Abstract
Purpose
Our study provides epidemiologic data on the prevalence of refractive errors in all age group ≥5 years in Korea.
Methods
In 2008 to 2012, a total of 33,355 participants aged ≥5 years underwent ophthalmologic examinations. Using the right eye, myopia was defined as a spherical equivalent (SE) less than -0.5 or -1.0 diopters (D) in subjects aged 19 years and older or as an SE less than -0.75 or -1.25 D in subjects aged 5 to 18 years according to non-cycloplegic refraction. Other refractive errors were defined as follows: high myopia as an SE less than -6.0 D; hyperopia as an SE larger than +0.5 D; and astigmatism as a cylindrical error less than -1.0 D. The prevalence and risk factors of myopia were evaluated.
Results
Prevalence rates with a 95% confidence interval were determined for myopia (SE <-0.5 D, 51.9% [51.2 to 52.7]; SE <-1.0 D, 39.6% [38.8 to 40.3]), high myopia (5.0% [4.7 to 5.3]), hyperopia (13.4% [12.9 to 13.9]), and astigmatism (31.2% [30.5 to 32.0]). The prevalence of myopia demonstrated a nonlinear distribution with the highest peak between the ages of 19 and 29 years. The prevalence of hyperopia decreased with age in subjects aged 39 years or younger and then increased with age in subjects aged 40 years or older. The prevalence of astigmatism gradually increased with age. Education was associated with all refractive errors; myopia was more prevalent and hyperopia and astigmatism were less prevalent in the highly educated groups.
Conclusions
In young generations, the prevalence of myopia in Korea was much higher compared to the white or black populations in Western countries and is consistent with the high prevalence found in most other Asian countries. The overall prevalence of hyperopia was much lower compared to that of the white Western population. Age and education level were significant predictive factors associated with all kinds of refractive errors.
Keywords: Astigmatism, Hyperopia, Myopia, Refractive errors
Refractive error is one of the most common causes of visual impairment worldwide and is the second leading cause of treatable blindness [1]. An increasing number of epidemiologic studies focusing on refractive errors have been conducted, both in developing countries and in developed countries [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17]. However, there are few published studies that encompass all age groups and specifically report changes in prevalence with age. There are a few studies [18,19] that have reported detailed data on the prevalence of various refractive errors in the Korean population. However, there is still little known about the prevalence of various refractive errors across age groups. South Korea has experienced rapid socioeconomic growth over the past several decades, and the estimated increase in the prevalence of refractive errors is a major public health and socioeconomic concern.
The Korea National Health and Nutrition Examination Survey (KNHANES, http://knhanes.cdc.go.kr) is an annual nationally representative survey conducted by the Ministry of Health and Welfare in South Korea. The Korean Ophthalmological Society has participated in this survey since July 2008 and has conducted ophthalmological interviews and examinations with the purpose of elucidating the prevalence of common eye disorders, including refractive errors. On behalf of the Epidemiologic Survey Committee of the Korean Ophthalmological Society, we report the prevalence and risk factors of refractive errors in all age groups ≥5 years among the general South Korean population derived from a nationwide epidemiological survey. This study utilized all the data from ophthalmologic examinations conducted in the KNAHNES from 2008 to 2012.
Materials and Methods
Statement of ethics
Ophthalmic examinations were conducted under the supervision of the Epidemiologic Survey Committee of the Korean Ophthalmological Society. This survey was reviewed and approved by the institutional review board of the Korea Centers for Disease Control and Prevention (KCDC), and all participants provided written informed consent. The study was conducted in accordance with the Declaration of Helsinki.
Study design and population
A detailed description of the sampling, enumeration, visual acuity, and ocular examination procedures was previously published [18]. All examinations and health interviews were conducted in mobile centers by trained team members, including ophthalmology residents or ophthalmologists.
Examination methods and definition of refractive errors
Refractive errors and visual acuity were examined in subjects aged 5 years or older. Refractive error was measured three times using an autorefractor-keratometer (KR8800; Topcon, Tokyo, Japan) under non-cycloplegic conditions. Average values of the three refraction measurements were printed from the autorefractor and were recorded using a negative cylinder notation. Participants were excluded from analyses if any of the following was present: (1) aged less than 5 years; (2) a history of cataract surgery in the right eye; (3) a history of laser refractive surgery in the right eye; or (4) missing autorefractor data of the right eye due to lack of time, inability to comply with the protocol, or equipment malfunction. Prevalence was calculated using the refractive error data of 33,355 participants for the right eye only. The refractive data was converted to the spherical equivalent (SE), which was derived by adding the spherical component of the refraction to one-half the value of the cylindrical component. We defined myopia using two thresholds. For subjects aged 19 years or older, criteria were SE <-0.5 and <-1.0 diopters (D). Since non-cycloplegic autorefraction is likely to be overestimated in the young population, we used a more strict definition of myopia for subjects aged 5 to 18 years: SE <-0.75 rather than SE <-0.5 D, and SE <-1.25 rather than SE <-1.0 D. High myopia was defined and analyzed as an SE <-6.0 D. Hyperopia was defined as an SE >+0.5 D. Astigmatism was defined as a cylindrical error (Cyl) ≤-1.0 D, without reference to the axis. Astigmatism was defined as "with-the-rule" if the axis was between 0 and 15 or 165 and 180 degrees, as "against-the-rule" if the axis was between 75 and 105 degrees, and as "oblique" if the axis was from 16 to 74 degrees or 106 to 164 degrees. Additionally, we provided the prevalence of refractive errors using the KCDC definition of the other eye in the supplementary material. Another study population was selected to assess the KCDC definition of refractive errors of either eye. The KCDC defined refractive error as follows: myopia as SE ≤-0.75 D, hyperopia as SE ≥+1.0 D, astigmatism as Cyl ≤-0.75 D in either eye, and anisometropia as SE difference ≥2.0 D or as cylindrical difference ≥1.5 D between the eyes.
