Abstract
Background:
Accurate diagnosis is key to success. Diagnosing the pulpal status in varied clinical situations poses a challenge to the clinician. Electric pulp test (EPT) is one of the valuable attempts in evaluating the sensibility of pulp tissue. The aim of this study was to find out and compare the threshold levels and optimal electrode placement site for EPT in fluorosed and nonfluorosed anterior teeth.
Materials and Methodology:
Eighty volunteers recruited for this study were divided into two groups based on the incidence of dental fluorosis. Electric pulp testing was done on either of the central incisors in fluorosed and nonfluorosed group. Four sites on each crown were tested 4 times with digitest electric pulp tester, and the mean of the threshold responses was recorded. The data were analyzed with SPSS, version 11. Means of variables from each location were compared using one-way ANOVA and Tukey's post-hoc test while the critical level of significance was set at P < 0.05.
Results:
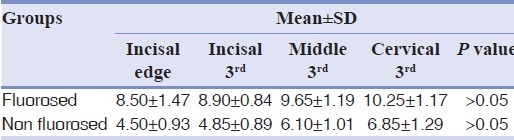
The mean and standard deviation of threshold levels in fluorosed teeth were greater when compared to that of nonfluorosed teeth at all sites with incisal edge showing the least mean threshold levels for both the groups (P > 0.05).
Conclusion:
Within the limitations of this study, it can be concluded that fluorosed teeth respond to higher threshold levels than the non-fluorosed teeth, and incisal edge was the optimal electrode placement site.
Keywords: Dental fluorosis, diagnosis, electric pulp test, electrode placement site, threshold response
INTRODUCTION
Successful endodontic treatment begins with an accurate diagnosis, which is the cornerstone for a successful treatment plan[1] wherein, the clinician should go through various diagnostic modalities before diagnosis and treatment plan.[2] Thorough clinical examination, detailed case history, radiographs, and pulp sensibility tests together aid in the diagnosis of dental pulp health and not the outcome of only one specific test.[3,4] In clinical practice, pulp sensibility tests (thermal and electric pulp tests [EPTs]) assess the integrity of the nerve fibers in the dentin-pulp complex by applying the stimulus to the outer surface of the tooth, whereas pulp vitality tests should assess the blood supply of the dental pulp.[5,6] Several devices that rely on the tooth's electrical properties are used in dentistry. Electronic root apex locators, pulp vitality tester, and early caries lesion detectors are some of such devices.[7]
EPT is more reliable than thermal tests[8] and is a technique sensitive procedure.[9,10] The ability of EPT to indicate pulp sensibility is based on the sensitivity of neural transmission. A positive response usually indicates vital sensory fibers presence. Nevertheless, it does not imply on blood supply which reflects the pulp vitality.[11] EPT is based on stimulation of intact Aδ nerves in the pulp-dentine complex by applying an electric current on the tooth surface, which results in an ionic shift in the dentinal fluid within the tubules causing local depolarization and subsequent generation of an action potential from the intact nerve and relies on subjective assessments and comments from the patient. These can lead to false-positive and false-negative results.[9,10,11] The various factors that influence EPT result for false positive or false negative response include the thickness of enamel and dentine, concentration of pulpal neural elements, direction of dentinal tubules, amount of dentinal fluid, and the distance between the electrode tip and the pulp.[12,13] EPT is an important aid and when properly used, is a safe clinical test that can provide useful information regarding health and disease of pulp tissue.[14,15,16]
Dental fluorosis is a developmental disturbance of dental enamel caused by excessive exposure to high concentration of fluoride during tooth development.[17] In routine clinical scenario fluorosed teeth are different from normal teeth. They pose many challenges in diagnosis and treatment planning to the clinician right from pulp sensibility tests, shade selection, shade mimicking, etching and bonding procedures during composite restorations.
