Abstract
Background:
Topical anesthesia has been widely advocated as an important component of atraumatic administration of intraoral local anesthesia. The aim of this study was to use direct observation of children's behavioral pain reactions during local anesthetic injection using cotton-roll vibration method compared with routine topical anesthesia.
Materials and Methods:
Forty-eight children participated in this randomized controlled clinical trial. They received two separate inferior alveolar nerve block or primary maxillary molar infiltration injections on contralateral sides of the jaws by both cotton-roll vibration (a combination of topical anesthesia gel, cotton roll, and vibration for physical distraction) and control (routine topical anesthesia) methods. Behavioral pain reactions of children were measured according to the author-developed face, head, foot, hand, trunk, and cry (FHFHTC) scale, resulting in total scores between 0 and 18.
Results:
The total scores on the FHFHTC scale ranged between 0-5 and 0-10 in the cotton-roll vibration and control methods, respectively. The mean ± standard deviation values of total scores on FHFHTC scale were lower in the cotton-roll vibration method (1.21 ± 1.38) than in control method (2.44 ± 2.18), and this was statistically significant (P < 0.001).
Conclusion:
It may be concluded that the cotton-roll vibration method can be more helpful than the routine topical anesthesia in reducing behavioral pain reactions in children during local anesthesia administration.
Keywords: Dental fear, local anesthesia, pediatric dentistry
INTRODUCTION
The terms “dental fear” and “dental anxiety” are often used synonymously and are considered to be a common problem. While they can affect people of all ages, the condition appears to develop mostly in childhood.[1,2,3,4] Fear of pain from the needle during local anesthesia, the mainstay of pain control during intraoral operative procedures, has been frequently indicated to be the most fear-evoking stimulus for dentally anxious children.[2,5]
Needle insertion and the deposition of solution are two aspects of local anesthetic injection that can cause pain. Topical anesthesia has been widely advocated as a method for reducing the discomfort associated with needle insertion and is an important component of atraumatic administration of intraoral local anesthesia.[6,7,8] The additional time required to apply topical anesthesia may increase the child's apprehension concerning the approaching procedure,[8] and the usefulness of topical anesthesia has been debated in several studies. It also seems that the benefits of topical anesthetics are not only pharmacological but also psychological.[7,8,9,10,11]
Pain is a complex behavioral phenomenon that is not fully understood. Behavioral pain reaction ratings by direct observation, reports from the child or accompanying parent, and physiological measures are three main techniques for the assessment of dental fear and behavior management problems during the administration of local anesthesia.[1,12,13] In the present study, observational technique has been chosen for behavioral pain reaction assessment for two reasons. The first is that children are not aware that they want to receive an injection. The second is that the capacity of younger children for self-report of subjective experiences is doubtful.[13]
Distraction during an injection has always been a technique to avert discomfort and negative feelings about that procedure as well as the entire dental appointment.[8] Hence, the aim of this study was to use direct observation to compare children's behavioral pain reactions when receiving anesthesia by cotton-roll vibration method versus routine topical anesthesia procedure.
MATERIALS AND METHODS
In this randomized controlled clinical trial, 48 children with a mean age of 5.94 ± 1.88 (3.25-9.6) years, referred to a private specialty pediatric dental clinic, were entered into the study to assess their reactions to each of two methods of local anesthesia administration including cotton-roll vibration method versus control method. Based on a pilot study conducted on 20 children, and by considering a power level of 0.80, an alpha level of 0.05, and Δ = 0.5 as the underlying treatment benefit for cotton-roll vibration method versus control method in children's behavioral pain reactions, the final sample size was determined as 48 children. To be included in the study, children had to be healthy with no history of systemic or psychological diseases, have no previous dental history, and were required to have two separate inferior alveolar nerve block or primary maxillary molar infiltration injections on contralateral sides of the jaws in the treatment process, with written parental permission. Children would be excluded from the study if they had a previous history of local anesthesia injection in another clinic and/or had a severe gag reflex. The protocol of this study was reviewed and approved by the Medical Research Ethics Committee of Rafsanjan University of Medical Sciences.
Children were introduced to dentistry in one or two sessions via prophylaxis with a rubber cup in a slow-speed handpiece and fluoride therapy. Before the first session of treatment with local anesthesia injection, the method of injection (cotton roll or control) was randomly assigned by the toss of a coin. Each child received the other method on the other side of the mouth at the next session.
