Abstract
Summary
We evaluated healthcare utilization associated with treating different fracture types in over 51,000 women aged ≥55 years. Over the course of 1 year, there were five times more non-hip, non-spine fractures than hip or spine fractures, resulting in twice as many days of hospitalization and rehabilitation/nursing home care for non-hip, non-spine fractures.
Purpose
To evaluate the medical healthcare utilization associated with treating several types of fractures in women aged 55 years or older from various geographic regions.
Methods
Information from the Global Longitudinal study of Osteoporosis in Women (GLOW) was collected via self-administered patient questionnaires at baseline and year 1 (n=51,491). Self-reported clinically recognized low-trauma fractures at year 1 were classified as incident spine, hip, wrist/hand, arm/shoulder, pelvis, rib, leg, and other fractures. Healthcare utilization data were self-reported and included whether the fracture was treated at a doctor’s office/clinic or at a hospital. Patients were also asked if they had undergone surgery or been treated at a rehabilitation center or nursing home.
Results
Over the 1-year study period, there were 195 spine, 134 hip, and 1,654 non-hip, non-spine fractures. In the GLOW cohort, clinical vertebral fractures resulted in 617 days of hospitalization and 512 days of rehabilitation/nursing home care, while hip fractures accounted for 1,306 days of hospitalization and 1,650 days of rehabilitation/nursing home care. Of particular interest is the result that non-hip, non-spine fractures resulted in 3,805 days in hospital and 5,186 days of rehabilitation/nursing home care.
Conclusions
While hip and vertebral fractures are well recognized for their associated increase in health resource utilization, non-hip, non-spine fractures, by virtue of their 5-fold greater number, require significantly more healthcare resources.
Keywords: Osteoporosis, Healthcare utilization, Geographic region, Healthcare services, Fracture
Introduction
For patients with osteoporosis, traditional fracture sites include hip, spine, and forearm, but low-energy trauma fractures may occur at virtually any site, including non-hip, non-spine fractures of the proximal humerus, ribs, tibia, pelvis, knee, and ankle [1–6]. Approximately 30% of postmenopausal women in the USA and Europe are estimated to have osteoporosis, of whom 40% will sustain one or more fragility fractures in their remaining lifetime [7]. In the European Union, the number of fractures is estimated at 3.79 million [8]. Over 200 million people worldwide are reported to have osteoporosis [9]. Of these fractures, non-hip, non-spine fractures have not been recognized for their impact on health services.
In addition to significant morbidity and mortality [10–12], fractures are associated with substantial healthcare resource utilization and cost [13]. The worldwide economic burden of osteoporosis is expected to increase in the future, as life expectancy and the elderly population, who are at high risk of fracture, increase [14–16]. The elevated burden may place a strain on accessing healthcare resources; thus, further research is needed into the healthcare utilization associated with various fracture types.
Using the Global Longitudinal study of Osteoporosis in Women (GLOW), we evaluated the direct medical healthcare utilization associated with treating several fracture types for women aged 55 years or older in 10 countries. The results are intended to provide a frame of reference for evaluating the cost effectiveness of public health measures to prevent fractures, and to guide programs that assess healthcare resources. We hypothesize that non-hip, non-spine fractures will result in a high use of healthcare resources.
Methods
Details regarding the study design, participant selection and methods have been previously reported [10] and are outlined here. Briefly, GLOW is an ongoing, prospective, multinational, physicians’ practice-based study that includes a total of 17 physician practice sites from 10 countries (Australia, Belgium, Canada, France, Germany, Italy, Netherlands, Spain, UK, and USA) in Australia, Europe, and North America. These sites were selected based on the ability of the local investigators to consistently administer the survey; on the availability of a wide spectrum of osteoporosis treatment options and bone densitometry; and the existence of prior studies in these regions, which would provide data for comparison with the GLOW sample. The study was designed to advance the understanding of international patterns of susceptibility, recognition, management, and patient outcomes in women aged 55 years or older at risk of osteoporosis. In general, some specific aims of the GLOW study were to describe the distribution of risk factors for osteoporosis and fractures, identify the differences in physician patterns of diagnosis and management of osteoporosis, characterize factors that influence patient persistence with treatment, and evaluate the cost effectiveness of care of interventions for the prevention and management of osteoporosis. Each study site obtained ethics committee approval to conduct the study in the specific location.
Physician and patient selection
Primary care practices typical of each region were recruited through primary care networks organized for administrative, research, or educational purposes, or by identifying all physicians in a geographic area. Physician networks included regional health system-owned or managed practices, health maintenance organizations, independent practice associations, and other primary care practice networks.
Primary care physicians were defined as those who spent most of their time providing primary healthcare to patients. Depending on the country in which the study site was located, this included internists, family practitioners, and general practitioners who provided primary care. If the physician network or study area included more eligible physicians than were required to recruit a sufficient number of patients, a random sample of those physicians within the network or study was invited. Each practice provided a list of the names and addresses of women aged 55 years or older who had visited their physician in the past 24 months. Based on these lists, participants were recruited. Sampling was stratified by age to ensure that two-thirds of participants were women aged 65 years or older. Approximately 3,000 patients were sought at each site. Patients were excluded if they were unable to complete the study survey due to cognitive impairment, language barriers, institutionalization, or illness severity.
