1 Scope and Purpose of the Guideline
1.1 Statement of problem
The mean duration of a normal pregnancy, calculated from the 1st day of the last menstrual period, is 280 days or 40 + 0 weeks of gestation (GW). A pregnancy prolonged by more than 14 days, in other words, a pregnancy lasting 294 days or 42 + 0 GW or more, is defined by the WHO and FIGO as prolonged, post-term or post-mature pregnancy. The period between 40 + 0 and 41 + 6 GW is referred to as late-term pregnancy.
More than 40 % of all pregnant women give birth after the expected date of delivery. Management of pregnant women with no onset of labor ranges from expectant management consisting only of intensive monitoring of mother and child to induction of labor.
1.2 Patient target population
This guideline focuses on the large group of women with low-risk singleton pregnancies who have no specific pregnancy risks (e.g. gestational diabetes, preeclampsia or IUGR).
1.3 Target users and area of care
This guideline aims to provide evidence-based recommendations to both gynecologists in private practice and physicians working in maternity hospitals to assist in decision-making when advising and managing pregnant women who are past their estimated and verified due date. This guideline differentiates between late-term pregnancy (40 + 0 GW to 41 + 6 GW) and post-term pregnancy (from 42 + 0 GW).
2 Epidemiology, Pathophysiology and Symptoms
2.1 Incidence
The incidence of post-term pregnancies according to reports published in the United Kingdom and the USA is 4.4–5.3 %. Data from Sweden reported an incidence of 6.5 % despite ultrasound screening done prior to GW 20.
In Germany, Austria and Switzerland, ultrasound is offered comprehensively in the 1st trimester as a standard procedure to all pregnant women since many years. Ultrasound examination performed in the 1st trimester results in a more precise estimation of the due date (compared to calculation based on the date of the last menstrual period), meaning that pregnancies which continue until ≥ 42 + 0 weeks are “genuine post-term pregnancies”. Data from the Institute for Applied Quality Improvement and Research in Healthcare in Germany (AQUA) for the year 2011 reported a gestational age at delivery of 42 + 0 weeks or above for only 0.61 % of newborns (3965 of 650 597 neonates). The estimated date of delivery was exceeded in 37.1 % of cases.
2.2 Etiology and pathogenesis
The etiology of late-term pregnancy has not yet been comprehensively investigated. Possible causes still being considered include primigravity, low socio-economic status, BMI > 35 and male gender of the fetus.
2.3 Pathophysiological aspects
Placental function and placental reserve capacity play important roles in late-term pregnancy. Despite the decreased rate of placental growth in the 3rd trimester, various adaptive mechanisms mean that the placenta can still considerably increase its functional capacity.
If placental function remains unimpaired after the estimated due date has passed, this will lead to increasing fetal weight gain. This explains the higher rates (20–25 %) of neonates with a birth weight of 4000 g in the group of newborns delivered at 42 + 0 GW compared to neonates born at 40 + 0 GW. From 41 + 0 GW, the risk of a birth weight of more than 4499 g is 3.5 times higher compared to delivery at term (OR = 3.5; 95 % CI: 3.4–3.7). This carries obstetrical risks for both the mother and the fetus (protracted labor, operative vaginal delivery, extended maternal soft-tissue injuries, shoulder dystocia, neonatal clavicular fracture, obstetrical brachial plexus palsy).
It is well documented that reduced amniotic fluid volume is an indication of placental insufficiency and is associated with increased perinatal morbidity (umbilical cord compression in oligohydramnios, abnormal CTG sub partu, meconium aspiration).
2.4 Perinatal mortality and morbidity in late-term and post-term pregnancy
Placental reserve capacity is a decisive factor for perinatal mortality and neonatal morbidity in late-term pregnancy. Continued fetal growth associated with sufficient placental reserve and decreased placental supply can both increase neonatal morbidity and mortality. These risks do not increase only from 42 + 0 GW. The risk of intrauterine fetal death, perinatal death, neonatal death and neonatal morbidity (aspiration; umbilical cord complications; prenatal, perinatal and postnatal asphyxia; pneumonia; sepsis; neurological birth trauma; peripheral nerve damage and fractures) increases continually in late-term pregnancy.
