Abstract
The Edwin Bierman Award Lecture is presented in honor of the memory of Edwin L. Bierman, MD, an exemplary scientist, mentor, and leader in the field of diabetes, obesity, hyperlipidemia, and atherosclerosis. The award and lecture recognizes a leading scientist in the field of macrovascular complications and contributing risk factors in diabetes. George L. King, MD, of the Section of Vascular Cell Biology and Complications, Dianne Nunnally Hoppes Laboratory for Diabetes Complications, Joslin Diabetes Center, Harvard Medical School, Boston, MA, received the prestigious award at the American Diabetes Association’s 75th Scientific Sessions, 5–9 June 2015, in Boston, MA. He presented the Edwin Bierman Award Lecture, “Selective Insulin Resistance and the Development of Cardiovascular Disease in Diabetes,” on Sunday, 7 June 2015.
This review is focused on the factors and potential mechanisms that are causing various cardiovascular pathologies. In diabetes, insulin’s actions on the endothelium and other vascular cells have significant influence on systemic metabolisms and the development of cardiovascular pathologies. Our studies showed that insulin receptors on the endothelium are important for insulin transport across the endothelial barrier and mediate insulin’s actions in muscle, heart, fat, and the brain. Insulin actions on the vascular cells are mediated by two pathways involving the actions of either IRS/PI3K/Akt or Grb/Shc/MAPK. Insulin’s activation of IRS/PI3K/Akt results in mostly antiatherogenic actions, as this pathway induces activation of eNOS, the expressions of HO-1 and VEGF, and the reduction of VCAM-1. In contrast, insulin’s activation of the Grb/Shc/MAPK pathway mediates the expressions of ET-1 and PAI-1 and migration and proliferation of contractile cells, which have proatherogenic actions. Elevated levels of glucose, free fatty acids, and inflammatory cytokines due to diabetes and insulin resistance selectively inhibit insulin’s antiatherogenic actions via the IRS/PI3K/Akt pathway. This review provides evidence to support the importance of insulin actions in preventing cardiovascular pathology that can be selectively inhibited via the IRS/PI3K/Akt cascade in diabetes.
Introduction
It is my great honor to receive the Edwin Bierman Lecture Award at the 75th Scientific Sessions of the American Diabetes Association in Boston and give this lecture. Dr. Bierman was an outstanding scientist in vascular biology with special focus regarding lipids and atherosclerosis in people with diabetes. In addition, I had the personal privilege of being taught by Dr. Bierman while I was an intern and resident at the University of Washington Hospitals.
My research has focused on characterizing the mechanisms that are causing a variety of vascular complications in people with diabetes including retinopathy, nephropathy, and cardiovascular diseases (CVD). In this review I will focus on the factors and potential mechanisms by which diabetes is causing a variety vascular complications, especially those that are accelerating the progression of atherosclerosis. In general, complications of diabetes have been classified into those affecting the large arteries (macrovessels) or those involving the capillaries (microvessels) (1). This separation of diabetic vascular complications according to vascular sizes has been important in the understanding of their pathogenesis as the risk factors for causing the macrovascular and microvascular diseases are significantly different (1). For example, the most noted microvascular complications are retinopathy and nephropathy, which are predominantly associated with and caused by the presence of hyperglycemia (2). Thus, microvascular complications developed after the onset of diabetes can be dramatically prevented and their progression delayed by glycemic control in patients with type 1 and type 2 diabetes (3,4). In contrast, the risk factors for CVD are noted to occur preceding the diagnosis of type 2 diabetes and are associated with both insulin resistance and hyperglycemia (1). There are multiple risk factors that can lead to an increased prevalence of CVD: elevated free fatty acids (FFAs), hypertension, hyperlipidemia or dyslipidemia, and inflammation, to name a few (1). Thus, it is not surprising that glycemic control alone may not significantly reduce the risk of CVD in people with diabetes (4–6). In fact, people with insulin resistance and obesity have an elevated risk for CVD similar to that of those with diabetes (7). However, it is important to note that people with type 1 diabetes also have an elevated risk of CVD with insulin deficiency and modest insulin resistance, underscoring the importance of hyperglycemia (8).
In this review I will focus on the actions of insulin in insulin resistance or insulin deficiency that could either protect or accelerate pathologies on the arterial wall. In addition, I will also discuss the potential mechanisms by which hyperglycemia could be inhibiting the action of insulin in a selective manner. There are multiple pathologies in the cardiovascular system that can be induced by insulin resistance or deficiency or by hyperglycemia that are associated with diabetes. These include endothelial dysfunction, acceleration of atherosclerosis, increased risk of restenosis after stent placement, poor collateral vascular formation or angiogenesis, cardiomyopathy, and fibrosis of the myocardium (2). My laboratory has been focused on the role of insulin and its resistance with the additional risk imposed by hyperglycemia to accelerate the development of all of these complications in the cardiovascular system. Here, I will briefly describe the potential protective actions of insulin in normal physiology and how they are selectively inhibited by hyperglycemia and other factors such as inflammation to cause selective insulin resistance in multiple cardiovascular tissues, inducing the pathologies described above. This review is focused on insulin’s actions on the vascular wall with emphasis on the development of atherosclerosis. However, a detailed description on the complex topic of atherosclerosis is not possible here and has been reviewed extensively by others (9).
The Paradox of How Both Hyperinsulinemia and Insulin Deficiency Are Associated With CVD
Hyperinsulinemia is clearly related to insulin resistance and has also been shown to increase the risk of CVD in certain populations (10). It is likely that most of the associations between the increased risk of CVD and hyperinsulinemia are the result of insulin resistance. The increased risk of CVD in patients with type 1 diabetes who have insulin deficiency has been attributed to poor glycemic control and peripheral hyperinsulinemia due to exogenous insulin treatment (11).
