Abstract
Tanshinone IIA is the active compound isolated from Salvia miltiorrhiza bunge, which is a traditional Chinese medicine known as Danshen. The aim of the present study was to assess the effect of Tanshinone IIA on the regulation of lipid metabolism in the livers of hyperlipidemic rats and the underlying molecular events. An in vivo model of hyperlipidemia was established in rats, with the animals receiving a daily dose of Tanshinone IIA. The serum lipid profiles were analyzed using an automatic biochemical analyzer, and the histopathological alterations and lipid deposition in liver tissue were assessed using hematoxylin and eosin staining, and oil red O staining, respectively. The mRNA expression levels of microRNA (miR)-33a, ATP-binding cassette transporter (ABC)A1, ABCG1, sterol regulatory element-binding protein 2 (SREBP-2), proprotein convertase subtilisin/kexin type 9 (Pcsk9) and low-density lipoprotein receptor (LDL-R) in liver tissues were measured using reverse transcription-quantitative polymerase chain reaction, and the protein expression levels of ABCA1, ABCG1, SREBP-2, Pcsk9, and LDL-R were analyzed using western blotting. Tanshinone IIA reduced lipid deposition and improved histopathology in the rat liver tissue, however, did not alter the lipid profile in rat serum. In addition, Tanshinone IIA treatment suppressed the expression of miR-33a, whereas the protein expression levels of ABCA1, SREBP-2, Pcsk9 in addition to LDL-R mRNA and protein were upregulated. In conclusion, the present study indicated that Tanshinone IIA attenuated lipid deposition in the livers of hyperlipidemic rats and modulated the expression of miR-33a and SREBP-2/Pcsk9 signaling pathway proteins.
Keywords: hyperlipidemia, Tanshinone IIA, miR-33a, SREBP-2 Pcsk9
Introduction
Hyperlipidemia refers to abnormally elevated levels of lipids or lipoproteins in the bloodstream, and is a significant risk factor associated with numerous diseases, including ventricular remodeling, cardiac hypertrophy and cardiac dysfunction (1). A previous study demonstrated that hyperlipidemia has a direct association with an increase in the number and size of atheromatous plaques and thus has been considered as a contributor to atherosclerosis (2). Patients with hyperlipidemia usually have higher levels of total cholesterol (TC), triglycerides (TG), and low-density lipoprotein cholesterol (LDL-C), however, relatively lower levels of high-density lipoprotein cholesterol (HDL-C) compared with healthy controls (3). High plasma TC, TG or LDL-C levels or low plasma HDL-C levels may result in damage to vascular endothelial cells and initiates atherosclerosis (4). By contrast, HDL-C has been generally accepted to serve a protective role in the suppression of the formation of atherosclerosis (5). Thus, clinical control of hyperlipidemia may prevent atherosclerosis and cardiovascular diseases.
Tanshinone IIA is a pharmacologically active compound isolated from Salvia miltiorrhiza bunge, and is known as Danshen in traditional Chinese medicine. Tanshinone IIA has been used historically in traditional Chinese medicine to prevent and treat cardiovascular diseases in Asian countries, due to its putative cardioprotective and anti-atherosclerotic effects. Numerous experimental and clinical studies have indicated that Tanshinone IIA possesses a variety of biological activities, including, but not limited to, vasodilatory, anti-atherosclerosis, anti-oxidation, anti-inflammatory, anti-hyperlipidemic and anti-adipogenic effects (6–9). However, the underlying mechanisms of Tanshinone IIA activity remain to be determined. In a previous study, Tanshinone IIA treatment increased HDL-C level and reduced LDL-C levels in C57BL/6J mice fed with a high fat-diet (9). Additionally, Tanshinone IIA has been shown to reduce the formation of atherosclerotic plaques without a significant effect on alterations in the lipid profile (6,10). A previous study indicated that Tanshinone IIA served an anti-atherosclerotic effect via the inhibition of Toll-like receptor 4 and tumor necrosis factor-α expression in EA.hy926 cells following stimulation with lipopolysaccharides (11). Additionally, protective effects of Tanshinone IIA have been indicated on apoptosis induced by H2O2 in EA.hy926 cells (12).
Increasingly, evidence indicates that sterol regulatory element-binding protein 2 (SREBP-2) and LDL receptor (LDL-R) are transcription factors involved in the regulation of cholesterol metabolism (13–15). Furthermore, there is a binding site for SREBP localized in the promoter region of proprotein convertase subtilisin/kexin type 9 (Pcsk9) (16) and thus, SREBP regulates expression of Pcsk9 at the transcriptional level. Reductions in hepatic cholesterol levels are able to activate the SREBP signaling pathway to upregulate the expression of Pcsk9 and LDL-R simultaneously (15,17), and in turn, increase the levels of LDL particles by reducing LDL-R (18). Conversely, inhibition of SREBP expression in the liver has been shown to reduce the levels of Pcsk9 and LDL-R (19). In addition, a previous study indicated that microRNA (miR)-33, an intronic miRNA residing in the SREBP-2 gene, serves a crucial role in the regulation of HDL metabolism, cholesterol efflux and fatty acid β-oxidation through the modulation of the expression of the ATP-binding cassette transporter A1 (ABCA1) and G1 (ABCG1) (20–23). However, in mice, but not in humans, miR-33 overexpression has been observed to reduce cholesterol efflux to nascent HDL (24). Thus, inhibition of endogenous miR-33 levels may possess therapeutic function to upregulate HDL levels by repressing ABCA1 and ABCG1 expression (25,26). Thus, in the present study, experiments were conducted to elucidate the potential mechanisms of Tanshinone IIA activity in vivo on lipid metabolism and the underlying molecular events.
