Abstract
Introduction
The SOCEUS survey aims to evaluate how contrast-enhanced ultrasound (CEUS) is effectively used in the focal liver lesions characterization.
Materials and methods
In the survey were involved Verona, Brescia and Trieste Radiological Centers and Arezzo and Bologna Non-radiological Centers. Inclusion criteria were liver focal lesion detection at conventional ultrasound and studied by means of CEUS, with or without CT or MRI examinations, done previous or subsequent to CEUS.
Results
1069 forms were collected. Patients with benign lesions, who did not undergo any other studies, were 255/561 (45.5 %). Among patients with diagnosis of hemangioma at CEUS, those who had no other investigations were 129/267 (48.3 %). Patients with malignant lesions who had studies pre-CEUS (CT and/or MRI) were 328/508 (65 %), whereas those who had examinations post-CEUS (CT and/or MRI) were 218/508 (42.9 %). Concordance rate between CEUS and CT investigations pre- and post-CEUS was, respectively, 66 and 89 %. Concordance rate between CEUS and MRI studies pre- and post-CEUS was, respectively, 87.5 and 81.5 %.
Conclusion
This study proves contrast-enhanced ultrasound correct application in the involved centers.
Keywords: Focal liver lesions, Contrast-enhanced ultrasound, CEUS, Multicenter study
Riassunto
Introduzione
Il sondaggio SOCEUS ha lo scopo di valutare come l’ecografia con mezzo di contrasto sia effettivamente impiegata nella caratterizzazione delle lesioni focali epatiche.
Materiali e Metodi
Nel sondaggio sono tati coinvolti i centri radiologici di Verona, Brescia e Trieste e i centri non radiologici di Arezzo e Bologna. I criteri di inclusione sono stati la presenza di lesione focale epatica all’esame ecografico convenzionale studiata con ecografia con mezzo di contrasto, con o senza correlazione TC or RM, prima o dopo l’esame ecografico.
Risultati
Sono state raccolte 1069 schede. I pazienti con lesioni benigne che non hanno fatto altri esami sono stati 255/561 (45.5 %). Dei pazienti con diagnosi di angioma alla ecografia con mezzo di contrasto, quelli che non hanno eseguito altre indagini sono stati 129/267 (48.3 %). I pazienti con lesioni maligne sottoposti ad indagini pre-ecografia con mezzo di contrasto (TC e/o RM) sono stati 328/508 (65 %), mentre quelli che hanno eseguito esami post- ecografia con mezzo di contrasto (TC e/o RM) sono stati 218/508 (42.9 %). La concordanza tra ecografia con mezzo di contrasto ed esame TC pre- e post-ecografia con mezzo di contrasto sono rispettivamente state pari al 66 e 89 %. La concordanza tra l’ecografia con mezzo di contrasto e l’esame RM pre- e post-ecografia con mezzo di contrasto sono state rispettivamente di 87.5 e 81.5 %.
Conclusione
Lo studio prova che l’ecografia con mezzo di contrasto è utilizzata correttamente nei Centri valutati.
Introduction
Ultrasound study is often the first examination in liver pathology study, due to its ubiquity and its low cost. However, very often a focal liver lesion detection causes diagnostic problems, due to poor specificity of many findings that cannot be classified easily [1].
The application of contrast-enhanced ultrasound (CEUS) during a conventional ultrasound study can improve the differentiation among benign and malignant liver focal lesions, thus avoiding the use of CT and MRI in those cases of benign lesions with atypical appearance at conventional ultrasound [2].
In 2004, the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) edited first CEUS guide lines, then updated in 2008 and in 2012, recommending in clinical practice the use of CEUS in evaluation of liver focal lesions [3–5]. According to the National Health Institute Italian guide lines, use of CEUS is recommended for the detection and the characterization of focal liver lesions [6].
The SOCEUS project (Survey CEUS—Contrast-Enhanced Ultrasound) is a multicenter retrospective study based on clinical records of three radiological institutes and two non-radiological institutes, with the aim of evaluating CEUS role in diagnostic work-up of focal liver lesions in centers that use highly this imaging method.