2.4.1 Perinatal mortality
Several large retrospective studies were done in Scandinavia, England and the USA which showed – after analysis of the risks associated with late-term and post-term pregnancy – that the risk of fetal intrauterine death (IUFD) was lowest at 38 weeks of gestation and subsequently increased more and more steeply with increasing gestational age. The fetuses of primigravid pregnant women aged 35 years and above were found to be particularly at risk for IUFD after 40 GW.
However, recent data from the state of Baden-Württemberg in Germany showed a distinctly flatter rise in the rates of IUFD between 41 + 0 GW and 41 + 6 GW. But from 42 + 0 GW the risk was also found to be significantly increased (Fig. 1).
Fig. 1.
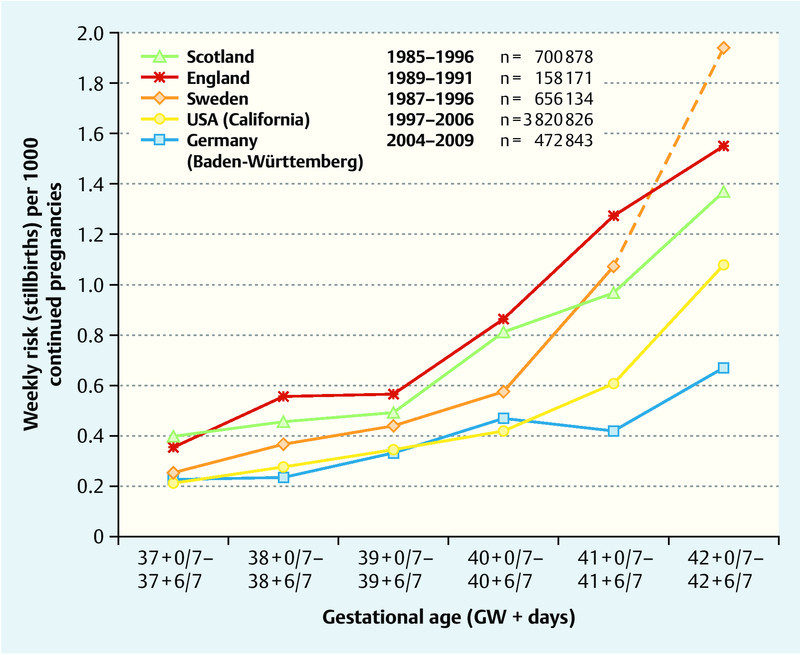
International comparison of weekly risk of stillbirth for every 1000 late- and post-term pregnancies at the beginning of each week: Scotland: [Smith 2001]; England [Hilder 1998]; Sweden [Divon 2004]; California [Rosenstein 2012]; Baden-Württemberg [Weiss 2013]. Fisherʼs Exact Test for 41 + 0–41 + 6 GW: Baden-Württemberg vs. Scotland, England and Sweden: p < 0.001; Baden-Württemberg vs. California: p < 0.05.
2.4.1.1 Influence of other constellations of maternal risk factors on fetal mortality
Out of the non-pregnancy-induced risk factors (i.e., maternal obesity, maternal age, parity and smoking), maternal obesity (BMI at the start of pregnancy ≥ 30 kg/m2) was found in 8–18 % to be significantly associated with IUFD, with maternal age above 35 years associated in 7–11 %, smoking associated in 4–7 % and primigravity associated in up to 15 % with IUFD.