Independent variables
The analyzed sociodemographic variables were age, gender, household monthly income (lowest quintile/2nd to 4th quintile/highest quintile), highest educational level achieved (elementary school or lower/middle school/high school/college graduate or higher), and residential area (rural: town [eup], township [myeon], or neighborhood [dong]/urban: city [si], county [gun], and district [gu]). Quintiles of income were divided using the data from KNHANES 2008-2012 before the exclusion criteria were applied.
Statistical analysis
Basic study population characteristics were reported. To determine the age- and gender-standardized prevalence of refractive error, the prevalence was calculated according to the guidelines of the KNHANES 2008-2012 data analysis using a poststratification adjustment. Poststratified weight was calculated based on the response and extraction rates in order to reflect the distribution of the 2010 Korean population by age groups of 5-year intervals and by gender. Consequently, the sum of the weight according to KNHANES 2008-2012 was representative of the Korean population as of 2010. Data was analyzed using the survey procedure of Stata SE ver. 13 (Stata Co., College Station, TX, USA) to account for the sample design and sampling weight adjusted for oversampling and nonresponders. Multivariate logistic regression analysis including age, gender, household monthly income, education, and residential area was conducted to identify the sociodemographic risk factors of refractive errors. Adjusted odds ratios and 95% confidence intervals (CIs) were calculated. Only adults aged 19 years or older, assumed to be finished growing, were included for evaluating risk factors of various refractive errors. Results with p-values less than 0.05 were considered statistically significant.
Results
Baseline characteristics of the study population
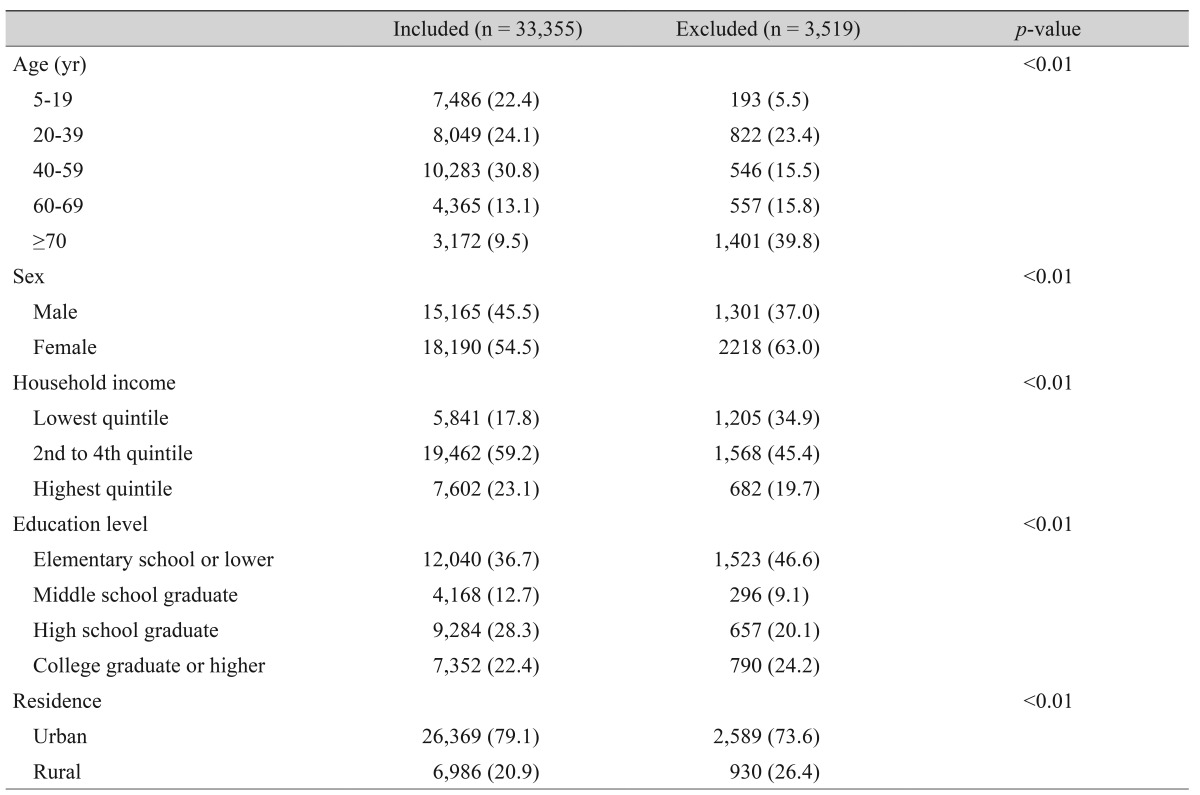
A comparison of the demographic characteristics of the 33,355 subjects included in this study with those excluded from this study (n = 3,519) is provided in Table 1. Included participants were more likely to be younger, male, in a higher income group, and living in an urban area than those who were excluded from this analysis. Another study population for estimating prevalence of refractive errors using KCDC definition included 33,922 participants.
Table 1. Demographics of the study participants from the Korea National Health and Nutrition Examination Survey 2008-2012.
Values are presented as number (%); Chi-square's test was used to calculate the p-value.