After many years of introduction of CEUS in Italy (2001), this study aims to evaluate how this imaging method is effectively used in focal liver lesions characterization: specifically, if it is used as a “problem-solving” examination in doubtful cases at conventional ultrasound or, at least, if it is considered as an added value to the reference imaging methods CT and MRI.
Materials and methods
In this survey were involved Verona, Brescia and Trieste Radiological Centers and Arezzo and Bologna Non-radiological Centers. They were asked to fill in forms series about CEUS studies done in patients with liver focal lesions in the triennium 2010–2013. Inclusions criteria were liver focal lesion detection at conventional ultrasound and/or at CEUS study, with or without a CT or MRI examinations, previous or subsequent to CEUS, describing the lesion, in the same institute or in a different one.
A form was used for data collections. In this form it was asked to insert data from imaging medical reports (conventional ultrasound, CT and MRI), to provide a detailed description, to suggest the diagnostic hypothesis at the end of every study and to specify temporal order of examinations execution. So this study was based on the analysis of medical reports written during studies execution and it did not provide for images revision in retrospect.
No informed consent was necessary in this retrospective study.
Data analysis
All forms received from involved centers were analyzed independently and clustered for diagnosis, evaluating the presence of CT and/or MRI studies pre- and post-CEUS examination and the concordance among diagnosis and enhancement patterns at CEUS with reference imaging methods. Later, the obtained results from different centers were compared among them.
The appearance of every focal liver lesions in different examinations was considered concordant both when was reported the same enhancement pattern after contrast medium injection and when was reported the same conclusive diagnosis, in the absence of enhancement pattern description.
Results
1069 forms were collected. From these 1069, 656 from radiological centers (395 men and 261 women, age 22–96 years) and 413 from non-radiological centers (198 men and 215 women, age 17–90 years).
