Abstract
Text-messaging interventions present a novel approach for targeting high-risk men who have sex with men (MSM) who may not respond to or may be difficult to reach for face-to-face or site-based interventions. Project Tech Support (N = 52) was an open label pilot study testing the feasibility and utility of a text-messaging intervention to reduce methamphetamine use and high-risk sexual behaviors among out-of-treatment MSM. Participants in the two-week intervention received social support and health education text messages transmitted in real-time. At follow-up, there were significant decreases in frequency of methamphetamine use and unprotected sex while on methamphetamine (both p < .01), and a significant increase in self-reported abstinence from methamphetamine use (13.3% vs. 48.9%; p<.001). Additionally, participants reported reductions of unprotected anal intercourse with HIV-positive partners (p < .01); with HIV-negative partners, participants reported fewer insertive and receptive episodes (both p < .05). Findings demonstrate that text messaging is a promising intervention for reaching and potentially changing HIV high-risk behaviors among out-of-treatment, methamphetamine-using MSM.
Keywords: MSM, methamphetamine, HIV, text messaging, mobile communication technology
Introduction
Men who have sex with men (MSM) is the only risk category in the United States in which HIV infections have continued to steadily increase since the early 1990s [1]. Nationally, 64.3% of adult and adolescent males living with HIV/AIDS were exposed to HIV through male-to-male sexual contact [2]. Among this population, substance-using MSM – particularly methamphetamine-using MSM – are at significantly greater risk of HIV acquisition and transmission than any other behavioral risk group, as these men often engage in concurrent drug and sexual HIV-risk behaviors [3,4].
Methamphetamine use is highly integrated into gay male socio-sexual contexts, such as circuit parties, sex clubs, and bathhouses [5–9]. In Los Angeles County, approximately 11% of MSM report using methamphetamine in the previous twelve months [10], 20 times the prevalence in the general population [11]. The association between methamphetamine use and increased risk of HIV infection among MSM is apparent: the prevalence of HIV infection among MSM methamphetamine users increases as methamphetamine use moves from occasional use, to recreational use, to chronic abuse due to users concurrently engaging in high-risk sexual behaviors [4].
A variety of approaches have been undertaken to reduce methamphetamine use among MSM such as motivational interviewing [12,13], cognitive behavioral therapy [13–16], contingency management [15,17], and many of the evidence-based interventions listed in the CDC-compendium [18]. These interventions have varied in intensity, theoretical foundation and demand for resources. Internet, text messaging and other technology-based interventions present promising new ways to reach MSM who may not access or respond to face-to-face interventions [19–22]. One challenge is that face-to-face interventions typically require participants to adhere to a predetermined schedule for counseling or group sessions and this time commitment can present difficulties for methamphetamine-using MSM. In contrast, technology-based interventions can offer HIV prevention information in a manner that is convenient, confidential and can be carried out in real time; in other words, instantaneously. Thus, real time interventions occur at the times when a person is most likely to consider engaging in high-risk behaviors and when face-to-face contact is often not feasible [23]. Technology-based interventions also offer greater anonymity and may be implemented at a lower cost [24,25]. A communication technology particularly well suited to real-time technology-based interventions is short messaging service (SMS), also commonly known as text messaging or texting. SMS text messaging allows for instantaneous delivery of messages with a maximum of 160 characters directly to individuals at nearly any time, place, or setting [26].
A 2009 review [27] of behavior change interventions delivered by text message concluded that in developed countries, use of text messaging is commonplace across diverse age groups, cultures and socioeconomic backgrounds. Text-messaging interventions have effectively impacted a wide range of health issues such as smoking cessation [28–30], diabetes self-management [31–35], HIV medication adherence [36–38], hepatitis vaccination [39], and bulimia nervosa [40]. Studies promoting sexual health have used text messages for communication between sexual health clinics and patients [20,41], partner notification and sexual contact tracing [42], contraception reminders [43], and sexual health promotion and education [22,41,44] with promising results.
Studies using text messaging have varied in design. Some studies used only scripted messages such as scheduled medication reminders [20]. Another advertised a phone number and a text code to identify the topic the participant was requesting information on such as “text 2442 if you want info on where to get free condoms in your area.” The participants then received text information and referrals relative to that topic [34]. Incoming messages can also be answered extemporaneously by a health professional or by a computer that responds with a predetermined (scripted) response based on keywords in the message [23]. Other interventions have used a combination of extemporaneous and scripted health-promoting messages [21,45]. Scripted messages can be tailored based on the most current information provided by participants [21,46] and can be scheduled to be delivered en masse at the times when people are likely to be making choices about potentially high-risk behaviors. When used this way, scripted messages can be a source of support and information without requiring a dialogue. However, holding a dialogue in real-time can also be of crucial importance to influencing sexual and drug risk behaviors [47]. Real-time extemporaneous text messaging transmitted by trained interventionists provides an advantageous opportunity to create an immediate response at a critical time, which is not possible with scripted messages.
Gay consumers have been identified as being among the earliest adopters of information technology communications [48] making them an ideal population for technology-based interventions. In an HIV medication adherence study using text messaging, gay and lesbian participants were more likely to respond to text messages than heterosexual or bisexual participants [45]. It is important to continue to investigate theory-based text messaging as a mode of delivery for HIV prevention interventions and to continue testing systematic programs with one- and two-way communication capacity, especially given the promising results of recent text-messaging interventions among populations of MSM [19,45]
The report that follows describes outcomes from Project Tech Support, a pilot study testing the feasibility and utility of a real-time text-messaging intervention to reduce methamphetamine use and high-risk sexual behaviors among out-of-treatment MSM in Los Angeles County. We hypothesized that brief interventions using text messaging could be delivered successfully to reduce methamphetamine use and concomitant sexual risk behaviors.
