Abstract
Foreign body aspiration is seen frequently in pediatric and geriatric patients, but it can also be seen in adults. Needle aspiration is a common problem in our country. Foreign body aspiration can lead to complete airway obstruction, asphyxia and death but sometimes symptoms may not be evident during the early period of aspiration and patients may present with complications afterwards. Early diagnosis is important in foreign body aspiration for prevention of mortality and complications. Suspicion aroused by patient history is the first step towards a diagnosis. Plain radiography and tomography may be used for imaging. Bronchoscopy is performed for diagnosis if there is uncertainty after imaging and may also be used for the treatment of diagnosed cases. In this article, we present a foreign body aspiration case that presented with difficulty and pain while swallowing, subsequently found to be the result of a needle that was stuck between the oropharynx and epiglottis.
Keywords: Emergency medicine, Foreign body, Respiratory aspiration
1. Introduction
Tracheobronchial foreign body aspiration is a life threatening health problem which can be seen in all age groups. Approximately 75–85% of foreign body aspiration cases are seen in children under the age of 15 and the elderly.1 Although rarely seen in adults, foreign body aspiration may be seen in patients with neurological diseases, under the influence of alcohol or sedative drugs, with a seizure condition, exposed to facial trauma, or receiving general anesthesia. Frequently seen foreign bodies in the airway include beads, toy parts, and nuts in preschool children; erasers or plastic pen caps in school children; needles, bone fragments and dentures in adults.2
Although foreign body aspiration often leads to acute symptoms such as cough and airway obstruction symptoms, it may also present with delayed symptoms or complications such as pneumonia, atelectasis, and recurrent pulmonary infections, especially in geriatric patients. The diagnosis of foreign body aspiration can be made by history and radiological examinations. Once diagnosed, airway foreign bodies should be removed by flexible or semi-rigid bronchoscopy.3 Rarely, thoracotomy may be required for the treatment of deeply located foreign bodies.4
Foreign body aspiration leads to asphyxia and acute fatal respiratory failure if it causes complete or near complete obstruction at the level of trachea. On the other hand, foreign bodies which advance to the lower levels of the tracheobronchial tree, may cause deterioration of ventilation, and infection in pulmonary regions distal to the obstruction. In this report, we present a patient who aspirated a foreign body that luckily remained in the oropharynx before reaching the trachea.
2. Case report
A sixty-four-year-old male patient was admitted to the emergency department after choking on an injector needle. The patient explained that he inhaled the needle as he was preparing to inoculate his animals. While he was trying to open the cap over the needle of the injector with his mouth, he began to talk and suddenly choked on the needle. The patient had difficulty in swallowing and he felt something stinging in his throat. In physical examination, the patient's general condition was good, his vital signs were within normal limits. Inspection of the mouth and tonsils revealed no pathological findings. Respiratory sounds were normal. Other system examinations were normal.