However, recently, the ORIGIN Trial (Outcome Reduction With Initial Glargine Intervention) did not show any increased risk of cardiovascular events with the use of long-acting insulin (12). Thus, the increased CVD risk in type 1 diabetes is likely due to the myriad of metabolic abnormalities caused by insulin deficiency and hyperglycemia, such as dyslipidemia, hypertriglyceridemia, oxidized and glycolated proteins, decreased expression of angiogenic and vasotropic cytokines, and elevation of inflammatory cytokines (8).
As the ORIGIN Trial suggested that insulin may not increase the risk for cardiovascular events when hyperinsulinemia is induced by exogenous insulin injection, we have also studied whether endogenous hyperinsulinemia may increase the development of atherosclerosis. Using ApoE−/− mice that also had a single allele of the insulin receptor (IR) deleted, we studied the effect of hyperinsulinemia on atherosclerosis (13). Plasma insulin levels in the Insr−/+ApoE−/− mice were 50% higher than those in control ApoE−/− mice, but glucose tolerance tests were not different. Similarly, insulin sensitivity and signaling were comparable between Insr−/+ApoE−/− mice and control ApoE−/− mice. Infusion studies of insulin analogs showed that the mechanism for the elevated endogenous hyperinsulinemia in the Insr−/+ApoE−/− mice was related to the disposal of circulating insulin due to a 50% reduction of IRs in the various tissues (13). The extent of atherosclerotic lesions was not different between the Insr−/+ApoE−/− mice and the control ApoE−/− mice, even after 52 weeks of hyperinsulinemia. These data showed that endogenous hyperinsulinemia alone without insulin resistance will not enhance the severity of atherosclerosis (13).
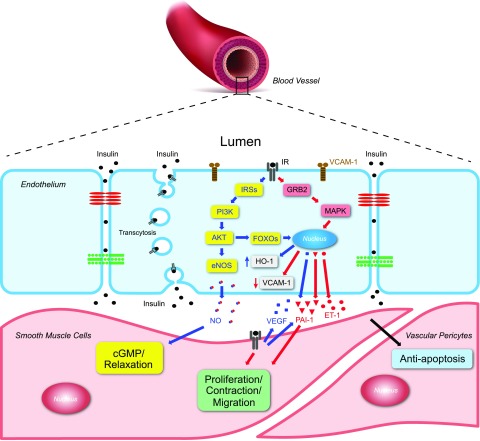
Our research has suggested that insulin interacts with the vascular wall in many ways (Fig. 1). In general, the endothelium can regulate the transport of insulin into the peripheral tissues that have continuous capillaries such as skeletal muscle, adipose tissue, the central nervous system, and others (14). Insulin can also induce action on vascular cells that we have postulated to be predominantly antiatherogenic, indicating that insulin could have protective actions on the vascular wall. However, there is a great deal of interest and controversy regarding the role of insulin on the vascular wall, suggesting that insulin could have either protective/antiatherogenic or proatherogenic actions depending on the insulin level and its activation of different insulin-sensitive pathways (15). We have postulated that insulin actions in the vascular cells can be either anti- or proatherosclerotic depending on the signaling pathways that have been activated.
Figure 1.
Effects of insulin’s many actions on the vascular wall. Insulin binds to the insulin receptor in the plasma membrane of the endothelium to mediate many actions, which can induce or inhibit many vasotropic substances. This schema represents the interaction of insulin with ECs and contractile cells in the arteries and capillaries to regulate many of its functions via transport of insulin across the endothelium and by the activation of the IRS/PI3K/Akt and SOS/Grb2/MAPK pathways. IRSs, IRS1/2.
Here, I will provide a general summary on insulin actions on the vascular wall and the concept of selective insulin resistance, which we believe is responsible for the majority of accelerated risk for cardiovascular pathology in people with diabetes and insulin resistance.
Insulin Signaling on the Vascular Tissue and Cells
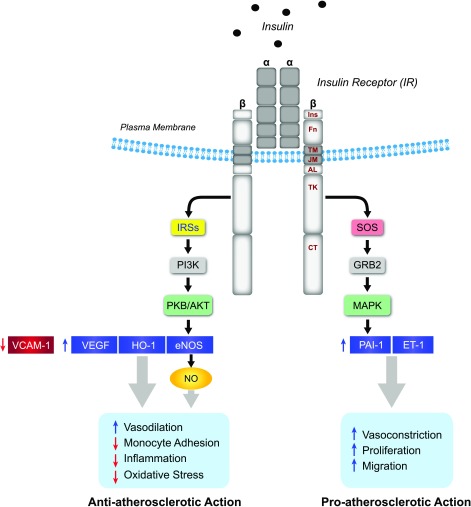
All cells in the arteries and capillaries have IRs, including the inflammatory cells that have migrated into the arterial walls (16). Similar to those in other types of cells, IRs in the vascular wall are composed of a binding α subunit connected by disulfide bonds to a β subunit, which is a tyrosine kinase (Fig. 2). IRs exist as heterodimers that can also form hybrid receptors with IGF1 receptors (17). Once insulin binds to the α subunit, the β subunit is activated with a series of tyrosine phosphorylations in the various domains of the β subunit, which can modulate tyrosine kinase activity (18). The signaling of insulin is mediated by at least two major pathways to activate phosphorylation of either the PI3K/Akt or the MAPK/Erk pathway system (Fig. 2). In order to activate the Akt cascade, the β subunit, once tyrosine phosphorylated, will recruit IR substrates 1 and 2 (IRS1/2), which are activated by tyrosine phosphorylation with subsequent binding to the PI3K. This in turn activates kinases PDK1 and PKB/Akt, leading to a host of metabolic actions such as translocation of GLUT4 to mediate glucose transport in myocardium or the regulation of the expressions of eNOS, VEGF, antioxidant enzyme HO-1, and VCAM-1 (19–22). Alternatively, the activated β subunit can interact with Grb2 and Shc, which do not need the activation of IRS1/2. The activation of Grb2 can induce the activation of G protein Ras, which will cause a cascade of phosphorylation from Raf to activate MAPKs such as MEK1 and ERK1/2. These are known to stimulate mitogenic actions or chronic actions of insulin including cell migration, expression of endothelin 1 (ET-1) (23) and PAI-1, and even the proliferation of pericytes and vascular smooth muscle cells (VSMCs) (24,25).