2.4.2 Neonatal morbidity
An increase of severe neonatal acidosis (umbilical artery blood pH < 7.0 and base excess > − 12) has been reported for neonates from 40 + 0 GW, together with increased rates of meconium aspiration and shoulder dystocia. This shows that neonatal morbidity is similar to neonatal mortality in that it does not suddenly increase on reaching a gestational age of 42 + 0 GW. Most morbidity risks increase steadily. In principle, they are correlated with placental function: decreased placental reserve increases the risk of hypoxia-induced complications while undiminished placental reserve leads to increased fetal growth after the estimated due date is passed, with an increased potential for complications attributable to increasing fetal size.
Data on this issue is available from the perinatal surveys in Germany and Austria; analysis of the data showed a doubled incidence of acidosis between 37 + 0 GW and 42 + 6 GW.
Analysis of the incidence of fetal macrosomia showed an increase in newborns with a birth weight of more than 4000 g from 7 % in 39 + 0 to 39 + 6 GW to more than 22 % at 42 + 0 to 42 + 6 GW.
2.4.3 Maternal morbidity
Between 40 + 0 GW and 41 + 6 GW the rate of cesarean sections increased from 20 to 34 % and the rate of operative vaginal deliveries rose almost continuously from 8.5 to 15.5 %. The increasing number of macrosomic fetuses is likely to have played an important part in the increased rates of cesarean sections and operative vaginal deliveries. The higher incidence of third- or fourth-degree lacerations, secondary postpartum bleeding, and prolonged labor must also be interpreted as a result of increased numbers of neonates with a birth weight of more than 4000 g.
3 Recommendations
3.1 General principles
The general approach should consist of individual risk-adapted management done in consultation with the pregnant woman.
3.2 Information provided to pregnant women
The information provided to pregnant women must factor in the womanʼs individual risk situation. A BMI of more than 30 kg/m2 independently increases the risk of IUFD by a factor of 1.6 irrespective of whether the pregnancy is late-term or post-term and must be included in the advice given to the pregnant woman in addition to the other risk factors for IUFD (age, parity, smoking). The morbidity risk for mother and child created by increasing fetal size which, in turn, depends on how long past the due date they are, must also be discussed.
If there is an indication for inducing labor, the patient must be given information about the expected time frame (which cannot be individually predicted) and about the planned or recommended procedure used to induce labor. The fact that induction does not lead to higher rates of cesarean section should also be mentioned as reassurance.
3.3 Recommendations for diagnosis
It is important to determine gestational age as early and precisely as possible.
There is currently no evidence-based method which can be used to diagnose potential relative placental insufficiency in late-term and post-term pregnancy. CTG results allow inferences to be made about the current condition of the fetus and are performed without the patient experiencing contractions (non-stress test = NST).
The amniotic fluid volume can be assessed relatively quickly and easily by ultrasound. The aim of amniotic fluid volume measurement is to detect cases with oligohydramnios. The two most frequently used methods are amniotic fluid index and measurement of the deepest vertical amniotic fluid pocket. In late-term pregnancy, oligohydramnios on ultrasound is defined either as an amniotic fluid index of < 5 cm or an amniotic fluid pocket of < 3 cm on vertical measurement of the largest pocket.
The use of Doppler sonography to monitor late-term and post-term pregnancy is being discussed. At present, however, a final assessment of the validity of Doppler indices in low-risk late-term pregnancy has not been done, meaning that method should not be routinely used without other and additional indications.
3.4 Recommendations for the clinical management of low-risk pregnancies
3.4.1 37 + 0 weeks of gestation to 39 + 6 weeks of gestation
In low risk pregnancies, there is no reason to recommend induction of labor. Monitoring should be carried out in accordance with the recommendations of the German Maternity Directive.
Patients aged more than 40 years can be offered induction of labor from 39 + 0 GW onwards in accordance with RCOG recommendations (RCOG 2013) (EL IV).
3.4.2 40 + 0 GW to 40 + 6 GW
When the calculated due date is achieved, the pregnant women should be checked again to ensure that the pregnancy really is a low-risk pregnancy. Ultrasound examination with assessment of fetal weight and determination of amniotic fluid volume to exclude oligohydramnios or previously undetected IUGR is suitable for this (EL IV).