Questionnaire design and administration
Information was collected at cohort entry via a self-administered patient questionnaire that covered the following domains: patient characteristics and risk factors, perception about fracture risk and osteoporosis, medication use (currently taking or ever taken), medical diagnoses, healthcare use and access, physical activity, and physical and emotional health status. Where possible, items from published validated instruments were used, including the National Health and Nutrition Examination Survey, EuroQol EQ-5D, and SF-36 [17–19].
An annual follow-up questionnaire was also sent to all study participants. The follow-up survey included items similar to the baseline questionnaire plus questions regarding persistence with medication, reasons for non-adherence, and new fracture status. Completed questionnaires were sent to the central coordinating center, where they were scanned electronically, and data fields were audited visually by a person trained to process the forms.
Fracture types
Clinically recognized, incident, low-trauma, vertebral and non-vertebral fractures were based on self-reports documented in the year 1 follow-up questionnaire. For the purposes of the current study, all participants were subdivided into eight fracture groups according to their incident fracture status: those with incident hip, spine (excluding neck fractures), wrist/hand, arm/shoulder, pelvis, rib, leg, and other fractures. Other fracture sites included ankle, foot, knee, clavicle, elbow, coccyx, sternum, and neck. Women who fractured more than one bone were included.
Healthcare utilization
Data on healthcare utilization were gathered from the year 1 follow-up questionnaire. A number of healthcare services were examined, including whether the patient had their fracture treated at a doctor’s office/clinic or at a hospital. Patients were also asked if they had undergone surgery to treat their fracture, and whether they spent any time in a rehabilitation center/unit or nursing home. The length of stay for those who utilized hospital, rehabilitation center, or nursing home care was collected.
Other factors
Individual characteristics were collected from self-reports and included the age of the patient, prior fracture status, number of co-morbid conditions, osteoporosis medications, general health, height, weight, education level, insurance coverage, and region (North America, which included United States of America and Canada; South Europe, which included France, Italy, and Spain; and North Europe, which included Belgium, Germany, Netherlands, and UK). Comorbid conditions included asthma, emphysema, joint disease/osteoarthritis, stroke, colitis, celiac disease, Parkinson’s disease, multiple sclerosis, cancer, type I diabetes, rheumatoid arthritis, hypertension, and heart disease. Osteoporosis medications included bisphosphonates, raloxifene, teriparatide, tibolene, calcitonin, and strontium ranelate.
Statistics
Descriptive statistics were calculated for all variables and included means and standard deviations (SDs) for continuous variables and counts and percentages for categorical variables. Wilcoxon rank sum tests were performed to compare differences in length of stay at the hospital, rehabilitation center, or nursing home between spine, hip, and non-hip, non-spine fractures. Multivariable linear regression analysis was conducted to assess the association among various participant characteristics and length of stay at the hospital, rehabilitation center, or nursing home. The participant characteristics that were examined include co-morbidities, prior fracture, osteoporosis medications and age. P-values from statistically significant results from F-tests were reported. ANOVA F-tests were performed to evaluate the association between regions and length of stay at the hospital, rehabilitation center, or nursing home. Australia was not included in the regional comparisons due to difficulty in placing this country in an appropriate region. All analyses were performed with SAS statistical software version 9.2 for Windows (SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics of those patients with fracture(s) by year 1 were categorized according to fracture type (Table 1). Of the GLOW population of 51,491 participants, a total of 1,898 developed a new fracture over the 1-year study period. Among the 1,898 patients with fracture, their mean (SD) age was 71 (9) years, 44% (n=822) had a prior baseline fracture, and 83% had at least one other disease condition. General health reported as excellent/very good ranged from 21% for those with spine fractures to 35% for those with wrist/hand fractures (Table 1). Most new fractures occurred in individuals between 65 and 84 years of age and the percent of patients using health care services varied with age and place of service (Tables 2–3).
Table 1.
Baseline characteristics of the 1,898 women with fracture(s) by year 1a
| Baseline characteristics | New fracture at specific location | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Spineb (n=195) | Hip (n=134) | Non-spine, non-hip (n =1,654) | Wrist/hand (n=419) | Arm/shoulder (n=197) | Pelvis (n=89) | Rib (n=252) | Leg (n=207) | Otherc (n=658) | |
| Patient demographics, mean (SD) | |||||||||
| Age (years) | 73 (9) | 76 (9) | 70 (9) | 70 (9) | 72 (9) | 75 (9) | 71 (10) | 71 (10) | 69 (9) |
| BMI (kg/m2) | 26 (7) | 25 (5) | 27 (6) | 27 (6) | 27 (5) | 25 (5) | 27 (6) | 28 (7) | 27 (6) |
| Patient history, n (%) | |||||||||
| Prior fractures | 107 (56) | 68 (52) | 699 (43) | 171 (42) | 82 (43) | 51 (61) | 140 (57) | 108 (53) | 248 (39) |
| ≥1 comorbid condition(s) | 137 (87) | 93 (87) | 1,157 (82) | 297 (81) | 141 (83) | 64 (93) | 171 (86) | 142 (78) | 461 (83) |
| General health excellent/very good | 41 (21) | 38 (29) | 527 (32) | 144 (35) | 54 (28) | 19 (22) | 65 (26) | 57 (28) | 220 (34) |
| Insurance coverage | 146 (82) | 85 (73) | 1,190 (80) | 281 (76) | 129 (76) | 67 (85) | 182 (78) | 149 (81) | 499 (82) |
| Highest education level | 24 (13) | 14 (11) | 266 (17) | 65 (16) | 23 (12) | 8 (9) | 39 (16) | 33 (17) | 117 (18) |
SD standard deviation
Some women did not have complete data on all baseline characteristics
Excluding neck fractures
Other fractures included ankle, foot, knee, clavicle, elbow, coccyx, sternum, neck
Table 2.