Methods
The Institutional Review Boards from both the research institute and the funding agency approved the study and provided oversight for all study activities.
Participants
Participants were recruited from October 2008 to May 2009 through a multi-level, community-wide effort targeting out-of-treatment, methamphetamine-using MSM. The collaborative partners included 15 community-based organizations, seven commercial sex venues, and three local governmental bodies. Outreach venues included bathhouses, sex clubs, bars and street outreach. Additionally, flyers and club cards were distributed at gay pride and other community events and at collaborating community-based agencies. Internet recruitment was utilized via Craigslist.org and the study website, and advertisements were placed in local gay magazines.
Potential participants were deemed eligible for the study if they identified as male, were between the ages of 18 and 65 years, had unprotected anal intercourse with a non-primary male partner in the previous two months, used methamphetamine in the previous two months, were not currently in or seeking drug treatment, had not received a HIV-positive diagnosis in the previous six months, were a current resident of Los Angeles County not planning to move outside of Los Angeles County in the next five months, were willing to provide informed consent, agreed to comply with study procedures, and were willing to participate in a two-week text-messaging intervention. Individuals were excluded if they did not meet all criteria or were unable to understand the informed consent document.
Procedure
Potential participants interested in Project Tech Support called the study phone number for a brief pre-screening; those eligible were scheduled for an intake appointment within two-to-three days. At intake, potential participants were rescreened and those eligible began the informed consent process, completed an audio computer-assisted self-interview (ACASI) baseline assessment, received a urinalysis test to assess recent drug use, and a rapid oral HIV antibody test. Follow-up evaluations were conducted two months following the two-week test-messaging intervention. Participants were compensated $25 upon completion of the intake and baseline assessment, and $50 for completing the follow-up evaluation. Additionally, at the completion of the intervention, participants were allowed to keep the mobile text-messaging device.
After the baseline ACASI assessment, participants were given a T-Mobile Sidekick (a cellular phone that was commonly used for text messaging at the time of the study) and received an orientation to the text-messaging intervention. Orientation included an explanation of the text-messaging device and on the types of messages the participants would receive. Participants were asked five brief questions regarding their methamphetamine use, which served to help the research staff to specifically tailor text messages (e.g., “Where do you use meth? At home? At a club or bar? At a bathhouse or sex club?”). Participants were informed that messages may be transmitted to the study staff at any time; however, they should expect to receive a response only during active study hours, which were Monday and Tuesday 12:00 PM to 8:00 PM, Wednesday and Thursday 12:00 PM to 1:00 AM, Friday 12:00 PM to 2:00 AM, Saturday 3:30 PM to 2:00 AM, and Sunday 3:30 PM to 12:00 AM. Study hours were determined during the formative stage [21] as those when high-risk activity was most likely to occur. Participants were shown a list of community referrals for services that were pre-programmed into the text-messaging device and were given instructions on how to access the referral list. Prior to the participant receiving a text-messaging unit, the device was checked and tested to ensure the unit was working properly.
Intervention
Following baseline, participants engaged in a two-week text-messaging intervention with study staff; a thorough description of the development of the intervention is presented elsewhere [21]. Social support and health education messages were transmitted in real-time. Once the participant received their device, within 30 minutes of leaving the study site, they were sent a welcome message. This initial message was not a risk-reduction message, but included a prompt asking the participant to respond. For example, “Thx 4 ur participation! Text us w/?s” or “Would like 2 hear from U, hit us up.”
For the first three days of the intervention, following the initial welcome message, the participant received a minimum of one and a maximum of three pre-written risk-reduction messages per day. If a participant did not respond to any of the risk-reduction messages during the first three days of the intervention, they received a minimum of one and a maximum of two pre-written risk-reduction messages per day for the next three days. If a participant did not respond after six days the pre-written risk-reduction text messages were reduced to one message per day until either the participant responded or the end of the two-week intervention period. All pre-written risk-reduction messages to non-responders were sent during the hours of 12:00 PM and 12:00 AM. The intent of this “step-down” process was to maintain some communication while, at the same time, safeguard participants who are passive non-responders.
Study participants who responded to the pre-written risk-reduction messages were sent real-time text messages back from the research staff during active study hours. To maintain consistency between text-messaging correspondences, the research staff placed an upper limit on each “text messaging conversations” of approximately 20 messages sent per party (i.e., 20 messages from the staff to the participant and 20 messages from the participant to the staff), or 40 messages total per conversation. The research staff engaged in a maximum of four “text messaging conversations” per day, per participant. However, if a participant requested a referral toward the end of the “text messaging conversation,” the conversation was not aborted but, rather, the referral was given.
During the formative stage of the study, 400 text messages were developed based on the behavioral change theories of Social Support Theory (such as, “PNP? Drink water, remember ur limits” or “Mix & match ur clothes, not ur drugs”), Health Belief Model (such as, “Get his #, not his STD” or “Don’t brush ur teeth 2 hrs B4 sex”), and Social Cognitive Theory (such as, “HIV is not a gift, disclose ur status” or “Think about ur choices, R they rite 4 U?”) [21]. Pre-written text messages were categorized in the computer database, by their theoretical base and by participant profile (e.g., HIV status, whether a participant went online to hookup, whether a participant frequented a commercial sex venue). Based on their responses to the five brief questions regarding their methamphetamine use administered at baseline as well as their text-messaging conversations, participants received messages that fit their profile. During the two-week intervention, social support and health education extemporaneous text messages were easily integrated with the pre-written text messages.
Following the two-week intervention period, all study participants, whether responsive or non-responsive, received one pre-written “stay in touch” message per week. These “stay in touch” messages were also used to schedule the two-month follow-up evaluation. Additionally, participants were sent a reminder message (such as, “We have ur appt set for ____, is that still ok 4 u?” or “UR follow up appt is _____, C U then!”) or received a phone call one day prior to their scheduled two-month follow-up evaluation.