The factors that influence EPT are the thickness of enamel and dentine, morphology of teeth, concentration of pulpal neural elements, direction of dentinal tubules, and the distance between the electrode tip and the pulp.[18,19,20] Many studies were done earlier to evaluate the optimal electrode placement site and threshold levels of EPT with varied opinions.[20,21,22]
The hypermineralized enamel in fluorosed teeth may influence the fluid concentration in the dentinal tubules, which is thought to play a vital role in the conduction of electric impulses.[11,23] In fluorosed enamel, hydroxyapatite crystals are substituted by fluorapatite crystals, which may result in ionic shift in the dentinal fluid.[24]
To best of our knowledge until date, no study has been done to evaluate threshold response and optimal electrode placement site on fluorosed teeth. Therefore, the aim of this study was to evaluate lowest threshold response and optimal electrode placement site for EPT in fluorosed anterior teeth.
MATERIALS AND METHODS
This clinical study was carried out in the Department of Conservative Dentistry and Endodontics, Kamineni Institute of Dental Sciences, Narketpally, Nalgonda (District), Telangana, State, India. Nalgonda District is globally recognized for the incidence of severe systemic and dental fluorosis with fluoride concentration up to 14ppm. Ethical clearance for the study was obtained from the Research and Ethics Committee of the Kamineni Institute of Dental Sciences.
Eighty volunteers of either gender, between 20 and 40 years old with intact maxillary central incisors with Thylstrup and Fejerskov Index (TFI) score 1-4 were selected [Figure 1]. Oral prophylaxis was performed for all the volunteers before proceeding for the study. Clinical examination was done independently by two different investigators, after wiping dry the teeth to assess the fluorotic severity according to the TFI.[25] Moreover, scores were recorded separately to avoid operator bias. Based on the incidence of fluorosis, total of 80 volunteers were divided into two groups as:
Figure 1.

The teeth with mild flourosis and intact crown (Thylstrup and Fejerskov Index score-2) selected for the study.
Group 1- Volunteers with incidence of dental fluorosis (TFI score was between 1 and 4)
Group 2- Volunteers without incidence of dental fluorosis (TFI score was 0).
To standardize the study, we selected either of the maxillary central incisors with an intact crown from each volunteer [Figure 1]. Baseline bitewing and periapical radiographs were taken for teeth which had neither history of orthodontic treatment nor trauma. The teeth with signs of surface loss (erosion, abrasion, attrition, abfraction), teeth with surface pitting, (TFI 5-9), cracks, inter proximal caries, metallic restorations, malformed teeth, traumatized teeth, endodontically treated teeth and teeth with periapical pathology were excluded from the study. Subjects taking narcotics, alcohol or nonsteroidal anti-inflammatory drugs and with a history of mental and emotional instability were excluded from the study.
The participants were informed fully about the procedure being carried out and informed consent was obtained. Tooth to be tested was isolated with rubber dam without the clamp. The test was conducted with a digitest EPT (Parkell, Farmingdale, NY, USA) in accordance with the manufacturer's instructions (a monopolar EPT with anodal electrode probe tip and diameter of 2 mm was used in the study). The circuit was completed when the subject rested a finger on the lip clip of the EPT. The tip of the electrode was lightly coated with toothpaste as a conducting medium, a gentle pulsed stimulus was applied to the tooth until the subject felt and noted a sensation such as tingling, stinging, warmth, or heat. They were instructed to release the clip on the first detection of a warm, tingling or painful sensation. The digital display readout of the pulp tester at which the subject first noted the above mentioned sensation was defined as the threshold.
Four sites (incisal edge, incisal third, middle third, and cervical third) on the labial surface of each tooth were tested. Four readings were made on the labial surface of each site in sequence, starting from the incisal edge to cervical third. To eliminate the phenomenon of nerve accommodation, at least 1 min was allowed to elapse before the tooth was revisited. The mean of the four readings from each site was scored.
The data were analyzed with SPSS, (IBM SPSS Statistics Version 19.0.0.329). Means of variables from each location were compared using one-way ANOVA and Tukey's Post-hoc test.
RESULTS
A total of 80 volunteers were recruited in this study and were categorized into two groups of 40 each. Three hundred and twenty electrode placement sites on 80 teeth were studied and analyzed statistically. A total of 640 readings from each group were obtained. Results were expressed as a mean ± standard deviation. The mean ± standard deviation threshold levels in the fluorosed group were 9.32 ± 1.35, whereas in nonfluorosed group, it was 5.57 ± 1.40. The higher threshold values were recorded in the fluorosed group when compared to that of nonfluorosed group and were statistically significant (P < 0.05).
