Abstract
Objectives
To explore whether the psychologic variables anxiety, depression, and fear-avoidance beliefs, and interactions between these variables, are associated with physical function in patients with knee osteoarthritis (OA). We hypothesized lower levels of function would be related to higher anxiety, higher depression, and higher fear-avoidance beliefs, and that high levels of 2 of these factors simultaneously might interact to have a greater adverse effect on physical function.
Design
Cross-sectional, correlational design.
Setting
Institutional practice.
Participants
Subjects included patients with knee OA (N=182; age, mean ± SD, 63.9±8.8y; 122 women).
Interventions
Not applicable.
Main Outcome Measures
Self-report measures of function included the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index, the Lower Extremity Function Scale (LEFS), and the Knee Outcome Survey-Activity of Daily Living Scale. The Get Up and Go test was used as a physical performance measure of function. Self-report measures for psychologic variables included the Beck Anxiety Inventory, the Center for Epidemiological Studies Depression Scale, and the Fear Avoidance Belief Questionnaire-Physical Activity Scale modified for the knee.
Results
Higher anxiety was related to poorer function on the WOMAC physical function. Both high anxiety and fear avoidance beliefs were related to poorer function on the LEFS and Knee Outcome Survey-Activity of Daily Living Scale. There was no association between the psychologic variables and the Get Up and Go test. The anxiety X depression interaction was associated with the LEFS.
Conclusions
Anxiety and fear-avoidance beliefs are associated with self-report measures of function in patients with knee OA. Depression may influence scores on the LEFS under conditions of low anxiety.
Keywords: Anxiety, Depression, Fear, Knee, Osteoarthritis, Rehabilitation
Over 4.3 million older adults in the United States are affected by knee OA, a chronic and disabling condition that is among the leading causes of pain and functional limitations.1 Multiple studies have examined determinants of function in knee OA and found that a wide variety of factors including demographic, clinical, and biomechanical factors have significant associations with functional status.2–7 In addition, growing evidence suggests psychologic factors such as anxiety, fear, and depression may also relate to physical function in patients with knee OA.8–12
Although the terms anxiety and fear are often used simultaneously, Leeuw et al13 have described a distinction between these 2 variables.13 According to Leeuw,13 fear is an emotional reaction to a specific, identifiable threat that may increase sympathetic nervous system arousal and induce defensive or escape behavior to remove the specific threat. Where fear is concerned, the threatening stimulus or event is in the present tense. Anxiety is similar to fear in that it is also an emotional reaction associated with a heightened state of arousal, but the focus of the threat is unclear.13 The threatening stimulus is not specific and identifiable, and anxiety may be more associated with an anticipation (future tense) of a threatening situation, rather than a well defined threatening stimulus.13 Anxiety may induce more preventive behaviors such as avoidance of situations that the person might anticipate could be potentially threatening or anxiety-producing. Anxious people may be hypervigilent, in that they are over focused on scanning their environment for potential threats.13
Fear and anxiety may both contribute to the fear-avoidance model in musculoskeletal disorders. The fear-avoidance model is based on the idea that the way a person interprets pain may lead to 1 of 2 pathways: (1) an adaptive response in which acute pain, while an annoyance, is not perceived as threatening, and so the person confronts the pain and is more likely to return to and maintain daily activities that help achieve functional recovery; or (2) a non-adaptive response in which pain is perceived as threatening and leads to maladaptive behaviors including pain-related fear, avoidance, and hypervigilance.13 In the long term, these behaviors may result in increased disuse and disability, which further decrease the opportunity to disprove the fear of movement and fear of pain.
Avoidance behaviors have been associated with disability in a variety of musculoskeletal conditions,14, 15 most notably in low back pain, in which fear-avoidance beliefs have been shown to predict changes in disability.16 Fear is thought to lead to avoidance of activities believed to be painful or harmful, which may lead to increased disability through the detrimental effects of physical inactivity and weakening of the musculoskeletal system.14 A study by Heuts et al11 found that pain related fear and fear of movement were present and associated with function in patients with knee OA. Some investigators have also found anxiety to be associated with function measures in subjects with knee OA,8–10 while others have not found this to be the case.
In addition to fear and anxiety, depression may be associated with reduced function in people with knee OA. According to the National Institute of Mental Health, depression is a mood disorder that can be characterized by persistent sadness; feelings of helplessness, hopelessness, or worthlessness; pessimism; and irritability.17 A person with depression may also lose interest in daily activities, hobbies, and recreation.17 Therefore, it is understandable that depression could be associated with poor physical function. Where knee OA is concerned, there is conflicting evidence regarding the association of depression with measures of physical function, with some investigators reporting significant associations8, 9 and others finding no association.
The psychologic variables of fear, anxiety, and depression can be associated with each other, and therefore it may be possible that they could interact to have a greater effect on physical function. For example, Leeuw et al13 suggest that fear of pain may be secondary to the fear of anxiety-related sensations associated with pain. In such an instance, it may be possible that in someone who is already an anxious person, the combined effect of both fear and anxiety may have a greater manifestation of poor function, which might create more difficulty in overcoming functional deficits associated with musculoskeletal pathology. To our knowledge, there have been no studies that have examined how fear, anxiety, and depression may interact to influence physical function in subjects with knee OA.