Staff Training
The staff delivering the intervention was ethnically diverse and reflected the study’s target population, i.e., all identified as gay men and most were former methamphetamine users. To adequately conduct the study during the late night and early morning hours that were necessary to deliver the intervention during real time, four part-time staff – rather than two full-time staff – were hired. Prior to conducting the intervention, each staff received certification for working with human subjects and were trained extensively on all study procedures, including an understanding of the behavioral change theories on which the pre-written text messages were based, establishing trust and rapport with participants, the ACASI assessment, and providing culturally appropriate referrals. Research staff were also trained on delivering the appropriate pre-written messages and how to respond and provide social support and health education messages for any related requests for information the scripted messages did not address. The staff was instructed to memorize the pre-written text messages so these messages could be naturally integrated into the text conversations. Research staff “mocked” text conversations with other staff and all study procedures were observed by the Project Director until proficiency was demonstrated.
Assessments
Core Assessment
An ACASI core assessment gathered information on demographic characteristics, drug and alcohol use, injection patterns, sexual risk behaviors, mental health status, social networks, social support, health beliefs and self-efficacy. The specific primary outcomes analyzed from baseline to follow-up include Likert-style items such as “In the last two months, how often have you used methamphetamine?”, or behavior recall items such as “How many times have you had anal sex with your non-primary male partner in the last 2 months?”, and can be found in Tables 2 and 3. The core assessment was self-administered by respondents in a private room using a laptop computer equipped with audio headphones and took approximately 45 minutes to complete. Research staff remained in close proximity to assist with any technical problems or concerns. The computer program moved through the sections automatically and let the participant know when the interview was completed. The ACASI was administered at baseline and two-month follow-up evaluations.
Table 2.
Methamphetamine Use Outcomes
| Baseline N and % (N=52) |
Follow-Up N and % (N=48) |
||||
|---|---|---|---|---|---|
| How Often Participant Uses Methamphetamine*** (n= 28) | |||||
| < Once a Month | 0 | 0.0% | 7 | 25.0% | |
| Once a Month | 1 | 3.6% | 1 | 3.6% | |
| 2–3 Days a Month | 8 | 28.6% | 10 | 35.7% | |
| Once a Week | 3 | 10.7% | 3 | 10.7% | |
| 2–3 Days a Week | 12 | 42.9% | 5 | 17.9% | |
| 4–6 Days a Week | 2 | 7.1% | 1 | 3.6% | |
| Every Day | 2 | 7.1% | 1 | 3.6% | |
| Length of Time Since Last Used Methamphetamine** (n = 45) | |||||
| Day(s) | 20 | 39.2% | 17 | 37.8% | |
| Week(s) | 23 | 45.% | 9 | 20.0% | |
| Month(s) | 2 | 3.9% | 19 | 42.2% | |
| Year(s) | 0 | 0.0% | 0 | 0.0% | |
| Injected Methamphetamine in Previous 2 Months* (n = 48) | |||||
| Yes | 10 | 20.8% | 4 | 8.3% | |
| Stopped Having Unprotected Sex on Methamphetamine** (n = 43) | |||||
| Yes | 9 | 20.9% | 19 | 44.2% | |
| Stopped Using Methamphetamine*** (n = 45) | |||||
| Yes | 6 | 13.3% | 22 | 48.9% | |
p < .05;
p < .01;
p < .001
Table 3.
Unprotected Anal Sex with Primary/Non-Primary Male Partners in the Previous Two Months
| Primary Partner HIV Status | Baseline Mean (SD) |
Follow-Up Mean (SD) |
|
|---|---|---|---|
| HIV positive | (n = 9) | (n = 5) | |
| # of Times as “Top” | 2.2 (3.4) | 3.6 (6.4) | |
| … while on Alcohol | 1.3 (3.3) | 1.8 (3.5) | |
| … while on Drugs | 1.9 (3.4) | 2.4 (4.8) | |
| # of Times as “Bottom” | 7.7 (8.6) | 4.2 (8.8) | |
| … while on Alcohol | 5.6 (7.6) | 3.2 (6.6) | |
| … while on Drugs | 5.1 (6.6) | 3.2 (6.6) | |
| HIV negative | (n = 6) | (n = 6) | |
| # of Times as “Top” | 10.5 (15.0) | 4.5 (6.4) | |
| … while on Alcohol | 8.0 (13.4) | 2.7 (3.9) | |
| … while on Drugs | 8.3 (15.7) | 4.2 (5.6) | |
| # of Times as “Bottom” | 8.3 (18.1) | 2.3 (2.7) | |
| … while on Alcohol | 3.3 (6.1) | 1.4 (2.2) | |
| … while on Drugs | 3.3 (6.1) | 1.6 (1.7) | |
| HIV Status Unknown | (n = 4) | (n = 0) | |
| # of Times as “Top” | 9.3 (4.8) | 0.0 (0.0) | |
| … while on Alcohol | 3 (2.7) | 0.0 (0.0) | |
| … while on Drugs | 7.8 (4.2) | 0.0 (0.0) | |
| # of Times as “Bottom” | 2 (2.5) | 0.0 (0.0) | |
| … while on Alcohol | 1.5 (2.4) | 0.0 (0.0) | |
| … while on Drugs | 1.8 (2.4) | 0.0 (0.0) | |
|
| |||
| Non-Primary Partner HIV Statusa | |||
|
| |||
| HIV positive | (n = 48) | ||
| # of Partners** | 4.4 (6.8) | 1.9 (4.4) | |
| # of Times as “Top” | 2.7 (5.0) | 1.8 (4.1) | |
| # of Times as “Bottom”* | 3.7 (8.1) | 1.2 (2.4) | |
| # of Partners while on Alcohol | 2.3 (5.2) | 0.9 (3.6) | |
| # of Partners while on Drugs** | 3.4 (5.2) | 1.6 (4.1) | |
| HIV negative | (n = 48) | ||
| # of Partner** | .9 (1.9) | 0.2 (0.8) | |
| # of Times as “Top”** | 0.7 (1.7) | 0.2 (0.6) | |
| # of Times as “Bottom”* | 0.7 (2.3) | 0.0 (0.2) | |
| # of Partners while on Alcohol* | 0.5 (1.3) | 0.1 (0.5) | |
| # of Partners while on Drugs** | 0.8 (1.5) | 0.2 (0.5) | |
p < .05;
p < .01
Categories are not mutually exclusive (participants could have multiple non-primary partners).