Figure 2.
Schema of IR structure and insulin signaling pathways in vascular cells. Insulin’s actions in vascular cells are mediated by the activation of either the IRS/PI3K/Akt or the SOS/Grb2/MAPK pathway. The IRS/PI3K/Akt pathway can activate eNOS and regulate the expression of HO-1, VEGF, and VCAM-1, which have antiatherosclerotic actions. In contrast, the SOS/Grb2/MAPK pathway activates vasocontraction and proliferation, which are proatherosclerotic effects. AL, activation loop; CT, carboxy-terminal tail; Fn, fibronectin type domains; Ins, insert in Fn; IRSs, IRS1/2; JM, juxtamembrane domain; TK, tyrosine-kinase domain; TM, transmembrane domain.
The analysis of the various functions of insulin outlined in Fig. 2 in vascular cells suggested to us that activity mediated through the activation of IRS/PI3K/Akt pathways can cause anti-inflammatory and antioxidative stress actions, which can be antiatherogenic. In contrast, insulin actions mediated through Grb2 and Shc, leading to MAPK activation, mediate biologic actions that would promote inflammation and restenosis (26). This dichotomy of insulin’s action in the vascular cells has led us to propose the idea of selective insulin resistance induced by diabetes, which will be discussed below (27). First, specific vasotropic actions of insulin in the vascular cells will be reviewed.
In Vascular Endothelial Cells
IRs in the endothelium have a unique function, which is to transport insulin across the endothelial barrier in order to mediate its actions in the surrounding tissues (Fig. 1). This function is especially important in those tissues that have continuous endothelium with tight junctions, such as those in the brain and retina; in addition, this process appears to be important also in muscle, myocardium, and possibly brown adipose tissue (28). We showed that IRs can mediate the transport of insulin across the endothelial barrier via a receptor-mediated pathway without significant degradation (14). Subsequent studies by others have shown that this is a part of the caveolin cycling process (29,30). This transcytosis process has been shown to be decreased in insulin resistance, as IRs can be downregulated in the presence of hyperinsulinemia (28).
It is also interesting that insulin has a great deal of specific endothelial functions. It is unclear, however, how insulin can be transported across the endothelium without degradation and how it can still mediate a whole set of cellular actions that should be limited in time, usually by its degradation as in other cells (14). The vascular-specific actions of insulin in the endothelium include regulating the expressions of VCAM-1, VEGF, ET-1, HO-1, and others, but one of the most important actions of insulin that is specific to the endothelium is that it increases the expression and the activation of eNOS (21,31). As endothelial cells (ECs) contain mainly GLUT1, insulin does not have significant effects on glucose transport (32). However, hyperinsulinemia may affect glucose metabolism via glycolysis and oxidative phosphorylation via mitochondria and alter EC migration, branching, and proliferation (33).
Insulin’s activation of eNOS to produce nitric oxide (NO) enhances smooth muscle vasodilatation and blood flow, which is impaired in obesity and insulin-resistant states (34). Insulin’s action in ECs has been well characterized as that of a vasodilator via NO production (34–36). NO is synthesized from l-arginine and O2 by eNOS with l-citrulline. The activity of eNOS is regulated by several mechanisms including posttranslational modification, allosteric enzyme activation, and subcellular localization (34). Among these mechanisms, insulin-stimulated NO synthesis is dependent on the IR/IRS1/PI3K/Akt pathway with the activation of Akt-mediated phosphorylation of eNOS at Ser1177, which is independent from the calmodulin intracellular Ca2+ concentrations in ECs (31). Furthermore, Ser615 of eNOS also contributes to insulin-mediated NO synthesis. Insulin may also decrease the interaction of caveolin-1 (Cav-1), a negative regulator of eNOS activity, and increase its association with eNOS-Hsp90, which promotes eNOS activity (37). Lastly, insulin has also been reported to increase the expression of eNOS at the transcription step (21). Other studies have reported that insulin can induce l-arginine transport into ECs and palmitoylation of eNOS to form eNOS–Cav-1, which translocates to plasma membrane (37). In insulin-resistant and diabetic states, NO production is reduced by the inhibition of insulin-induced eNOS phosphorylation and neutralized by the increased oxidant production of the vascular cells in response to hyperglycemia (34).
Insulin has also been shown to regulate the expression of HO-1 and VEGF and lower the expression of VCAM-1 in ECs (19,20,22). Regarding these actions, we have reported that insulin at physiological concentrations can increase the expression of VEGF and HO-1 and decrease the expression of VCAM-1 mainly via the IRS/PI3K/Akt pathway (Fig. 2). As increasing HO-1 may improve vascular functions with antioxidative stress actions (HO-1) and lowering VCAM-1 has anti-inflammatory effects by decreasing monocyte binding and uptake into the arterial wall, we believe the selective loss of these actions will lead to elevated risk of atherosclerosis. In addition, insulin has also been shown to increase the expressions of ET-1 and PAI-1, possibly through the MAPK pathways (38). As the MAPK pathways are not known to be inhibited in diabetes by either FFAs or hyperglycemia, these actions of insulin may actually enhance the atherogenic process. Insulin has many vasotropic actions in the endothelium mediated by either IRS/PI3K/Akt or MAPK pathways.