The current evidence suggests that fear, anxiety, and depression may play a role in determining the functional status of patients with knee OA. However, the results of studies examining the association of these variables in subjects with knee OA are not consistent and are sometimes limited by small sample size. In addition, the potential interactive effects of these variables on measures of physical function in subjects with knee OA have not yet been explored. Therefore, we believe that further examination of the role these psychologic variables have in influencing measures of physical function was warranted. The aim of this study was to explore whether fear, anxiety, and depression and interactions among these factors are associated with physical function in patients with knee OA. We hypothesized that lower levels of function would be related to higher fear, higher anxiety, and higher depression, and that high levels of 2 of these factors at once might interact to have a greater adverse effect on physical function.
METHODS
The data reported here were drawn from an ongoing randomized controlled trial comparing 2 exercise rehabilitation regimens for patients with knee OA.18 The current cross sectional study looks at associations using the baseline data.
Subjects
Subjects included 182 people, 40 years of age and older, who met the 1986 American College of Rheumatology clinical criteria for knee OA,19 and had grade II or greater Kellgren and Lawrence20 radiographic changes. The 1986 criteria for diagnosis of knee OA include knee pain and osteophytes with at least 1 of the following: age 50 years or older, morning stiffness less than 30 minutes, or crepitus with active motion of the knee. Subjects were excluded from the study if they (1) had only patellofemoral joint radiographic changes, (2) had conditions that would place them at risk for injury during the exercise training program (eg, requiring an assistive device for ambulation, history of 2 or more falls in the previous year, unable to ambulate 100 feet independently), (3) had undergone total knee arthroplasty, (4) exhibited uncontrolled hypertension, (5) had a history of cardiovascular disease, (6) had a history of neurologic disorders that affected lower extremity function (eg, stroke, peripheral neuropathy), (7) had conditions that would place them at risk for re-injury during quadriceps strength testing (eg, recent corticosteroid injection to the quadriceps or patellar tendons, quadriceps or patellar tendon rupture, patellar fracture), or (8) reported vision problems that affected their ability to perform basic mobility tasks. All subjects signed an informed consent form approved by the University of Pittsburgh Institutional Review Board prior to participation in the study.
Measures
Data for this study were collected in 1 session. Subjects completed surveys on demographic information, fear avoidance beliefs, anxiety, depression, and self-report measures of physical function. They also completed the Get Up and Go test, a performance-based measure of physical function.
Fear-avoidance beliefs were measured using the FABQ-PA, which was originally developed for low back pain.21 A modified version of the FABQ-PA has been used by van Baar et al22 to assess fear-avoidance beliefs in people with knee pathology. The FABQ-PA for our study was modified from the low back version by replacing the word “back” with “knee,” and replacing the example physical activities of “bending, lifting, walking and driving” with “running, walking, kneeling, and driving.” The FABQ-PA quantifies the level of fear associated with physical activity including querying on beliefs about the association of physical activity with pain and harm to the knee. The scale consists of 4 items, each scored 0 to 6, with a maximum of 24. Higher scores represent greater fear avoidance beliefs. The Cronbach alpha value of the FABQ-PA subscale in our sample of patients with knee OA was .75, indicating adequate internal consistency. There have been no other studies that we are aware of that have formally examined the psychometric properties of the FABQ-PA modified for the knee.
Anxiety was measured using the BAI.23 The BAI consists of 21 items, each scored 0 to 3, with higher scores representing higher levels of anxiety. It has been shown to be a reliable and valid measure to assess the presence and magnitude of anxiety symptoms.23, 24
Depression was measured using the CES-D.19 The CES-D is a 20-item self-report depression scale, each item scored 0 to 3, with higher scores representing greater symptoms of depression. The CES-D has been shown to be a reliable, valid, and sensitive tool for detecting depressive symptoms and changes in depression over time.25–27
The WOMAC Osteoarthritis Index is a disease specific measure of pain, stiffness, and physical function for people with knee OA. We used the 17-item physical function subscale (WOMAC-PF) as a measure for self-report of physical function. Each item is scored on a 5-point Likert scale with a maximum total of 68 for the physical function scale. Higher scores on the WOMAC represent greater limitations in function. The reliability, validity, and responsiveness of the WOMAC have been established.28–33
The LEFS is a 20-item self-report survey intended for use in patients with pathologies affecting lower extremity function.34 The scale queries patients on their ability to perform general activities of daily living, general recreational activities, specific daily physical tasks, and specific recreational or occupational related tasks. Each item is scored on a 5-point Likert scale with a maximum total of 80. Lower scores on the LEFS represent greater limitations in function. Good psychometric properties have been shown for a sample that included patients with knee OA.34
Activities of Daily Living Scale of the Knee Outcome Survey is a 14-item knee-specific measure of physical function that assesses the effects of knee impairment on activities of daily living.35 Each item is scored on a 6-point Likert scale. The Knee Outcome Survey-Activity of Daily Living Scale score is transformed to a 0 to 100 scale. Lower scores on the Knee Outcome Survey-Activity of Daily Living Scale represent greater limitations in function. Reliability, validity, and responsiveness were demonstrated in a population that included knee OA.35
The Get Up and Go test is a measure of balance and gait that we used as a physical performance measure of function.36 To perform the test, subjects were seated on a standard-height chair with armrests. On the command “go,” subjects stood up and walked along a level, unobstructed corridor as fast as possible. A stopwatch was used to measure the time it took for the subject to stand up and walk 15m (50 feet). Longer time to complete the Get Up and Go test represents greater limitation in function. We have demonstrated good intratester (ICC=.95) and intertester (ICC=.98) reliability for patients with knee OA in our laboratory.36
Data Analysis
We first examined descriptive statistics to assess for outliers and data distributions. Then we calculated bivariate correlation coefficients to look at associations among physical function variables, psychological variables, and demographic variables. Pearson correlation coefficients were used between normally distributed continuous variables, and Spearman rho coefficients were used for categorical and non-normally distributed continuous variables.