Age- and gender-standardized prevalence
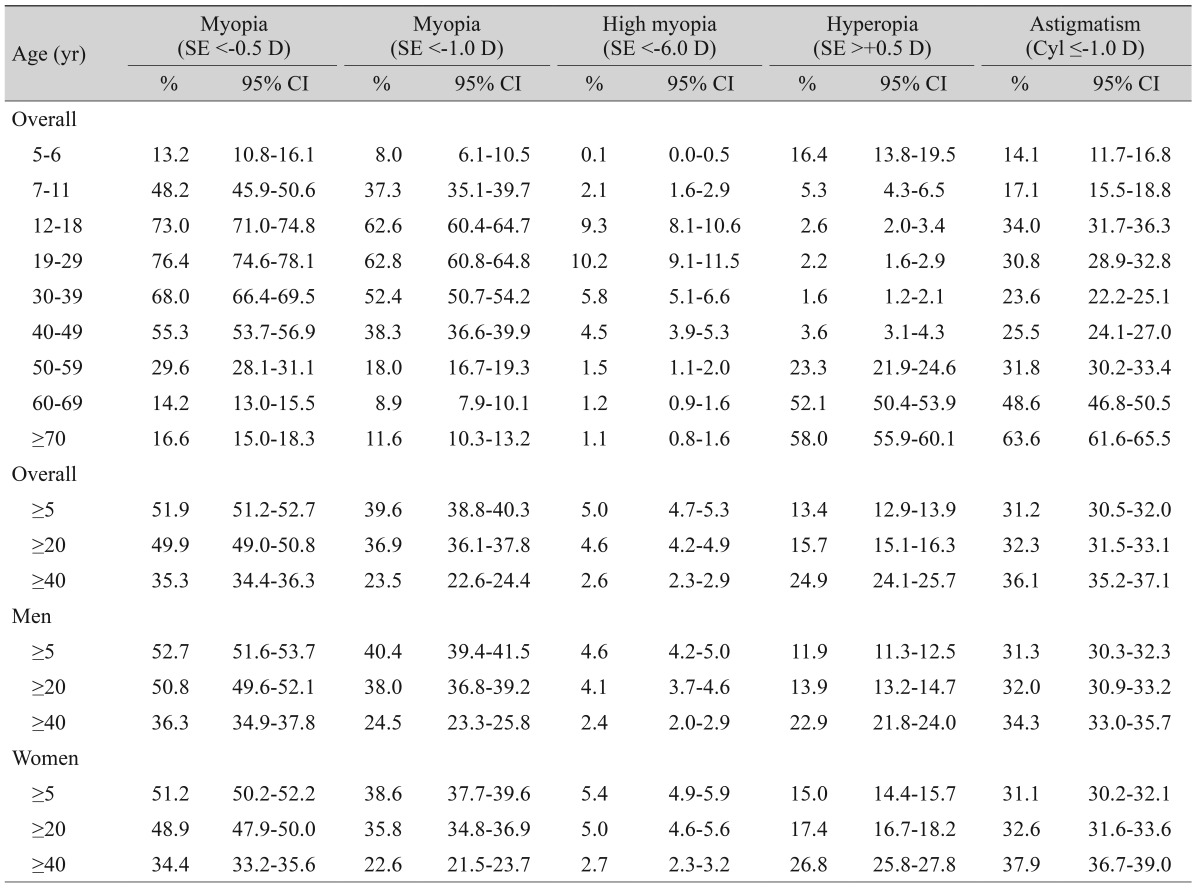
Table 2 provides the age- and gender-standardized prevalence of refractive errors in the right eyes. The prevalence with a 95% CI was determined for myopia (SE <-0.5 D, 51.9% [51.2 to 52.7]; SE <-1.0 D, 39.6% [38.8 to 40.3]), high myopia (5.0% [4.7 to 5.3]), hyperopia (13.4% [12.9 to 13.9]), and astigmatism (31.2% [30.5 to 32.0]) in all participants ≥5 years of age. The prevalence of myopia had a nonlinear distribution with the highest peak between the ages of 19 and 29 years, with a minor increase in subjects older than 70 years for both thresholds of myopia of -0.5 D and -1.0 D. High myopia showed a similar pattern to myopia, with the highest prevalence of 10.2% in the age group of 19 to 29 years, but without the minor increase in subjects over 70 years. The prevalence of hyperopia was lowest in subjects in their 30s (1.6%; CI, 1.2 to 2.1); it decreased with age in subjects aged 39 years or younger and then increased with age in subjects aged 40 years or older, with an abrupt increase in subjects aged 50 years or older. The prevalence of astigmatism gradually increased with age with a slight decrease around 30 to 39 year ages. Table 3 provides the prevalence of refractive errors using the KCDC definition.
Table 2. Age-standardized prevalence of refractive errors in the right eye (n = 33,355).
Myopia was defined as SE <-0.75 D and SE <-1.25 D for subjects aged 5 to 18 years. Complex sample analysis was performed with reference to weight, stratification variance, and cluster variance, following the statistical guidelines of the Korea Centers for Disease Control and Prevention. Age- and gender-standardized prevalence was provided based on post-stratified weight.
SE = spherical equivalent; D = diopters; CI = confidence interval; Cyl = cylindrical error.