Contrast-enhanced ultrasound (CEUS) and reference imaging methods
Patients with liver focal lesions investigated at CEUS with studies pre-CEUS (CT and MRI) were 506/1069 (47.3 %); patients with studies post-CEUS were 379/1069 (35.4 %); patients who were studied only with CEUS were 277/1069 (25.9 %).
Discriminating the results on different examinations type (CT or MRI), it was seen that 445/1069 patients had CT studies pre-CEUS (41.6 %), of which 362/445 (81.3 %) in the same institute, and that 230/1069 patients had CT post-CEUS (21.5 %). MRI investigations pre-CEUS were 95/1069 (8.9 %), of which 75/95 (78.9 %) in the same institute; MRI studies post-CEUS were 172/1069 (16.1 %).
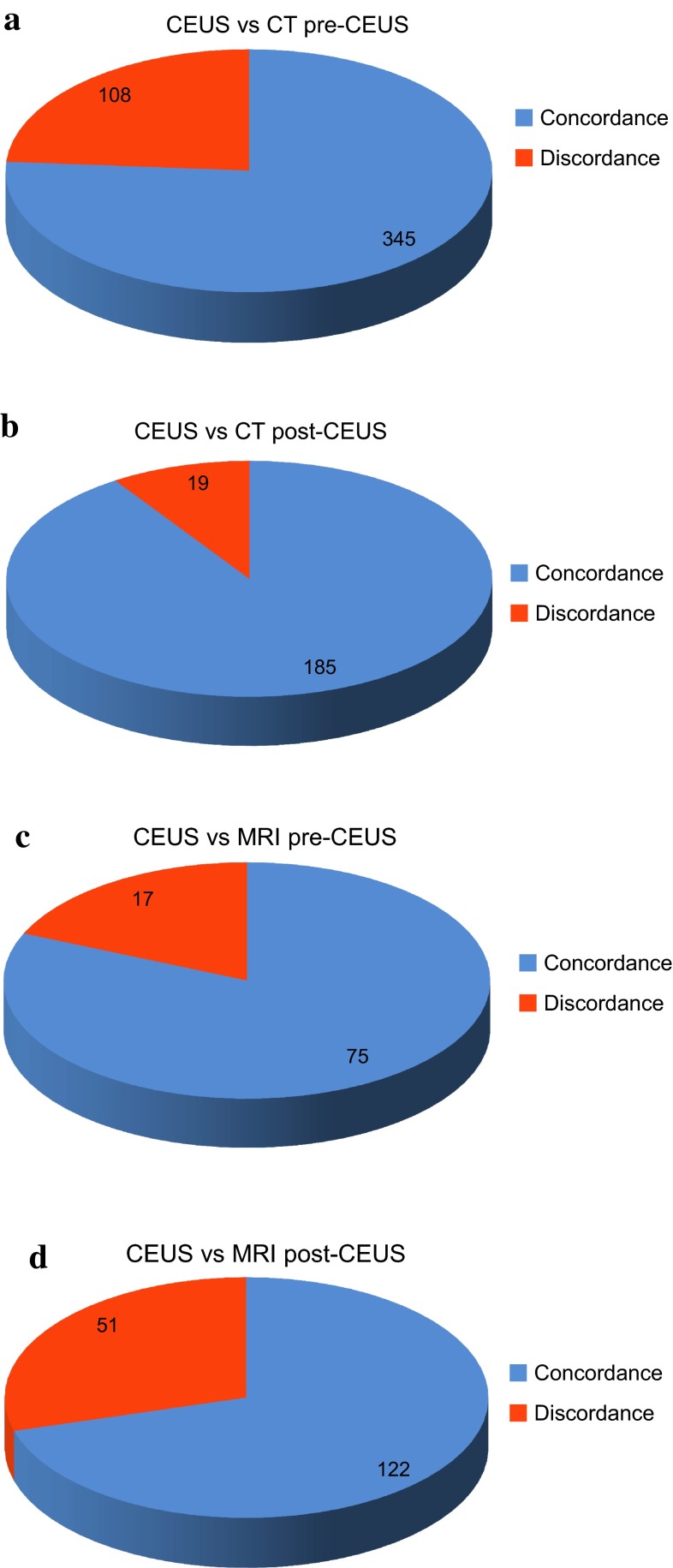
Analyzing the concordance among different described enhancement patterns and reported diagnosis at CEUS, CT and MRI investigations (Fig. 1), it was found that in patients who had CT pre-CEUS the concordance rate was of 333/445 (74.8 %), in patients who had CT post-CEUS the concordance rate was of 194/230 (84.3 %), in patients who had MRI pre-CEUS the concordance rate was of 74/95 (77.9 %) and in patients who had MRI post-CEUS the concordance rate was of 123/172 (71.6 %).
Fig. 1.
Concordance between CEUS and reference imaging methods. CEUS vs CT pre (a) and CT post (b) CEUS. CEUS vs MRI pre (c) ad MRI post (d) CEUS
At CEUS was overall diagnosed 561/1069 (52.5 %) benign lesions and 508/1069 (47.5 %) malignant lesions.
Benign lesions
Benign lesions diagnosed by CEUS were: hemangioma (267/561, 47.6 %), focal nodular hyperplasia (128/561, 22.8 %), not specified benign lesion (43/561, 7.7 %), regenerative nodule (36/561, 6.4 %), fatty focal area (24/561, 4.3 %), simple cyst (16/561; 2.9 %), focal fatty sparing area (15/561, 2.7 %), surgical results (12/561, 2.1 %), necrotic nodule (5/561, 0.9 %), abscess (4/561, 0.7 %), parasitic cyst (4/561, 0.7 %), shunt (3/561, 0.5 %), biliary cystadenoma (3/561, 0.5 %), adenoma (1/561, 0.2 %).
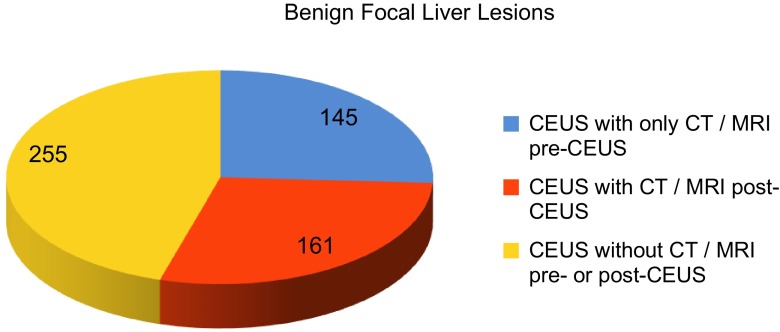
Patients with benign lesion (Fig. 2) who did not undergo other studies were 255/561 (45.5 %). Patients who had pre-CEUS studies (CT or MRI) were 178/561 (31.7 %); those who had only pre-CEUS studies were 145/561 (25.8 %). Patients who had post-CEUS examinations (CT or MRI) were 161/561 (28.7 %).