To assess how psychologic variables and their interactions relate to function in patients with knee OA, we conducted a series of linear regressions with each of our physical function measures (WOMAC-PF, LEFS, Knee Outcome Survey-Activity of Daily Living Scale, Get Up and Go) as the dependent variable. All independent variables were standardized, and interaction terms between psychologic variables were computed with standardized values to reduce multi collinearity and facilitate testing interaction terms. First, to control for demographic variables that could be associated with physical function, we entered sex, age, height, weight, intensity of knee pain (worst pain in the past 24 hours rated on a 0–10 numeric pain rating scale), years with a physician’s diagnosis of knee OA, and the radiographic severity of knee OA (Kellgren and Lawrence20 grading scale) into the model. Second, we entered the main effect biobehavioral variables FABQ-PA, BAI, and CES-D and 2-way interaction terms between the biobehavioral variables (FABQ-PA X BAI, FABQ-PA X CES-D, and BAI X CES-D) into the model. Three-way interactions were not explored because of the concern that we were underpowered to assess 3-way interactions. Statistical significance was determined using an alpha level of .05. Regression coefficients and standardized beta coefficients for each variable in the final model were calculated, and the significance of each was tested under the null hypothesis that the coefficient was not different from 0. Regression diagnostics were performed to assess whether our model met the linear regression assumptions of normality, homoscedasticity, and linearity. Finally, we graphed the interaction effects by using the unstandardized beta values from the final regression model.
RESULTS
Our analysis included 182 subjects who had a mean age of 64 years and of whom 122 (67%) were women. There were 159 (87%) white subjects, 17 (9%) black subjects, 2 each Asian and Native American, and 2 subjects who selected “other” to categorize their race. Table 1 summarizes descriptive statistics for age, sex, height, weight, knee pain, years with a physician’s diagnosis of knee OA, radiographic severity of knee OA, measures of physical function, and psychologic variables used in the analysis.
Table 1.
Descriptive Statistics for Demographic Factors, Measures of Physical Function, and Biobehavioral Factors for 182 Subjects
| Continuous Variables | Mean ± SD | Range |
|---|---|---|
| Age (y) | 63.90 ± 8.8 | 40–85 |
| Height (cm) | 167.73 ± 9.44 | 146.50–196.00 |
| Weight (kg) | 85.86 ± 19.02 | 45.67–159.68 |
| Knee pain (0–10) numeric pain rating scale) | 4.53 ± 2.51 | 0–10 |
| WOMAC-PF | 19.70 ± 12.09 | 0–59 |
| LEFS* | 51.31 ± 14.03 | 13–80 |
| Activity of Daily Living Scale | 67.13 ± 17 93 | 12.8–100 |
| Get Up and Go test* | 9.59 ± 2.22 | 5.00–19.22 |
| FABQ-PA | 10.71 ± 6.22 | 0–24 |
| BAI† | 4.73 ± 5.36 | 0–29 |
| CES-D† | 7.30 ± 7.38 | 0–40 |
|
| ||
| Categorical Variables | No.(%) | Cumulative % |
|
| ||
| Women | 122 (67) | 67.0 |
| Years with diagnosis of OA Less than 1y | 30 (16.5) | 16.5 |
| 1–2 y | 32 (17.6) | 34.1 |
| 3–5y | 44 (24.1) | 58.2 |
| 5–10y | 30 (16.5) | 74.7 |
| More than 10y | 46 (25.3) | 100 |
| Radiographic severity (Kellgren and Lawrence grade) | ||
| Grade II | 27 (14.8) | 14.8 |
| Grade III | 86 (47.3) | 62.1 |
| Grade IV | 69 (37.9) | 100 |
n=181 for the LEFS and n=179 for the Get Up and Go test because of missing data.
Median values for the nornormally distributed BAI and CES-D are 3.0 and 5.0, respectively.
Bivariate correlations revealed significant associations between each psychologic variable and all 3 self-report measures of function (table 2). High levels of fear-avoidance beliefs, anxiety, and depression were associated with reduced selfreported function. The only psychologic variable to have a significant association with the performance-based measure of function was the BAI, indicating that high levels of anxiety were associated with slower performance in the Get Up and Go. For the covariates, higher age and female sex were associated with greater time to complete the Get Up and Go, and female sex was also associated with lower self-reported function. Taller subjects had faster performance in the Get Up and Go and reported better function according to the WOMAC-PF and Knee Outcome Survey-Activity of Daily Living Scale, but not the LEFS. Higher weight and greater knee pain were associated with reduced self-reported function, but not with the performance-based Get Up and Go. Greater number of years with a diagnosis of knee OA yielded a small association with lower Knee Outcome Survey-Activity of Daily Living Scale scores, and greater severity of radiographic knee OA was associated with worse function on the WOMAC-PF, the LEFS, and the Get Up and Go.
Table 2.