Materials and methods
Animals and rat hyperlipidemia model
The study was approved by the ethics committee of Liaoning University of Traditional Chinese Medicine experimental animal ethics committee (Shenyang, China). A total of 90 male Sprague-Dawley rats (6 weeks old, 200±10 g) were obtained from Vital River Laboratories Co., Ltd. (Beijing, China) and housed in a climate-controlled environment (22±1°C, humidity at 50±5%) with a 12/12 h light/dark cycle and ad libitum access to water. The rats were randomly divided into control, hyperlipidemia (HLP) and Tanshinone IIA treatment (TAN) groups, with 30 rats in each group. The control rats were fed with a regular balanced diet, while the HLP and TAN groups were fed with a high-fat diet (6% sucrose, 1% sodium glutamate, 5% yolk powder, 8% peanut oil, 1.5% cholesterol, 0.4% methylthiouracil, 0.2% cholate and 73.3% regular balanced diet) for 3 months. Following this, the TAN group received 1.2 ml of sodium Tanshinone IIA sulfonate (Shanghai No. 1 Biochemical & Pharmaceutical Co., Ltd., Shanghai, China) at a dose of 10 mg/kg by daily intraperitoneal injection for an additional 3 months, whereas the control and HLP groups received the same amount of phosphate-buffered saline (PBS) for the same period of time.
Collection of sera and lipid profiling
Following the treatment process, the rats (n=6) were anesthetized with 10% chloral hydrate and aortic blood was collected for 2 h at room temperature. The blood samples were then centrifuged at 4°C, 300 × g for 20 min, and the serum was collected and stored at −80°C until use. For the lipid profiling, the serum samples were analyzed using an automatic TBA-120FR biochemical analyzer (Toshiba Corporation, Tokyo, Japan). Levels of TG, TC, HDL-C and LDL-C in the serum were measured using the corresponding kits (all from Sichuan Maker Biotechnology Co., Ltd., Sichuan, China).
Hematoxylin and eosin (H&E) staining of liver tissues
Liver tissues were collected (n=3), fixed in 4% formaldehyde for 24 h at 4°C, dehydrated through an ethanol series (70–100%), cleared in xylene and embedded in paraffin. The tissue was cut into 5 µm thick sections and dewaxed in xylene, rehydrated through a 70–100% ethanol series, and then stained with hematoxylin, differentiated in 70% acid ethanol and further stained with eosin. Subsequently, the tissue sections were dehydrated through 70–100% ethanol, cleared in xylene, and mounted using Permount Mounting Medium (BioWorld Technology, Inc., Atlanta, Georgia, USA). The tissue sections were photographed using a BX51-WIF light microscope linked to a digital charge-coupled device (CCD) camera (Olympus Corporation, Tokyo, Japan).
Oil Red O staining of liver tissues
For Oil Red O staining, frozen sections were prepared (6 µm) from liver tissue samples (n=3) and fixed in 50% ethanol. Subsequently, sections were stained with Oil Red O (Beijing Noble Rider Technology Co., Ltd., Beijing, China) for 8 min and differentiated with 50% ethanol, rinsed with tap water, and counterstained with hematoxylin. Following a final rinse in tap water, the sections were mounted with glycerin jelly. The sections were photographed using the light microscope linked to a digital CCD camera (Olympus Corporation).
Immunohistochemistry
The expression of SREBP-2, Pcsk9, and LDL-R proteins was assessed in paraffin-embedded liver tissues. In brief, tissue sections were dewaxed in xylene, rehydrated through a 70–100% ethanol series, and then incubated in 0.3% H2O2 in PBS to block endogenous peroxidase activity and 10% skim milk in PBS to block non-specific protein binding of the secondary antibodies. Subsequently, the sections were incubated with primary polyclonal rabbit anti-rat SREBP-2 (cat no. 980594w), LDL-R (cat no. YSLS15w), PCSK9 (cat no. bs-6060R) antibodies (all from BIOSS, Beijing, China). at 4°C overnight, then washed with PBS three times and incubated with a horseradish peroxidase (HRP)-conjugated goat anti-rabbit secondary antibody (1:1,000; 36J00180; Beijing Dingguo Changsheng Biotechnology Co., Ltd., Beijing, China) at room temperature for 1 h. The peroxidase activity was detected using 3, 3′-diaminobenzidine tetrahydrochloride solution. Following washing and counterstaining with hematoxylin, the sections were mounted using AquaMount [Hyde Entrepreneurship (Beijing) Biological Technology Co., Ltd., Beijing, China] and photographed and scored using the light microscope linked to a digital CCD camera (Olympus Corporation). The area of positive expression of each section was observed at the low magnification (×10), then 4 randomly selected fields were captured at high magnification (×40). Exposure conditions were consistent. Images were semi-quantitatively analysed using Image-Pro Plus software (Media Cybernetics, Inc., Rockville, MD, USA). The the integrated optical density of each image was measured and an average from 4 images was calculated for each section.
RNA isolation and reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was isolated from liver tissue (n=3) using a TRIzol reagent (Takara Biotechnology Co., Ltd., Dalian, China) and reverse transcribed into cDNA using the miScript II RT kit (Qiagen GmbH, Hilden, Germany), according to the manufacturer's instructions. To assess the levels of miR-33, total RNA was isolated using a miRNeasyMini kit (Qiagen GmbH), amplified using specific primers to miR-33 and normalized to small U6 RNA (Qiagen GmbH). The miR-33 transcripts were amplified as follows: Initial denaturation at 94°C for 10 min; 35 cycles of denaturation at 94°C for 1 min, annealing at 55°C for 15 sec and extension at 70°C for 15 sec; and a final extension step at 70°C for 5 min. To measure the levels of gene transcripts, the following rat primers were used: LDL-R, foward 5′-GGGTTCTTGTCCATCTTCC-3′ and reverse 5′-ACTGGGTTGTCAAAGTTTATG-3′; SREBP-2, forward 5′-GTGGGCTGAGAAGAAAGATG-3′ and reverse 5′-CCAGAGGCAGAAAGGAGA C-3′; and glyceraldehyde 3-phosphate dehydrogenase (GAPDH), forward 5′-TGTGTCCGTCGTGGATCTGA-3′ and reverse 5′-TTGCTGTTGAAGTCGCAGGAG-3′. All primers were designed using Premier 5.0 software (PREMIER Biosoft, Palo Alto, CA, USA) and custom-synthesized by Takara Biotechnology Co., Ltd. RT-qPCR was performed in triplicate using a SYBR Green Master Mix (Takara Biotechnology Co., Ltd.) in an ABI 7500 PCR Sequence Detector (Applied Biosystems; Thermo Fisher Scientific, Inc., Waltham, MA, USA). The transcripts were amplified by 40 cycles of 95° for 2 min, 95°C for 30 sec and 60°C for 30 sec. The gene transcripts were normalized to GAPDH. The RNA levels measured by RT-qPCR were quantatified used the 2−ΔΔCq method.