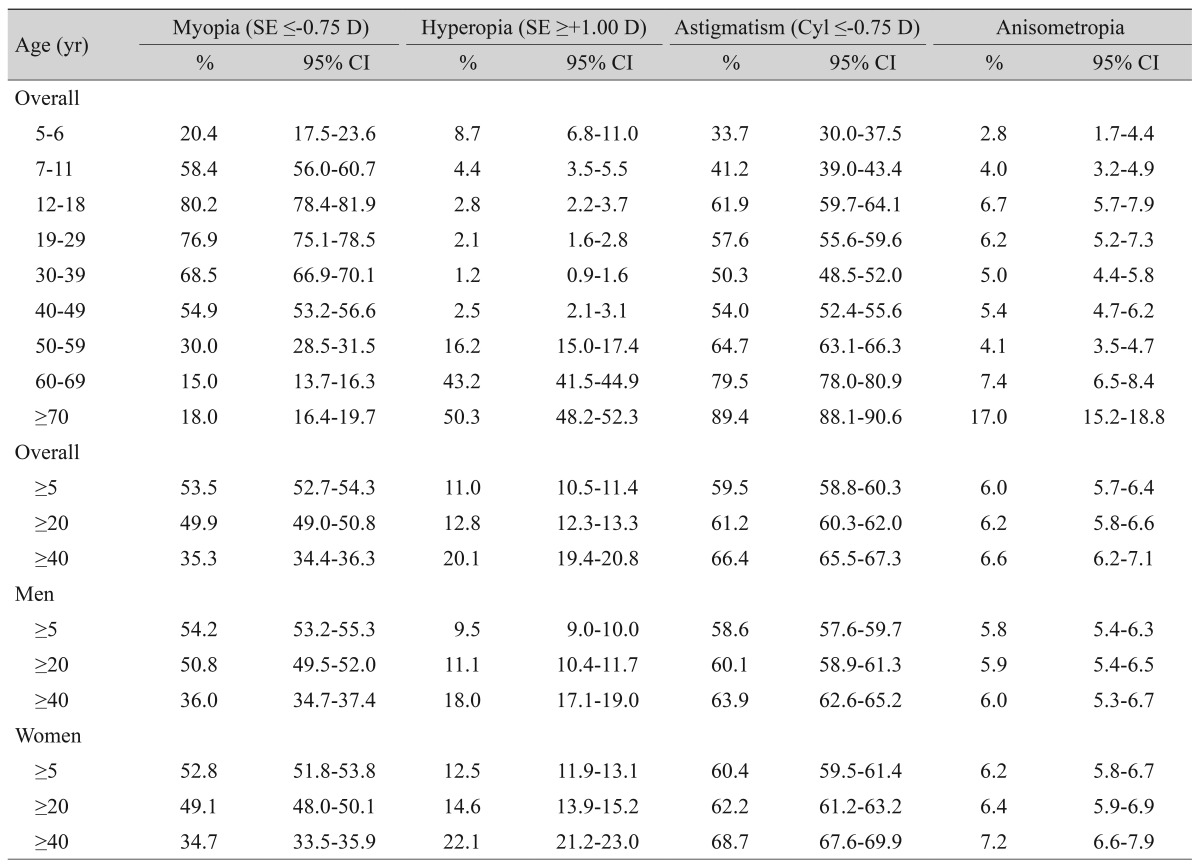
Table 3. Age-standardized prevalence of refractive errors in either eye according to the Korea Centers for Disease Control and Prevention definition (n = 33,922).
Anisometropia was defined as an SE difference ≥2.0 D or a cylindrical difference ≥1.5 D in either eye. Complex sample analysis was performed with reference to weight, stratification variance, and cluster variance, following the statistical guidelines of the Korea Centers for Disease Control and Prevention. Age- and gender-standardized prevalence and age-standardized prevalence was provided based on post-stratified weight.
SE = spherical equivalent; D = diopters; CI = confidence interval; Cyl = cylindrical error.
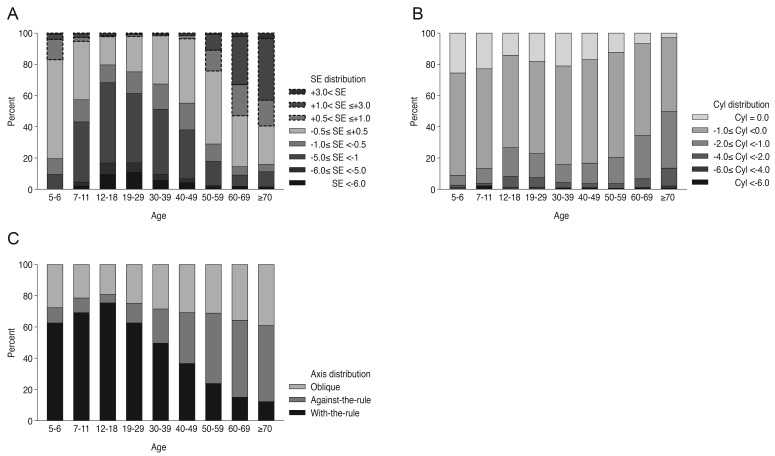
Fig. 1 shows 100% stacked column charts of the refractive error distribution in the right eye by age group. Myopia was more prevalent in children, adolescents, and young adults, whereas hyperopia was more prevalent among very young children of 5 to 6 years of age, middle-age, and elderly subjects (Fig. 1A). Hyperopia showed a relatively lower prevalence of less than 5% from 12 to 49 years of age. The proportion of emmetropia between -0.5 and +0.5 D started at approximately 60% in children 5 to 6 years of age, decreased in adolescents 12 to 18 years old, increased to approximately 40% in subjects 50 to 59 years of age, and then decreased with increasing age thereafter. The prevalence of astigmatism generally increased with age, with a relatively low prevalence in the 30 to 39 year age group (Fig. 1B). Older adults were more likely to have "against-the-rule" astigmatism than were younger people (Fig. 1C).
Fig. 1. Age-specific proportions of refractive errors in the right eye by (A) spherical equivalent (SE), (B) cylindrical error (Cyl), and (C) axis distribution of astigmatism (n = 33,355).