Urine Drug Screen
Urine samples were collected, monitored and analyzed onsite at baseline and two-month follow-up evaluation using a five-panel FDA-approved urine test cup (Phamatech, Inc., San Diego, CA). The test cup screened for metabolites of the following drugs of abuse at the noted cut-off levels: Amphetamine (1000 ng/mL), Cocaine (300 ng/mL), Methamphetamine (500 ng/mL), Opiate (300 ng/mL), and THC (50 ng/mL). Results are coded qualitatively (above or below threshold). In addition to the urinalyses, participants were also asked to self-report their recent substance use via the ACASI.
Oral Rapid HIV-antibody Test
Participants received an oral rapid HIV-antibody test (OraQuick) at baseline only; tests were administered by research staff certified as a HIV testing counselor. Participants who showed documentation of a HIV-positive serostatus, which could include a prescription for antiretroviral medication, were not given a HIV-antibody test. Participants who tested preliminary positive on the rapid test were immediately referred to a local community clinic for a confirmatory test and were offered local healthcare and social support referrals. Pursuant to the eligibility criteria these participants were deemed ineligible for study participation.
Statistical Analyses
Participant sociodemographic characteristics, methamphetamine use, and high-risk sexual behaviors were compared from baseline (N=52) to follow-up (n=48) evaluation. All primary outcome variables can be found in Tables 2 and 3; variables in Table 2 are measured as indicated by the measurement categories indicated, and all variables found in Table 3 are measured as “counts” of behavior in the previous two months. Wilcoxon sign rank tests of equivalence are applied to comparisons of ordinal variables (e.g., frequency of methamphetamine use, length of time since last use), while paired t-tests are used to test for significant differences between baseline and follow-up mean scores for all remaining analyses but those referencing sexual behaviors with primary partners (upper half of Table 3). These analyses used unpaired t-tests due to the nature of the data (wholly different participants qualified for response to the question at baseline than at follow-up). Missing data are noted in the tables. All significance tests are two-tailed. All data was analyzed using Stata 10SE [49].
Results
Study Progress and Retention
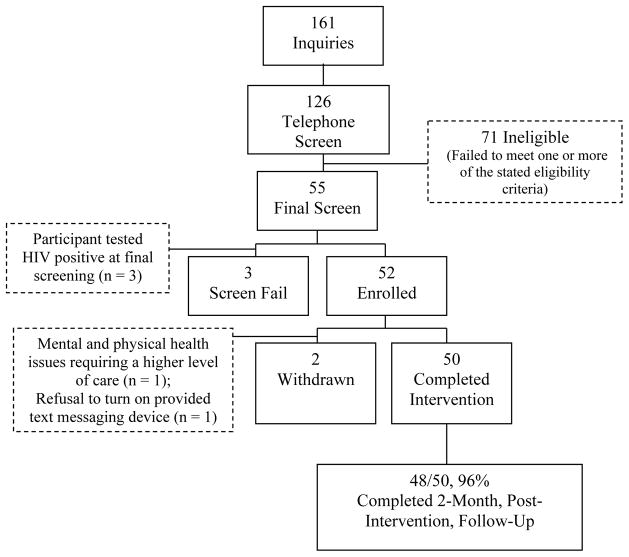
Between October 2008 and May 2009, 52 participants enrolled in the study (see Figure 1). Study progress and retention are shown in Figure 1.
Figure 1. Project Tech Support.
Study Progress and Retention
Sociodemographic Characteristics
Participants reported a median age of 36 years (IQR=30–42.5). Racial/ethnic categories were predominantly Hispanic/Latino (38.5%), Caucasian/white (34.6%), and African American/black (21.2%). Most participants identified as gay (80.8%). The majority of participants had a high school/GED equivalent education (86.5%), and most participants were unemployed (73.1%). Considering all sources of monetary gain (e.g., legal employment, welfare, sex work), participants reported a median annual income of $15,000 (IQR=$5,000-$15,000). Over half of participants (59.6%) were HIV infected at baseline and nearly a third (28.9%) were homeless.
Methamphetamine Use
Participants reported significant decreases in the frequency of methamphetamine use in the previous two months (range = 1, 7) from baseline to follow-up (Wilcoxon z=3.53; p < .001). The modal response category changed from “2–3 Days a Week” at baseline to “2–3 Days a Month” at follow-up evaluation. Additionally, participants reported a significant increase in the length of time since their last use of methamphetamine (range = 0, 3) from baseline to follow-up (Wilocoxon z=−2.95 ; p < .01). Although not significant, urinalysis results showed a reduction in the number of participants testing positive for recent methamphetamine metabolites (use within 40 to 72 hours) from baseline to follow-up (42.3% vs. 39.5%; ns), supporting the self-reported data.