Protein extraction and western blotting
Total cellular protein was extracted from rat liver tissues (n=3) using radioimmunoprecipitation assay lysis buffer (Beyotime Institute of Biotechnology, Shanghai, China) and the protein concentration was measured using Bicinchoninic Acid Protein Assay kit (Beijing Dingguo Changsheng Biotechnology Co., Ltd., Beijing, China). To measure the expression levels of ABCA1, ABCG1, SREBP-2, Pcsk9 and LDL-R proteins, 80 µg of protein samples were separated on a 10% sodium dodecyl sulfate-polyacrylamide electrophoresis gel (Beijing Solarbio Science and Technology Co., Ltd., Beijing, China) and transferred onto polyvinylidene fluoride membranes (EMD Millipore, Billerica, MA, USA). The membranes were blocked with 5% skin, high protein, high calcium milk powder (Inner Mongolia Yili Industrial Group Co., Ltd., Hohhot, China). The membranes were then incubated overnight at 37°C with rabbit anti-rat SREBP-2, LDL-R, PCSK9, ABCA1 (cat no. bs-1627R), ABCG1 (cat no. bs-1231R) and GAPDH (No. bs-2188R) primary antibodies (all 1:300; BIOSS), and then with the HRP-conjugated goat anti-rabbit secondary antibody (1:200) for 1 h at 37°C. Protein bands were visualized using an enhanced chemiluminescence kit (Thermo Fisher Scientific, Inc.) and exposed to X-ray films (Kodak, Rochester, NY, USA). Protein expression levels were normalized to GAPDH levels.
Statistical analysis
Data were expressed as the mean ± standard deviation. Comparisons between the group values were performed by one-way analysis of variance. Tukey's test was used for multiple comparisons between the groups. P<0.05 was considered to indicate a statistically significant difference.
Results
Tanshinone IIA alterations in lipid levels in sera and lipid deposition in the liver
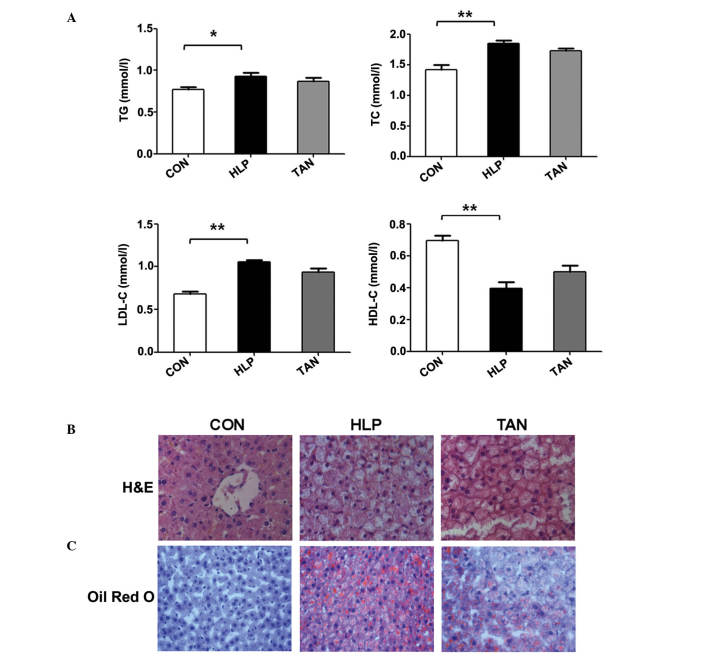
In the present study, an in vivo experiment was performed to assess the effects of Tanshinone IIA on alterations in the lipid levels in sera and lipid deposition in the liver. The results indicated that compared with the control rats, the HLP rats had significantly higher serum levels of TG, TC and LDL-C, however, significantly lower serum levels of HDL-C (P<0.05 or P<0.01). Compared with the HLP group, the TAN group did not exhibit altered lipid profiles (Fig. 1A).
Figure 1.
Tanshinone IIA alterations in the lipid levels in sera and lipid deposition in the liver. (A) TG, TC, LDL-C and HDL-C serum lipid levels. (B) H&E staining indicating the alterations in the liver cells, such as lipid droplets. (C) Oil red O staining showing the lipid droplets in the liver tissue. Data are presented as the mean ± standard deviation. *P<0.05, **P<0.01 vs. CON group. TG, triglycerides; TC, total cholesterol; LDL-C, low-density lipoprotein-cholesterol; HDL-C, high-density lipoprotein-cholesterol; H&E, hematoxylin and eosin; CON, control; HLP, high lipid diet-fed rats; TAN, Tanshinone IIA treatment of high lipid diet-fed rats.
Furthermore, H&E stained liver sections indicated that the hepatic cord is arranged normally in the control rats and that hepatocytes display normal morphology, with a large round nucleus in the centre and little accumulation of lipid droplets in the cytoplasm. There was no infiltration of inflammatory cells in the lobules. However, in the HLP rats, severe hepatic steatosis was observed, and hepatocytes were swollen and round, and the cytoplasm was loose and contained large lipid droplets (Fig. 1B). In a number of hepatocytes, the nucleus was located in the periphery, and lipid vacuoles of varying size and inflammatory cells were observed. In the TAN rats, the level of hepatic steatosis, the number of lipid vacuoles and hepatocyte size were all reduced (Fig. 1B). The oil red O staining indicated that the hepatocytes in the HLP rats had significantly greater numbers of lipid droplets compared with the control rats, whereas the number of lipid droplets in hepatocytes was significantly reduced in the TAN rats (Fig. 1C).