Fracture type by age group
| Baseline characteristics | New fracture at specific location | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Spineb (n=195) | Hip (n=134) | Non-spine, non-hip (n =1,654) | Wrist/hand (n=419) | Arm/shoulder (n=197) | Pelvis (n=89) | Rib (n=252) | Leg (n=207) | Otherc (n=658) | |
| Age group: % | |||||||||
| 55–64 years | 19.5 | 13.4 | 33.1 | 32.0 | 26.9 | 13.5 | 31.0 | 31.4 | 38.3 |
| 65–74 years | 31.8 | 26.1 | 34.0 | 34.6 | 26.4 | 27.0 | 30.6 | 31.4 | 35.7 |
| 75–84 years | 38.0 | 41.0 | 25.9 | 27.7 | 37.6 | 42.7 | 30.6 | 26.6 | 20.4 |
| 85+ years | 10.8 | 19.4 | 7.0 | 5.7 | 9.1 | 16.9 | 7.9 | 10.6 | 5.6 |
Table 3.
Health care service used by age group
| Age group: % | Office/clinic (n=1266) |
Hospital (n=1206) |
Rehab (n=291) |
Nursing home (n=66) |
|---|---|---|---|---|
| 55–64 years | 31.2 | 29.6 | 18.2 | 10.5 |
| 65–74 years | 34.3 | 33.1 | 26.7 | 19.4 |
| 75–84 years | 27.3 | 28.7 | 36.6 | 47.8 |
| 85+ years | 7.2 | 8.6 | 18.5 | 22.4 |
Healthcare service use between the different fracture types was driven by the number of fractures. There were a total of 195 clinical spine fractures, 134 hip fractures, and 1,654 non-hip, non-spine fractures. A breakdown of healthcare utilization by fracture type is shown in Table 4. For those that were hospitalized, the mean hospital length of stay for hip fractures was 13 days; for non-hip, non-spine fractures, it was 10 days (Table 4). The total number of hospital days was greatest for non-hip, non-spine fractures at 3805 days, 2.9 times greater than that seen for hip fractures (1,306 days) (Fig. 1). Total rehabilitation days were also greatest for non-spine, non-hip fractures at 4,083 days, compared to 1,252 for hip fractures and 392 for clinical spine fractures (Fig. 1). A similar pattern was also seen for total nursing home days: for non-hip, non-spine (1,103), hip (398), and clinical spine (120), respectively (Fig. 1). Results suggested that prior fractures were associated with longer hospital length of stay (p-value=0.004) compared with individuals without prior fracture. However, osteoporosis medications and other disease conditions were not found to be statistically significant with respect to length of stay at the three locations measured. Table 5 displays the descriptive statistics for length of stay by region and fracture type.
Table 4.
Length of stay by fracture type (n=1898a)
| Healthcare service used | New fracture at specific location | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Spineb (n=195) | Hip (n=134) | Non-hip, non-spine (n=1,654) | Wrist/hand (n=419) | Arm/shoulder (n=197) | Pelvis (n=89) | Rib (n=252) | Leg (n=207) | Otherc (n=658) | |
| Hospital (n) | n=56 | n=99 | n=369 | n=81 | n=62 | n=36 | n=40 | n=107 | n=111 |
| Mean (SD) days | 11 (13) | 13 (16) | 10 (15) | 7 (11) | 9 (13) | 18 (19) | 17 (22) | 15 (21) | 9 (12) |
| Median days | 6 | 8 | 5 | 3 | 4 | 10 | 6 | 7 | 4 |
| Rehab (n) | n=20 | n=58 | n=149 | n=19 | n=25 | n=23 | n=14 | n=59 | n=41 |
| Mean (SD) days | 20 (12) | 22 (20) | 27 (25) | 18 (21) | 31 (28) | 23 (13) | 32 (29) | 31 (27) | 27 (26) |
| Median days | 18.5 | 14 | 20 | 10 | 21 | 21 | 21 | 21 | 18 |
| Nursing home (n) | n=7 | n=14 | n=38 | n=6 | n=8 | n=10 | n=4 | n=12 | n=9 |
| Mean (SD) days | 17 (15) | 28 (25) | 29 (27) | 35 (37) | 13 (8) | 34 (29) | 65 (39) | 41 (35) | 37 (26) |
| Median days | 14 | 20 | 20 | 18 | 15.5 | 20 | 75 | 25.5 | 30 |
Some women did not have complete data on all healthcare utilization characteristics
Excluding neck fractures
Other fractures included ankle, foot, knee, clavicle, elbow, coccyx, sternum, neck
Figure 1.