Fig. 2.
CEUS examinations in patients with benign focal liver lesions
Concordance rate among CEUS and CT investigations pre-CEUS and CT post-CEUS was, respectively, 64.9 and 62.1 %. Concordance rate among CEUS and MRI examinations pre-CEUS and MRI post-CEUS was, respectively, 64.1 and 65.4 %.
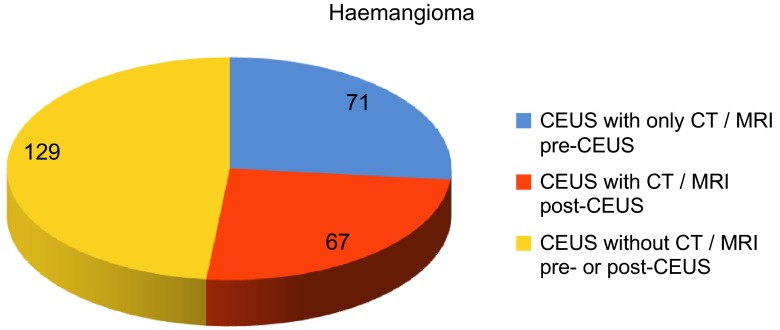
Regarding patients with diagnosis of hemangioma at CEUS (Fig. 3), those who had no other investigations were 129/267 (48.3 %). Those who had CT pre-CEUS were 79/267 (29.6 %), of which 59/79 (74.6 %) in the same institute where CEUS was done; in 61/79 (77.2 %) cases there was concordance between the two different imaging methods. Patients who had CT post-CEUS were 33/267 (12.4 %) and among which there was concordance in 26/33 (78.9 %) cases. Patients with diagnosis of hemangioma who had MRI pre-CEUS were 13/267 (4.9 %), of which 6/13 (46.2 %) in the same institute where CEUS was done; in 10/13 (76.9 %) cases there was concordance between the two different imaging methods. Patients who had MRI post-CEUS were 40/267 (15 %) and among which there was concordance in 29/40 (72.5 %) cases.
Fig. 3.
CEUS examinations in patients with hemangioma atypical at conventional ultrasound study
Patients with diagnosis of focal nodular hyperplasia at CEUS that were not studied with other kind of investigations were 96/128 (75 %). Those who had studies pre-CEUS (CT or MRI) were 12/128 (9.4 %), of which 10/128 (7.8 %) had only studies pre-CEUS. Patients who had CT or MRI post-CEUS were 22/128 (17.2 %). Patients who had CT pre-CEUS were 4/128 (3.1 %) and they had it in the same institute where CEUS was done, all of them with concordance between the two studies. Those who had CT post-CEUS, in the same institute were 2/128 (1.5 %) and the 50 % demonstrated concordance between the two investigations. Patients with diagnosis of focal nodular hyperplasia who had MRI pre-CEUS were 8/128 (6.2 %), of which 8/8 in the same institute where CEUS was done and there was concordance in 7/8 (87.5 %) cases. Those who had MRI post-CEUS in the same institute were 20/128 (15.6 %); in 18/20 (90 %) cases there was concordance between the two different studies.
Malignant lesions
Malignant lesions were: metastases (264/508, 52 %), hepatocellular carcinoma (194/508, 38.1 %), cholangiocarcinoma (24/508, 4.7 %), not specified malignant lesion (21/508, 4.1 %), lymphoma (2/508, 0.4 %), metastases from hypervascular tumors (2/508, 0.4 %), gallbladder carcinoma (1/508, 0.2 %).