VSMCs and Capillary Pericytes
VSMCs and pericytes surround the endothelium, and their main function is to regulate the tone of the arteries and capillaries by their contractile properties. Both of these cell types have IRs with structures similar to those in other cells (16). In addition, the number of IRs on VSMCs appears to be significantly lower than those on ECs. In contrast, capillary pericytes appear to have a large number of IRs (39). Insulin can stimulate the activation of both the IRS/PI3K/Akt cascades and the MAPK/Erk pathways in these cells. Specific actions in VSMCs induced by insulin have not generally been well described. In most cases, VSMCs and pericytes are indirectly regulated by insulin through NO activation of cGMP and in response to vasodilation (40). Similarly, ET-1 secreted from ECs can also activate phospholipase C-β and cause the influx of Ca2+ from the sarcoplasmic reticulum, which leads to the activation of myosin light-chain kinase, again leading to vasocontraction (41). However, insulin has been shown to induce the expression of ET-1 in pericytes and VSMCs, which can be enhanced by PKC activation (42). In addition, insulin can also affect migration, apoptosis, and proliferation of VSMCs and pericytes. Reports have indicated that insulin may also increase the expression of ETA receptors to increase vascular tone (43). Most of the direct effects of insulin on VSMCs appear to be mediated via the activation of the MAPK pathway and usually require high concentrations of insulin. For example, insulin’s actions on migration and proliferation usually require 10–100 nmol/L of insulin as compared with its action on phosphorylated eNOS, which can be stimulated by 1–10 nmol/L of insulin (32). As migration and proliferation of VSMCs can contribute to restenosis and atherosclerosis, it is believed that insulin’s effect via hyperinsulinemia may contribute to these biological actions (1). Hyperglycemia has also been shown to affect proliferation and hypertrophy of VSMCs, possibly via the activation of PKC α isoform, contributing to the atherosclerotic process (44). Interestingly, we have reported that high glucose levels have the opposite effect in the capillary pericytes by inducing apoptosis, which appears to be mediated by at least two mechanisms including NF-κB activation due to oxidative stress and activation of p38 MAPK; the latter induces overexpression of SHP-1, a tyrosine phosphatase, which can inhibit antiapoptotic growth factors such as PDGF and insulin by dephosphorylating their receptors (45).
Monocytes and Macrophages
Monocytes and macrophages are important players in the development of atherosclerosis. Macrophages in the vascular wall are a main component of the atherosclerotic and restenotic processes. IRs, which can activate both IRS/PI3K/Akt and MAPK pathways, have been found in both monocytes and macrophages. In macrophages, insulin signaling through the IRS2/PI3K pathway can inhibit the expressions of proinflammatory chemokine MCP-1, as shown in macrophages with a specific deletion of IRS2 (46). Wild-type mice transplanted with IR−/− bone marrow showed macrophages lacking IR accumulation in the blood vessel wall without proinflammatory stimuli. A second study reported that macrophages with IR deficiency increased endoplasmic reticulum stress and apoptosis and necrotic core formation in the late stage of atherosclerotic lesions (47). These studies suggest that selective insulin resistance through the IRS/PI3K/Akt pathway in macrophages may contribute to atherosclerosis development.
Heart and Myocardial Blood Vessels
In the myocardium, insulin can induce the uptake of glucose via PI3K- and Akt-mediated recruitment of glucose transporter GLUT4 and also enhance glucose oxidation (48,49). Another key insulin action in the heart is its impact on cardiac metabolism by increasing energy production from carbohydrate oxidation. To generate ATP production in the heart, FFAs are transported into cardiomyocytes and enter the mitochondrial matrix for β-oxidation. The acetyl-CoA resulting from β-oxidation enters the tricarboxylic acid cycle, producing NADH and FADH2 products, which enter the electron transport chain to generate ATP. However, insulin-mediated cardiac metabolism and function are impaired with decreasing glucose uptake and inhibition of glucose utilization in insulin-resistant and diabetic states (48). As a result, the heart’s utilization of FFAs is increased in parallel with elevated reactive oxygen species, decreased cardiac mitochondrial function, and some increases in apoptosis (50). Similar to its effect on peripheral blood flow, insulin has an inotropic effect in myocardium via the PI3K pathway (51). In addition, we have reported that insulin is a key regulator of VEGF and angiogenesis in the myocardium via the IRS/PI3K/Akt pathway in response to hypoxia (52). In insulin-resistant or -deficient states, VEGF expressions are decreased in the myocardium or chronic wounds (53,54), which is the major reason for the decreased angiogenesis or collateral vessel formation in response to hypoxia in diabetes (53,54). We have reported that mice with IR deletion in the myocardium had less capillary density with hypoxia and lower levels of VEGF and angiogenesis. These abnormalities of angiogenesis were also reproduced in cultured cardiomyocytes isolated from insulin-resistant or diabetic rats and fibroblast cells from patients with diabetes. The mechanism responsible for the poor response was the inhibition of insulin’s action of the IRS/PI3K/Akt pathway by PKC activation induced by hyperglycemia or elevated FFAs in insulin resistance or diabetes (54).
Selective Insulin Resistance
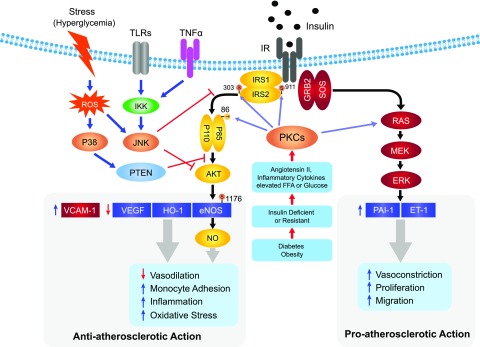
We proposed the idea of selective insulin resistance in order to explain the paradoxical findings that both loss of insulin actions and hyperinsulinemia appear to exaggerate the atherosclerotic process (Fig. 3). Our initial report showed that in the arteries from animal models of insulin resistance or diabetes and from patients with diabetes, insulin’s activation of phosphorylated Akt (pAkt) was blunted with parallel reduction of its antiatherogenic actions such as activation of eNOS (27). However, insulin’s action of MAPK/Erk was not inhibited (27). Since the first report of these findings, similar selective resistance has been shown in many tissues including myocardium, renal glomeruli, capillaries, fibroblasts, and even the liver. This selective inhibition of insulin’s pathway of IRS/PI3K/Akt coincided with all of insulin’s known vascular actions that have antiatherosclerotic or proangiogenic activities. These included activation of eNOS, increased expression of HO-1 and VEGF, and, most recently, the findings on the inhibition of VCAM-1 (Fig. 2). Similarly, insulin’s activation of MAPK was not inhibited and may even be enhanced; this activation was tied to proatherosclerotic actions such as expression of ET-1 and its receptors and migration and proliferation of VSMCs (Fig. 3). Interestingly, insulin’s actions via MAPK activation required high levels of insulin, which could explain the correlation of hyperinsulinemia with increased risk for atherosclerosis.