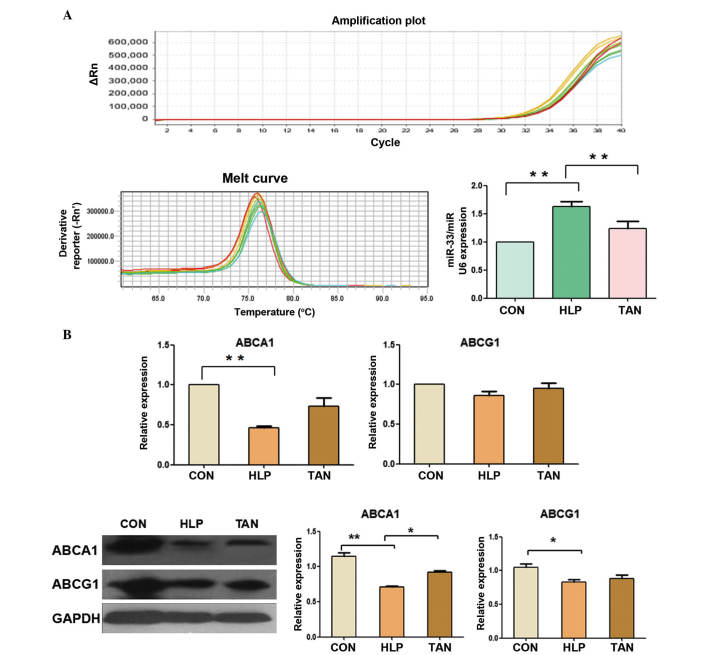
Tanshinone IIA regulation of miR-33a, ABCA1 and ABCG1 expression in the liver
The expression levels of miR-33a in the livers of HLP rats was significantly upregulated compared with the control rats (P<0.01), whereas the expression levels of miR-33a were significantly reduced in the TAN rats (P<0.01; Fig. 2A), indicating that Tanshinone IIA was able to control miR-33a expression in the rat liver.
Figure 2.
Tanshinone IIA regulation of miR-33a, ABCA1 and ABCG1 expression in the liver. (A) RT-qPCR measurement of miR-33a expression in rat liver tissue. (B) RT-qPCR and western blotting analyses of ABCA1 and ABCG1 expression in liver tissue. Data are presented as the mean ± standard deviation. *P<0.05, **P<0.01. miR, microRNA; ABCA1, ATP-binding cassette transporter A1; ABCG1, ATP-binding cassette transporter G1; RT-qPCR, reverse trancription-polymerase chain reaction; CON, control; HLP, high lipid diet-fed rats; TAN, Tanshinone IIA treatment of high lipid diet-fed rats; GAPDH, glyceraldehyde 3-phosphate dehydrogenase.
Furthermore, expression of ABCA1 mRNA and protein in the liver of HLP rats was significantly downregulated compared with the control rats (P<0.01), whereas the expression levels of ABCA1 protein were significantly higher in the TAN rats compared with the HLP rats (P<0.05), however, the levels of ABCA1 mRNA showed no significant alteration (Fig. 2B). In addition, the expression levels of ABCG1 mRNA and protein showed no significant alterations between the TAN and HLP rats (Fig. 2B).
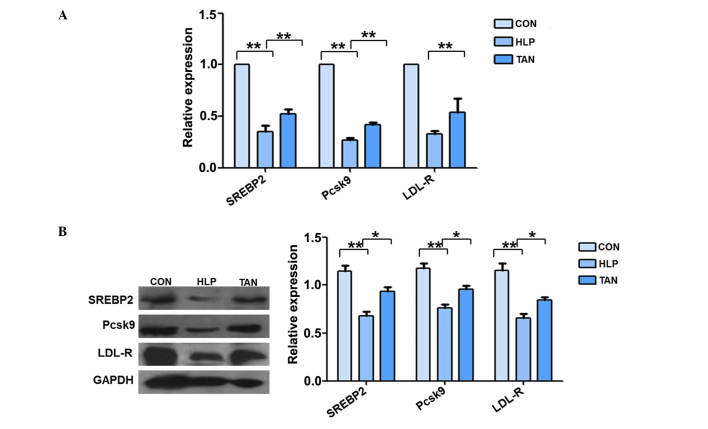
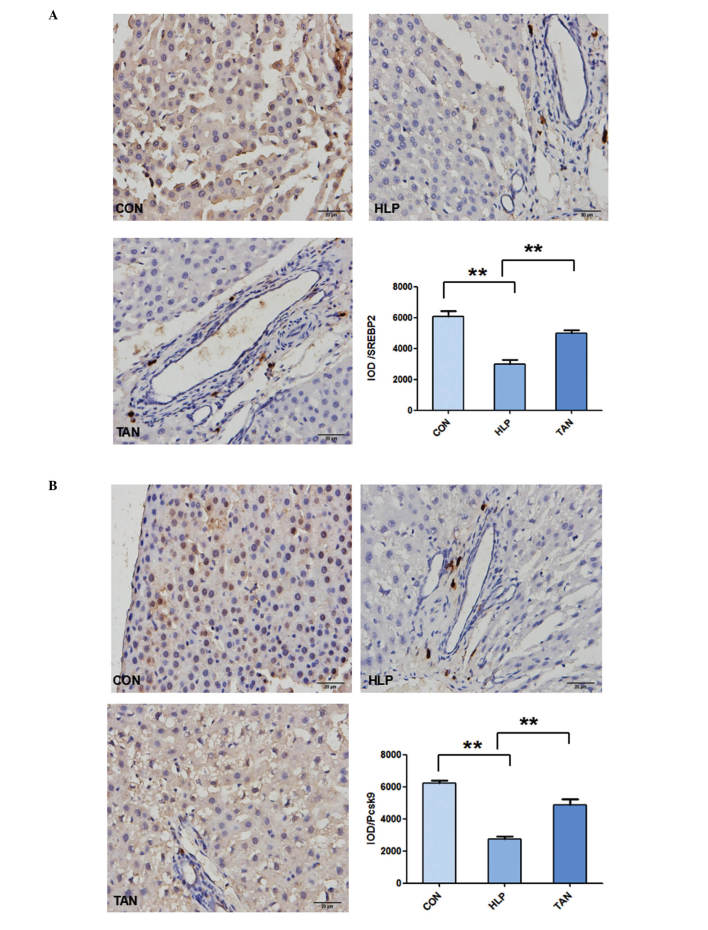
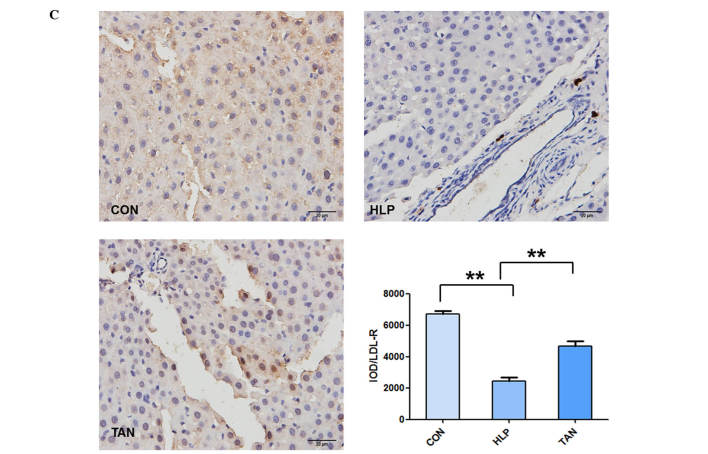
Tanshinone IIA regulation of SREBP-2, Pcsk9 and LDL-R mRNA and protein expression in the liver
The mRNA expression levels of SREBP-2, Pcsk9 and LDL-R were significantly reduced in the liver tissue of HLP rats compared with the control rats (P<0.01; Fig. 3A). However, the mRNA expression levels of SREBP-2 and Pcsk9 were significantly upregulated in the liver tissue of TAN rats, with no alterations observed in LDL-R mRNA expression. The western blotting data supported the RT-qPCR data (Fig. 3B). The immunohistochemical staining additionally indicated that the liver tissues from the HLP rats exhibited weak staining for SREBP-2, Pcsk9 and LDL-R compared with the control rats, whereas the liver tissues from the TAN rats indicated stronger staining for SREBP-2, Pcsk9 and LDL-R (P<0.01; Fig. 4).
Figure 3.