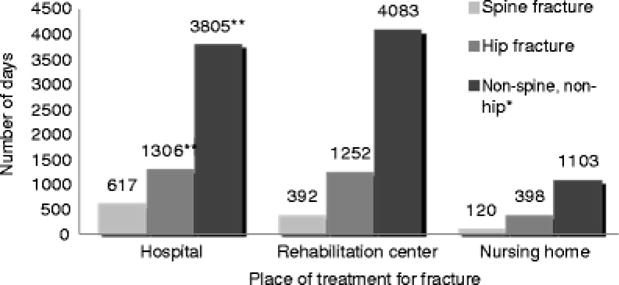
Numbers of days in a hospital, rehabilitation center, or nursing home for patients with a fracture of the spine, hip, or non-spine, non-hip. Single asterisk (*): non-spine, non-hip fractures included wrist/hand, arm/shoulder, pelvis, rib, leg, and other fractures (other fractures sites included ankle, foot, knee, clavicle, elbow, coccyx, sternum, and neck). **P value<0.001, significant difference in LOS for hip versus non-spine, non-hip fractures
Table 5.
Length of stay by region and fracture type
| n, mean (SD), median | LOS Hospital | LOS Rehab | LOS Nursing home |
|---|---|---|---|
| Spine | |||
|
| |||
| North America | n=29, 7 (9)*, 3 | n=10, 15 (7), 14.5 | n=4, 20 (18), 17.5 |
| North Europe | n=18, 13 (11), 9.5 | n=5, 16 (9), 14 | n=2, 7 (8), 6.5 |
| South Europe | n=7, 20 (23)*, 7 | n=2, 44 (23), 44 | n=1, 28 (−), 28 |
| Hip | |||
|
| |||
| North America | n=57, 10 (15), 6 | n=37, 16 (15), 14 | n=9, 27 (28), 20 |
| North Europe | n=16, 15 (9), 13 | n=5, 41 (34), 28 | n=1, 40 (.), 40 |
| South Europe | n=22, 19 (21), 10 | n=14, 28 (19), 20.5 | n=4, 29 (21), 20 |
| Non-spine, non-hip | |||
|
| |||
| North America | n=175, 9 (16), 4 | n=105, 27 (27), 17 | n=27, 35 (30), 21 |
| North Europe | n=95, 12 (10), 10 | n=12, 27 (15), 23 | n=4, 10 (3), 10 |
| South Europe | n=76, 9 (12), 4 | n=20, 33 (26), 25.5 | n=6, 17 (11), 17.5 |
Statistically significant difference between North America and South Europe (p=0.016)
Healthcare service use varied by fracture type (Table 6). Only 3.3% of hip fractures were treated at the physician’s office/clinic only, compared with 36% of rib fractures. A total of 92% of hip fractures received treatment at a hospital, while fewer than half of the patients with rib fractures visited a hospital. Overnight stays in hospital were highest for hip fracture patients (92%) and lowest for wrist/hand (30%) and other fractures (34%). Women with hip fractures had the highest surgery rates (89%), whereas those with spine, pelvis, rib, and other fractures had surgery rates of 30% or less. Other than women with hip fractures (57%), less than 50% of patients with fractures used rehabilitation centers for treatment (Table 6). Fewer than 20% of patients with fractures went to a nursing home for treatment; while women with hip and pelvis fractures were most likely (16% and 17%, respectively) to be treated in a nursing home for their fracture.
Table 6.