Figure 3.
Selective insulin resistance in vascular ECs. Selective insulin resistance in ECs occurs when angiotensin II, elevated FFA and glucose levels, and proinflammatory cytokines induced by diabetes and insulin resistance stimulate PKC isoforms and other stress kinases to phosphorylate IRS1/2 and PI3K and inhibit only the IRS/PI3K/Akt pathway. In contrast, insulin’s stimulation of the SOS/Grb2/MAPK pathway is unaffected or even enhanced. The selective loss of insulin’s actions via the IRS/PI3K/Akt pathway causes the reduction of insulin’s antiatherosclerotic action and contributes to the acceleration of atherosclerosis and other cardiovascular pathologies in diabetes. PTEN, phosphatase and tensin homolog; ROS, reactive oxygen species.
Recently, more information has become available on the biochemical understanding of the development of selective insulin resistance. Multiple pathophysiological stimuli such as angiotensin, oxidants, inflammatory cytokines, hyperglycemia, and FFAs have been shown to cause selective inhibition of the IRS/PI3K/Akt pathway and even enhance the MAPK cascade (Fig. 3).
These pathophysiological stimuli impaired insulin action at multiple levels including the IR, IRS1/2, and PI3K level. Decreased expression or increased degradation of the IR and IRS1/2 due to pathologically increased posttranslational modifications such as glycosylation and phosphorylation has been reported (55–57). At the biochemical level, insulin signaling can be inhibited by increasing serine/threonine phosphorylation of the IR or IRS1 (58), which reduces insulin-induced tyrosine phosphorylation of IRS1 and suppresses the interaction of p85α of PI3K, resulting in decreased Akt phosphorylation and activation. Our study showed that Thr86 of p85α/PI3K is phosphorylated by angiotensin II or PKCα, -β, and -δ activation; this inhibits its association with IRS1 and decreases activation of the insulin- or VEGF-induced Akt/eNOS cascade (59). These serine/threonine phosphorylation sites have a negative effect on insulin signaling at Ser24, Ser267, Ser270, Ser307, Ser332, Ser357, Ser522, Ser612, Ser632/635, Ser662, and Ser1099/1100 on IRS1. IRS2 has been recognized as an important mediator of insulin signaling and actions in ECs as well (60). We have reported that there are multiple serine/threonine phosphorylation sites at Thr348 and at Ser488 and Ser484 on IRS2 that can be induced by PKC activation (61). This study showed that phosphorylated Ser303 and Ser675 on IRS2 by angiotensin II or PKCβ2 activation inhibits insulin-induced tyrosine phosphorylation of IRS2 and Akt/eNOS activation. These phosphorylation sites and the negative regulation of insulin signaling via serine/threonine phosphorylation of IRS1/2 were induced by extracellular stimuli such as angiotensin II, FFAs, or the TNFα intrinsic pathway involving PKC, NF-κB, and JNK pathways (62–64). In contrast, MAPK activation may also induce serine phosphorylation of IRS1 and turn off insulin signaling, suggesting that MAPK activation may also contribute to insulin resistance (65).
In insulin resistance or deficiency and in diabetes, there is a loss of insulin’s antiatherogenic actions via the IRS/PI3K/Akt cascade, which diminishes the expression of human HO-1 and the activation of eNOS and enhances VCAM-1 expression, all of which leads to the acceleration of atherosclerosis. Selective loss of the IRS/Akt pathway can decrease VEGF expression in the myocardium, which impairs collateral vessel formation in response to hypoxia and causes a poor outcome from an acute coronary occlusion (53). In contrast, the activated MAPK pathway has proatherosclerotic actions, as it increases the expressions of PAI-1 and ET-1 (Fig. 3).
Rodent models of Atherosclerosis Support Selective Insulin Resistance for the Development of Atherosclerosis
Several reports have shown that the deletion of Akt in the endothelium increased atherosclerosis, whereas the deletion of FoxO decreased atherosclerosis (66,67). However, these studies did not directly address the effect of insulin on the endothelium and its actions on atherosclerosis. We have directly studied the effect of deleting the IR in ECs and its effect on atherosclerosis on ApoE−/− mice. IRs were specifically deleted in ApoE−/− mice in order to test, directly, whether the deletion of insulin action in the endothelium can affect systemic insulin sensitivity and atherosclerosis. We have found that mice devoid of the IR (EIRAKO), specifically in the endothelium, did not differ from wild-type mice regarding insulin sensitivity, glucose intolerance, plasma lipids, or blood pressure (22). However, the severity of atherosclerotic lesions was more than twofold higher in EIRAKO mice. The potential mechanism for the increased atherosclerosis was related to the loss of insulin’s inhibitory actions of VCAM-1. Insulin decreased the expression of VCAM-1 at physiological levels in ECs via the IRS/PI3K/Akt pathway. Thus, in the EIRAKO mice, VCAM-1 expression was increased in the artery, which enhanced the binding and uptake of monocytes, elevating inflammatory cells in the atherosclerotic plaque (67). This finding, for the first time, clearly demonstrated that the overall insulin action at physiological levels has antiatherogenic actions, therefore suggesting that enhancing insulin action on the endothelium will be able to decrease atherosclerosis in diabetic or insulin-resistant states.
