INTRODUCTION
Primary central nervous system lymphoma (PCNSL) is defined as lymphoma confined to the brain, eye, spinal cord, or leptomeninges. It constitutes approximately 3% of all brain tumors, and 2–3% of all cases of non-Hodgkin lymphoma. Ocular involvement can be detected during clinical staging in about 20% of patients with PCNSL, with primary vitreous retinal lymphoma being the most common subtype. Uveal involvement of PCNSL is uncommon, and PCNSL with ciliary body involvement (CBL), to the best of our knowledge, has not been reported.
CASE REPORT
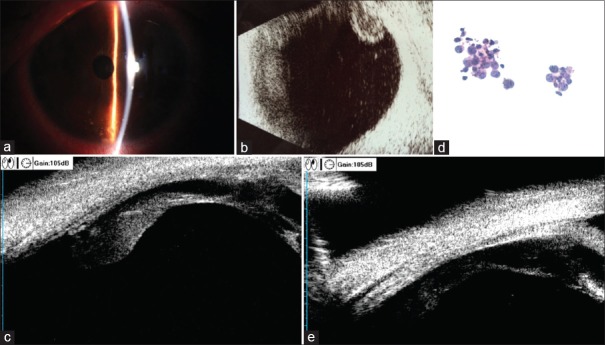
A 25-year-old male was presented to our hospital with projectile vomiting in March 2010. Brain magnetic resonance imaging (MRI) revealed multiple lesions with oval shaped hyperintensities on T1-weighted image [Figure 1a], and immunohistochemistry of the brain biopsy revealed large atypical CD20 and CD79α positive lymphoid cells. He was diagnosed as PCNSL of the diffuse large B-cell type and was treated with seven courses of chemotherapy (methotrexate [MTX], vincristine, ifosfamide, and dexamethasone) followed by one course of brain radiotherapy (3690cGy/22f/30d for whole brain and DT900cGy/5f/7d for local) in a period of 19 months. Remarkable remission of the lesions was observed [Figure 1b]. In October 2012, he was admitted to a local hospital with cataract and vitreous hemorrhage in the left eye and underwent combined phacoemulsification, intraocular lens implantation and vitrectomy. After surgery, however, his left eye had recalcitrant anterior chamber inflammation, vitreous haze, and increased intraocular pressure (IOP), and was referred to our center in March 2013. On admission, his best-corrected visual acuity (BCVA) was 1.2 in the right eye (OD) and 0.1 in the left eye (OS); IOP was 21 mmHg (1 mmHg = 0.133 kPa) OD and 34.1 mmHg OS; the left eye had mild anterior chamber inflammation with 1+ keratic precipitates, flare, and cells [Figure 2a], as well as scattered white lesions in the anterior chamber angle; dilated examination revealed vitreous opacity and a plurality of white lumps on the surface of inferior retina, while no significant findings were noted in the fundus. B-scan ultrasound revealed vitreous opacity and epiretinal deposits [Figure 2b], and ultrasound biomicroscopy (UBM) showed confluent ciliary body masses with almost 360° involved [Figure 2c]. Diagnostic vitrectomy was performed and cytology of the vitreous specimen revealed large atypical lymphoid cells [Figure 2d] which were CD20+ on flow cytometry. Brain MRI, cerebrospinal fluid and bone marrow cytologies were negative for malignancy. The patient was treated with ocular intensity modulation radiated therapy (IMRT, 45 Gy). One month later, BCVA of the left eye improved to 0.5 and IOP reduced to 16 mmHg without any IOP-lowering drugs, accompanied by a resolution of intraocular inflammation. UBM demonstrated regression of the ciliary body lesions [Figure 2e].
Figure 1.
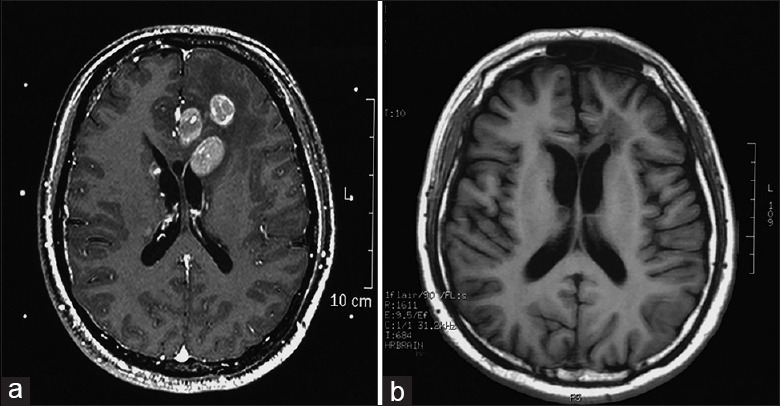
(a) Brain MRI at base line showed multiple lesions with oval shaped hyperintensities on T1-weighted MRI (T1-weighted image). (b) Significant regression of the lesions was observed after systemic chemotherapy and brain radiotherapy. MRI: Magnetic resonance imaging.