In both methods, a standardized script of verbal distraction was used. A cylindrical cotton roll with a cherry-flavored red Master-Dent 20% benzocaine topical anesthesia gel (Dentonics, Inc., Monroe, NC, USA) applied to its head, without waiting for topical anesthesia gel to affect, was used for physical distraction in the cotton-roll method. Initially, the other head of the cotton roll was used to dry the needle insertion area for 2-3 s after which the cotton roll was rotated, and the gel was in contact with the needle insertion area kept in position by the dentist's left hand. Then, the dentist used his right hand and peripheral vision to smoothly and slowly bring the syringe to the child's mouth, and the cotton roll with gel remained in place with a mild vibratory stimulus applied by the left hand during the around 1 min injection of a carpule with 2% lidocaine and 1/80,000 epinephrine (Darou Pakhsh, Tehran, Iran) by means of a 27-gauge needle (Technophar s.p.a., Delebio, Italy). After injection, the syringe was removed, and mild vibratory stimuli with the cotton roll continued for a few seconds while the dentist pretended that this was the fault of the microbes of the tooth that did not want to sleep.
In the control method, the same amount of the same topical anesthesia gel applied using a cotton-tipped applicator for 1 min to the needle insertion area, which had been adequately dried with a 1 inch ×1 inch cotton gauze pad for a few seconds (routine topical anesthesia procedure according to the textbook).[8] After that, the applicator was removed, and the syringe was brought to the child's mouth smoothly and slowly with the dentist using peripheral vision, and with the same local anesthetic and the same needle gauge an injection was administered for 1 min. All these procedures have been done by the first author of the study. The local anesthesia duration was recorded in seconds from the start of drying until removing of the syringe and cotton roll in the control and cotton roll methods, respectively.
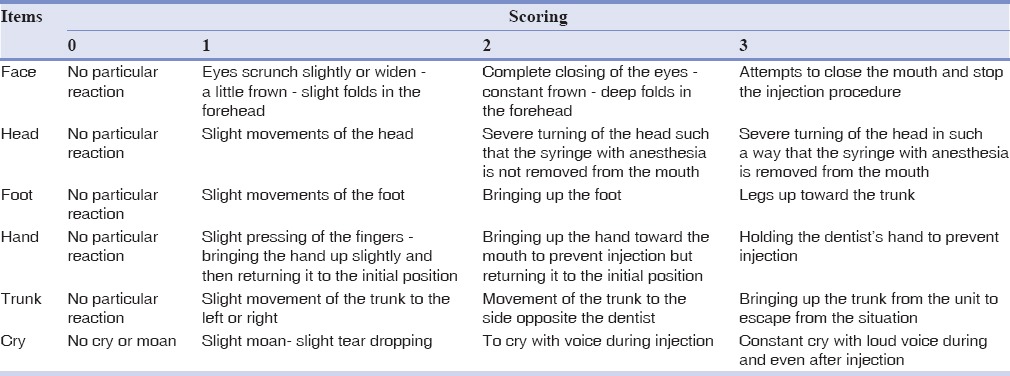
The children's behavioral pain reactions were measured according to the author-developed face, head, foot, hand, trunk, and cry (FHFHTC) scale, which was inspired by the face, legs, activity, cry, and consolability scale[14] for scoring postoperative pain in young children. The content validity of this scale has been evaluated by seven pediatric dentists. In this scale, each item is scored from zero to three [Table 1], which results in a total score of 0-18. To be more precise, these reactions were recorded by two extra nurses present in the treatment room who were unaware of the philosophy of the research. One nurse recorded the face, head, and cry reactions, and the other recorded the hand, foot, and trunk reactions.
Table 1.
Face, head, foot, hand, trunk, and cry scale for assessment of behavioral pain reactions in children during local anesthesia injection
In this clinical trial, the patient and statistical analyzer were blind. Results are presented as mean ± standard deviation (SD) for numeric variables, including reaction to local anesthesia, and are summarized by absolute frequencies and percentages for categorical variables. Reactions to local anesthesia in the cotton roll and control methods were compared by a paired t-test since only one group of children received the two local anesthesia procedures. Reactions to local anesthesia were compared by independent two-sample t-test across children <6 and ≥6 years of age. For statistical analysis, the statistical software SPSS version 15.0 for Windows (SPSS Inc., Chicago, IL, USA) was used. All P values were two-tailed, with statistical significance defined as P ≤ 0.05.