We propose that selective insulin resistance in the endothelium can be induced by diabetes with the elevation of glucose, FFAs, and other inflammatory cytokines. These conditions will cause elevation of diacylglycerol to activate stress kinase and PKC to phosphorylate serine or threonine in IRS1/2 and PI3K and inhibit their activities, causing selective insulin resistance and increasing atherosclerosis (Fig. 3). There is supportive evidence to show that PKC activation, especially of the β isoform, can enhance atherosclerosis, as the use of a selective PKC β isoform inhibitor was found to decrease atherosclerosis in ApoE−/− mice (68). Again, to test directly how PKCβ activation in the endothelium can affect atherosclerosis in insulin-resistant and diabetic states, we overexpressed the PKCβ2 isoform in the endothelium using the vascular EC cadherin promotor on the ApoE−/− mice. When placed on a high-fat diet, transgenic PKCβ ApoE−/− mice did not differ from ApoE−/− mice regarding systemic insulin sensitivity, plasma lipids, or blood pressure. However, insulin actions in the endothelium and femoral artery were selectively impaired with respect to pAkt and eNOS activation. Other proatherogenic actions were also increased such as leukocyte binding to ECs and the expression of ET-1. The severity of atherosclerosis in the aorta from the transgenic PKCβ ApoE−/− mice was significantly increased, as measured by the content of fat, VSMCs, macrophages, and extracellular matrix in the arterial walls (69).
These studies have clearly demonstrated that IRs on the endothelium can mediate multiple actions through at least two major pathways involving either the IRS/PI3K/Akt or the Grb/Shc/MAPK cascade, with the former mediating more antiatherogenic and the latter more proatherogenic actions. In obesity, insulin resistance, and diabetes, there is a selective loss of insulin action via IRS/PI3K/Akt pathways, possibly through PKC activation resulting in the selective loss of insulin’s antiatherogenic actions. These findings suggest that enhancing insulin actions in the endothelium specifically by targeting the IRS/PI3K/Akt pathway can decrease the accelerated atherosclerosis, fibrosis, poor collateral formation, and cardiomyopathy observed in people with insulin resistance and diabetes. We believe that there are multiple therapeutic sites of intervention possible on the endothelium that can specifically enhance insulin’s actions without affecting systemic metabolism in order to decrease atherosclerosis in people with diabetes and insulin resistance.
Article Information
Funding. The authors are grateful for the support of National Institutes of Health (NIH) grant 5P30-DK-036836. G.L.K. is supported by NIH grant R01-DK-053105 and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant 1DP3-DK-094333-01. Q.L. was supported by the American Diabetes Association Mentor-Based Postdoctoral Fellowship Award.
The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
References
- 1.Rask-Madsen C, King GL. Vascular complications of diabetes: mechanisms of injury and protective factors. Cell Metab 2013;17:20–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kitada M, Zhang Z, Mima A, King GL. Molecular mechanisms of diabetic vascular complications. J Diabetes Investig 2010;1:77–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med 2000;342:381–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel A, MacMahon S, Chalmers J, et al.; ADVANCE Collaborative Group . Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–2572 [DOI] [PubMed] [Google Scholar]
- 5.Gerstein HC, Miller ME, Ismail-Beigi F, et al.; ACCORD Study Group . Effects of intensive glycaemic control on ischaemic heart disease: analysis of data from the randomised, controlled ACCORD trial. Lancet 2014;384:1936–1941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duckworth W, Abraira C, Moritz T, et al.; VADT Investigators . Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129–139 [DOI] [PubMed] [Google Scholar]
- 7.Laakso M. Cardiovascular disease in type 2 diabetes from population to man to mechanisms: the Kelly West Award Lecture 2008. Diabetes Care 2010;33:442–449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Livingstone SJ, Looker HC, Hothersall EJ, et al. Risk of cardiovascular disease and total mortality in adults with type 1 diabetes: Scottish registry linkage study. PLoS Med 2012;9:e1001321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature 2011;473:317–325 [DOI] [PubMed] [Google Scholar]
- 10.Després JP, Lamarche B, Mauriège P, et al. Hyperinsulinemia as an independent risk factor for ischemic heart disease. N Engl J Med 1996;334:952–957 [DOI] [PubMed] [Google Scholar]
- 11.de Ferranti SD, de Boer IH, Fonseca V, et al. Type 1 diabetes mellitus and cardiovascular disease: a scientific statement from the American Heart Association and American Diabetes Association. Diabetes Care 2014;37:2843–2863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gerstein HC, Bosch J, Dagenais GR, et al.; ORIGIN Trial Investigators . Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med 2012;367:319–328 [DOI] [PubMed] [Google Scholar]
- 13.Rask-Madsen C, Buonomo E, Li Q, et al. Hyperinsulinemia does not change atherosclerosis development in apolipoprotein E null mice. Arterioscler Thromb Vasc Biol 2012;32:1124–1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.King GL, Johnson SM. Receptor-mediated transport of insulin across endothelial cells. Science 1985;227:1583–1586 [DOI] [PubMed] [Google Scholar]
- 15.Rask-Madsen C, King GL. Mechanisms of disease: endothelial dysfunction in insulin resistance and diabetes. Nat Clin Pract Endocrinol Metab 2007;3:46–56 [DOI] [PubMed] [Google Scholar]
- 16.Jialal I, Crettaz M, Hachiya HL, et al. Characterization of the receptors for insulin and the insulin-like growth factors on micro- and macrovascular tissues. Endocrinology 1985;117:1222–1229 [DOI] [PubMed] [Google Scholar]