Tanshinone IIA regulation of SREBP-2, Pcsk9 and LDL-R mRNA and protein expression levels in the liver. (A) Reverse transcription-polymerase chain reaction measurement of SREBP-2, Pcsk9 and LDL-R mRNA expression levels in rat liver tissue. (B) Western blotting analysis of SREBP-2, Pcsk9 and LDL-R protein expression levels in the liver. Data are presented as the mean ± standard deviation. *P<0.05, **P<0.01. SREBP-2, sterol regulatory element-binding protein 2; Pcsk9, proprotein convertase subtilisin/kexin type 9; LDL-R, low-density lipoprotein receptor; CON, control; HLP, high lipid diet-fed rats; TAN, Tanshinone IIA treatment of high lipid diet-fed rats; GAPDH, .glyceraldehyde 3-phosphate dehydrogenase.
Figure 4.
Immunohistochemical detection of SREBP-2, Pcsk9 and LDL-R expression in the liver tissue. Tissue from the CON, HLP and TAN groups was collected and stained with antibodies against SREBP-2, Pcsk9 and LDL-R. (A) SREBP-2 protein expression in liver tissue. (B) Pcsk9 protein expression in liver tissue. Data are presented as the mean ± standard deviation. **P<0.01. SREBP-2, sterol regulatory element-binding protein 2; Pcsk9, proprotein convertase subtilisin/kexin type 9; LDL-R, low-density lipoprotein receptor; CON, control; HLP, high lipid diet-fed rats; TAN, Tanshinone IIA treatment of high lipid diet-fed rats; IOD, integrated optical density. (C) LDL-R protein expression in liver tissue. Data are presented as the mean ± standard deviation. **P<0.01. LDL-R, low-density lipoprotein receptor; CON, control; HLP, high lipid diet-fed rats; TAN, Tanshinone IIA treatment of high lipid diet-fed rats; IOD, integrated optical density.
Discussion
Tanshinone is an active compound in Danshen, a traditional Chinese medicine, which has been used historically for the prevention and treatment of cardiovascular diseases in China. There are four major lipophilic components of Tanshinone, namely Tanshinone I, Tanshinone IIA, Tanshinone IIB and crypto Tanshinone. Of these, Tanshinone IIA is the most abundant derivative and structural representative of the Tanshinones (7). In the current study, the in vivo effects of Tanshinone IIA were investigated in a rat model of hyperlipidemia, which indicated that Tanshinone IIA was able to reduce lipid deposition in the liver, without altering the blood lipid profile following a three-month treatment. At the gene level, Tanshinone IIA inhibited miR-33a expression in the liver and upregulated ABCA1, ABCG1, SREBP-2 and Pcsk9 expression. These genes may form a miR-33a/SREBP-2/Pcsk9 signaling pathway to regulate lipid metabolism (27–29). Thus, the current study indicates that Tanshinone IIA should be further studied due to their potential use clinically to prevent or treat fatty liver and associated diseases.