RESULTS
Twenty-five children received the cotton-roll vibration method and 23 received the control method before administration in the first injection session. The median (1st quartile, 3rd quartile) time between the first and second injection sessions was 4 (2, 7) days. The minimum and maximum (mean ± SD) of local anesthesia duration were 65 and 100 (78.94 ± 8.05) and 120 and 155 (135.08 ± 10.70) s in the cotton-roll vibration and control methods, respectively. The duration of local anesthesia administered by the cotton-roll vibration method was, on average, around 56 s shorter than the control method.
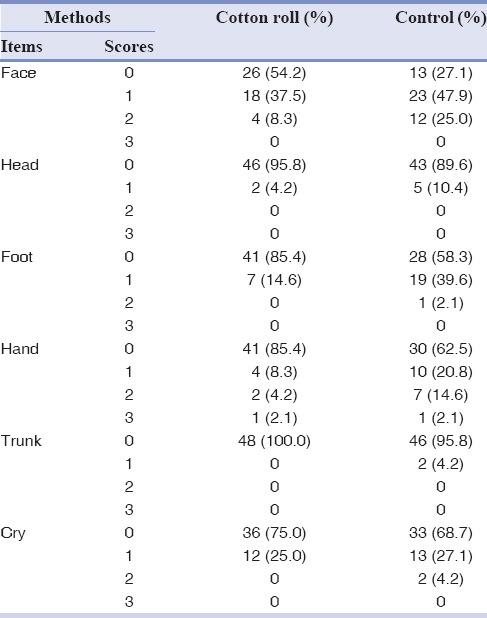
Table 2 presents the frequency distribution of behavioral pain reaction scores in the FHFHTC scale in two methods. In both methods, the most and least behavioral pain reactions were observed in the face and trunk, respectively.
Table 2.
Frequency distribution of behavioral pain reaction scores in the face, head, foot, hand, trunk, and cry scale in two methods (n=48)
The total scores of FHFHTC scale ranged between 0-5 and 0-10 in the experimental and control methods, respectively. The mean ± SD of total scores on FHFHTC scale was found to be statistically lower in the experimental method (1.21 ± 1.38) compared with the control method (2.44 ± 2.18), and paired t-tests showed that it was significant (P < 0.001).
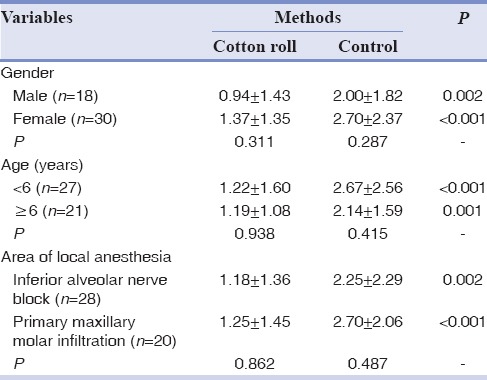
Comparison of mean behavioral pain reaction scores according to gender, age, and area of local anesthesia in two methods is presented in Table 3. As can be seen in Table 3, regardless of gender, age, and area of local anesthesia, the mean behavioral pain reaction scores were significantly lower in the cotton-roll vibration method than in the other method (P < 0.05). In each method, however, there were no statistically significant differences of behavioral pain reaction scores according to these variables (P > 0.05).
Table 3.
Comparison of mean behavioral pain reaction scores according to gender, age, and area of local anesthesia in two methods
DISCUSSION
Making good memories for children during dental visits is one of the most important aims of pediatric dentistry. Dental anxiety and fear-related behaviors associated with dental injections are undoubtedly among the most challenging aspects of pediatric dentistry, and proper intraoral local anesthesia is the mainstay of pain control during dentistry procedures.[2,7,15] Despite improvements in pain control, dental fear has remained relatively constant during the last 50 years, and the use of topical anesthesia is the most commonly advocated technique to reduce pain associated with oral injections.[3,7,11]
The results of this study indicated that the total scores for pain behavioral reaction in the cotton-roll group (that we did not wait for topical anesthesia gel to affect) were significantly lower than those in the routine topical anesthetic method (1 min gel application to the needle insertion area) that may confirm the hypothesis that topical anesthesia has more psychological effects than pharmacological effects. This hypothesis was stated in Meechan's review of intraoral topical anesthesia.[7]
As a general rule, topical anesthetics by affecting superficial tissues pharmacologically (2-3 mm), prevent deep tissues becoming anesthetized.[16] Results of this study indicated that regardless of the local anesthesia area (inferior alveolar nerve block with approximately 20 mm of needle penetration and primary maxillary molar infiltration with a few millimeters of needle penetration), the cotton-roll method caused fewer behavioral reactions to pain. This finding may also demonstrate that the psychological aspect of topical anesthesia is more effective than the pharmacological one.