Bivariate Correlations Between Demographics, Measures of Function, and Biobehavioral Factors
| Age | Height | Weight | Sex(ρ) | Pain | OA Duration | OA Severity | FABQ-PA | BAI (ρ) | CES-D (ρ) | |
|---|---|---|---|---|---|---|---|---|---|---|
| WOMAC-PF | −.121 | −.183* | .251† | .240† | .671† | .127 | .212† | .218† | .429† | .224† |
| LEFS | .115 | .109 | −.269† | −.177* | −.558† | −.136 | −.246† | −.283† | −.390† | −.206† |
| ADLS | .135 | .153* | −.296† | −.288† | −.629† | −.181* | −.264 | −.263† | −.433† | −.272† |
| GUAG | .297† | −.353† | .048 | .456† | .079 | .038 | .163* | .005 | .158* | .125 |
| FABQ-PA | −.181* | .091 | .185* | −.039 | .202† | .017 | .086 | .160* | .156 | |
| BAI (ρ) | −.061 | −.065 | .143 | .146* | .381† | .039 | .073 | .450† | ||
| CES-D (ρ) | −.053 | −.101 | .106 | .088 | .187† | −.063 | .013 |
NOTE. Spearman rho coefficient was calculated for variables not normally distributed.
Abbreviations: ADLS, Knee Outcome Survey-Activities of Daily Living Scale; GUAG. Get Up and Go test.
P<.05.
P<.01.
The results of the linear regression on the WOMAC-PF indicated that higher anxiety (higher BAI score) was significantly associated with worse function (higher WOMAC-PF score) when controlling for sex, age, height, weight, knee pain, years with a diagnosis of knee OA, and radiographic severity of knee OA (table 3). FABQ-PA, BAI, and the BAI X CES-D interaction were significantly associated with the LEFS when controlling for sex, age, height, weight, knee pain, years with a diagnosis of knee OA, and radiographic severity of knee OA (see table 3). Worse physical function (lower LEFS score) was related to higher fear-avoidance beliefs, higher anxiety, and the interaction between anxiety and depression. Only FABQ-PA and BAI were significantly associated with the Knee Outcome Survey-Activity of Daily Living Scale when controlling for sex, age, height, weight, knee pain, years with a diagnosis of knee OA, and radiographic severity of knee OA (see table 3). Worse physical function (lower Knee Outcome Survey-Activity of Daily Living Scale score) was associated with higher fear-avoidance beliefs and higher anxiety. None of the psychologic variables or interactions were significantly associated with the performance-based outcome measure Get Up and Go when controlling for sex, age, height, weight, knee pain, years with a diagnosis of knee OA, and radiographic severity of knee OA (see table 3). All variance inflation factors were less than 10, indicating no multicollinearity (see table 3). Observation of residual plots demonstrated that our models fit the linear regression model assumptions of normality, homoscedasticity, and linearity.
Table 3.
Regression Models on Physical Function Measures
| Dependent | Independent | R2 | Adjusted R2 | df | P† | β | P‡ | VIF |
|---|---|---|---|---|---|---|---|---|
| WOMAC-PF | Modal 1: sex, age, height, weight, pain, OA duration, OA severity | .51 | .49 | 7, 174 | <.01 | |||
| Modal 2* | .54 | .51 | 13, 168 | <.01 | ||||
| FABQ-PA | .09 | .11 | 1.154 | |||||
| BAI | .20 | .02 | 2.774 | |||||
| CES-D | .03 | .66 | 1.986 | |||||
| FAEQ-PA × BAI | −.01 | .41 | 1.923 | |||||
| FABQ-PA × CES-D | .15 | .86 | 1.891 | |||||
| BAI × CES-D | −.12 | .13 | 2.450 | |||||
| LEFS | Modal 1: sex, ege, height, weight, pain, DA duration, OA severity | .41 | .39 | 7, 173 | <.01 | |||
| Modal 2* | .50 | .46 | 13, 167 | <.01 | ||||
| FABQ-PA | −.23 | <.01 | 1.162 | |||||
| BAI | −.21 | .03 | 2.773 | |||||
| CES-D | −.06 | .44 | 1.997 | |||||
| FABQ-PA × BAI | .02 | .78 | 1.935 | |||||
| FABQ-PA × CES-D | −.13 | .07 | 1.909 | |||||
| BAI × CES-D | .23 | <.01 | 2.451 | |||||
| ADLS | Modal 1: sex, age, height, weight, pain, DA duration, OA severity | .49 | .47 | 7, 174 | <.01 | |||
| Modal 2* | .54 | .51 | 13, 168 | <.01 | ||||
| FABQ-PA | −.13 | .02 | 1.154 | |||||
| BAI | −.35 | <.01 | 2.774 | |||||
| CES-D | −.10 | .16 | 1.986 | |||||
| FABQ-PA × BAI | .04 | .59 | 1.923 | |||||
| FABQ-PA × CES-D | −.03 | .69 | 1.891 | |||||
| BAI × CES-D | .11 | .19 | 2.450 | |||||
| GUAG | Modal 1: sex, ege, height, weight, pain, OA duration, OA severity | .36 | .33 | 7, 171 | <.01 | |||
| Modal 2* | .39 | .34 | 13, 165 | <.01 | ||||
| FABQ-PA | .05 | .43 | 1.142 | |||||
| BAI | −.08 | .43 | 2 785 | |||||
| CES-D | .17 | .06 | 1.984 | |||||
| FABQ-PA × BAI | −.09 | .29 | 1.919 | |||||
| FABQ-PA × CES-D | .08 | .33 | 1.885 | |||||
| BAI × CES-D | −.12 | .20 | 2.453 |
Abbreviations: ADLS, Knee Outcome Survey-Activities of Daily Living Scale; GUAG. Got up and Go test; VIF, variable inflation factor.