Fat-enriched diets have been used for decades to model obesity, hyperlipidemia, dyslipidemia and insulin intolerance in rodents (30). In the current study, rats were fed with a high-fat diet for three months to establish a rat model of hyperlipidemia according to previous studies (31). Following 3 months of a high fat diet, a group of rats were treated with Tanshinone IIA for a further 3 months. The aim of the present study was to demonstrate Tanshinone IIA activity against hyperlipidemia in vivo, with the data indicating that Tanshinone IIA is able to reduce lipid deposition in the liver, however, did not affect the serum lipid profile. Clinically, lipid deposition in the liver can result in fatty liver, abnormal liver function or cirrhosis, which may be due to non-alcoholic fatty liver disease or excessive alcohol consumption. The prevalence of non-alcoholic fatty liver disease ranges from 9–36.9% of the population in different parts of the world (32–34). From use in Chinese clinics, Danshen has been observed to display no notable side effects; thus, Tanshinone IIA may have potential in aiding the control of fatty livers.
Cholesterol is an essential structural component of the cell membrane in the majority of vertebrates, and its transportation requires lipoproteins in the human body (35). It is known that LDL is the main carrier of cholesterol in the blood, and altered serum LDL levels are considered a major risk factor for cardiovascular disease (36). LDL-R, a transmembrane glycoprotein, is the predominant molecule to maintain serum LDL levels and serves an important role in cholesterol homeostasis (37,38). When cells accumulate excess sterols, LDL-R expression on the cell surface will reduced. By contrast, upon depletion of intracellular cholesterol, cells express a high level of LDL-R (39). Previous studies have indicated that Pcsk9 is highly expressed in the liver and contributes to cholesterol homeostasis by regulating LDL-R levels (39,40). Pcsk9 mutations have been associated with autosomal dominant hypercholesterolemia, which is characterized by high LDL levels (41). In support of this, the current study indicated that Tanshinone IIA is able to promote Psck9 expression in liver tissue. miRNAs are a class of non-coding small RNAs, ~18–22 nucleotides long, which serve an important role in the regulation of gene expression at the post-transcriptional level (42,43). Previous studies have demonstrated that miR-33 is able to regulate cholesterol efflux and HDL biogenesis by suppressing expression of the ABC transporters, ABCA1 and ABCG1 (39,26). These transporters promote the efflux of phospholipids and cholesterol to their associated apolipoprotein, apo-A1, to generate nascent, discoidal HDL particles, a critical step for the initiation of reverse cholesterol transport to the liver for excretion (5). A previous study demonstrated that there are three highly conserved miR-33 binding sites in the 3′-untranslated region of ABCA1, and that miR-33 overexpression represses the expression of ABCA1 protein in a variety of cells (20). SREBPs are transcription factors that bind to the sterol regulatory element DNA sequence, TCACNCCAC, to regulate the cholesterol biosynthetic pathway (44). Hepatic cholesterol deprivation results in SREBP cleavage-activating protein escorting SREBP to the Golgi apparatus for processing and activation, followed by transportation to the nucleus and the upregulation of target gene expressions (45,46). In the current study, miR-33a expression was observed to be upregulated, whilst the expression levels of ABCA1 and ABCG1 were reduced in the liver tissues of HLP rats, which further supports that ABCA1 and ABCG1 are the miR-33a target genes. Thus, further studies should investigate whether the effect of Tanshinone IIA is mediated by suppression of miR-33a expression.
To conclude, the current study indicates that Tanshinone IIA is able to attenuate lipid deposition in the livers of hyperlipidemic rats, and modulate the expression of miR-33a and SREBP2/Pcsk9 signaling pathway proteins. Further studies are required to investigate the underlying molecular mechanisms and to assess the potential clinical use of Tanshinone IIA.
Acknowledgments
The current study was supported by the National Natural Science Foundation of China (grant no. 81202834), National Program on Key Basic Research Project (973 Program) (grant no. 2013CB531704), Natural Science Foundation of Liaoning Province (grant no. 2015020394), and Institutions of Higher Learning Talents Support Program in Liaoning Province (grant no. LR2015041).
References
- 1.Chait A, Brunzell JD. Acquired hyperlipidemia (secondary dyslipoproteinemias) Endocrinol Metab Clin North Am. 1990;19:259–278. [PubMed] [Google Scholar]
- 2.Williams AD. Hyperlipidaemia and atherogenesis. Med Hypotheses. 1990;33:213–217. doi: 10.1016/0306-9877(90)90179-I. [DOI] [PubMed] [Google Scholar]
- 3.Xie Y, He YB, Zhang SX, Pan AQ, Zhang J, Guan XH, Wang JX, Guo WS. Treatment of combined hyperlipidemia patients by jiangzhi tongluo soft capsule combined atorvastatin calcium tablet: A clinical study. Chin J Int Trad Western Med. 2014;34:1059–1063. In Chinese. [PubMed] [Google Scholar]
- 4.Fruebis J, Bird DA, Pattison J, Palinski W. Extent of antioxidant protection of plasma LDL is not a predictor of the antiatherogenic effect of antioxidants. J Lipid Res. 1997;38:2455–2464. [PubMed] [Google Scholar]
