Abstract
Fifty years after Chen has performed the first forearm replantation, we report our first case of hand replantation in a sub-Saharan African country. The etiology of the amputation was machete due to interpersonal violence. The amputation was trans-carpal, guillotine-type, subtotal non-viable maintained with a small skin bridge. The replantation procedure was successful. At one year follow-up, the functional result according to Chen's criteria was excellent. Through this first experience, we can state that hand replantation can be performed successfully both in survival and function in a non-specialized hospital of a sub-Saharan African country.
Keywords: Africa, hand, replantation, Togo
INTRODUCTION
Macroreplantations refer to amputations proximal to wrist or ankle joints. When there is evidence of a residual circulation the term revascularisation is used.[1] Since the first successful replantation of an arm in 1962 by Malt and McKhann in Boston and forearm in 1963 by Chen et al. in Shanghai,[2,3] the procedure has become common in developed countries. Replantation and revascularisation surgery requires the existence of a specialised centre, well-trained teams and microsurgeons, something that is not always available in sub-Saharan countries where refashioning and closure of the amputation stump are the common surgical procedures.[4,5] To the best of our knowledge, except in the Republic of South Africa, no case of hand replantation has been reported in a sub-Saharan country till now.
We report a case of hand replantation with 1-year follow-up.
CASE REPORT
A 17-year-old right-hand dominant male student was transferred to our traumatology Emergency Department (ED) on the 13th December 2012, 5 h after his left hand had been amputated in a knife fight. He was non-smoker with a poorly controlled seizure disorder. His left hand had been sharply amputated at the level of zone V with only a skin bridge at the lateral border of the wrist. X-ray showed that the amputation was through the distal third of scaphoid, capitate, hamate and base of the fifth metacarpal [Figure 1]. He had no other injuries. We immediately wrapped the hand in a fabric-containing ice to minimize warm ischaemia after we put a vascular shunt on the radial artery (use of a venous catheter 14-gauge) in the ED.
Figure 1.

(a) Subtotal non-viable left-hand amputation, (b) pre-operative X-ray showing fracture of scaphoid, capitate, hamate and parcelar articular fracture of the base of the fifth metacarpal
As the patient desired to keep his hand and his mother signed the consent form, the decision to attempt replantation was taken at the 7th h. The team consisted of plastic surgeon, anaesthesiologist and two theatre nurses. The procedure was done with nerve-block anaesthesia followed by general anaesthesia.
The patient was kept in a warm room with a postoperative orthosis and the hand elevated. The hand's circulation was monitored postoperatively by clinically observing for ischaemia signs. There were no vascular complications and no need for blood transfusion. A neurologist ordered anti-seizure protocol. We started low molecular weight heparin intraoperatively which was continued for 1 week, and aspirin (100 mg) was given for 1 month. Broad-spectrum antibiotique (cephalosporin and aminoside) were given intravenously for 5 days. On the 30th postoperative day, a superficial infection appeared at one K-wire site and was treated with broad-spectrum antibiotics and K-wire removal.
On the third post-operative day passive motion of the shoulder, elbow and digits was commenced. On the 10th day, the active motion of the wrist and digits was initiated within the confines of the orthosis by physiotherapy. At 3 weeks, the orthosis was removed for exercises and put for the rest of the day. At 6 weeks, the splint was totally removed. Special exercises to assist with activities of daily living were also done. Grip strength, forearm strengthening with rollers was used. Manual resistive strengthening for intrinsic and extrinsic muscles was done. All this protocol was used continuously for 4 months. However, it was difficult to maintain this regularly for the next 6 months because of the patient's uncontrolled seizure disorder and social condition. General anaesthesia was needed twice for the passive joint motion because of pain. No secondary surgical procedures were performed.