Utilization of healthcare services by fracture type (n=1,898a)
| Healthcare service used | New fracture at specific location | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Spineb (n=195) | Hip (n=134) | Non-hip non-spine (n=1,654) | Wrist/hand (n=419) | Arm/shoulder (n=197) | Pelvis (n=89) | Rib (n=252) | Leg (n=207) | Otherc (n=658) | |
| Office/clinic, n/n | 121/165 | 76/124 | 1,111/1,522 | 270/379 | 130/181 | 45/81 | 164/236 | 140/191 | 456/596 |
| (%) | (73) | (61) | (73) | (71) | (72) | (56) | (69) | (73) | (77) |
| Office/clinic only, n/n | 44/152 | 4/121 | 384/1,443 | 66/367 | 28/174 | 14/76 | 78/219 | 26/183 | 181/557 |
| (%) | (29) | (3.3) | (27) | (18) | (16) | (18) | (36) | (14) | (32) |
| Hospital, n/n | 101/165 | 117/127 | 1,045/1,511 | 313/389 | 149/184 | 60/78 | 104/225 | 163/193 | 371/579 |
| (%) | (61) | (92) | (69) | (80) | (81) | (77) | (46) | (84) | (64) |
| Overnight in hospital, n/n | 57/95 | 102/111 | 385/960 | 85/281 | 66/138 | 37/57 | 43/98 | 110/152 | 115/339 |
| (%) | (60) | (92) | (40) | (30) | (48) | (65) | (44) | (72) | (34) |
| Surgery, n/n | 29/99 | 103/116 | 348/998 | 114/296 | 49/141 | 16/59 | 16/98 | 105/154 | 107/355 |
| (%) | (29) | (89) | (35) | (39) | (35) | (27) | (16) | (68) | (30) |
| Rehabilitation center, n/n | 24/161 | 69/122 | 225/1,441 | 47/357 | 43/176 | 27/79 | 19/217 | 73/178 | 64/563 |
| (%) | (15) | (57) | (16) | (13) | (24) | (34) | (8.8) | (41) | (11) |
| Nursing home, n/n | 8/153 | 19/116 | 50/1,394 | 8/349 | 12/168 | 13/75 | 6/216 | 17/174 | 13/534 |
| (%) | (5.2) | (16) | (3.6) | (2.3) | (7.1) | (17) | (2.8) | (9.8) | (2.4) |
Some women did not have complete data on all healthcare utilization characteristics
Excluding neck fractures
Other fractures included ankle, foot, knee, clavicle, elbow, coccyx, sternum, neck
Discussion
In our large, international, observational study, we found that healthcare resource utilization (total hospital days, total rehabilitation days, and total nursing home days) varied among fracture types. While we are accustomed to hip fractures having a significant impact on healthcare utilization, they should be viewed in the context of the incident rates of all fractures. In the past, hip fractures were the easiest fracture type to capture accurately; and their associated healthcare costs were the easiest to quantitate. Indeed, it was often argued that their costs dwarfed the costs of other fractures. We now recognize that most fractures after the age of 50 years [20], even fractures that occur after trauma [21], are fragility fractures and should be included in fracture analyses. In the current study, 93% of fractures were at sites other than the hip and, as a consequence, women with non-hip fractures used a greater total amount of healthcare resources than those with hip fractures.
Even though patients with hip fractures had longer mean hospital stays than those with spine or all non-hip, non-spine fractures combined, and are therefore the focus of most health economic studies, they do not represent the vast majority of fragility fractures seen clinically. In our study, non-hip, non-spine fractures comprised the vast majority of fractures, and therefore, consistent with our hypothesis, had a high number of total hospital days, total rehabilitation days, and total nursing home days. Investigators have also found differences in hospital admissions depending on fracture type. Knowelden et al. [20] estimated the percentage of hospitalized patients to be in the order of 95% for hip fractures, 39% for vertebral fractures, 20% for other sites (pelvis, hand and phalanges, femoral fractures excluding the neck, distal lower extremity), 14% for humerus, and 8% for forearm. However, hospital admission rates have also been shown to fluctuate for individual fracture types. For example, data suggest that between 8% and 33% of all patients with clinical vertebral fractures are hospitalized [21–24]. In addition, while a Swiss study demonstrated a 50% hospitalization rate for individuals with forearm fractures, others have found rates that were dramatically lower [25–27].
There are many potential reasons why hospital rates fluctuate within fracture types. The apparent variation in hospital use may be due to poor coding of vertebral fractures. For instance, 52% of vertebral fractures admitted to the hospital via an emergency department have “vertebral fracture” registered as the cause of hospitalization and recorded as the principal diagnosis at hospital discharge. In the remaining cases, hospital admission was linked to other diseases, including acute exacerbation of chronic obstructive pulmonary disease, pneumonia, acute bronchitis, or congestive heart failure [28]. Furthermore, not all hospital admissions due to osteoporosis are documented as a spine fracture, but rather as back pain or kyphosis [29]. Other fracture types with obvious osteoporosis-associated features, such as peripheral fractures after minor trauma, are frequently inaccurately coded as “fracture” in the hospital statistics, rather than “fracture and osteoporosis”. In general, coding errors may be caused by uncertainty regarding the relevance of the trauma or because the physicians regard osteoporosis as an age-related process rather than a disease [30]. In addition, the severity of a fracture may help to determine hospital admission. Researchers have shown that approximately 30% of patients with spine fractures seek medical attention when the fracture occurs, but this rate increases to 80% with more severe degrees of vertebral deformity [28]. The presence or absence of care paths may have an effect on length of hospital stay, with well-established care paths associated with shortened length of stays [33]. Furthermore, complications caused by fracture, including neurological deficits resulting from vertebral fractures or algodystrophy for wrist fractures, and the patient’s quality of life prior to the fracture, may have an impact on hospitalization [30, 31]. Patients with rib fractures often do not seek any medical care as there is little that can be done other than pain relief.
In addition to the burden of hip fracture, other fracture types have a large impact on healthcare utilization, given the high incident rate of these fractures (93%) compared with hip (7%). Other investigators have found high admission rates for fractures not traditionally considered to be “osteoporotic”. Johnell et al. found that between the ages of 50 and 54 years, bed occupancy is approximately four times higher from fractures at sites other than the hip [32]. Furthermore, fractures at sites other than the traditional hip, spine, and forearm/wrist contribute to 33% of hospital discharges with a primary diagnosis of fracture and 62% of discharges with a secondary diagnosis of fracture [33].