When multiple comparisons were done among the groups, it was observed that there was a significant difference between incisal edge, middle and cervical thirds (P < 0.05). But no statistically significant difference between incisal edge and incisal third was noted (P > 0.05) [Table 1].
Table 1.
Mean and standard deviation at different sites in fluorosed and nonfluorosed teeth
DISCUSSION
Many studies earlier were done to evaluate the optimal electrode placement site and threshold levels of EPT with varied opinions. Bender et al.[20] concluded that placing the electrode at the incisal edge of anterior teeth evoked a response with the least amount of electrical current.[20] According to Lin et al.[26] the optimum site for pulp testing for first molars is the mesiobuccal cusp tip. Kalhoro et al.[27] conducted a study on premolar and stated that the buccal cusp tip of both maxillary and mandibular premolars were the site with the lowest threshold to EPT stimulation. In this study, maxillary central incisors with intact crowns were selected which differ from the earlier studies in relation to the sample size, population characteristics, and study design.
Endemic fluorosis continues to remain a challenging International Dental Health Problem. Nalgonda District of Telangana, India consists of areas with various levels of fluoride in drinking water, starting from below-optimum to optimum and above-optimum levels (up to14ppm). This area is ideal for assessing the prevalence and severity of dental fluorosis.
The earliest manifestation of dental fluorosis is an outer hypermineralized layer with a porous hypomineralized subsurface; the pores are occupied by enamel secretory proteins that are retained due to the effect of the excessive fluoride level on ameloblasts. Clinically, the porosity in the subsurface of enamel reflects as the opacity of the enamel, ranging from fine white opaque lines running across the tooth on all parts of the enamel to entirely chalky white teeth.[28]
Excessive fluoride concentration can cause the change of teeth structure and strength. High fluoride concentration on fluorosis enamel indicates the substitution of OH− by F− increasing the surface roughness of enamel surface.[28]
In the present study to measure dental fluorosis, TFI was used. This index allows correlation between the clinical appearance of fluorosis and pathological changes and is normally the index of choice for evaluation of fluorotic severity.
In the present study, maxillary central incisors were selected, as these teeth are of prime aesthetic concern and are considered to be most at risk for fluorosis.[29]
Volunteers within a narrow range of age group were selected to avoid sensitivity variation caused by secondary dentine deposition which causes a reduction in the volume of pulp, dental caries and tooth wear.[27,30]
In the present study, fluorosed teeth showed high threshold response when compared to nonfluorosed teeth, possible reasons may be hypermineralized enamel, which might influence the fluid concentration in the dentinal tubules, which is thought to play a vital role in the conduction of electric impulses.[9,28] In fluorosed enamel hydroxyapatite crystals are substituted by fluorapatite crystals which may result in ionic shift in the dentinal fluid.[24]
In the present study, in both fluorosed and nonfluorosed teeth incisal edge showed lowest threshold levels for EPT when compared to incisal, middle and cervical thirds because the enamel is thinnest incisally with the highest concentration of neural elements in the pulp horns while in the cervical area the number of nerve fibers decrease.[31] The straight course of dentinal tubules at the incisal edges of anterior teeth offers faster flow rate to the electric current.[12] This explains why the threshold values were lower at the incisal edge region than in the cervical third. These results were in accordance with Bender et al.[20] who found that the lowest threshold response was at the incisal edge. Structural and morphological variations of fluorosed anterior teeth did not show any variation in the optimal electrode placement site when compared to nonfluorosed teeth but have shown higher threshold levels to EPT. The possible reasons could be because of hypermineralized enamel, which might influence the fluid concentration in the dentinal tubules, which is thought to play a vital role in the conduction of electric impulses.[11,23] In fluorosed enamel hydroxyapatite crystals are substituted by fluorapatite crystals which may result in ionic shift in the dentinal fluid.[24]
During the study, it was observed that teeth with mild fluorosis which mimics nonfluorosed teeth reported high threshold levels for EPT which could be misread as delayed response of nonfluorosed teeth. In such cases, the clinician should take care not to misinterpret it as delayed response.