If this examination and maternal history do not give any reasons to terminate the pregnancy, then the mother can continue to be managed expectantly until 40 + 6 GW while taking account of the recommendations listed in 3.1–3.3. Irrespective of this, termination of the pregnancy is indicated when results of the most recent examination indicate a risk for mother or child.
If the pregnant woman decides to continue to wait beyond her expected due date, CTG monitoring of the fetus from 40 + 0 GW is already part of the usual standard of care offered even in Germany, Austria and Switzerland even in low-risk pregnancies although the benefit of this monitoring has not been verified through evidence obtained in prospective randomized studies. The current AWMF guideline on the use of CTG in pregnancy and during delivery (available in German as: “Anwendung des CTG während Schwangerschaft und Geburt”) states that CTG monitoring is only indicated in low-risk late-term pregnancy from 41 + 0 GW onwards. However, the Authors are of the opinion that, in accordance with existing clinical practice, CTG monitoring should also be performed in low-risk pregnancies after the calculated due date (Good Clinical Practice).
3.4.3 41 + 0 GW to 41 + 6 GW
The most recent Cochrane Review for the year 2012 showed that if labor was induced from 41 + 0 GW
perinatal mortality was significantly reduced (RR: 0.31; 95 % CI: 0.12–0.81),
the risk of meconium aspiration syndrome was significantly reduced (RR: 0.50; 95 % CI: 0.34–0.73),
the risk of a birth weight of more than 4000 g was significantly reduced (RR: 0.73; 95 % CI: 0.64–0.84), and
the rate of cesarean sections was significantly reduced (RR: 0.89; 95 % CI: 0.81–0.97).
The Authors of this Guideline therefore recommend offering pregnant women the option of inducing labor from 41 + 0 GW and state that induction of labor must be recommended by 41 + 3 GW at the latest (EL I).
If one or several moderate risks are added, the recommendation to induce labor in individual cases will be made at 41 + 0 GW. If the pregnant woman decides to continue waiting until 41 + 6 GW after being advised and informed of all risks, then – in the absence of risks and if amniotic fluid volumes, measured every 2 days, are normal and the NST shows no signs of fetal compromise – expectant management can continue till 41 + 6 GW without increasing the risk of IUFD compared to the previous week. In individual cases, shorter monitoring intervals can be agreed on if the patient wishes for more intensive monitoring as part of an individualized approach.
The consultation should also include informing the patient that continuing the pregnancy beyond 42 + 0 GW should be avoided and that at that point, at the latest, the pregnancy should be terminated through induction of labor or cesarean section.
3.4.4 From 42 + 0 GW
From ≥ 42 + 0 GW induction of labor or termination of pregnancy with cesarean section is indicated even without the presence of other risk factors (EL Ia). The risk of IUFD increases significantly from this point on. Neonatal morbidities such as shoulder dystocia, meconium aspiration syndrome, peripartal asphyxia and pneumonia also increase significantly. Neonatal mortality is also increased as a result of increased perinatal morbidity (EL IIa). All of these risks should be mentioned to the pregnant women during the consultation.
4 Prevention
According to one study, regular coitus around the expected date of delivery resulted in a reduction of the duration of pregnancies of > 41 + 0 weeks and a lower rate of induction of labor (EL IIa). However the Cochrane Review did not consider this effect to be verified.
Prophylactic weekly membrane stripping is also an option from 38 GW onwards. Although some studies have reported that stripping is beneficial and involves no risks, because of the potential pain stripping can cause, its use should be limited to specially selected cases.
5 Appendix: Diagram for Recommended Management of Late-term, Low-risk, Singleton Pregnancy
If risks emerge or the findings of examinations are pathological (e.g. oligohydramnios), the decision regarding further management must be taken based on the individual patient and clinical considerations (induction/C-section/intensification of biophysical monitoring/in-patient monitoring, etc.) (Fig. 2).