In the cotton-roll vibration method, which was described here and has been used for several years by the author, the main component is to pretend that the use of colored topical anesthesia gel makes the teeth's microbes “sleepy.” Distracting the child's attention from the syringe by application of vibratory stimuli of the needle insertion area by the cotton roll during injection also plays an important role in this method. The results of this study indicate that utilizing this method has certain advantages for dentists. It requires shorter duration of intraoral local anesthesia than the method using routine topical anesthesia procedure, thereby resulting in shorter treatment duration, which is especially useful in pediatrics. It also has shown significantly reduced pain behavioral reactions than the method using routine topical anesthesia. Recently, vibratory devices that attach to dental syringes have been introduced[8] to facilitate counter-irritation in the injection area to modify noxious input, but in this cotton-roll vibration method, the cotton roll, which is available in all dental clinics, plays this role.
In the routine topical anesthesia, the cotton-tipped applicator with the topical anesthesia gel should be placed at the site of needle penetration for at least 1 min.[8] Compared with the cotton-roll vibration method, this has two disadvantages: The additional time required to apply the gel may make the child apprehensive concerning the impending procedure,[8] and also, because the child's mouth remains open for longer time in this technique, saliva will accumulate in the mouth, leading to discomfort for the child.
In the present study, the author-made FHFHTC scale, a behavioral rating scale relying on direct observation, was used to assess behavioral pain reactions, for several reasons. First, observational scales are preferred when the capacity for self-report of subjective experiences is not available or when the veracity of self-report is doubtful.[17] (The age range of the children in this study was 3.25-9.6 years). Second, although the self-report scales are gold standard,[13,17] they should be explained to the patients, but in this study we wanted to distract the child and pretend that nothing special happened. Thus, children should not be asked to explain what happened during the procedure. Third, this scale for behavioral pain reaction measurement is easy to use, and trained personnel can easily document it without being noticed by the child.
This FHFHTC scale for behavioral pain assessment also has two disadvantages: The first is a disadvantage of all observational scales. Behavioral pain reactions are what we observe while pain is what the patient feels, and the two do not always correlate,[1] and the second disadvantage is that sometimes the same scores for different items on this scale do not have the same value in pain reactions, for example, to cry with voice during injection (cry item) and bringing up the foot (foot item) both received a score of two, but they do not have the same value in pain presentation.
In this study, the FHFHTC items receiving the most and least reaction were face and trunk, respectively [Table 2]. The face is always the first part of the body to show emotion, including pain and facial expression, has been considered to be a more valid component for the assessment of pain.[13,18] The least reaction (trunk) can be explained by the fact that because the children were in a supine position during intraoral local anesthesia injections, it was more difficult for trunk reactions to occur.
CONCLUSION
The physical distraction with cotton-roll method can be more helpful than the routine topical anesthesia procedure in reducing behavioral pain reactions in children during local anesthesia administration
Topical anesthesia may have more psychological effects than pharmacological effects in reducing behavioral pain reactions in children during local anesthesia administration.
Financial support and sponsorship
This work was supported by Rafsanjan University of Medical Sciences (grant number: 31/9/3768). It has been registered in IRCT (IRCT2013042113076N1).
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or non-financial in this article.
ACKNOWLEDGMENTS
We acknowledge the contribution of Drs. Nematollahi H., Sarraf A., Mazhari F., Poreslami H., Shafiei A., Sharifi M., Khoramian S., and especially Ravari A., in content validity evaluation of the author-developed questionnaire of this research.