This base line study was done only on the anterior teeth with mild fluorosis with intact enamel surface. Further studies are required in posterior and severe fluorosed teeth for better understanding of the threshold response of fluorosed teeth to EPT.
CONCLUSION
Within the limitations of the study, it was observed that fluorosed teeth responded to high threshold levels, and the appropriate electrode placement site was the incisal edge.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or non-financial in this article.
ACKNOWLEDGMENTS
We would like to acknowledge Principal and Ethical committee of Kamineni institute of Dental Sciences, Narketpally, Telangana State for providing the needful help and support.
REFERENCES
- 1.Kulild JC. Diagnostic testing. In: Ingle JI, Bakland LK, Baumgartner JC, editors. Ingle's Endodntics. 6th ed. Hamilton: BC Decker Inc; 2008. pp. 532–546. [Google Scholar]
- 2.Noblett WC, Wilcox LR, Scamman F, Johnson WT, Diaz-Arnold A. Detection of pulpal circulation in vitro by pulse oximetry. J Endod. 1996;22:1–5. doi: 10.1016/S0099-2399(96)80226-3. [DOI] [PubMed] [Google Scholar]
- 3.Pitt Ford TR, Patel S. Technical equipment for assessment of dental pulp status. Endod Topics. 2004;7:2–13. [Google Scholar]
- 4.Gopikrishna V, Pradeep G, Venkateshbabu N. Assessment of pulp vitality: A review. Int J Paediatr Dent. 2009;19:3–15. doi: 10.1111/j.1365-263X.2008.00955.x. [DOI] [PubMed] [Google Scholar]
- 5.Nair BG, Reddy KA, Reddy MG, Reddy N. A review of laser dopplerflowmetry and pulse oximetry in dental pulp vitality. J Clin Diagn Res. 2011;5:903–5. [Google Scholar]
- 6.Lin J, Chandler NP. Electric pulp testing: A review. IntEndod J. 2008;41:365–74. doi: 10.1111/j.1365-2591.2008.01375.x. [DOI] [PubMed] [Google Scholar]
- 7.Gharizadeh N, Kaviani A, Nik S. Effect of using electric current during dentin bonding agent application on microleakage under simulated pulpal pressure condition. Dent Res J (Isfahan) 2010;7:23–7. [PMC free article] [PubMed] [Google Scholar]
- 8.Abdullah BA. Reliability of vitality tests. Jordan Dent J. 2001;16:72–7. [Google Scholar]
- 9.Cooley RL, Barkmeier WW. An alternative to electric pulp testing. Quintessence Int. 1977;8:23–5. [PubMed] [Google Scholar]
- 10.Millard HD. Electric pulp testers. Council on dental materials and devices. J Am Dent Assoc. 1973;86:872–3. [PubMed] [Google Scholar]
- 11.Pantera EA, Jr, Anderson RW, Pantera CT. Reliability of electric pulp testing after pulpal testing with dichlorodifluoromethane. J Endod. 1993;19:312–4. doi: 10.1016/s0099-2399(06)80463-2. [DOI] [PubMed] [Google Scholar]
- 12.Udoye CI, Jafarzadeh H, Okechi UC, Aguwa EN. Appropriate electrode placement site for electric pulp testing of anterior teeth in Nigerian adults: A clinical study. J Oral Sci. 2010;52:287–92. doi: 10.2334/josnusd.52.287. [DOI] [PubMed] [Google Scholar]
- 13.Grossman LL. Endodontic Practice. Philadelphia: Lea and Febiger; 1981. pp. 17–22. [Google Scholar]
- 14.Seltzer S, Bender IB, Ziontz M. The dynamics of pulp inflammation: Correlations between diagnostic data and actual histologic findings in the pulp. Oral Surg Oral Med Oral Pathol. 1963;16:969–77. doi: 10.1016/0030-4220(63)90201-9. [DOI] [PubMed] [Google Scholar]