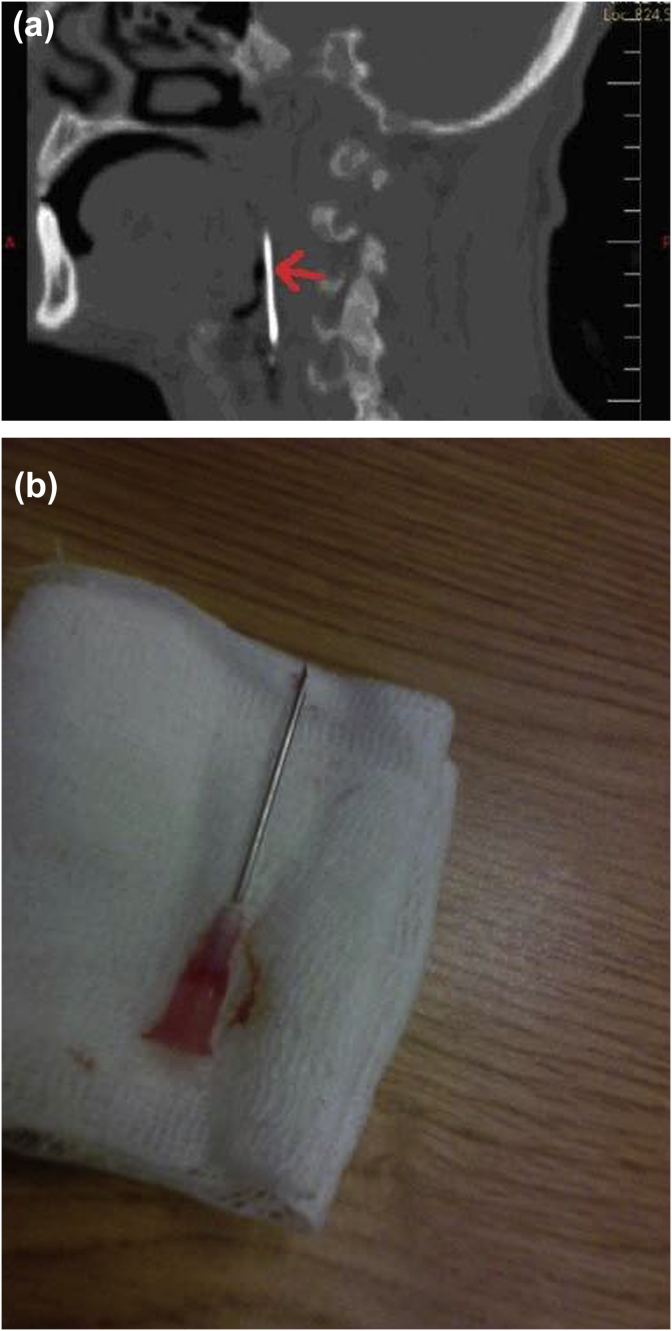
Initially, a lateral cervical radiograph was taken and the needle was observed in the oropharynx. The patient was evaluated by the otorhinolaryngology department. Computed tomography was performed in order to define the exact location of the needle. In computed tomography of the neck, the needle was about 4 cm long and was located in the oropharynx on the epiglottis towards the back of the tongue (Fig. 1a).
Fig. 1.
(a) Hyperdense needle seen in cervical computed tomography. (b) Needle removed by endoscopy.
The needle was removed in the operating room with the guidance of endoscopy by the department of otolaryngology (Fig. 1b). Since the tip of the injector needle was stuck on top of the epiglottis, the needle could not advance any further forward in the airway and the patient was protected from a possible tracheal aspiration. There were no complications during the removal process. The patient was prescribed antibiotics and analgesic treatment and discharged with recommendations.
3. Discussion
The history of the patient is very important for the diagnosis of a foreign body aspiration. Therefore, diagnosis is easier in adult patients who are able to describe the event of aspiration when compared to children or elderly patients who cannot describe it. In our case, the patient expressed that he aspirated the needle, so the diagnosis was easy to make.
Airway foreign body aspiration is often diagnosed in the early stages of the disease mostly because it causes symptoms such as shortness of breath, coughing, wheezing, and stridor. However, in some cases, the diagnosis can be difficult due to absence of typical symptoms or if the foreign body cannot be detected radiologically. In one study, it was reported that in 21.8% of cases, diagnosis is delayed for 30 days or longer.5 Aspirated foreign body's structural features and its location in the tracheobronchial tree may cause delays in diagnosis.6 Usually cough begins immediately after aspiration of foreign body, but afterwards the patient may be asymptomatic for a period of time.7 In our case, the needle was stuck on the epiglottis and it caused early symptoms such as dysphagia and a stinging sensation while swallowing, thus, symptoms lead to the diagnosis of foreign body aspiration.
Cases of needle aspiration in Turkey have been seen more frequently in children in the family as well as adults due to an increase in the wearing of headscarves. People usually try to fix their headscarves with both hands while holding the needles in their mouths. The needle is usually aspirated during activities that require deep inspiration, such as coughing, laughing and talking while they are holding the needles in their mouths.3 In our case, the patient tried to talk while he was opening the cap of the needle with his mouth and he aspirated the needle.