Significantly fewer participants reported having injected methamphetamine in the previous two months at follow-up than at baseline (20.8% vs. 8.3%; t=2.21, p < .05). Additionally, of those respondents who reported some lifetime engagement in unprotected sex while on methamphetamine, significantly more participants reported that they had stopped having unprotected sex while on methamphetamine during this same time period (20.9% vs. 44.2%; t=−2.89, p < .01). Lastly, significantly more participants at follow-up than at baseline reported having stopped using methamphetamine altogether (13.3% vs. 48.9%; t =−4.51, p < .001).
Sexual Behaviors and HIV Status
Table 3 details participants’ unprotected sexual behaviors with primary and non-primary partners in the previous two months. The table presents the data stratified first by partner type (i.e., primary vs. non-primary), and then by the HIV status of that partner. Participants with HIV-negative primary partners decreased their number of sexual risk behaviors for all measured behavioral categories. For participants with HIV-positive primary partners, participants decreased unprotected receptive anal intercourse and increased unprotected insertive anal intercourse. None of the observed changes in unprotected sex with primary partners were statistically significant. It is also important to note that although at baseline some participants reported they did not know their primary partner’s HIV status, there were no participants at follow-up that did not know their primary partner’s HIV status.
Participants reported having unprotected anal intercourse with significantly fewer HIV-positive non-primary partners from baseline to follow-up (4.4 [6.8] vs. 1.9 [4.4]; t=2.92, p < .01). While participants did not report significantly fewer times of unprotected insertive anal intercourse with HIV-positive non-primary partners (p = .1), they did report significantly fewer times of unprotected receptive anal intercourse (3.7 [8.1] vs. 1.2 [2.4]; t=2.27, p < .05). Additionally, participants showed a significant reduction in number of non-primary HIV-positive partners when using drugs (t=2.78, p < .01), and reductions in number of HIV-positive non-primary partners while on alcohol is trending towards significance (t=1.87, p = .067).
Number of HIV-negative non-primary unprotected anal sex partners significantly decreased from baseline to follow-up (0.9 [1.9] vs. 0.2 [0.8]; t=2.79, p < .01). Participants reported significantly fewer sexual encounters where they were the insertive partner (0.7 [1.7] vs. 0.2 [0.6]; t=2.72, p < .01), and significantly fewer sexual encounters where they were the receptive partner (0.7 [2.3] vs. 0.0 [0.2]; t=2.0, p ≤.05). Lastly, participants reported fewer HIV-negative non-primary partners with which they had unprotected anal sex while using substances. For alcohol use, the number of HIV-negative non-primary partners reduced significantly (0.5 [1.3] vs. 0.1 [.5]; t=2.28, p < .05), with similar reductions in HIV-negative non-primary partners observed in drug use (0.8 [1.5] vs. 0.2 [0.5]; t=3.38, p < .01).
Discussion
The use of a text-messaging intervention for out-of-treatment methamphetamine-using MSM appears to be feasible and acceptable as a HIV prevention strategy. Project Tech Support was conducted with 52 members of the target population and achieved a follow-up rate of 96%, further demonstrating the feasibility of conducting a text-messaging intervention with highly impacted populations under experimental conditions. The findings presented here demonstrate that this novel text-messaging intervention is a culturally competent intervention for methamphetamine-using MSM and an innovative way to reach them in real time when they are most likely to make high-risk drug and sexual decisions and are in need of referrals and support.
Participants achieved significant reductions in methamphetamine use during the course of the intervention. Frequency of use, injection use, unprotected sex while high, and overall methamphetamine use prevalence all decreased, while the average time interval between episodes of use increased. The ability of an intervention to reduce methamphetamine use is crucial when dealing with methamphetamine-using MSM populations, given the high prevalence of use in this population [50–52], and its intimate connection to HIV risk behavior [9,53,54]. It is encouraging that the text-messaging intervention was able to reduce not only overall usage, but specifically injection use and use during sex, two of the most high-risk behaviors for HIV transmission.
Participation in the intervention was associated with reductions in HIV sexual risk behavior. Participants reduced receptive anal sex with HIV-positive primary partners for the comparatively less risky insertive anal sex (a non-significant change). Additionally, while some participants reported not knowing their primary partner’s HIV serostatus at baseline, all participants knew their primary partner’s HIV serostatus by follow-up.
Reductions of high-risk sexual behaviors with non-primary partners is critical as these encounters are often with anonymous partners, transient or fleeting in nature, with less likelihood of status disclosure and more likelihood of disease transmission across social networks [55,56]. Participants displayed nearly ubiquitous significant reductions in unprotected anal intercourse with non-primary partners. Only the amount of unprotected insertive anal intercourse with HIV-positive partners did not significantly reduce, though a reduction was observed. The demonstrated association between participation in the text-messaging intervention and reductions in unprotected anal intercourse with non-primary partners is encouraging, as it implies that the intervention may be reducing risk behavior in the type of sexual encounters posing greatest risk for HIV transmission.
The association between the text messaging intervention and reductions in unprotected anal sex with non-primary partners may highlight the greatest strength of an asynchronous, portable, and culturally competent intervention like the one employed here, i.e., the ability to reach participants when they are at greatest risk, and are most in need of health-promoting and social support messages. Exigent crises of judgment and temptation may be most likely to occur in real time (i.e., on the streets, in the clubs). This context is far removed from the treatment centers where support and information about sexual health are made available. By contrast, a text-messaging intervention can be accessed nearly anywhere and may be able to intervene in situations that are outside the purview of more standard methods of care. The dramatic and ubiquitous decreases in HIV risk behaviors with non-primary partners is evidence that such interventions may influence decision making in the types of interactions of greatest interest to HIV researchers and prevention specialists.