- 15.Mumford JM. Pain perception threshold on stimulating human teeth and the histological condition of the pulp. Br Dent J. 1967;123:427–33. [PubMed] [Google Scholar]
- 16.Dummer PM, Hicks R, Huws D. Clinical signs and symptoms in pulp disease. Int Endod J. 1980;13:27–35. doi: 10.1111/j.1365-2591.1980.tb00834.x. [DOI] [PubMed] [Google Scholar]
- 17.Den Besten PK. Dental fluorosis: Its use as a biomarker. Adv Dent Res. 1994;8:105–10. doi: 10.1177/08959374940080010201. [DOI] [PubMed] [Google Scholar]
- 18.Lilja J. Sensory differences between crown and root dentin in human teeth. Acta Odontol Scand. 1980;38:285–91. doi: 10.3109/00016358009033595. [DOI] [PubMed] [Google Scholar]
- 19.Byers MR, Dong WK. Autoradiographic location of sensory nerve endings in dentin of monkey teeth. Anat Rec. 1983;205:441–54. doi: 10.1002/ar.1092050409. [DOI] [PubMed] [Google Scholar]
- 20.Bender IB, Landau MA, Fonsecca S, Trowbridge HO. The optimum placement-site of the electrode in electric pulp testing of the 12 anterior teeth. J Am Dent Assoc. 1989;118:305–10. doi: 10.14219/jada.archive.1989.0096. [DOI] [PubMed] [Google Scholar]
- 21.Jacobson JJ. Probe placement during electric pulp-testing procedures. Oral Surg Oral Med Oral Pathol. 1984;58:242–7. doi: 10.1016/0030-4220(84)90145-2. [DOI] [PubMed] [Google Scholar]
- 22.Cooley RL, Robison SF. Variables associated with electric pulp testing. Oral Surg Oral Med Oral Pathol. 1980;50:66–73. doi: 10.1016/0030-4220(80)90334-5. [DOI] [PubMed] [Google Scholar]
- 23.Torres-Gallegos I, Martinez-Castañon GA, Loyola-Rodriguez JP, Patiño-Marin N, Encinas A, Ruiz F, et al. Effectiveness of bonding resin-based composite to healthy and fluorotic enamel using total-etch and two self-etch adhesive systems. Dent Mater J. 2012;31:1021–7. doi: 10.4012/dmj.2012-140. [DOI] [PubMed] [Google Scholar]
- 24.Christensen GJ. Clinical factors affecting adhesion. Oper Dent Suppl. 1992;5:24–31. [PubMed] [Google Scholar]
- 25.Sherwood IA. Fluorosis varied treatment options. J Conserv Dent. 2010;13:47–53. doi: 10.4103/0972-0707.62631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin J, Chandler N, Purton D, Monteith B. Appropriate electrode placement site for electric pulp testing first molar teeth. J Endod. 2007;33:1296–8. doi: 10.1016/j.joen.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Kalhoro FA, Khoso NA, Salem AM, Shaikh MA. Selecting the appropriate electrode placement site for pulp tester on first premolar teeth. Pak Oral Dent J. 2012;32:132–5. [Google Scholar]
- 28.Fejerskov O, Manji F, Baelum V. The nature and mechanisms of dental fluorosis in man. J Dent Res. 1990;69:692–700. doi: 10.1177/00220345900690S135. [DOI] [PubMed] [Google Scholar]
- 29.Whelton HP, Ketley CE, McSweeney F, O’Mullane DM. A review of fluorosis in the European Union: Prevalence, risk factors and aesthetic issues. Community Dent Oral Epidemiol. 2004;32(Suppl 1):9–18. doi: 10.1111/j.1600-0528.2004.00134.x. [DOI] [PubMed] [Google Scholar]
- 30.Hargreaves KM, Goodis HE. Seltzer and Bender's dental pulp. Chicago: Quintissence; 2002. pp. 197–9. [Google Scholar]
- 31.Al-Salman TH. The effects of type of tooth and the placement site of electrode on the electrical pulp testing of the anterior teeth. Al-Rafidain Dent J. 2005;5:97–102. [Google Scholar]