Sex, age, height, weight, pain, years with a diagnosis of OA (OA duration), and radiographic severity of OA (OA severity) are controlled.
Significance level for potential confounders.
P value for each predictor variable of interest.
Exploration of the anxiety X depression interaction indicated that the LEFS scores for the high anxiety line remained the same for both low and high conditions of depression (56.6 for low depression and 58.0 for high depression). However, LEFS scores for the high anxiety line reduced from 65.4 to 60.7 when the conditions changed from low to high depression (fig 1).
Fig 1.
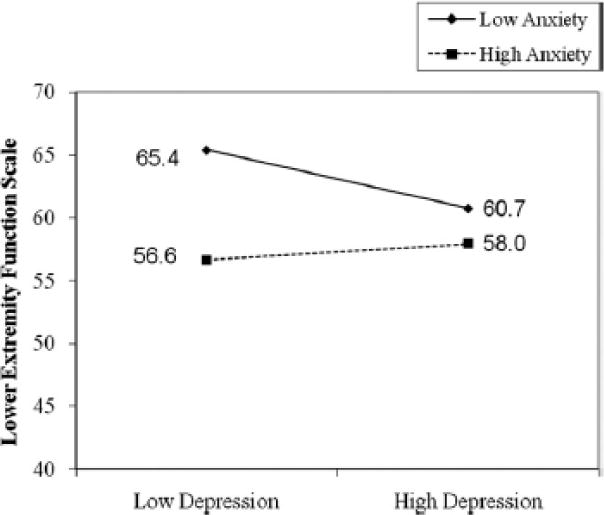
Simple regression line plot of BAI × CES-D interaction on physical function as measured by LEFS. Low and high depression and anxiety were delineated by 1 SD below and above the respective means.
DISCUSSION
Our results indicate that both anxiety and fear-avoidance beliefs are significant associates of self-report physical function in patients with knee OA. Higher anxiety and higher fear avoidance beliefs are independently related to poorer function. These findings were relevant to the Knee Outcome Survey- Activity of Daily Living Scale and the LEFS, but not the WOMAC-PF, in which only anxiety was an associate. The fact that this association was present in 2 of the 3 self-reported function measures provides some stability of this conclusion.
The association of higher anxiety with worse function is in concordance with prior literature3–5 and supports the importance of addressing anxiety in addition to physical impairments in the assessment of patients with knee OA.8–10 One postulated explanation for anxiety’s role in determining function is via a cognitive mechanism in which emotional experiences can trigger the experience of symptoms and perceived function and/or the converse, in which the experience of symptoms and perceived function can trigger emotional experiences.37 While the exact nature of the relationship is not clarified, some research has suggested a link of psychologic factors, including anxiety, to knee pain.8,9,38,39 The experience of pain could predispose to psychologic distress (or increase in psychologic distress), which leads to potential amplification of pain experience.40 Anxiety may account for some variation in reported pain and therefore affect perception of function. Another mechanism, a behavioral mechanism, has been proposed whereby an emotional or catastrophizing anticipation of pain increases the tendency to avoid activities believed to be pain-related, which plays into a cycle of less activity, muscle weakness, and vulnerability of the joint to more damage, pain, and disability.37 Longitudinal studies are needed to help clarify and confirm the relationship of anxiety with function, including examining the potential mediating effect of pain.
Consistent with prior literature in low back pain14, 16 and 1 study on knee OA,11 we found that higher fear-avoidance beliefs were related to worse self-reported function. While these preliminary results do not fully establish the fear-avoidance belief model in knee OA, we are encouraged to examine further the role of fear-avoidance beliefs as an important predictor of function in subjects with knee OA. There have been studies using subjects with low back pain that indicate fear avoidance beliefs can be modified during the course of rehabilitation to improve treatment outcome.41, 42 The interventions are designed to disconfirm the belief that engaging in physical activities will be harmful to the subject. This is done by educating the patients on proper adaptive behaviors versus maladaptive behaviors in response to pain, encouraging subjects to focus their attention on physical activity accomplishments rather than on their level of pain to gauge their progress, instruction in proper ergonomic principles for performing various physical activities, and graded exposure to exercise and fear-producing physical activities in therapy to reduce gradually the fear associated with the performance of these activities.41, 42 This type of approach may also be beneficial for people with knee OA, but the research for this population is limited. Keefe et al43 have described a pain coping training program that is combined with an exercise program for people with knee OA that can improve physical fitness, muscular strength, pain coping, and self efficacy.
Interestingly, depression was not significantly associated in any of our models of self-report function, even though our bivariate correlations and prior literature suggested it might be. Differences in the literature could be related to the use of different measures and outcomes. One of the prior studies that found depression to be a significant predictor found it related only to the Medical Outcomes Study 36-Item Short-Form Health Survey, a generic health measure, and not to the disease- specific WOMAC-PF.12 It is possible that depression has an impact on general health status, but not functional status related specifically to OA. A relatively low incidence of depressive symptoms in our population could also contribute to a lack of finding. Only about 11% of subjects scored 16 or higher on the CES-D, which is the cutoff to suggest clinically significant depressive symptoms. Another possibility is that because anxiety and depression often occur concurrently (they were moderately correlated, p=0.45, in our sample), perhaps anxiety’s effect on function dominates any effect that concurrent depression may have on function.