Our study method has several strengths. First, GLOW data allowed for the assessment of healthcare utilization in a “real-world” setting, and included areas of healthcare use such as office/clinic visits and rehabilitation that are not commonly investigated. In addition, we examined many different fracture types. We utilized data from patient questionnaires and collected the information in a similar manner from the different geographic regions, which enabled accurate comparisons of patients’ healthcare use across different geographic areas and national boundaries. We therefore avoided problems with data quality due to differences in regional or national databases [32]. Finally, many osteoporotic patients, especially the elderly, are likely to have multiple conditions; we therefore included in our analyses many potential confounding factors that may influence healthcare utilization.
Our study also has several limitations, which should be considered when interpreting these results. GLOW is a practice-based rather than a population-based study and is therefore subject to biases both in the selection of physicians, and in the sampling and recruitment of patients. Nonetheless, we attempted to diminish selection bias by producing a survey method that imposed low respondent burden. Study patients were not required to participate in clinic visits, to avoid requirements that might make involvement more difficult for women who are in poor health or have no or limited access to transportation. Furthermore, high participant response rates at most sites suggest that the study burden was low. All data were collected by patient self-report and may be limited by recall bias. However, studies that have examined the validity of self-report of prescription medication use and fractures have shown reasonable accuracy [34]. Other than surgery, the procedures performed at the hospital were not examined, and data that may explain geographic regional differences were not collected. As a result, further investigation is needed to fully explain regional differences observed in the current study. In addition, our questionnaire asked if patients went to a rehabilitation center or nursing home, and these differences may not have been appreciated by the participants. Other potential limitations are that data regarding differences among insurers (within and among third party insurers and publicly funded insurance), which may influence hospitalization rates for patients, were not collected. Also, we did not report subclinical vertebral fractures because X-ray films were not a part of GLOW. Research has found that subclinical vertebral fractures are less severe than clinically recognized fractures and severity may be associated with healthcare utilization. Finally, only women were included in the study, and given that other investigators have found that healthcare utilization differs between the sexes, inferences regarding healthcare use should not be generalized to men [32].
Conclusions
Osteoporosis is a common disease and has become a major public health problem worldwide. Patients who experience fractures are in need of healthcare services. The utilization of these resources is particularly high for hip fracture patients. Nonetheless, as a result of the high incidence of other fracture types, significant healthcare services are utilized for all fractures. Given that the negative consequences of fractures are dramatic and that effective therapies that reduce future fracture risk are available, it is important to promote the early detection of patients who are at high risk of fractures so that appropriate interventions may be implemented. Furthermore, the resource utilization patterns identified in the current study may assist health planners in developing future healthcare services.
Acknowledgments
We thank the physicians and project coordinators participating in GLOW. Editorial support for the final version of this article, comprising language editing, content checking, formatting and referencing was provided by Sophie Rushton-Smith, PhD. Dr Boonen is senior clinical investigator of the Fund for Scientific Research, Flanders, Belgium (FWO-Vlaanderen) and holder of the Leuven University Chair in Metabolic Bone Diseases. Financial support for the GLOW study is provided by Warner Chilcott Company, LLC and sanofiaventis to the Center for Outcomes Research, University of Massachusetts Medical School. The sponsor had no involvement in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Contributor Information
G. Ioannidis, St. Joseph’s Hospital, McMaster University, 501-25 Charlton Ave E, Hamilton, ON L8N 1Y2, Canada
J. Flahive, Center for Outcomes Research, University of Massachusetts Medical School, Worcester, MA, USA
L. Pickard, St. Joseph’s Hospital, McMaster University, 501-25 Charlton Ave E, Hamilton, ON L8N 1Y2, Canada
A. Papaioannou, St. Joseph’s Hospital, McMaster University, 501-25 Charlton Ave E, Hamilton, ON L8N 1Y2, Canada
R. D. Chapurlat, Division of Rheumatology, INSERM UMR 1033, Université de Lyon, Hospices Civils de Lyon, Hôpital E Herriot, Lyon, France