Figure 2.
(a) Anterior segment photography of the left eye showed the mutton-fat keratic precipitates scattered over the lower part of the cornea. (b) B-scan ultrasound of the left eye demonstrated vitreous opacity and epiretinal deposits. (c) Ultrasound biomicroscopy showed lesions grew over the pars plana of the ciliary body at the 3 o'clock position before radiotherapy. (d) Cytology of the vitreous specimen demonstrated large atypical lymphoid cells similar to those found in the brain tumor (HE, original magnification×40). (e) Ciliary body mass regressed after radiotherapy.
DISCUSSION
Primary intraocular lymphoma (PIOL) is rare with an incidence of about 4.8/million and approximately 300 new cases each year in the United States. While it typically affects seniors aged 60–85 years old, younger patients have been reported. The vast majority of PIOL is diffuse large B-cell lymphoma involving vitreous–retina complex; PIOL originates in the ciliary body (PCBL) is extremely rare,[1,2,3,4] and CBL of PCNSL, as is the case of our current patient, to the best of our knowledge, has not been reported.
Reported cases with ciliary body lymphoma were usually presented as mild anterior inflammation, secondary glaucoma, and concomitant iris infiltration;[1,2,3,4] none had systemic or CNS involvement except for one case in whom skin was involved later.[2] Our current patient, however, was a young male who complained blurred vision in the left eye 3 years after the diagnosis of PCNSL (diffuse large B-cell), and a complete ophthalmic examination revealed mild anterior inflammation, scattered granular white lesions in the angle of anterior chamber, as well as vitreous opacity with unremarkable fundus; UBM revealed epiretinal deposits and ciliary body masses with almost 360° involved. PCBLs were generally extranodal marginal zone type lymphoma[3,4] with few cases of T-cell or diffuse large B-cell types reported.[2,3] In our patient, however, the diagnosis of diffuse large B-cell lymphoma was established by cytology combining flow cytometry of both brain and vitreous samples.
Currently, high-dose MTX combining other chemotherapeutic agents, followed by whole brain radiotherapy, is recommended for treatment of PCNSL; in cases with ocular involvement, intravitreal injection of MTX or rituximab and ocular radiotherapy are suggested.[5] These treatments have improved the survival of PCNSL to 3+ years. This patient had dramatic clinical responses to systemic chemotherapy combining brain radiotherapy on diagnosis of PCNSL in 2010, and to IMRT on diagnosis of ocular recurrence in 2013, providing more evidence to the effectiveness of the above-mentioned treatment modalities.
In conclusion, ciliary body recurrence of lymphoma should be taken into consideration in PCNSL patients who presented with anterior chamber inflammation, raised IOP and unremarkable fundus. UBM is useful for evaluation of ciliary body lymphoma, and a vitreous or tissue biopsy should be considered in these patients for histopathology, which is the gold standard for the diagnosis of PCNSL/PIOL. Combined treatments of chemotherapy with radiotherapy might extend the survival time and preserve visual acuity for patients with ciliary body lymphoma.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Li-Min Chen
REFERENCES
- 1.Ahmed M, Androudi S, Brazitikos P, Paredes I, Foster CS. 360 degrees iris-ciliary body B-cell lymphoma masquerading as post-cataract uveitis. Semin Ophthalmol. 2004;19:127–9. doi: 10.1080/08820530490882706. doi: 10.1080/08820530490882706. [DOI] [PubMed] [Google Scholar]
- 2.Yahalom C, Cohen Y, Averbukh E, Anteby I, Amir G, Pe'er J. Bilateral iridociliary T-cell lymphoma. Arch Ophthalmol. 2002;120:204–7. [PubMed] [Google Scholar]
- 3.Mashayekhi A, Shields CL, Shields JA. Iris involvement by lymphoma: A review of 13 cases. Clin Experiment Ophthalmol. 2013;41:19–26. doi: 10.1111/j.1442-9071.2012.02811.x. doi: 10.1111/j.1442-9071.2012.02811.x. [DOI] [PubMed] [Google Scholar]
- 4.Konstantinidis L, Angi M, Coupland SE, Damato B. Primary B-cell lymphoma of the ciliary body with 360° ('ring'-like) growth pattern. Eye (Lond) 2013;28:355–6. doi: 10.1038/eye.2013.282. doi: 10.1038/eye.2013.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davis JL. Intraocular lymphoma: A clinical perspective. Eye (Lond) 2013;27:153–162. doi: 10.1038/eye.2012.250. doi: 10.1038/eye.2012.250. [DOI] [PMC free article] [PubMed] [Google Scholar]