- 17.Soos MA, Siddle K. Immunological relationships between receptors for insulin and insulin-like growth factor I. Evidence for structural heterogeneity of insulin-like growth factor I receptors involving hybrids with insulin receptors. Biochem J 1989;263:553–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Virkamäki A, Ueki K, Kahn CR. Protein-protein interaction in insulin signaling and the molecular mechanisms of insulin resistance. J Clin Invest 1999;103:931–943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Geraldes P, Yagi K, Ohshiro Y, et al. Selective regulation of heme oxygenase-1 expression and function by insulin through IRS1/phosphoinositide 3-kinase/Akt-2 pathway. J Biol Chem 2008;283:34327–34336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jiang ZY, He Z, King BL, et al. Characterization of multiple signaling pathways of insulin in the regulation of vascular endothelial growth factor expression in vascular cells and angiogenesis. J Biol Chem 2003;278:31964–31971 [DOI] [PubMed] [Google Scholar]
- 21.Kuboki K, Jiang ZY, Takahara N, et al. Regulation of endothelial constitutive nitric oxide synthase gene expression in endothelial cells and in vivo : a specific vascular action of insulin. Circulation 2000;101:676–681 [DOI] [PubMed] [Google Scholar]
- 22.Rask-Madsen C, Li Q, Freund B, et al. Loss of insulin signaling in vascular endothelial cells accelerates atherosclerosis in apolipoprotein E null mice. Cell Metab 2010;11:379–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oliver FJ, de la Rubia G, Feener EP, et al. Stimulation of endothelin-1 gene expression by insulin in endothelial cells. J Biol Chem 1991;266:23251–23256 [PubMed] [Google Scholar]
- 24.Nagai M, Kamide K, Rakugi H, et al. Role of endothelin-1 induced by insulin in the regulation of vascular cell growth. Am J Hypertens 2003;16:223–228 [DOI] [PubMed] [Google Scholar]
- 25.Schneider DJ, Absher PM, Ricci MA. Dependence of augmentation of arterial endothelial cell expression of plasminogen activator inhibitor type 1 by insulin on soluble factors released from vascular smooth muscle cells. Circulation 1997;96:2868–2876 [DOI] [PubMed] [Google Scholar]
- 26.Ward CW, Gough KH, Rashke M, Wan SS, Tribbick G, Wang J. Systematic mapping of potential binding sites for Shc and Grb2 SH2 domains on insulin receptor substrate-1 and the receptors for insulin, epidermal growth factor, platelet-derived growth factor, and fibroblast growth factor. J Biol Chem 1996;271:5603–5609 [DOI] [PubMed] [Google Scholar]
- 27.Jiang ZY, Lin YW, Clemont A, et al. Characterization of selective resistance to insulin signaling in the vasculature of obese Zucker (fa/fa) rats. J Clin Invest 1999;104:447–457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barrett EJ, Liu Z. The endothelial cell: an “early responder” in the development of insulin resistance. Rev Endocr Metab Disord 2013;14:21–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang H, Wang AX, Barrett EJ. Caveolin-1 is required for vascular endothelial insulin uptake. Am J Physiol Endocrinol Metab 2011;300:E134–E144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang H, Wang AX, Aylor K, Barrett EJ. Caveolin-1 phosphorylation regulates vascular endothelial insulin uptake and is impaired by insulin resistance in rats. Diabetologia 2015;58:1344–1353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Montagnani M, Chen H, Barr VA, Quon MJ. Insulin-stimulated activation of eNOS is independent of Ca2+ but requires phosphorylation by Akt at Ser(1179). J Biol Chem 2001;276:30392–30398 [DOI] [PubMed] [Google Scholar]
- 32.King GL, Buzney SM, Kahn CR, et al. Differential responsiveness to insulin of endothelial and support cells from micro- and macrovessels. J Clin Invest 1983;71:974–979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilhelm K, Happel K, Eelen G, et al. FOXO1 couples metabolic activity and growth state in the vascular endothelium. Nature 2016;529:216–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang PL. eNOS, metabolic syndrome and cardiovascular disease. Trends Endocrinol Metab 2009;20:295–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Palmer RM, Ferrige AG, Moncada S. Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature 1987;327:524–526 [DOI] [PubMed] [Google Scholar]
- 36.Furchgott RF, Zawadzki JV. The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature 1980;288:373–376 [DOI] [PubMed] [Google Scholar]
- 37.Wang H, Wang AX, Liu Z, Chai W, Barrett EJ. The trafficking/interaction of eNOS and caveolin-1 induced by insulin modulates endothelial nitric oxide production. Mol Endocrinol 2009;23:1613–1623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Muniyappa R, Montagnani M, Koh KK, Quon MJ. Cardiovascular actions of insulin. Endocr Rev 2007;28:463–491 [DOI] [PubMed] [Google Scholar]
- 39.King GL, Goodman AD, Buzney S, Moses A, Kahn CR. Receptors and growth-promoting effects of insulin and insulinlike growth factors on cells from bovine retinal capillaries and aorta. J Clin Invest 1985;75:1028–1036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Begum N, Sandu OA, Duddy N. Negative regulation of rho signaling by insulin and its impact on actin cytoskeleton organization in vascular smooth muscle cells: role of nitric oxide and cyclic guanosine monophosphate signaling pathways. Diabetes 2002;51:2256–2263 [DOI] [PubMed] [Google Scholar]
- 41.Takeya K, Wang X, Sutherland C, et al. Involvement of myosin regulatory light chain diphosphorylation in sustained vasoconstriction under pathophysiological conditions. J Smooth Muscle Research 2014;50:18–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yokota T, Ma RC, Park JY, et al. Role of protein kinase C on the expression of platelet-derived growth factor and endothelin-1 in the retina of diabetic rats and cultured retinal capillary pericytes. Diabetes 2003;52:838–845 [DOI] [PubMed] [Google Scholar]
- 43.Hopfner RL, Hasnadka RV, Wilson TW, McNeill JR, Gopalakrishnan V. Insulin increases endothelin-1-evoked intracellular free calcium responses by increased ET(A) receptor expression in rat aortic smooth muscle cells. Diabetes 1998;47:937–944 [DOI] [PubMed] [Google Scholar]