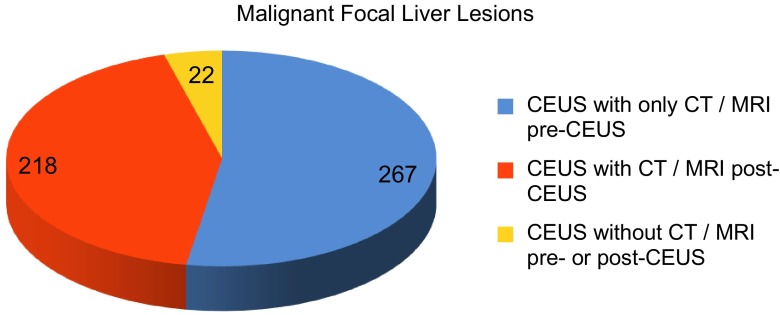
Patients with malignant lesions at CEUS (Fig. 4) who had no other examinations (CT and/or MRI) were 22/508 (4.3 %).
Fig. 4.
CEUS examinations in patients with malignant focal liver lesions
Patients who had imaging studies pre-CEUS (CT and/or MRI) were 328/508 (65 %), of which 268/508 (52.8 %) patients who had only investigations pre-CEUS. Those who had examinations post-CEUS (CT and/or MRI) were 218/508 (42.9 %). Concordance rate among CEUS and CT studies pre-CEUS and post-CEUS was, respectively, 66 and 89 %. Concordance rate among CEUS and MRI examinations pre- and post-CEUS was, respectively, 87.5 and 81.5 %.
Patients with diagnosis of metastases at CEUS who had CT pre-CEUS were 178/264 (67.4 %), of which 120/178 in the same institute. There was concordance in 160/178 (89.9 %) cases. Patients with diagnosis of metastases at CEUS who had CT post-CEUS in the same institute were 71/264 (26.9 %) and in 63/71 (88.7 %) cases there was concordance. Patients with diagnosis of metastases at CEUS who had MRI pre-CEUS were 23/264 (8.7 %), of which 16/23 (7 %) in the same institute and in 20/23 (87 %) cases there was concordance. Those who had MRI post-CEUS in the same institute were 18/264 (6.8 %) and in 14/18 (77.8) cases there was concordance.
Patients with diagnosis of hepatocellular carcinoma (HCC) at CEUS who had pre-CEUS examinations (CT or MRI) were 110/193 (52.3 %) and those who had only pre-CEUS studies were 77/193 (39.9 %). Patients who had post-CEUS investigations (CT or MRI) were 116/193 (60.1 %). So every patient had at least a study pre- or post-CEUS.
Patients with diagnosis of HCC at CEUS who had CT pre-CEUS were 97/193 (50.2 %), of which 93/97 (95.9 %) in the same institute. From which, in 78/97 (80.4 %) cases there was concordance between the two imaging methods. Patients with diagnosis of HCC at CEUS who had CT post-CEUS were 82/193 (42.5 %) and in 75/82 (91.5 %) cases there were concordance. Patients with diagnosis of HCC at CEUS who had MRI pre-CEUS were 25/193 (13 %), of which 23/25 (92 %) in the same institute and from which in 23/25 (92 %) there was concordance between the two studies. Those with diagnosis of HCC at CEUS who had MRI post-CEUS were 39/193 (20 %) and in 34/39 (87.2 %) there was concordance.
Reference imaging methods and Radiological department and Non-Radiological Department
In radiological institutes
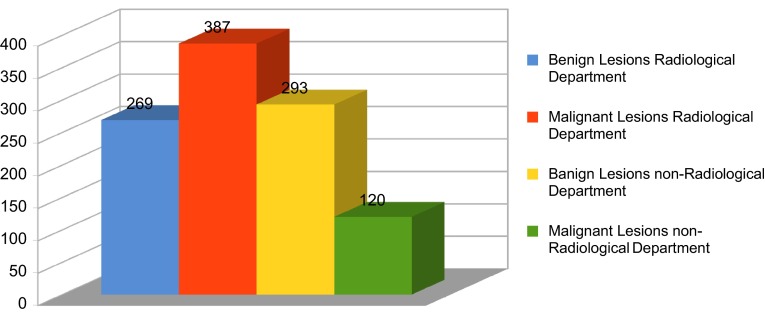
Regarding radiological institutes (Fig. 5); benign lesions were 269/656 (41 %) and malignant lesions were 387/656 (59 %).