Limitations
This study was limited by its design and size and the findings must be interpreted with caution. Without a comparison or control arm the observed reductions in methamphetamine use and high-risk sexual behaviors with non-primary partners are associational. Furthermore, the small sample size of this pilot study limits generalizability to other populations. Also, though the use of incentives at baseline and follow-up evaluation could have potentially introduced selection bias, exploratory sub-group analyses revealed no associations between participant incomes and the study primary outcomes, mitigating this concern. Additionally, one challenge in using the latest technological resources and channels in research is that the length of time it takes to obtain protocol approval and start interventions will always exceed the rate of technological advancement. As an example, when this project was first conceived, the messaging device considered for use was a simple two-way pager, which by current standards is now considered grossly obsolete. Project budgets will not always allow research studies to keep up with the speed of the technology. Finally, given the decision to use research staff rather than an automated texting intervention, staff costs were a consideration. However, implementing the intervention with trained research staff allowed for customized responses that fit the needs of the participants.
Conclusions
Results from the Project Tech Support pilot intervention indicate that a text-messaging intervention may be an effective way to transmit health-promoting and social support messages and referrals to out-of-treatment methamphetamine-using MSM. The Project Tech Support pilot study demonstrated the feasibility and acceptability of a text-messaging intervention as an effective means of reaching and communicating with this high-risk population. These findings will be helpful as larger randomized controlled trials are conceived and conducted to evaluate efficacy, cost effectiveness and sustainability. It is likely, however, that the devices, messaging systems, software, and Internet access protocols will be changing more rapidly than the rate with which these research studies can keep up. It will be important to be flexible going forward and to glean the most important lessons that can be reliably taken into development of future studies.
Table 1.
Demographic and Sociodemographic Characteristics at Baseline (N = 52)
| Mean (SD) or N | Range or % | |
|---|---|---|
| Age | 36.5 (8.9) | 22–61 |
| Race/Ethnicity | ||
| Caucasian/white | 18 | 34.6% |
| African American/black | 11 | 21.2% |
| Hispanic/Latino | 20 | 38.5% |
| Multi/Other | 3 | 5.8% |
| Sexual Identity | ||
| Gay | 42 | 80.8% |
| Bisexual | 10 | 19.2% |
| Educational Attainment | ||
| Less than HS | 7 | 13.5% |
| HS or Equivalent | 13 | 25.0% |
| More than HS | 32 | 61.5% |
| Employment | ||
| Unemployed | 38 | 73.1% |
| Part-Time | 11 | 5.8% |
| Full-Time | 3 | 5.8% |
| Income | ||
| $13,558 ($14,360) | $0-$80,000 | |
| HIV Status | ||
| HIV+ | 31 | 59.6% |
| HIV− | 21 | 40.4% |
| Homeless | ||
| Yes | 15 | 28.9% |
Acknowledgments
This study was generously supported by the Centers for Disease Control and Prevention, grant #UR6PS000312. Drs. Reback and Shoptaw acknowledge additional support from the National Institute of Mental Health (P30 MH58107 awarded to M.J. Rotheram-Borus, Ph.D.). The research team would like to thank the community partners – Asian Pacific AIDS Intervention Team, Being Alive, Los Angeles Gay and Lesbian Center, and The Wall/Las Memorias – for their participation in the study.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
References
- 1.Hall HI, Song RG, Rhodes P, et al. Estimation of HIV incidence in the United States. J Am Med Assoc. 2008 Aug 6;300(5):520–9. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report, 2006. Atlanta, GA: US Department of Health and Human Services, CDC; 2008. [Google Scholar]
- 3.Hirshfield S, Remien RH, Walavalkar I, Chiasson MA. Crystal methamphetamine use predicts incident STD infection among men who have sex with men recruited online: a nested case-control study. J Med Internet Res. 2004 Oct-Dec;6(4):42–9. doi: 10.2196/jmir.6.4.e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shoptaw S, Reback CJ. Associations between methamphetamine use and HIV among men who have sex with men: a model for guiding public policy. J Urban Health. 2006 Nov;83(6):1151–7. doi: 10.1007/s11524-006-9119-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colfax GN, Mansergh G, Guzman R, et al. Drug use and sexual risk behavior among gay and bisexual men who attend circuit parties: a venue-based comparison. J Acquir Immune Defic Syndr. 2001 Dec 1;28(4):373–9. doi: 10.1097/00126334-200112010-00011. [DOI] [PubMed] [Google Scholar]
- 6.Mansergh G, Colfax GN, Marks G, et al. The Circuit Party Men’s Health Survey: findings and implications for gay and bisexual men. Am J Public Health. 2001 Jun;91(6):953–8. doi: 10.2105/ajph.91.6.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ober A, Shoptaw S, Wang PC, Gorbach P, Weiss RE. Factors associated with event-level stimulant use during sex in a sample of older, low-income men who have sex with men in Los Angeles. Drug Alcohol Depend. 2009 Jun 1;102(1–3):123–9. doi: 10.1016/j.drugalcdep.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reback CJ. The social construction of a gay drug: methamphetamine use among gay and bisexual males in Los Angeles. City of Los Angeles: AIDS Coordinator’s Office; 1997. [Accessed September 16, 2011]. Available at: http://www.friendscommunitycenter.org/documents/Social_Construction_of_a_Gay_Drug.pdf. [Google Scholar]