Functional evaluation was done at one year post replantation [Figure 2]. The patient recovered static two-point discrimination of 20 mm in all three peripheral nerves. His pinch strength was 50%, and grip strength was 40% of the opposite side. He had 45° of the active wrist with flexion and 35° of active wrist extension. Active range of motion in all fingers was 200° and thumb active range of motion was 130°. Intrinsic muscle function was good. The patient used the replanted hand for most daily tasks and some precise activities without pain or instability. The patient was highly satisfied with the result. He returned to the school.
Figure 2.
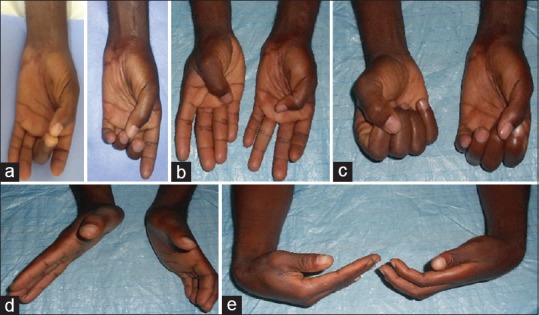
(a) Pollicidigital pinch, (b) thumb opposition, (c) grip strength, (d) wrist extension and (e) wrist flexion
DISCUSSION
In sub-Saharan countries, treatment of the majority of upper limb amputations is stump closure.[4,5] Reasons include ignorance, poverty, late presentation to the hospital, lack of proper care of amputated parts, lack of proper supplies at the hospital such as microsurgical sutures, instruments and magnification. Other relevant factors in Africa are the scarcity of hand surgeons, poor experience of surgeons and lack of a trained replantation team. The sequence of repair is directly influenced by the amount of muscle mass in the amputated part and ischaemia time.[6] In our case, warm ischaemia time was 5 h supported by a vascular shunt by the 6th h.
Psychological or neurologic illness has been cited as a contraindication to replantation.[7] Although our patient was epileptic, he did not develop any complication as a consequence of this.
We achieved a functional hand replantation in a sub-Saharan country just similar to other countries[8] probably because of the age the patient, the use of arterial shunt to reduce the ischaemia time and meticulous reparation of all tissues and hard work of physiotherapist. Through this first experience, we can state that hand replantation can be performed successfully both in survival and function in a non-specialised hospital of a sub-Saharan African country. This may be the beginning of a replantation team and populations need to be educated about conditions in order for replantation to be attempted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Biemer E. Definitions and classifications in replantation surgery. Br J Plast Surg. 1980;33:164–8. doi: 10.1016/0007-1226(80)90006-5. [DOI] [PubMed] [Google Scholar]
- 2.Malt RA, Mckhann C. Replantation of severed arms. JAMA. 1964;189:716–22. doi: 10.1001/jama.1964.03070100010002. [DOI] [PubMed] [Google Scholar]
- 3.Chen CW, Chien YC, Pao YS. Salvage of the forearm following complete traumatic amputation: Report of a case. Chin Med J (Engl) 1963;82:633–8. [PubMed] [Google Scholar]
- 4.Onuba O, Udoidiok E. The scope of amputation in developing countries. Postgraduate Doctor-Africa. 1989;11:118–21. [Google Scholar]
- 5.Omoke NI, Chukwu CO, Madubueze CC, Egwu AN. Traumatic extremity amputation in a Nigerian setting: Patterns and challenges of care. Int Orthop. 2012;36:613–8. doi: 10.1007/s00264-011-1322-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sabapathy SR, Venkatramani H, Bharathi RR, Bhardwaj P. Replantation surgery. J Hand Surg Am. 2011;36:1104–10. doi: 10.1016/j.jhsa.2011.03.039. [DOI] [PubMed] [Google Scholar]
- 7.Goldner RD, Urbaniak JR. Indications for replantation in the adult upper extremity. Occup Med. 1989;4:525–38. [PubMed] [Google Scholar]
- 8.Patel AA, Blount AL, Owens PW, Askari M. Functional outcomes of replantation following radiocarpal amputation. J Hand Surg Am. 2015;40:266–70. doi: 10.1016/j.jhsa.2014.10.017. [DOI] [PubMed] [Google Scholar]