K. G. Saag, University of Alabama-Birmingham, Birmingham, AL, USA
S. Silverman, Department of Rheumatology, Cedars-Sinai Medical Center, Los Angeles, CA, USA
F. A. Anderson, Jr, Center for Outcomes Research, University of Massachusetts Medical School, Worcester, MA, USA.
S. H. Gehlbach, Center for Outcomes Research, University of Massachusetts Medical School, Worcester, MA, USA
F. H. Hooven, Center for Outcomes Research, University of Massachusetts Medical School, Worcester, MA, USA
S. Boonen, Leuven University Center for Metabolic Bone Diseases, Division of Geriatric Medicine, Katholieke Universiteit Leuven, Leuven, Belgium
J. E. Compston, University of Cambridge School of Clinical Medicine, Addenbrooke’s Hospital, Cambridge, UK
C. Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton, UK
A. Díez-Perez, Hospital del Mar-IMIM-Autonomous University of Barcelona, Barcelona; and RETICEF, ISCIII Madrid; Spain
S. L. Greenspan, University of Pittsburgh, Pittsburgh, PA, USA
A. Z. LaCroix, Fred Hutchinson Cancer Research Center, Seattle, WA, USA
R. Lindsay, Regional Bone Center, Helen Hayes Hospital, West Haverstraw, NY, USA
J. C. Netelenbos, Department of Endocrinology, VU University Medical Center, Amsterdam, The Netherlands
J. Pfeilschifter, Department of Internal Medicine III, Alfried Krupp Krankenhaus, Essen, Germany
M. Rossini, Section of Rheumatology, Department of Medicine, University of Verona, Verona, Italy
C. Roux, Paris Descartes University, Cochin Hospital, Paris, France
P. N. Sambrook, University of Sydney-Royal North Shore Hospital, St Leonards, Sydney, NSW, Australia
E. S. Siris, Columbia University Medical Center, New York, NY, USA
N. B. Watts, Bone Health and Osteoporosis Center, University of Cincinnati, Cincinnati, OH, USA
J. D. Adachi, Email: jd.adachi@sympatico.ca, St. Joseph’s Hospital, McMaster University, 501-25 Charlton Ave E, Hamilton, ON L8N 1Y2, Canada, Tel: (905) 529-1317, Fax: (905) 521-1297.
References
- 1.Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993;94:646–650. doi: 10.1016/0002-9343(93)90218-e. [DOI] [PubMed] [Google Scholar]
- 2.Melton LJ., 3rd . Epidemiology of fractures. In: Riggs BL, Melton LJ 3rd, editors. Osteoporosis: etiology, diagnosis and management. Raven Press; New York: 1988. pp. 135–155. [Google Scholar]
- 3.Melton LJ, 3rd, Sampson JM, Morrey BF, Ilstrup DM. Epidemiologic features of pelvic fractures. Clin Orthop Relat Res. 1981:43–47. [PubMed] [Google Scholar]
- 4.Nilsson BE. Age and sex incidence of ankle fractures. Acta Orthop Scand. 1969;40:122–129. doi: 10.3109/17453676908989492. [DOI] [PubMed] [Google Scholar]
- 5.Rose SH, Melton LJ, 3rd, Morrey BF, Ilstrup DM, Riggs BL. Epidemiologic features of humeral fractures. Clin Orthop Relat Res. 1982:24–30. [PubMed] [Google Scholar]
- 6.Seeley DG, Browner WS, Nevitt MC, Genant HK, Scott JC, Cummings SR. Which fractures are associated with low appendicular bone mass in elderly women? The Study of Osteoporotic Fractures Research Group. Ann Intern Med. 1991;115:837–842. doi: 10.7326/0003-4819-115-11-837. [DOI] [PubMed] [Google Scholar]
- 7.Melton LJ, 3rd, Chrischilles EA, Cooper C, Lane AW, Riggs BL. Perspective. How many women have osteoporosis? J Bone Miner Res. 1992;7:1005–1010. doi: 10.1002/jbmr.5650070902. [DOI] [PubMed] [Google Scholar]
- 8.Kanis JA, Johnell O. Requirements for DXA for the management of osteoporosis in Europe. Osteoporos Int. 2005;16:229–238. doi: 10.1007/s00198-004-1811-2. [DOI] [PubMed] [Google Scholar]
- 9.Cooper C. Epidemiology of osteoporosis. Osteoporos Int. 1999;9(Suppl 2):S2–8. doi: 10.1007/pl00004156. [DOI] [PubMed] [Google Scholar]
- 10.Adachi JD, Adami S, Gehlbach S, Anderson FA, Jr, Boonen S, Chapurlat RD, Compston JE, Cooper C, Delmas P, Diez-Perez A, Greenspan SL, Hooven FH, LaCroix AZ, Lindsay R, Netelenbos JC, Wu O, Pfeilschifter J, Roux C, Saag KG, Sambrook PN, Silverman S, Siris ES, Nika G, Watts NB. Impact of prevalent fractures on quality of life: baseline results from the global longitudinal study of osteoporosis in women. Mayo Clin Proc. 2010;85:806–813. doi: 10.4065/mcp.2010.0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adachi JD, Ioannidis G, Pickard L, Berger C, Prior JC, Joseph L, Hanley DA, Olszynski WP, Murray TM, Anastassiades T, Hopman W, Brown JP, Kirkland S, Joyce C, Papaioannou A, Poliquin S, Tenenhouse A, Papadimitropoulos EA. The association between osteoporotic fractures and health-related quality of life as measured by the Health Utilities Index in the Canadian Multicentre Osteoporosis Study (CaMos) Osteoporos Int. 2003;14:895–904. doi: 10.1007/s00198-003-1483-3. [DOI] [PubMed] [Google Scholar]
- 12.Ioannidis G, Papaioannou A, Hopman WM, Akhtar-Danesh N, Anastassiades T, Pickard L, Kennedy CC, Prior JC, Olszynski WP, Davison KS, Goltzman D, Thabane L, Gafni A, Papadimitropoulos EA, Brown JP, Josse RG, Hanley DA, Adachi JD. Relation between fractures and mortality: results from the Canadian Multicentre Osteoporosis Study. CMAJ. 2009;181:265–271. doi: 10.1503/cmaj.081720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lindsay R. The burden of osteoporosis: cost. Am J Med. 1995;98:9S–11S. doi: 10.1016/s0002-9343(05)80038-5. [DOI] [PubMed] [Google Scholar]
- 14.Cooper C, Campion G, Melton LJ., 3rd Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 15.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407–413. doi: 10.1007/pl00004148. [DOI] [PubMed] [Google Scholar]
- 16.Melton LJ., 3rd Hip fractures: a worldwide problem today and tomorrow. Bone. 1993;14(Suppl 1):S1–8. doi: 10.1016/8756-3282(93)90341-7. [DOI] [PubMed] [Google Scholar]
- 17.Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305:160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC) National Health and Nutrition Examination Survey. NHANES 2005–2006: National Center for Health Statistics. 2008 http://www.cdc.gov/nchs/nhanes.htm Accessed: 28 March 2011.