Sociodemographic factors associated with refractive error in adults
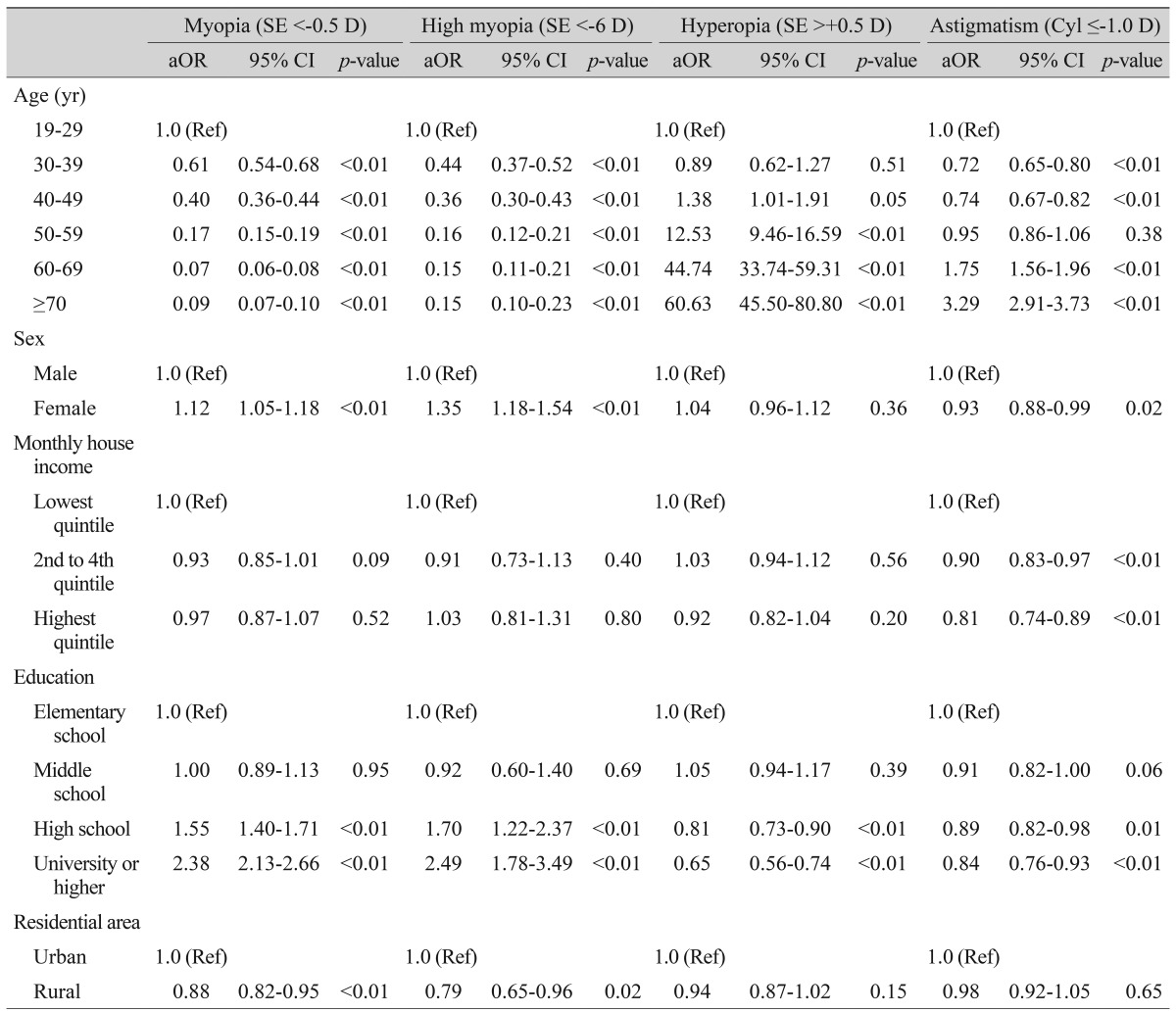
Table 4 provides the sociodemographic factors associated with refractive errors according to multivariate analysis of participants aged 19 years or older, reported with odds ratio and 95% CI. Among participants ≥19 years of age, risk of myopia and high myopia decreased and that of hyperopia and astigmatism increased with age. Female gender, higher education level, and urban residence were associated with a higher risk of both myopia and high myopia, whereas those with higher education levels were at significantly lower risk of hyperopia. Female gender, higher household income, and higher education were significant protective factors against astigmatism.
Table 4. Sociodemographic risk factors of refractive errors in the Korean population ≥19 years of age-multivariate logistic analysis (n = 26,174).
SE = spherical equivalent; D = diopters; aOR = adjusted odds ratio; CI = confidence interval; Cyl = cylindrical error.
Discussion
This study documented the prevalence of various refractive errors in the South Korean population ≥5 years of age based on a nationwide health survey and outlined independent sociodemographic risk factors for each refractive error.
Myopia and high myopia
The prevalence of myopia in children varies highly across regions, and our relatively high prevalence (73.0% in subjects between 12 and 18 years of age) was similar to those of other Asian countries, which have been shown to have some of the highest prevalence rates of myopia in the world [20]. A recent study of Sydney schoolchildren showed ethnic differences in myopia prevalence; children of East Asian ethnicity had a higher incidence of myopia than European Caucasian children [21]. The trend of increasing prevalence of myopia with increasing age in children and adolescents was explicitly evident in this study, which is also consistent with studies of children from China [6,10,17], Taiwan [9], Chile [7], and Germany [14]. On the other hand, the prevalence of myopia in Nepal was lower than that of other countries, without clear increasing or decreasing trends [8]. These different tendencies in myopia prevalence by age in children might be caused by different myopia-driving socioenvironmental factors in different regions, such as urbanization with an increase of formal education.