REFERENCES
- 1.Salem K, Kousha M, Anissian A, Shahabi A. Dental fear and concomitant factors in 3-6 year-old children. J Dent Res Dent Clin Dent Prospects. 2012;6:70–4. doi: 10.5681/joddd.2012.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Porritt J, Marshman Z, Rodd HD. Understanding children's dental anxiety and psychological approaches to its reduction. Int J Paediatr Dent. 2012;22:397–405. doi: 10.1111/j.1365-263X.2011.01208.x. [DOI] [PubMed] [Google Scholar]
- 3.Gustafsson A, Arnrup K, Broberg AG, Bodin L, Berggren U. Psychosocial concomitants to dental fear and behaviour management problems. Int J Paediatr Dent. 2007;17:449–59. doi: 10.1111/j.1365-263X.2007.00883.x. [DOI] [PubMed] [Google Scholar]
- 4.Locker D, Liddell A, Dempster L, Shapiro D. Age of onset of dental anxiety. J Dent Res. 1999;78:790–6. doi: 10.1177/00220345990780031201. [DOI] [PubMed] [Google Scholar]
- 5.Taani DQ, El-Qaderi SS, Abu Alhaija ES. Dental anxiety in children and its relationship to dental caries and gingival condition. Int J Dent Hyg. 2005;3:83–7. doi: 10.1111/j.1601-5037.2005.00127.x. [DOI] [PubMed] [Google Scholar]
- 6.Deepika A, Rao CR, Vinay C, Uloopi KS, Rao VV. Effectiveness of two flavored topical anesthetic agents in reducing injection pain in children: A comparative study. J Clin Pediatr Dent. 2012;37:15–8. doi: 10.17796/jcpd.37.1.h4jl152t334j3802. [DOI] [PubMed] [Google Scholar]
- 7.Meechan JG. Intraoral topical anesthesia. Periodontol 2000. 2008;46:56–79. doi: 10.1111/j.1600-0757.2008.00231.x. [DOI] [PubMed] [Google Scholar]
- 8.Wilson S. Local anesthesia and oral surgery in children. In: Casamassimo PS, Fields HW, McTigue DJ, Nowak AJ, editors. Pediatric Dentistry: Infancy Through Adolesence. 5th ed. St. Louis: Elsevier Saunders; 2013. pp. 398–410. [Google Scholar]
- 9.Nusstein JM, Beck M. Effectiveness of 20% benzocaine as a topical anesthetic for intraoral injections. Anesth Prog. 2003;50:159–63. [PMC free article] [PubMed] [Google Scholar]
- 10.Fukayama H, Suzuki N, Umino M. Comparison of topical anesthesia of 20% benzocaine and 60% lidocaine gel. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:157–61. doi: 10.1067/moe.2002.124858. [DOI] [PubMed] [Google Scholar]
- 11.Martin MD, Ramsay DS, Whitney C, Fiset L, Weinstein P. Topical anesthesia: Differentiating the pharmacological and psychological contributions to efficacy. Anesth Prog. 1994;41:40–7. [PMC free article] [PubMed] [Google Scholar]
- 12.Klingberg G, Broberg AG. Dental fear/anxiety and dental behaviour management problems in children and adolescents: A review of prevalence and concomitant psychological factors. Int J Paediatr Dent. 2007;17:391–406. doi: 10.1111/j.1365-263X.2007.00872.x. [DOI] [PubMed] [Google Scholar]
- 13.Arif-Rahu M, Fisher D, Matsuda Y. Biobehavioral measures for pain in the pediatric patient. Pain Manag Nurs. 2012;13:157–68. doi: 10.1016/j.pmn.2010.10.036. [DOI] [PubMed] [Google Scholar]
- 14.Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S. The FLACC: A behavioral scale for scoring postoperative pain in young children. Pediatr Nurs. 1997;23:293–7. [PubMed] [Google Scholar]
- 15.Majstorovic M, Veerkamp JS. Relationship between needle phobia and dental anxiety. J Dent Child (Chic) 2004;71:201–5. [PubMed] [Google Scholar]
- 16.Malamed SF, editor. Handbook of Local Anesthesia. 6th ed. St. Louis: Mosby Elsevier; 2013. Clinical action of specific agent; pp. 52–75. [Google Scholar]
- 17.Hadjistavropoulos T, Craig KD. A theoretical framework for understanding self-report and observational measures of pain: A communications model. Behav Res Ther. 2002;40:551–70. doi: 10.1016/s0005-7967(01)00072-9. [DOI] [PubMed] [Google Scholar]
- 18.Breau LM, McGrath PJ, Craig KD, Santor D, Cassidy KL, Reid GJ. Facial expression of children receiving immunizations: A principal components analysis of the child facial coding system. Clin J Pain. 2001;17:178–86. doi: 10.1097/00002508-200106000-00011. [DOI] [PubMed] [Google Scholar]