- 44.Fujita N, Furukawa Y, Du J, et al. Hyperglycemia enhances VSMC proliferation with NF-κB activation by angiotensin II and E2F-1 augmentation by growth factors. Mol Cell Endocrinol 2002;192:75–84 [DOI] [PubMed] [Google Scholar]
- 45.Geraldes P, Hiraoka-Yamamoto J, Matsumoto M, et al. Activation of PKC-δ and SHP-1 by hyperglycemia causes vascular cell apoptosis and diabetic retinopathy. Nat Med 2009;15:1298–1306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mita T, Azuma K, Goto H, et al. IRS-2 deficiency in macrophages promotes their accumulation in the vascular wall. Biochem Biophys Res Commun 2011;415:545–550 [DOI] [PubMed] [Google Scholar]
- 47.Han S, Liang CP, DeVries-Seimon T, et al. Macrophage insulin receptor deficiency increases ER stress-induced apoptosis and necrotic core formation in advanced atherosclerotic lesions. Cell Metab 2006;3:257–266 [DOI] [PubMed] [Google Scholar]
- 48.Abel ED, O’Shea KM, Ramasamy R. Insulin resistance: metabolic mechanisms and consequences in the heart. Arterioscler Thromb Vasc Biol 2012;32:2068–2076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jia G, DeMarco VG, Sowers JR. Insulin resistance and hyperinsulinaemia in diabetic cardiomyopathy. Nat Rev Endocrinol 2016;12:144–153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gray S, Kim JK. New insights into insulin resistance in the diabetic heart. Trends Endocrinol Metab 2011;22:394–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Belke DD, Betuing S, Tuttle MJ, et al. Insulin signaling coordinately regulates cardiac size, metabolism, and contractile protein isoform expression. J Clin Invest 2002;109:629–639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.He Z, Opland DM, Way KJ, et al. Regulation of vascular endothelial growth factor expression and vascularization in the myocardium by insulin receptor and PI3K/Akt pathways in insulin resistance and ischemia. Arterioscler Thromb Vasc Biol 2006;26:787–793 [DOI] [PubMed] [Google Scholar]
- 53.Chou E, Suzuma I, Way KJ, et al. Decreased cardiac expression of vascular endothelial growth factor and its receptors in insulin-resistant and diabetic states: a possible explanation for impaired collateral formation in cardiac tissue. Circulation 2002;105:373–379 [DOI] [PubMed] [Google Scholar]
- 54.Khamaisi M, Katagiri S, Keenan H, et al. PKCδ inhibition normalizes the wound-healing capacity of diabetic human fibroblasts. J Clin Invest 2016;126:837–853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sun XJ, Goldberg JL, Qiao LY, Mitchell JJ. Insulin-induced insulin receptor substrate-1 degradation is mediated by the proteasome degradation pathway. Diabetes 1999;48:1359–1364 [DOI] [PubMed] [Google Scholar]
- 56.Hirashima Y, Tsuruzoe K, Kodama S, et al. Insulin down-regulates insulin receptor substrate-2 expression through the phosphatidylinositol 3-kinase/Akt pathway. J Endocrinol 2003;179:253–266 [DOI] [PubMed] [Google Scholar]
- 57.Haruta T, Uno T, Kawahara J, et al. A rapamycin-sensitive pathway down-regulates insulin signaling via phosphorylation and proteasomal degradation of insulin receptor substrate-1. Mol Endocrinol 2000;14:783–794 [DOI] [PubMed] [Google Scholar]
- 58.White MF. IRS proteins and the common path to diabetes. Am J Physiol Endocrinol Metab 2002;283:E413–E422 [DOI] [PubMed] [Google Scholar]
- 59.Maeno Y, Li Q, Park K, et al. Inhibition of insulin signaling in endothelial cells by protein kinase C-induced phosphorylation of p85 subunit of phosphatidylinositol 3-kinase (PI3K). J Biol Chem 2012;287:4518–4530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kubota T, Kubota N, Kumagai H, et al. Impaired insulin signaling in endothelial cells reduces insulin-induced glucose uptake by skeletal muscle. Cell Metab 2011;13:294–307 [DOI] [PubMed] [Google Scholar]
- 61.Park K, Li Q, Rask-Madsen C, et al. Serine phosphorylation sites on IRS2 activated by angiotensin II and protein kinase C to induce selective insulin resistance in endothelial cells. Mol Cell Biol 2013;33:3227–3241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Boden G. Role of fatty acids in the pathogenesis of insulin resistance and NIDDM. Diabetes 1997;46:3–10 [PubMed] [Google Scholar]
- 63.Nakatani Y, Kaneto H, Kawamori D, et al. Modulation of the JNK pathway in liver affects insulin resistance status. J Biol Chem 2004;279:45803–45809 [DOI] [PubMed] [Google Scholar]
- 64.Solinas G, Naugler W, Galimi F, Lee MS, Karin M. Saturated fatty acids inhibit induction of insulin gene transcription by JNK-mediated phosphorylation of insulin-receptor substrates. Proc Natl Acad Sci U S A 2006;103:16454–16459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gual P, Grémeaux T, Gonzalez T, Le Marchand-Brustel Y, Tanti JF. MAP kinases and mTOR mediate insulin-induced phosphorylation of insulin receptor substrate-1 on serine residues 307, 612 and 632. Diabetologia 2003;46:1532–1542 [DOI] [PubMed] [Google Scholar]
- 66.Fernández-Hernando C, Ackah E, Yu J, et al. Loss of Akt1 leads to severe atherosclerosis and occlusive coronary artery disease. Cell Metab 2007;6:446–457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tsuchiya K, Tanaka J, Shuiqing Y, et al. FoxOs integrate pleiotropic actions of insulin in vascular endothelium to protect mice from atherosclerosis. Cell Metab 2012;15:372–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kong L, Shen X, Lin L, et al. PKCβ promotes vascular inflammation and acceleration of atherosclerosis in diabetic ApoE null mice. Arterioscler Thromb Vasc Biol 2013;33:1779–1787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li Q, Park K, Li C, et al. Induction of vascular insulin resistance and endothelin-1 expression and acceleration of atherosclerosis by the overexpression of protein kinase C-β isoform in the endothelium. Circ Res 2013;113:418–427 [DOI] [PMC free article] [PubMed] [Google Scholar]