [PubMed] [Google Scholar]
- 49.Nuffield Council on Bioethics . 2009. Dementia: Ethical issues. Available at: http://nuffieldbioethics.org/project/dementia/. Accessed June 4, 2014. [Google Scholar]
- 50.Fischer M.A., Stedman M.R., Lii J., Vogeli C., Shrank W.H., Brookhart M.A. Primary medication non-adherence: Analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010;25:284–290. doi: 10.1007/s11606-010-1253-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nowrangi M.A., Rao V., Lyketsos C.G. Epidemiology, assessment, and treatment of dementia. Psychiatr Clin North Am. 2011;34:275–294. doi: 10.1016/j.psc.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 52.Leuzy A., Gauthier S. Ethical issues in Alzheimer's disease: An overview. Expert Rev Neurother. 2012;12:557–567. doi: 10.1586/ern.12.38. [DOI] [PubMed] [Google Scholar]
- 53.Storandt M., Morris J.C. Ascertainment bias in the clinical diagnosis of Alzheimer disease. Arch Neurol. 2010;67:1364–1369. doi: 10.1001/archneurol.2010.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stern Y. Cognitive reserve in ageing and Alzheimer's disease. Lancet Neurol. 2012;11:1006–1012. doi: 10.1016/S1474-4422(12)70191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Trevena L.J., Zikmund-Fisher B.J., Edwards A., Gaissmaier W., Galesic M., Han P.K. Presenting quantitative information about decision outcomes: A risk communication primer for patient decision aid developers. BMC Med Inform Decis Mak. 2013;13(Suppl 2):S7. doi: 10.1186/1472-6947-13-S2-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lee S.M., Roen K., Thornton A. The psychological impact of a diagnosis of Alzheimer's disease. Dementia (London) 2014;13:289–305. doi: 10.1177/1471301213497080. [DOI] [PubMed] [Google Scholar]
- 57.Roberts J.S., Christensen K.D., Green R.C. Using Alzheimer's disease as a model for genetic risk disclosure: Implications for personal genomics. Clinical Genetics. 2011;80:407–414. doi: 10.1111/j.1399-0004.2011.01739.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Roberts J.S., Dunn L., Rabinovici G. Amyloid imaging, risk disclosure, and Alzheimer's disease: Ethical and practical issues. Neurodegener Dis Manag. 2013;3:219–229. doi: 10.2217/nmt.13.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mitsis E.M., Bender H.A., Kostakoglu L., Machac J., Martin J., Woehr J.L. A consecutive case series experience with [18F] florbetapir PET imaging in an urban dementia center: Impact on quality of life, decision making, and disposition. Mol Neurodegener. 2014;9:10. doi: 10.1186/1750-1326-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]