Fig. 2.
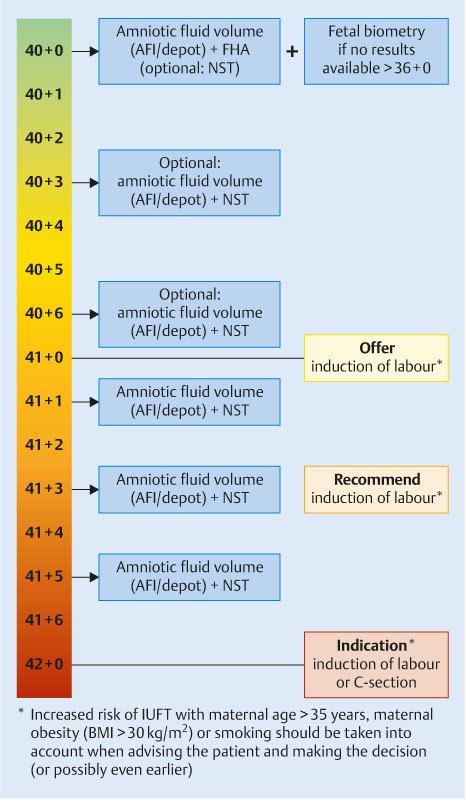
Graphical scheme of the recommendations in cases of low risk pregnancies from 40 + 0 GW onwards. AFI = amniotic fluid index, depot = deepest vertical pocket, NST = non-stress test, FHA = fetal heart activity
The guidelines published by Scientific Medical Societies in Germany are aids which have been systematically developed to assist physicians when making decisions in specific situations. The guidelines are based on current scientific knowledge and on established methods which have been proven in practice; the aim is to improve safety in medicine but also to take economic aspects into account. The guidelines are not legally binding for physicians and therefore the guidelines neither create liability nor do they constitute a release from liability. AWMF takes the greatest care when registering and publishing the guidelines of different scientific societies; nevertheless, AWMF cannot be held responsible for the accuracy of their contents. Please administer doses in accordance with manufacturerʼs instructions!
© Deutsche Gesellschaft für Gynäkologie und Geburtshilfe
Approved for electronic publication: AWMF online
| Date of compilation | 02/2010 |
| Revised | 02/2014 |
| Next planned revision | 01/2017 |
| Long version | Vorgehen bei Terminüberschreitung und Übertragung; AWMF Registry No. 015/065; classification: S1; effective: 28.02.2014, valid until January 31, 2017; www.awmf.org/ |
| Guideline report | Guideline report on the S1-Guideline 015/065: Vorgehen bei Terminüberschreitung und Übertragung, effective: 02/2 014; http://www.awmf.org/ |
| Statement of conflict of interest | All members of the commission signed a statement on potential conflicts of interest. Potential CoI were assessed with regard to their relevance for the contents of the guidelines. The members reported having no contact to persons who might be relevant for the guideline. The CoI table can be viewed at http://www.awmf.org/. |
| Slide show version | Vorgehen bei Terminüberschreitung und Übertragung. www.awmf.org/ |
| Contributing professional societies and organizations |
|
| Authors of the last revised version |
|
Footnotes
Note: The long version together with the full list of references and the guideline report are available in German from the AWMF homepage (www.awmf.org). AWMF is the Association of Scientific Medical Societies in Germany. Citation: National German Guideline (S1): Management of late-term and post-term pregnancy, AWMF Registry No. 015/065. Geburtsh Frauenheilk 2014; 74: 1099–1103
Supporting Information
German supporting information for this article
References
- The complete list of references can be viewed in the long version of the Guideline on the AWMF homepage (www.awmf.org).
- The validity of the guideline was confirmed by the Board of the DGGG [German Society for Gynecology and Obstetrics] and the DGGG Guidelines Commission in February 2014. The guideline will remain valid until 01/2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
German supporting information for this article