- 5.Tall AR, Yvan-Charvet L, Terasaaka N, Pagler T, Wang N. HDL, ABC transporters and cholesterol efflux: Implications for the treatment of atherosclerosis. Cell Metab. 2008;7:365–375. doi: 10.1016/j.cmet.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Tang F, Wu X, Wang T, Wang P, Li R, Zhang H, Gao J, Chen S, Bao L, Huang H, Liu P. Tanshinone IIA attenuates atherosclerotic calcification in rat model by inhibition of oxidative stress. Vascul Pharmacol. 2007;46:427–438. doi: 10.1016/j.vph.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Gao S, Liu Z, Li H, Little PJ, Liu P, Xu S. Cardiovascular actions and therapeutic potential of Tanshinone IIA. Atherosclerosis. 2012;220:3–10. doi: 10.1016/j.atherosclerosis.2011.06.041. [DOI] [PubMed] [Google Scholar]
- 8.Xu W, Yang J, Wu LM. Cardioprotective effects of anshinone IIA on myocardial ischemia injury in rats. Pharmazie. 2009;64:332–336. [PubMed] [Google Scholar]
- 9.Gong Z, Huang C, Sheng X, Zhang Y, Li Q, Wang MW, Peng L, Zang YQ. The role of Tanshinone IIA in the treatment of obesity through peroxisome proliferator-activated receptor gamma antag-onism. Endocrinology. 2009;150:104–113. doi: 10.1210/en.2008-0322. [DOI] [PubMed] [Google Scholar]
- 10.Tang FT, Cao Y, Wang TQ, Wang LJ, Guo J, Zhou XS, Xu SW, Liu WH, Liu PQ, Huang HQ. Tanshinone IIA attenuates atherosclerosis in ApoE (−/−) mice through down-regulation of scavenger receptor expression. Eur J Pharmacol. 2011;650:275–884. doi: 10.1016/j.ejphar.2010.07.038. [DOI] [PubMed] [Google Scholar]
- 11.Jia LQ, Feng JY, Yang GL, Chen WN, Chen Y. Effect of Tanshinone IIA on TLR4 and TNF-α of endothelial cells induced by LPS. Chin J Cell Mol Immunol. 2011;27:733–735. In Chinese. [PubMed] [Google Scholar]
- 12.Jia LQ, Yang GL, Ren L, Chen WN, Feng JY, Gao Y, Zhang L, Li XT, Lei P. Tanshinone IIA reduces apoptosis induced by hydrogen peroxide in the human endothelium-derived EA.hy926 cells. J Ethnopharmacol. 2012;143:100–108. doi: 10.1016/j.jep.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 13.Horie T, Ono K, Horiguchi M, Nishi H, Nakamura T, Nagao K, Kinoshita M, Kuwabara Y, Marusawa H, Iwanaga Y, et al. MicroRNA-33 encoded by an intron of sterol regulatory element-binding protein 2 (SREBP-2l) regulates HDL in vivo. Proc Natl Acad Sci USA. 2010;107:17321–17326. doi: 10.1073/pnas.1008499107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dávalos A, Goedeke L, Smibert P, Ramirez CM, Warrier NP, Andreo U, Cirera-Salinas D, Rayner K, Suresh U, Pastor-Pareja JC, et al. miR-33a/b contribute to the regulation of fatty acid metabolism and insulin signaling. Proc Natl Acad Sci USA. 2011;108:9232–9237. doi: 10.1073/pnas.1102281108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu CY, Tang ZH, Liu LS, Jiang ZS. Selecting pharmacological targets of Pcsk9. Chin J Biochem Mol Biol. 2009;25:991–996. In Chinese. [Google Scholar]
- 16.Costet P, Cariou B, Lambert G, Lalanne F, Lardeux B, Jarnoux AL, Grefhorst A, Staels B, Krempf M. Hepatic Pcsk9 expression is regulated by nutritional status via insulin and sterol regulatory element-binding protein 1c. J Biol Chem. 2006;281:6211–6218. doi: 10.1074/jbc.M508582200. [DOI] [PubMed] [Google Scholar]
- 17.Attie AD. The mystery of Pcsk9. Arterioscler Thromb Vasc Biol. 2004;24:1337–1339. doi: 10.1161/01.ATV.0000137288.82390.04. [DOI] [PubMed] [Google Scholar]
- 18.Steinberg D, Witztum JL. Inhibition of Pcsk9: A powerful weapon for achieving ideal LDL cholesterol levels. Proc Natl Acad Sci USA. 2009;106:9546–9547. doi: 10.1073/pnas.0904560106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dong B, Wu MH, Li H, Kraemer FB, Adeli K, Seidah NG, Park SW, Liu J. Strong iduction of Pcsk9 gene expression through HNF1alpha and SREBP-2: Mechanism for the resistance to LDL-cholesterol lowering effect of statins in dyslipidemic hamsters. J Lipid Res. 2010;51:1486–1495. doi: 10.1194/jlr.M003566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Najafi-Shoushtari SH, Kristo F, Li Y, Shioda T, Cohen DE, Gerszten RE, Näär AM. MicroRNA-33 and the SREBP host genes cooperate to control cholesterol homeostasi. Science. 2010;328:1566–1569. doi: 10.1126/science.1189123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Attie AD. ABCA1: At the nexus of cholesterol, HDL and atherosclerosis. Trends Biochem Sci. 2007;32:172–179. doi: 10.1016/j.tibs.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 22.Fernández-Hernando C, Ramírez CM, Goedeke L, Suárez Y. MicroRNAs in metabolic disease. Arterioscler Thromb Vasc Bio. 2013;33:178–185. doi: 10.1161/ATVBAHA.112.300144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gerin I, Clerbaux LA, Haumont O, Lanthier N, Das AK, Burant CF, Leclercq IA, MacDougald OA, Bommer GT. Expression of miR-33 froman SREBP-2 intron inhibits cholesterol export and fatty acid oxidation. J Biol Chem. 2010;285:33652–33661. doi: 10.1074/jbc.M110.152090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fernández-Hernando C, Suárez Y, Rayner KJ, Moore KJ. MicroRNAs in lipid metabolism. Curr Opin Lipidol. 2011;22:86–92. doi: 10.1097/MOL.0b013e3283428d9d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lewis GF, Rader DJ. New insights into the regulation of HDL metabolism and reverse cholesterol transport. Circ Res. 2005;96:1221–1232. doi: 10.1161/01.RES.0000170946.56981.5c. [DOI] [PubMed] [Google Scholar]