- 9.Semple SJ, Strathdee SA, Zians J, Patterson TL. Social and behavioral characteristics of HIV-positive MSM who trade sex for methamphetamine. Am J Drug Alcohol Abuse. 2010 Nov;36(6):325–31. doi: 10.3109/00952990.2010.505273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.HIV Epidemiology Program, Los Angeles County Department of Public Health. An epidemiologic profile of HIV and AIDS in Los Angeles County. 2009. [Google Scholar]
- 11.SAMHSA. Results from the 2007 National Survey on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse Mental Health Services Administration; 2008. [Google Scholar]
- 12.Mausbach BT, Semple SJ, Strathdee SA, Zians J, Patterson TL. Efficacy of a behavioral intervention for increasing safer sex behaviors in HIV-positive MSM methamphetamine users: results from the EDGE study. Drug Alcohol Depend. 2007;87:249–57. doi: 10.1016/j.drugalcdep.2006.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bux DA, Irwin TW. Combining motivational interviewing and cognitive-behavioral skills training for the treatment of crystal methamphetamine abuse/dependence. J Gay Lesbian Psychotherapy. 2006;10:143–52. [Google Scholar]
- 14.Reback CJ, Shoptaw S. Development of an evidence-based, gay-specific cognitive behavioral therapy intervention for methamphetamine-abusing gay and bisexual men [published online ahead of print November 25 2011] Addict Behav. 2011 doi: 10.1016/j.addbeh.2011.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shoptaw S, Reback CJ, Peck JA, et al. Behavioral treatment approaches for methamphetamine dependence and HIV-related sexual risk behaviors among urban gay and bisexual men. Drug Alcohol Depend. 2005;78:125–34. doi: 10.1016/j.drugalcdep.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 16.Shoptaw S, Reback C, Larkins S, et al. Outcomes using two tailored behavioral treatments for substance abuse in urban gay and bisexual men. J Subst Abuse Treat. 2008;35(3):285–93. doi: 10.1016/j.jsat.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Reback CJ, Peck JA, Dierst-Davies R, Nuno M, Kamien JB, Amass A. Contingency management among homeless, out-of-treatment men who have sex with men. J Subst Abuse Treat. 2010;39(3):255–63. doi: 10.1016/j.jsat.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention, HIV/AIDS Prevention Research Synthesis Project. Compendium of HIV prevention interventions with evidence of effectiveness. Atlanta, GA: Centers for Disease Control and Prevention; 1999. Nov, [Accessed July 6, 2011]. revised. Available at: http://www.cdc.gov/hiv/resources/reports/hiv_compendium/ [Google Scholar]
- 19.Moskowitz DA, Melton D, Owczarzak J. PowerON: the use of instant message counseling and the Internet to facilitate HIV/STD education and prevention. Patient Educ Couns. 2009 Oct;77(1):20–6. doi: 10.1016/j.pec.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bourne C, Knight V, Guy R, et al. Short message service reminder intervention doubles sexually transmitted infection/HIV re-testing rates among men who have sex with men. Sex Transm Infect. 2011 Apr;87(3):229–31. doi: 10.1136/sti.2010.048397. [DOI] [PubMed] [Google Scholar]
- 21.Reback CJ, Ling D, Shoptaw S, Rohde J. Developing a text messaging risk reduction intervention for methamphetamine-using MSM: research note. Open AIDS J. 2010;4:116–22. doi: 10.2174/1874613601004030116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rhodes SD, Vissman AT, Stowers J, et al. A CBPR partnership increases HIV testing among men who have sex with men (MSM): outcome findings from a pilot test of the CyBER/testing Internet intervention. Health Educ Behav. 2011 Jun 1;38(3):311–20. doi: 10.1177/1090198110379572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lim MSC, Hocking JS, Hellard ME, Aitken CK. SMS STI: a review of the uses of mobile phone text messaging in sexual health. Int J Std Aids. 2008 May;19(5):287–90. doi: 10.1258/ijsa.2007.007264. [DOI] [PubMed] [Google Scholar]
- 24.Atun RA, Sittampalam SR. A review of the characteristics and benefits of SMS in delivering healthcare. The roles of mobile phones in increasing accessibility and efficiency in healthcare, Vodafone policy paper series number 4. Vodafone. 2006:18–28. [Google Scholar]
- 25.Sherry E, Colloridi B, Warnke PH. Short message service (SMS): a useful communication tool for surgeons. ANZ J Surg. 2002;72(5):369. doi: 10.1046/j.1445-2197.2002.02411.x. [DOI] [PubMed] [Google Scholar]
- 26.Grinter RE, Eldridge MA. y do tngrs luv 2 txt msg? In: Prinz W, Jarke M, Rogers Y, Schmidt K, Wulf V, editors. ECSCW 2001. Bonn, Germany: Springer Netherlands; 2002. pp. 219–38. [Google Scholar]
- 27.Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med. 2009 Feb;36(2):165–73. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 28.Rodgers A, Corbett T, Bramley D, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control. 2005 Aug 1;14(4):255–61. doi: 10.1136/tc.2005.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Riley W, Obermayer J, Jean-Mary J. Internet and mobile phone text messaging intervention for college smokers. J Am Coll Health. 2008 Sep-Oct;57(2):245–8. doi: 10.3200/JACH.57.2.245-248. [DOI] [PubMed] [Google Scholar]
- 30.Vidrine DJ, Marks RM, Arduino RC, Gritz ER. Efficacy of cell phone–delivered smoking cessation counseling for persons living with HIV/AIDS: 3-month outcomes. Nicotine Tob Res. 2011 Jun 13;14:106–10. doi: 10.1093/ntr/ntr121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vähätalo MA, Virtamo HE, Viikari JS, Rönnemaa T. Cellular phone transferred self blood glucose monitoring: prerequisites for positive outcome. Practical Diabetes. 2004;21(5):192–4. [Google Scholar]