- 20.Knowelden J, Buhr AJ, Dunbar O. Incidence of Fractures in Persons over 35 Years of Age. A Report to the M.R.C. Working Party on Fractures in the Elderly. Br J Prev Soc Med. 1964;18:130–141. doi: 10.1136/jech.18.3.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cooper C, O’Neill T, Silman A. The epidemiology of vertebral fractures. European Vertebral Osteoporosis Study Group. Bone. 1993;14(Suppl 1):S89–97. doi: 10.1016/8756-3282(93)90358-h. [DOI] [PubMed] [Google Scholar]
- 22.Dolan P, Torgerson DJ. The cost of treating osteoporotic fractures in the United Kingdom female population. Osteoporos Int. 1998;8:611–617. doi: 10.1007/s001980050107. [DOI] [PubMed] [Google Scholar]
- 23.Finnern HW, Sykes DP. The hospital cost of vertebral fractures in the EU: estimates using national datasets. Osteoporos Int. 2003;14:429–436. doi: 10.1007/s00198-003-1395-2. [DOI] [PubMed] [Google Scholar]
- 24.Kanis JA, McCloskey EV. Epidemiology of vertebral osteoporosis. Bone. 1992;13(Suppl 2):S1–10. doi: 10.1016/8756-3282(92)90189-4. [DOI] [PubMed] [Google Scholar]
- 25.Garraway WM, Stauffer RN, Kurland LT, O’Fallon WM. Limb fractures in a defined population. II. Orthopedic treatment and utilization of health care. Mayo Clin Proc. 1979;54:708–713. [PubMed] [Google Scholar]
- 26.Kanis JA, Pitt FA. Epidemiology of osteoporosis. Bone. 1992;13(Suppl 1):S7–15. doi: 10.1016/s8756-3282(09)80004-5. [DOI] [PubMed] [Google Scholar]
- 27.Schwenkglenks M, Lippuner K, Hauselmann HJ, Szucs TD. A model of osteoporosis impact in Switzerland 2000–2020. Osteoporos Int. 2005;16:659–671. doi: 10.1007/s00198-004-1743-x. [DOI] [PubMed] [Google Scholar]
- 28.Bouza C, Lopez T, Palma M, Amate JM. Hospitalised osteoporotic vertebral fractures in Spain: analysis of the national hospital discharge registry. Osteoporos Int. 2007;18:649–657. doi: 10.1007/s00198-006-0292-x. [DOI] [PubMed] [Google Scholar]
- 29.Phillips S, Fox N, Jacobs J, Wright WE. The direct medical costs of osteoporosis for American women aged 45 and older, 1986. Bone. 1988;9:271–279. doi: 10.1016/8756-3282(88)90009-9. [DOI] [PubMed] [Google Scholar]
- 30.Lippuner K, von Overbeck J, Perrelet R, Bosshard H, Jaeger P. Incidence and direct medical costs of hospitalizations due to osteoporotic fractures in Switzerland. Osteoporos Int. 1997;7:414–425. doi: 10.1007/pl00004149. [DOI] [PubMed] [Google Scholar]
- 31.Johnell O, Gullberg B, Kanis JA. The hospital burden of vertebral fracture in Europe: a study of national register sources. Osteoporos Int. 1997;7:138–144. doi: 10.1007/BF01623689. [DOI] [PubMed] [Google Scholar]
- 32.Johnell O, Kanis JA, Jonsson B, Oden A, Johansson H, De Laet C. The burden of hospitalised fractures in Sweden. Osteoporos Int. 2005;16:222–228. doi: 10.1007/s00198-004-1686-2. [DOI] [PubMed] [Google Scholar]
- 33.King AB, Tosteson AN, Wong JB, Solomon DH, Burge RT, Dawson-Hughes B. Interstate variation in the burden of fragility fractures. J Bone Miner Res. 2009;24:681–692. doi: 10.1359/jbmr.081226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hooven FH, Adachi JD, Adami S, Boonen S, Compston J, Cooper C, Delmas P, Diez-Perez A, Gehlbach S, Greenspan SL, LaCroix A, Lindsay R, Netelenbos JC, Pfeilschifter J, Roux C, Saag KG, Sambrook P, Silverman S, Siris E, Watts NB, Anderson FA., Jr The Global Longitudinal Study of Osteoporosis in Women (GLOW): rationale and study design. Osteoporos Int. 2009;20:1107–1116. doi: 10.1007/s00198-009-0958-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