Additionally, we wondered whether depression might affect function through an interaction with anxiety or fear-avoidance beliefs, which we explored in our analysis. We found a significant anxiety-depression interaction only for the LEFS. In fact, the interaction seemed to apply when LEFS scores were relatively high. For example, when anxiety was high, LEFS scores remained similar, and slightly above the mean, regardless of the condition of depression (fig 1). When anxiety was low, LEFS scores were considerably higher than the mean but worsened as the condition of depression moved from low to high. These findings were not consistent with our hypothesis that combining high anxiety and depression would compound an adverse effect on function. The interaction seems to suggest further that anxiety may be the dominant variable. Although statistically significant, the clinical meaning of this interaction must be interpreted with caution. We must again qualify that only 11% of our sample had significant depression, and it must be acknowledged that perhaps the interaction result would be different if we had greater numbers of subjects with clinically significant depression in our sample.
Bair et al44 reported that when subjects have clinically significant anxiety and depression, they are more adversely affected with regard to musculoskeletal pain and pain-limiting function scores than when clinical anxiety or depression is present alone. In post hoc testing, we classified our subjects into categories depending on the presence or absence of clinically significant anxiety or depression so that we could determine whether our data would exhibit findings similar to those of Bair.44 Subjects were classified as having (1) no anxiety or depression, (2) anxiety only, (3) depression only, and (4) both anxiety and depression. Anxiety was considered present if subjects scored 8 or above on the BAI.45 Depression was considered present if subjects scored 16 or above on the CES-D.25 We performed an analysis of covariance, again controlling for sex, age, height, weight, knee pain, years with a diagnosis of knee OA, and radiographic severity of knee OA, to determine whether there were differences in LEFS scores among the 4 categories.
Table 4 provides the results of this analysis. Subjects with both anxiety and depression occurring simultaneously scored significantly lower than subjects without anxiety or depression, compared with subjects who had only anxiety or depression occurring in isolation. The 16-point difference in LEFS scores between the subjects with combined anxiety and depression and those without either anxiety or depression is also considered clinically significant (the minimum clinically significant difference of LEFS is 9 points). Although it must be recognized that sample size was quite different between the categories, our data do seem to support the finding by Bair44 that when clinically significant anxiety and depression occur simultaneously, there can be an additive adverse effect on function scores.
Table 4.
Comparison LEFS Scores Based on Subject Anxiety end/or Depression Status*
| Anxiety-Depression Status | LEFS Score Mean ± SD | No. |
|---|---|---|
| Mo anxiety or depression | 53.9±134 | 137 |
| Anxiety only | 44.8±12.3 | 25 |
| Depression only | 46.5±12.3 | 4 |
| Both anxiety and depression† | 37.8±16.0 | 16 |
Based on analysis of covariance controlling for sex, age, height, weight, knee pain years with a diagnosis of knee OA. and radiographic severity of knee OA.
Significantly different from subjects with no anxiety or depression, P=.01.
None of the psychologic variables—anxiety, depression, or fear-avoidance beliefs—was significantly related to the performance- based measure of function, the Get Up and Go test, in our model. Our results for anxiety and depression agree with prior literature concerning determinants of performance-based function.4,46 With the proposed decreased activity present in the fear-avoidance model, we expected that we might see a relationship between fear-avoidance beliefs and actual physical tasks; however, this was not the case. We were limited by the fact that we looked only at 1 performance-based measure. While Get Up and Go is a reliable measure, it may not encompass the whole construct of performance-based physical function. The test assesses the ability to rise from a chair, maintain balance, and walk, but these are not the only common functional activities that patients may be faced with on a regular basis. If those activities are not the ones feared as causing pain or harm, then performance of those tasks is likely not affected, even in someone with high fear-avoidance beliefs. Potentially a battery of performance-based measures would better capture the full scope of performance-based lower extremity function. Also, given the modest correlations we found between the self-report and performance-based measures (r range, 0.31–0.37), it is likely that the performance-based and self-reported functions measure different aspects of the construct physical function, and therefore, it is not surprising that they are affected differently by psychologic variables.
Study Limitations
The cross-sectional design of this study is a limitation. While we can discuss the associations we found, we cannot imply causality. Longitudinal analyses are necessary to explain further and confirm the presented associations. Additionally, there are other behavioral factors, such as self-efficacy and coping skills, that are important to consider, but we did not have the data to examine them. Keefe et al47 have reported that some subjects with knee OA who do not have effective coping skills engage in pain catastrophizing, an irrational view that the pain represents a much greater threat of harm or injury than is actually the case, which can also alter their lifestyles and ability to function. Unfortunately, we did not have pain catastrophizing data included in our study. It would be interesting to determine whether pain catastrophizing mediates the relationship between fear-avoidance beliefs and anxiety with function.
Another potential limitation is that the modifications of the FABQ-PA for use in patients with knee pathology have not been formally validated, to our knowledge. Without this formal validation, one can question the degree of accuracy for our estimates of the effects of fear on function in this study. We did report a reasonable degree of internal consistency in our sample (Cronbach a=.75), which provides evidence for reliability, but further study is needed to validate this modification more completely.
CONCLUSIONS
Anxiety and fear-avoidance beliefs are associated with selfreport function in patients with knee OA. The results of our study add further support to the notion that psychologic variables can influence the perception of functional ability in people with knee OA. Our findings did not support the notion that the psychologic variables may interact to produce an even greater adverse effect on physical function. Continued investigation is needed to determine whether anxiety and fear-avoidance beliefs adversely influence the outcome of rehabilitation programs designed to improve physical function.