Although aspirated foreign bodies usually go into the right main bronchus, if aspirated during inspiration, narrow diametered objects like needles may also enter the left main bronchus.3 In our case, the foreign body stuck on the epiglottis and did not advance further downwards.
Cervical and chest radiographs may be used to define the presence and the localization of radio opaque objects in the diagnosis of foreign body aspiration. Since metal needles are radio opaque, radiography is a proper method in defining the localization of the needle in suspected aspiration cases. Bronchoscopy or computed tomography may be required, if the foreign bodies can not be seen in direct radiography at all or it is difficult to define the exact location of the needle. In some cases, three-dimensional computed tomography is used for better visualization of foreign bodies.8 In our case, we used radiography as the first method for defining the localization of the foreign body, followed by computed tomography.
In the treatment of foreign bodies aspirated into the respiratory tract, the object is visualized and removed with rigid or flexible bronchoscopy. Thoracotomy may be required for removing objects which cannot be removed by bronchoscopy. In our case, the foreign body was removed by bronchoscopy easily, because it was stuck into the upper level of the airway which can be accessed relatively easily. Thanks to advances in the diagnosis and treatment of foreign bodies in airways, the mortality and morbidity rates have fallen below 1%.9
4. Conclusion
Foreign body aspiration is an emergency condition which requires prompt diagnosis and treatment. Delay in diagnosis may lead to various complications. The history is important for early diagnosis. Physical examination findings may not always be diagnostic. Foreign body aspiration should be kept in mind by emergency department physicians in the differential diagnosis in patients who present with complaints relating to their airway.
Conflict of interest
The authors declare that there is no potential conflicts of interest.
Footnotes
Peer review under responsibility of The Emergency Medicine Association of Turkey.
References
- 1.Cangır A.K., Kutlay H. Foreign body aspiration. Turk Klin J Surg Med Sci. 2006;2:17–21. [Google Scholar]
- 2.Steen K.H., Zimmermann T. Tracheobronchial aspiration of foreign bodies in children: a study of 94 cases. Laryngoscope. 1990;100:525–530. doi: 10.1288/00005537-199005000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Çevik Y., Daş M., Ahmedali A., Balkan E., İçme F. Scarf pin aspirations that required thoracotomy and pulmonary resection. Turk J Emerg Med. 2010;10:82–85. [Google Scholar]
- 4.Al-Ali M.A., Khassawneh B., Alzoubi F. Utility of fiberoptic bronchoscopy for retrieval of aspirated headscarf pins. Respiration. 2007;74:309–313. doi: 10.1159/000098477. [DOI] [PubMed] [Google Scholar]
- 5.Saquib Mallick M., Rauf Khan A., Al-Bassam A. Late presentation of tracheobronchial foreign body aspiration in children. J Trop Pediatr. 2005;51:145–148. doi: 10.1093/tropej/fmh103. [DOI] [PubMed] [Google Scholar]
- 6.Pogorzelski A., Zebrak J., Pawlik J., Cherian Z., Buchwald J. Bronchopulmonary complications due to aspiration of foreign bodies by children. Pediatr Pol. 1995;70:325–331. [Article in Polish] [Abstract] [PubMed] [Google Scholar]
- 7.Kaptanoglu M., Nadir A., Dogan K., Sahin E. The heterodox nature of “Turban Pins” in foreign body aspiration; the central anatolian experience. Int J Pediatr Otorhinolaryngol. 2007;71:553–558. doi: 10.1016/j.ijporl.2006.11.017. [DOI] [PubMed] [Google Scholar]
- 8.Gullupınar B, Sarıhan A, Ersoy G. Oh No! Pin again! A case of foreign body aspiration. J Clin Anal Med, doı: 10.4328/JcAM.919.
- 9.Paşaoğlu I., Doğan R., Demircin M., Hatipoğlu A., Bozer A.Y. Bronchoscopic removal of foreign bodies in children: retrospective analysis of 822 cases. Thorac cardiovasc Surg. 1991;39:95–98. doi: 10.1055/s-2007-1013940. [DOI] [PubMed] [Google Scholar]