Among the young adults aged 20 to 39 years, the prevalence of myopia and high myopia were higher compared to those of the white population in the United States [13], and this high prevalence was similar to other countries in Asia [22,23]. Myopia and high myopia seem to be more prevalent in Asia compared to all races in the United States, especially in the younger generations [13]. Unlike the large differences in prevalence across regions among young adults aged 20 to 39 years, the prevalence of myopia in the 40 years or older age group seemed to be similar across regions; even when differences were noted by region, the difference was not large [5,13,15,24]. The overall pattern of prevalence of myopia being higher in younger adults and lower in the elderly in this study was consistent with that of urbanized populations of Singapore [5,12], southern India [25], and the white United States population [2]. Urbanization and economic development including increasing level of education combined with genetic susceptibility might contribute to increasing trends of myopia in younger generations compared to older generations in these areas. The prevalence changes across age groups in this report were similar to those of other developing countries in Asia, which might reflect the age-related prevalence pattern of myopia in Asian countries with similar levels of urbanization. A myopic shift due to cataract might explain the minor increase of myopia in the participants ≥70 years of age. This pattern has been shown consistently in several studies of different ethnic groups, including Japanese subjects [24], all three ethnic groups in Singapore [5,12,16], Latinos in Los Angeles (United States) [26], and residents of Barbados [4].
A previous study comparing the prevalence of myopia in the United States between 1970 and 2000 revealed that the increase in the prevalence of myopia was more prominent in black participants than in white participants, and the researchers explained this by the increase of formal education, associated with associated with near work demands, in the black population [27]. The increased prevalence from around 20% in adults to over 70% in younger generations in this study can be explained using a cohort effect associated with urbanization and economic development combined with genetic susceptibility, rather than a direct effect of aging alone.
Hyperopia
In Asia, the prevalence of hyperopia has been reported to be around 20% to 35% among adults [5,12,28], which is similar to our data (24.9% in subjects, ≥40 years of age). When hyperopia was defined as SE ≥+0.5 D, the prevalence of hyperopia in the ≥40 years age group was about 20% greater than that of whites in Wisconsin, as reported by the Beaver Dam Eye Study (BDES) (49.0% in BDES; 28.0% in this KNHANES population, unpresented data) [2]. The prevalence of hyperopia, defined as SE >+0.5 D, was also higher in Australia (Blue Mountains Eye Study, BMES) [3] compared to Korea based on a similar age group of 44 years or older (55.6% in BMES; 36.5% in this KNHANES population, unpresented data). The low hyperopia prevalence in the 40 to 49 year age group (3.6%) might have contributed to this lower prevalence of hyperopia in Korean adults and can also be considered a result of a myopic shift in younger generations. The prevalence of hyperopia can be represented as a U-shaped curve, decreasing with age until the fourth decade, then abruptly increasing from the sixth decade onward (Table 2 and Fig. 1A). In children, the tendency of decreasing hyperopia with age was consistent with studies conducted in various other areas [6,10,17]. In adults, the trend of increasing hyperopia prevalence with age was shown in the NHANES [13], both the Chinese and Malay populations of Singapore [5,12], Sumatra [28], Germany [14], and the Baltimore Eye Study [29], although the specific ages for the beginning and end of the shifts varied across studies. Other epidemiologic studies have reported that, after the age of 60 years, the prevalence of hyperopia is no longer associated with age [2,3,4,29,30]. In Korea, the cataract surgery rate among the population in their 80s is almost 50% [31]. Therefore, the hyperopia prevalence might have been overestimated in our elderly subjects because severe cataracts that drive a myopic shift were more likely to have been removed by cataract surgery, and therefore, excluded from this study.
Astigmatism
Astigmatism (Cyl, ≤-1.0 D) was found in 14.1% of the Korean population aged 5 to 6 years. Among children aged less than 6 years, ethnic differences in the prevalence of astigmatism seem to exist, as Caucasians were less likely to have astigmatism compared to other ethnicities [32]. Astigmatism (Cyl, ≤-1.0 D) was found in 36.1% of this Korean population aged 40 years or older, which was similar to the prevalence found in adults in Sumatra (35.8%) [28] and the whole adult population of the NHANES in 1999 to 2004 (31.0%) [13] and slightly higher than that of the Singapore Malays (27.8%) and lower than that of the Singapore Chinese population (44.2%) [28]. The prevalence of astigmatism demonstrated an increasing trend with age, which is consistent with previous studies [11,12,29].
In our population, "with-the-rule" astigmatism was dominant in children and young adults, and the proportion of "against-the-rule" astigmatism increased with age after young adulthood. This trend was also reported in southern India [25]. It is not possible to make a direct conclusion about lifetime changes in astigmatism from this cross-sectional study; however, our results indicate that "against-the-rule" astigmatism is caused by changes related to aging.