List of Abbreviations
- BAI
Beck Anxiety Inventory
- CES-D
Center for Epidemiological Studies Depression Scale
- FABQ-PA
Fear Avoidance Belief Questionnaire-Physical Activity Scale
- ICC
intra-class correlation coefficient
- LEFS
Lower Extremity Function Scale
- OA
osteoarthritis
- WOMAC
Western Ontario and McMaster Universities
- WOMAC-PF
Western Ontario and McMaster Universities Osteoarthritis Index- Physical Function Subscale
Footnotes
Presented to the Association for Rheumatological Health Professions, October 26, 2008, San Francisco, CA.
References
- 1.Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991–94. J Rheumatol. 2006;33:2271–9. [PubMed] [Google Scholar]
- 2.Hurley MV, Rees J, Newham DJ. Quadriceps function, proprioceptive acuity, and functional performance in healthy young, middle-aged, and elderly subjects. Age Ageing. 1998;27:55–62. doi: 10.1093/ageing/27.1.55. [DOI] [PubMed] [Google Scholar]
- 3.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–95. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 4.Sharma L, Cahue S, Song J, Hayes KC, Pai Y-C, Dunlop DD. Physical functioning over three years in knee osteoarthritis: role of psychological, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48:3359–70. doi: 10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- 5.Fitzgerald GK, Piva SR, Irrgang JJ, Bouzubar F, Starz TW. Quadriceps activation failure as a moderator of the relationship between quadriceps strength and physical function in individuals with knee osteoarthritis. Arthritis Care Res. 2004;51:40–8. doi: 10.1002/art.20084. [DOI] [PubMed] [Google Scholar]
- 6.Fitzgerald GK, Piva SR, Irrgang JJ. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Care Res. 2004;51:941–6. doi: 10.1002/art.20825. [DOI] [PubMed] [Google Scholar]
- 7.Woods L, Peat G, Thomas E, Hay EM, Sim J. Associations between physical examination and self-reported physical function in community dwelling older adults with knee pain. Phys Ther. 2008;88:1–10. doi: 10.2522/ptj.20060372. [DOI] [PubMed] [Google Scholar]
- 8.Summers MN, Haley WE, Reveille JD, Alarcon GS. Radiographic assessment and psychologic variables as predictors of pain and functional impairment in osteoarthritis of the knee or hip. Arthritis Rheum. 1988;31:204–9. doi: 10.1002/art.1780310208. [DOI] [PubMed] [Google Scholar]
- 9.Salaffi F, Cavalieri F, Nolli M, Ferraccioli G. Analysis of disability in knee osteoarthritis: relationship with age and psychological variables but not with radiographic score. J Rheumatol. 1991;18:1581–6. [PubMed] [Google Scholar]
- 10.Creamer P, Lethbridge-Cejku M, Hochberg MC. Factors associated with functional impairment in symptomatic knee osteoarthritis. Rheumatology (Oxford) 2000;39:490–6. doi: 10.1093/rheumatology/39.5.490. [DOI] [PubMed] [Google Scholar]
- 11.Heuts PH, Vlaeyen JW, Roelofs J, et al. Pain-related fear and daily functioning in patients with osteoarthritis. Pain. 2004;110:228–35. doi: 10.1016/j.pain.2004.03.035. [DOI] [PubMed] [Google Scholar]
- 12.Maly MR, Costigan PA, Olney SJ. Determinants of self-report outcome measures in people with knee osteoarthritis. Arch Phys Med Rehabil. 2006;87:96–104. doi: 10.1016/j.apmr.2005.08.110. [DOI] [PubMed] [Google Scholar]
- 13.Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30:77–94. doi: 10.1007/s10865-006-9085-0. [DOI] [PubMed] [Google Scholar]
- 14.Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of painrelated fear in chronic back pain disability. Pain. 1999;80:329–39. doi: 10.1016/s0304-3959(98)00229-2. [DOI] [PubMed] [Google Scholar]
- 15.Denison E, Asenlof P, Lindberg P. Self-efficacy, fear avoidance, and pain intensity as predictors of disability in subacute and chronic musculoskeletal pain patients in primary health care. Pain. 2004;111:245–52. doi: 10.1016/j.pain.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 16.George SZ, Fritz JM, McNeil DW. Fear-avoidance beliefs as measured by the fear-avoidance beliefs questionnaire: change in fear-avoidance beliefs questionnaire is predictive of change in self-report of disability and pain intensity for patients with acute low back pain. Clin J Pain. 2006;22:197–203. doi: 10.1097/01.ajp.0000148627.92498.54. [DOI] [PubMed] [Google Scholar]
- 17.Depression. National Institute of Mental Health. 2009 Available at: http://www.nimh.nih.gov/health/topics/depression/index.shtml Accessed August 11, 2009.
- 18.Knee stability training in individuals with knee osteoarthritis. National Institutes of Health Clinical Trial Registry. 2009 Available at: http://www.clinicaltrials.gov/ct2/show/NCT00078624?term_osteoarthritis&rank_14. Accessed August 11, 2009.