- 32.Kwon HS, Cho JH, Kim HS, et al. Development of web-based diabetic patient management system using short message service (SMS) Diabetes Res Clin Pract. 2004;66(suppl 1):S133–7. doi: 10.1016/j.diabres.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 33.Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006;23(12):1332–8. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- 34.Rami B, Popow C, Horn W, Waldhoer T, Schober E. Telemedical support to improve glycemic control in adolescents with type 1 diabetes mellitus. Eur Journal Pediatr. 2006;165(10):701–5. doi: 10.1007/s00431-006-0156-6. [DOI] [PubMed] [Google Scholar]
- 35.Kim HS, Kim NC, Ahn SH. Impact of a nurse short message service intervention for patients with diabetes. J Nurs Care Qual. 2006;21(3):266–71. doi: 10.1097/00001786-200607000-00012. [DOI] [PubMed] [Google Scholar]
- 36.Simoni JM, Huh D, Frick PA, et al. Peer support and pager messaging to promote antiretroviral modifying therapy in Seattle: a randomized controlled trial. J Acq Imm Def. 2009 Dec 1;52(4):465–73. doi: 10.1097/qai.0b013e3181b9300c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kalichman SC, Kalichman MO, Cherry C, et al. Brief behavioral self-regulation counseling for HIV treatment adherence delivered by cell phone: an initial test of concept trial. Aids Patient Care STDS. 2011 May;25(5):303–10. doi: 10.1089/apc.2010.0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thirumurthy H, Haberer J, Habyarimana JP, Pop-Eleches C, Bangsberg DR. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders [response] AIDS. 2011 May 15;25(8):1138–9. doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vilella A, Bayas JM, Diaz MT, et al. The role of mobile phones in improving vaccination rates in travelers. Prev Med. 2004;38(4):503–9. doi: 10.1016/j.ypmed.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 40.Robinson S, Perkins S, Bauer S, et al. Aftercare intervention through text messaging in the treatment of bulimia nervosa—feasibility pilot. Int J Eat Disord. 2006;39(8):633–8. doi: 10.1002/eat.20272. [DOI] [PubMed] [Google Scholar]
- 41.Levine D, McCright J, Dobkin L, Woodruff AJ, Klausner JD. SEXINFO: a sexual health text messaging service for San Francisco youth. Am J Public Health. 2008 Mar;98(3):393–5. doi: 10.2105/AJPH.2007.110767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bilardi JE, Fairley CK, Hopkins CA, et al. Let them know: evaluation of an online partner notification service for chlamydia that offers e-mail and SMS messaging. Sex Transm Dis. 2010 Sep;37(9):563–5. doi: 10.1097/OLQ.0b013e3181d707f1. [DOI] [PubMed] [Google Scholar]
- 43.Lim MSC, Hocking JS, Aitken CK, et al. Impact of text and email messaging on the sexual health of young people: a randomised controlled trial. J Epidemiol Community Health. 2012;66:69–74. doi: 10.1136/jech.2009.100396. [DOI] [PubMed] [Google Scholar]
- 44.Noar SM, Webb EM, Van Stee SK, et al. Using computer technology for HIV prevention among African-Americans: development of a tailored information program for safer sex (TIPSS) Health Educ Res. 2011 Jun 1;26(3):393–406. doi: 10.1093/her/cyq079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Harris LT, Lehavot K, Huh D, et al. Two-way text messaging for health behavior change among human immunodeficiency virus-positive individuals. Telemed J E Health. 2010 Dec;16(10):1024–9. doi: 10.1089/tmj.2010.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ybarra ML, Bull SS. Current trends in Internet and cell phone based HIV prevention and intervention programs. Curr HIV/AIDS Rep. 2007;4(4):201–7. doi: 10.1007/s11904-007-0029-2. [DOI] [PubMed] [Google Scholar]
- 47.Tonigan JS, Rice SL. Is it beneficial to have an Alcoholics Anonymous sponsor? Psychol Addict Behav. 2010 Sep;24(3):397–403. doi: 10.1037/a0019013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kolko J. Silicon mountains, silicon molehills: geographic concentration and convergence of internet industries in the US. Inf Econ Policy. 2002 Jun;14(2):211–32. [Google Scholar]
- 49.Stata Statistical Software. Release 10 [computer program] College Station, TX: StataCorp LP; 2007. [Google Scholar]
- 50.Lyons T, Chandra G, Goldstein J, Ostrow DG. Breaking the bond between stimulant use and risky sex: a qualitative study. Subst Abus. 2010;31(4):224–30. doi: 10.1080/08897077.2010.514240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Menza TW, Hughes JP, Celum CL, Golden MR. Prediction of HIV acquisition among men who have sex with men. Sex Transm Dis. 2009 Sep;36(9):547–55. doi: 10.1097/OLQ.0b013e3181a9cc41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mimiaga MJ, Reisner SL, Fontaine YM, et al. Walking the line: stimulant use during sex and HIV risk behavior among Black urban MSM. Drug Alcohol Depend. 2010 Jul 1;110(1–2):30–7. doi: 10.1016/j.drugalcdep.2010.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Forrest DW, Metsch LR, LaLota M, et al. Crystal methamphetamine use and sexual risk behaviors among HIV-positive and HIV-negative men who have sex with men in South Florida. J Urban Helath. 2010 May;87(3):480–5. doi: 10.1007/s11524-009-9422-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gorbach PM, Weiss RE, Jeffries R, et al. Behaviors of recently HIV-infected men who have sex with men in the year postdiagnosis: effects of drug use and partner types. J Acquir Immune Defic Syndr. 2011;56(2):176–82. doi: 10.1097/QAI.0b013e3181ff9750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bowers JR, Branson CM, Fletcher J, Reback CJ. Differences in substance use and sexual partnering between men who have sex with men, men who have sex with men and women and transgender women. Cult Health and Sex. 2011 Mar 24;13(6):629–42. doi: 10.1080/13691058.2011.564301. [DOI] [PubMed] [Google Scholar]
- 56.Tobin KE, Latkin CA. An examination of social network characteristics of men who have sex with men who use drugs. Sex Transm Infect. 2008 Nov;84(6):420–4. doi: 10.1136/sti.2008.031591. [DOI] [PMC free article] [PubMed] [Google Scholar]