Sociodemographic factors and refractive error
This study confirmed the associations between age, household monthly income, education, and residential area and various refractive errors. Age and education were associated with all types of refractive errors. Women, those with a higher education level, and those living in an urban area were more likely to be myopic. It is difficult to form a firm conclusion regarding the association between gender and myopia prevalence considering the inconsistent results reported in previous studies [2,5,11,12,13]. Higher education [5,12,13,29,30] and urban residence [11] were generally considered risk factors for myopia, and our results support this association. Some studies, including the NHANES [13], the Tanjong Pagar Survey [5], and the Sumatra Eye Study [28], found that higher income is associated with an increasing prevalence of myopia; however, the present study did not show a significant association. Respondents with a higher level of education were less likely to have hyperopia in this study. Hyperopia was also reported to have a lower prevalence in respondents with a higher educational level in the Singapore Malay Eye Survey [12] and the Sumatra Eye Study [28]; however, the Meiktila Eye Study performed in rural Myanmar [33] reported a higher prevalence of hyperopia in subjects with higher education. In terms of astigmatism, higher educational level was associated with lower prevalence of astigmatism in our results. The Sumatra Eye study found no significant relationship between education level and astigmatism [28], whereas the Beijing Eye Study showed that astigmatism was associated with a low educational background [11].
The major strength of this study is that it used a large-scale, population-based sample that represents the entire general South Korean population across all ages. We report the prevalence of refractive errors, on behalf of the Epidemiologic Survey Committee of the Korean Ophthalmological Society, using data from 33,355 participants including all age groups ≥5 years, including the entire ophthalmic data of the KNHANES series. Our study has several limitations. As previously stated, the prevalence of myopia in children could have been overestimated, since cycloplegic refraction could not be performed due to the time constraints imposed by the comprehensive KNHANES examination. Accommodation might have affected the refractive error measurement, particularly in young children, although the autorefractor used an auto-fogging technique to minimize accommodation. Consequently, the prevalence of myopia could have been overestimated and that of hyperopia could have been underestimated in these young children [34]. However, the difference in refractive error caused by accommodation is likely not very large; a previous large epidemiologic study on Beijing children reported that the mean difference in autorefractometry with or without cycloplegia was only 0.29 ± 0.40 D in myopic eyes (SE <-0.5 D) [35]. Nonetheless, we used a higher SE value to define myopia, i.e., SE ≤-1.0 rather than ≤-0.75 D, in children and adolescents (aged 5 to 18) in order to minimize overestimation of myopia prevalence due to non-cycloplegic autorefraction. Second, the characteristics of participants were different from those of nonparticipants; KNHANES 2009-2012 participants who were included in this study were more likely to be young, male, in a higher income group, and living in an urban area than were those who were excluded from this study. However, we presented our results based on our inclusion criteria, and analyses of the subjects who had undergone ophthalmologic surgery that would affect refractive errors such as cataract surgery or laser refractive surgeries were excluded from our investigation, as has been done in other epidemiological studies.
In conclusion, we provide the prevalence of refractive errors in all age groups ≥5 years using a national representative sample. Our findings demonstrated that the prevalence of myopia was higher and that the prevalence of hyperopia was lower than those previously reported in Western countries. The prevalence of myopia was much higher in adolescents and young adults compared to the other age groups, which is consistent with that of other East Asian countries.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86:63–70. doi: 10.2471/BLT.07.041210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Q, Klein BE, Klein R, Moss SE. Refractive status in the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 1994;35:4344–4347. [PubMed] [Google Scholar]
- 3.Attebo K, Ivers RQ, Mitchell P. Refractive errors in an older population: the Blue Mountains Eye Study. Ophthalmology. 1999;106:1066–1072. doi: 10.1016/S0161-6420(99)90251-8. [DOI] [PubMed] [Google Scholar]
- 4.Wu SY, Nemesure B, Leske MC. Refractive errors in a black adult population: the Barbados Eye Study. Invest Ophthalmol Vis Sci. 1999;40:2179–2184. [PubMed] [Google Scholar]
- 5.Wong TY, Foster PJ, Hee J, et al. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci. 2000;41:2486–2494. [PubMed] [Google Scholar]
- 6.Zhao J, Pan X, Sui R, et al. Refractive Error Study in Children: results from Shunyi District, China. Am J Ophthalmol. 2000;129:427–435. doi: 10.1016/s0002-9394(99)00452-3. [DOI] [PubMed] [Google Scholar]
- 7.Maul E, Barroso S, Munoz SR, et al. Refractive Error Study in Children: results from La Florida, Chile. Am J Ophthalmol. 2000;129:445–454. doi: 10.1016/s0002-9394(99)00454-7. [DOI] [PubMed] [Google Scholar]
- 8.Pokharel GP, Negrel AD, Munoz SR, Ellwein LB. Refractive Error Study in Children: results from Mechi Zone, Nepal. Am J Ophthalmol. 2000;129:436–444. doi: 10.1016/s0002-9394(99)00453-5. [DOI] [PubMed] [Google Scholar]
- 9.Lin LL, Shih YF, Hsiao CK, et al. Epidemiologic study of the prevalence and severity of myopia among schoolchildren in Taiwan in 2000. J Formos Med Assoc. 2001;100:684–691. [PubMed] [Google Scholar]