- 19.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Arthritis Rheum. 1986;29:1039–49. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 20.Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wadell G, Newton M, Henderson I, Somerville D, Main CJ. A fear-avoidance beliefs questionnaire (FABQ) and the role of fearavoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–68. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 22.van Baar ME, Dekker J, Oostendorp RA, et al. The effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee; a randomized clinical trial. J Rheumatol. 1998;25:2432–9. [PubMed] [Google Scholar]
- 23.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psych. 1988;56:893–7. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 24.Beck AT, Steer RA, Ball R, Ciervo CA, Kabat M. Use of the Beck Anxiety and Depression Inventories for primary care with medical outpatients. Assessment. 1997;4:211–9. doi: 10.1177/107319119700400301. [DOI] [PubMed] [Google Scholar]
- 25.Radloff LS. The CES-D scale: a self-report depression scale for research in a general population. Appl Psychol Measurement. 1977;1:385–401. [Google Scholar]
- 26.Turk DC, Okifujie A. Detecting depression in chronic pain patients: adequacy of self-reports. Behav Res Ther. 1994;32:9–16. doi: 10.1016/0005-7967(94)90078-7. [DOI] [PubMed] [Google Scholar]
- 27.Weissman MM, Sholomksas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106:203–14. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 28.Bellamy N, Watson-Buchanan W, Goldsmith CH, Campbell J. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–40. [PubMed] [Google Scholar]
- 29.Bellamy N, Kean WF, Buchanan WW, Gerecz-Simon E, Campbell J. Double blind randomized controlled trial of sodium meclofenamate (Meclomen) and diclofenac sodium (Voltaren): post validation reapplication of the WOMAC osteoarthritis index. J Rheumatol. 1992;19:153–9. [PubMed] [Google Scholar]
- 30.Hawker G, Melfi C, Paul J, Green R, Bombardier C. Comparison of a generic (SF-36) and disease specific (WOMAC) instrument in the measurement of outcomes after knee replacement surgery. J Rheumatol. 1995;22:1193–6. [PubMed] [Google Scholar]
- 31.Jaeschke RS, Guyatt GH. Measurement of health status: ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407–15. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- 32.Ehrich EW, Davies GM, Watson DJ, Bolognese JA, Seidenberg BC, Bellamy N. Minimal perceptible clinical improvement with the Western Ontario and McMaster Universities osteoarthritis index questionnaire and global assessments in patients with osteoarthritis. J Rheumatol. 2000;27:2635–41. [PubMed] [Google Scholar]
- 33.McConnell S, Kolopack P, Davis AM. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum. 2001;45:453–61. doi: 10.1002/1529-0131(200110)45:5<453::aid-art365>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 34.Binkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. Phys Ther. 1999;79:371–83. [PubMed] [Google Scholar]
- 35.Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80-A:1132–45. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Piva SR, Fitzgerald GK, Irrgang JJ, Bouzubar F, Starz TW. Get Up and Go Test in patients with knee osteoarthritis. Arch Phys Med Rehabil. 2004;85:284–9. doi: 10.1016/j.apmr.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 37.Dekker J, Boot B, van der Woude LH, Bijlsma JW. Pain and disability in osteoarthritis: a review of biobehavioral mechanisms. J Behav Med. 1992;15:189–214. doi: 10.1007/BF00848325. [DOI] [PubMed] [Google Scholar]
- 38.Creamer P, Lethbridge-Cejku M, Costa P, Tobin JD, Herbst JH, Hochberg MC. The relationship of anxiety and depression with self-reported knee pain in the community: data from the Baltimore Longitudinal Study of Aging. Arthritis Care Res. 1999;12:3–7. doi: 10.1002/1529-0131(199902)12:1<3::aid-art2>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 39.Creamer P, Lethbridge-Cejku M, Hochberg MC. Determinants of pain severity in knee osteoarthritis: effect of demographic and psychosocial variables using 3 pain measures. J Rheumatol. 1999;26:1785–92. [PubMed] [Google Scholar]
- 40.Creamer P, Hochberg MC. The relationship between psychosocial variables and pain reporting in osteoarthritis of the knee. Arthritis Care Res. 1998;11:60–5. doi: 10.1002/art.1790110110. [DOI] [PubMed] [Google Scholar]
- 41.George SZ, Fritz JM, Bialosky JE, Donald DA. The effect of a fear-avoidance-based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine. 2003;28:2551–60. doi: 10.1097/01.BRS.0000096677.84605.A2. [DOI] [PubMed] [Google Scholar]
- 42.Woods MP, Asmundson GJ. Evaluating the efficacy of graded in vivo exposure for the treatment of fear in patients with chronic back pain: a randomized controlled clinical trial. Pain. 2008;136:271–80. doi: 10.1016/j.pain.2007.06.037. [DOI] [PubMed] [Google Scholar]
- 43.Keefe FJ, Blumenthal J, Baucom D, et al. Effects of spouseassisted coping skills training and exercise training in patients with osteoarthritic knee pain: a randomized controlled study. Pain. 2004;110:539–49. doi: 10.1016/j.pain.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 44.Bair MJ, Wu J, Damush TM, Sutherland JM, Kroenke K. Association of depression and anxiety alone and in combination with musculoskeletal pain in primary care patients. Psychosom Med. 2008;70:890–7. doi: 10.1097/PSY.0b013e318185c510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Beck AT, Steer RA. Beck Anxiety Inventory manual. San Antonio: Psychological Corp; 1993. [Google Scholar]
- 46.Maly MR, Costigan PA, Olney SJ. Contribution of psychosocial and mechanical variables to physical performance measures in knee osteoarthritis. Phys Ther. 2005;85:1318–28. [PubMed] [Google Scholar]
- 47.Keefe FJ, Kashikar-Zuck S, Opiteck J, Hage E, Dalrymple L, Blumenthal JA. Pain in arthritis and musculoskeletal disorders: the role of coping skills training and exercise interventions. J Orthop Sports Phys Ther. 1996;24:279–90. doi: 10.2519/jospt.1996.24.4.279. [DOI] [PubMed] [Google Scholar]