- 26.Rayner KJ, Sheedy FJ, Esau CC, Hussain FN, Temel RE, Parathath S, van Gils JM, Rayner AJ, Chang AN, Suarez Y, et al. Antagonism of miR-33 in mice promotes reverse cholesterol transport and regression of atherosclerosis. J Clin Invest. 2011;121:2921–2931. doi: 10.1172/JCI57275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rayner KJ, Esau CC, Hussain FN, McDaniel AL, Marshall SM, van Gils JM, Ray TD, Sheedy FJ, Goedeke L, Liu X, et al. Inhibition of miR-33a/b in non-human primates raises plasma HDL and lowera VLDL triglycerides. Nature. 2011;478:404–447. doi: 10.1038/nature10486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu W, Zhai C, Zhang X, Zhang H, Jiang M, Zhou S, Liu Y, Zhao N, Zhao J. Research of the whole grain-soybean compound package to regulate the cholesterol metabolism by SREBP-2, LDLR and visfatin. J Hyg Res. 2013;42:196–202. In Chinese. [PubMed] [Google Scholar]
- 29.Xu W, Liu L, Homby D. c-IAP1 binds and processes Pcsk9 protein: Linking the c-IAP1 in a TNF-α pathway to Pcsk9-mediated LDLR degradation pathway. Molecules. 2012;17:12086–12101. doi: 10.3390/molecules171012086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mani DN, Bawankule D, Saroj BK. Hyperlipidemic model: Studying lipid profile in small experimental animal. Int J Pharmacy Pharm Sci. 2012;4:337–340. [Google Scholar]
- 31.Munshi RP, Joshi SG, Rane BN. Development of an experimental diet model in rats to study hyperlipidemia and insulin resistance, markers for coronary heart disease. Indian J Pharmacol. 2014;46:270–246. doi: 10.4103/0253-7613.132156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Omagari K, Kadokawa Y, Masuda J, Egawa I, Sawa T, Hazama H, Ohba K, Isomoto H, Mizuta Y, Hayashida K, et al. Fatty liver in non-alcoholic non overweight Japanese adults: Incidence and clinical characteristics. J Gastroenterol Hepatol. 2002;17:1098–1105. doi: 10.1046/j.1440-1746.2002.02846.x. [DOI] [PubMed] [Google Scholar]
- 33.Hilden M, Christoffersen P, Juhl E, Dalgaard JB. Liver histology in a 'normal' population-examinations of 503 consecutive fatal traffic casualties. Scand J Gastroenterol. 1997;12:593–597. doi: 10.3109/00365527709181339. [DOI] [PubMed] [Google Scholar]
- 34.Shen L, Fan JG, Shao Y, Zeng MD, Wang JR, Luo GH, Li JQ, Chen SY. Prevalence of nonalcoholic fatty liver among administrative officers in Shanghai: An epidemiological survey. World J Gastroenterol. 2003;9:1106–1110. doi: 10.3748/wjg.v9.i5.1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ikonen E. Cellular cholesterol trafficking and compartmentalization. Nat Rev Mol Cell Biol. 2008;9:125–138. doi: 10.1038/nrm2336. [DOI] [PubMed] [Google Scholar]
- 36.Sone H, Tanaka S, Tanaka S, Iimuro S, Oida K, Yamasaki Y, Oikawa S, Ishibashi S, Katayama S, Ohashi Y, et al. Serum level of triglycerides is a potent risk factor comparable to LDL cholesterol for coronary heart disease in Japanese patients with type 2 diabetes: Subanalysis of the Japan Diabetes Complications Study (JDCS) J Clin Endocrinol Metab. 2011;96:3448–3456. doi: 10.1210/jc.2011-0622. [DOI] [PubMed] [Google Scholar]
- 37.Brown MS, Goldstein JL. A receptor-mediated pathway for cholesterol homeostasis. Science. 1986;232:34–47. doi: 10.1126/science.3513311. [DOI] [PubMed] [Google Scholar]
- 38.Sharpe LJ, Brown AJ. Rapamycin down-regulates LDL-receptor expression independently of SREBP-2. Biochem Biophys Res Commun. 2008;373:670–674. doi: 10.1016/j.bbrc.2008.06.108. [DOI] [PubMed] [Google Scholar]
- 39.Rayner KJ, Suárez Y, Dávalos A, Parathath S, Fitzgerald ML, Tamehiro N, Fisher EA, Moore KJ, Fernández-Hernando C. MiR-33 contributes to the regulation of cholesterol homeostasis. Science. 2010;328:1570–1573. doi: 10.1126/science.1189862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maxwell KN, Breslow JL. Adenoviral-mediated expression of Pcsk9 in mice results in a low-density lipoprotein receptor knockout phenotype. Proc Natl Acad Sci USA. 2004;101:7100–7105. doi: 10.1073/pnas.0402133101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abifadel M, Varret M, Rabès JP, Allard D, Ouguerram K, Devillers M, Cruaud C, Benjannet S, Wickham L, Erlich D, et al. Mutations in Pcsk9 cause autosomal dominant hypercholesterolemia. Nat Genet. 2003;34:154–156. doi: 10.1038/ng1161. [DOI] [PubMed] [Google Scholar]
- 42.Krol J, Loedige I, Filipowicz W. The widespread regulation of microRNA biogenesis, function and decay. Nat Rev Genet. 2010;11:597–610. doi: 10.1038/nrg2843. [DOI] [PubMed] [Google Scholar]
- 43.Kato M, de Lencastre A, Pincus Z, Slack FJ. Dynamic expression of small non-coding RNAs, including novel microRNAs and piRNAs/21U-RNAs, during Caenorhabditis elegans development. Genome Biol. 2009;10:R54. doi: 10.1186/gb-2009-10-5-r54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Roglans N, Peris C, Verd JC, Alegret M, Vázquez M, Sánchez RM, Laguna JC. Increase in hepatic expression of SREBP-2 by gemfibrozil administration to rats. Biochem Pharmacol. 2011;62:803–809. doi: 10.1016/S0006-2952(01)00701-8. [DOI] [PubMed] [Google Scholar]
- 45.Horton JD, Shimomura I. Sterol regulatory element-binding proteins: Activators of cholesterol and fatty acid biosynthesis. Curr Opin Lipidol. 1999;10:143–150. doi: 10.1097/00041433-199904000-00008. [DOI] [PubMed] [Google Scholar]
- 46.Horton JD. Sterol regulatory element-binding proteins: Transcriptional activators of lipid synthesis. Biochem Soc Trans. 2002;30:1091–1095. doi: 10.1042/bst0301091. [DOI] [PubMed] [Google Scholar]