- 10.He M, Zeng J, Liu Y, et al. Refractive error and visual impairment in urban children in southern China. Invest Ophthalmol Vis Sci. 2004;45:793–799. doi: 10.1167/iovs.03-1051. [DOI] [PubMed] [Google Scholar]
- 11.Xu L, Li J, Cui T, et al. Refractive error in urban and rural adult Chinese in Beijing. Ophthalmology. 2005;112:1676–1683. doi: 10.1016/j.ophtha.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 12.Saw SM, Chan YH, Wong WL, et al. Prevalence and risk factors for refractive errors in the Singapore Malay Eye Survey. Ophthalmology. 2008;115:1713–1719. doi: 10.1016/j.ophtha.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 13.Vitale S, Ellwein L, Cotch MF, et al. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol. 2008;126:1111–1119. doi: 10.1001/archopht.126.8.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jobke S, Kasten E, Vorwerk C. The prevalence rates of refractive errors among children, adolescents, and adults in Germany. Clin Ophthalmol. 2008;2:601–607. doi: 10.2147/opth.s2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krishnaiah S, Srinivas M, Khanna RC, Rao GN. Prevalence and risk factors for refractive errors in the South Indian adult population: the Andhra Pradesh Eye disease study. Clin Ophthalmol. 2009;3:17–27. [PMC free article] [PubMed] [Google Scholar]
- 16.Pan CW, Wong TY, Lavanya R, et al. Prevalence and risk factors for refractive errors in Indians: the Singapore Indian Eye Study (SINDI) Invest Ophthalmol Vis Sci. 2011;52:3166–3173. doi: 10.1167/iovs.10-6210. [DOI] [PubMed] [Google Scholar]
- 17.Wu JF, Bi HS, Wang SM, et al. Refractive error, visual acuity and causes of vision loss in children in Shandong, China: the Shandong Children Eye Study. PLoS One. 2013;8:e82763. doi: 10.1371/journal.pone.0082763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoon KC, Mun GH, Kim SD, et al. Prevalence of eye diseases in South Korea: data from the Korea National Health and Nutrition Examination Survey 2008-2009. Korean J Ophthalmol. 2011;25:421–433. doi: 10.3341/kjo.2011.25.6.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim EC, Morgan IG, Kakizaki H, et al. Prevalence and risk factors for refractive errors: Korean National Health and Nutrition Examination Survey 2008-2011. PLoS One. 2013;8:e80361. doi: 10.1371/journal.pone.0080361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saw SM, Katz J, Schein OD, et al. Epidemiology of myopia. Epidemiol Rev. 1996;18:175–187. doi: 10.1093/oxfordjournals.epirev.a017924. [DOI] [PubMed] [Google Scholar]
- 21.French AN, Morgan IG, Mitchell P, Rose KA. Risk factors for incident myopia in Australian schoolchildren: the Sydney adolescent vascular and eye study. Ophthalmology. 2013;120:2100–2108. doi: 10.1016/j.ophtha.2013.02.035. [DOI] [PubMed] [Google Scholar]
- 22.Rasmussen OD. Incidence of myopia in China: data and theses from periodical investigations covering thirty years residence, and association with refracting and hospital centres, in a score of the larger cities. Br J Ophthalmol. 1936;20:350–360. doi: 10.1136/bjo.20.6.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu HM, Seet B, Yap EP, et al. Does education explain ethnic differences in myopia prevalence? A population-based study of young adult males in Singapore. Optom Vis Sci. 2001;78:234–239. doi: 10.1097/00006324-200104000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Sawada A, Tomidokoro A, Araie M, et al. Refractive errors in an elderly Japanese population: the Tajimi study. Ophthalmology. 2008;115:363–370.e3. doi: 10.1016/j.ophtha.2007.03.075. [DOI] [PubMed] [Google Scholar]
- 25.Dandona R, Dandona L, Naduvilath TJ, et al. Refractive errors in an urban population in Southern India: the Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci. 1999;40:2810–2818. [PubMed] [Google Scholar]
- 26.Tarczy-Hornoch K, Ying-Lai M, Varma R. Myopic refractive error in adult Latinos: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2006;47:1845–1852. doi: 10.1167/iovs.05-1153. [DOI] [PubMed] [Google Scholar]
- 27.Vitale S, Sperduto RD, Ferris FL., 3rd Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127:1632–1639. doi: 10.1001/archophthalmol.2009.303. [DOI] [PubMed] [Google Scholar]
- 28.Saw SM, Gazzard G, Koh D, et al. Prevalence rates of refractive errors in Sumatra, Indonesia. Invest Ophthalmol Vis Sci. 2002;43:3174–3180. [PubMed] [Google Scholar]
- 29.Katz J, Tielsch JM, Sommer A. Prevalence and risk factors for refractive errors in an adult inner city population. Invest Ophthalmol Vis Sci. 1997;38:334–340. [PubMed] [Google Scholar]
- 30.Wensor M, McCarty CA, Taylor HR. Prevalence and risk factors of myopia in Victoria, Australia. Arch Ophthalmol. 1999;117:658–663. doi: 10.1001/archopht.117.5.658. [DOI] [PubMed] [Google Scholar]
- 31.Rim TH, Woo YJ, Park HJ, Kim SS. Current status and future expectations of cataract surgery in Korea: KNHANES IV. J Korean Ophthalmol Soc. 2014;55:1772–1778. [Google Scholar]
- 32.Wen G, Tarczy-Hornoch K, McKean-Cowdin R, et al. Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: multi-ethnic pediatric eye disease study. Ophthalmology. 2013;120:2109–2116. doi: 10.1016/j.ophtha.2013.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gupta A, Casson RJ, Newland HS, et al. Prevalence of refractive error in rural Myanmar: the Meiktila Eye Study. Ophthalmology. 2008;115:26–32. doi: 10.1016/j.ophtha.2007.02.025. [DOI] [PubMed] [Google Scholar]
- 34.Fotouhi A, Morgan IG, Iribarren R, et al. Validity of non-cycloplegic refraction in the assessment of refractive errors: the Tehran Eye Study. Acta Ophthalmol. 2012;90:380–386. doi: 10.1111/j.1755-3768.2010.01983.x. [DOI] [PubMed] [Google Scholar]
- 35.You QS, Wu LJ, Duan JL, et al. Factors associated with myopia in school children in China: the Beijing Childhood Eye Study. PLoS One. 2012;7:e52668. doi: 10.1371/journal.pone.0052668. [DOI] [PMC free article] [PubMed] [Google Scholar]