Fig. 5.
Benign and malignant focal liver lesions in radiological and non-radiological departments
Patients who had neither pre-CEUS studies nor post-CEUS studies were 85/656 (13 %). Patients who had pre-CEUS examinations were 396/656 (60 %), and those who had only pre-CEUS examinations were 287/656 43.7 %). Patients who had post-CEUS investigations were 284/656 (43.3 %).
Concordance rate among CT pre- and post-CEUS studies was, respectively, 84.3 and 83.6 %. Concordance rate among MRI pre- and post-CEUS investigations was, respectively, 79.5 and 75.8 %.
Patients with benign lesion at CEUS who had CT pre-CEUS were 111/269 (41.3 %), of which 90/111 (81.1 %) in the same institute where CEUS was done. Of patients who had CT pre-CEUS, in 77/111 (69.4 %) cases there was concordance between the two imaging methods. Patients with benign lesion at CEUS who had CT post-CEUS in the same institute were 45/269 (16.7 %) and in 23/45 (51.1 %) there was concordance. Patients with benign lesions at CEUS who had MRI pre-CEUS were 29/287 (10.1 %), of which 20/29 (69 %) in the same institute and among these latter cases, in 20/20 (100 %) there was concordance between the two studies. Patients with benign lesion at CEUS who had MRI post-CEUS were 77/269 (28.6 %) and in 55/77 (71.4 %) there was concordance.
Patients with malignant lesion at CEUS who had CT pre-CEUS were 240/388 (61.9 %), of which 179/240 (74.6 %) in the same institute. From those who had CT pre-CEUS in the same institute, there was concordance in 211/240 (87.9 %) cases. Patients who had CT post-CEUS in the same institute were 138/388 (35.6 %) with concordance in 120/138 (87 %) cases. Patients with malignant lesion at CEUS who had MRI pre-CEUS were 43/388 (11.1 %), of which 33/43 (76.9 %) in the same institute. Of those who had MRI pre-CEUS in the same institute, 38/43 (88.4 %) cases show concordance between the two examinations. Patients with malignant lesion at CEUS who had MRI post-CEUS were 43/388 (11.1 %), and in 34/43 (81 %) cases there was concordance.
In non-radiological institutes
Regarding non-radiological institutes (Fig. 5), benign lesions were 293/413 (70.9 %) and malignant lesions were 120/413 (29.1 %).
Patients who had pre-CEUS investigations were 125/413 (30.3 %); of which 121/413 (29.3 %) patients had only pre-CEUS studies. Patients who had post-CEUS examinations were 95/394 (23 %). Patients who had no other investigations pre- and/or post-CEUS, apart from CEUS, were 197/413 (43.1 %).
Concordance rate among CEUS and CT pre- and post-CEUS studies was, respectively, 75 and 76.6 %. Concordance rate among CEUS and MRI pre- and post-CEUS investigations was, respectively, 81.2 and 84.6 %.
Patients with benign lesion at CEUS who had CT pre-CEUS were 40/274 (14.6 %), of which 22/40 (55 %) in the same institute. Of those who had CT pre-CEUS in the same institute, 18/22 (81.8 %) cases show concordance between the two studies. Patients who had CT post-CEUS in the same institute were 21/274 (7.7 %) and in 13/21 (61.9 %) cases there was concordance. Patients with benign lesions at CEUS who had MRI pre-CEUS were 9/293 (3.1 %). Among patients who had MRI pre-CEUS in the same institute, 7/9 (77.8 %) show concordance. Patients with benign lesion at CEUS who had MRI post-CEUS were 27/293 (9.2 %) and in 21/27 (77.8 %) there was concordance between the two imaging methods.
Patients with malignant lesion at CEUS who had CT pre-CEUS were 64/120 (53.3 %), of which 55/64 (85.9 %) cases show concordance. Those who had CT post-CEUS in the same institute were 26/120 (21.7 %), and in everyone there was concordance. Patients with malignant lesion at CEUS who had MRI pre-CEUS were 7/120 (5.8 %), and among those who underwent studies in the same institute, 6/7 (85.7 %) cases show concordance. Those who had MRI post-CEUS were 21/120 (17.5 %) and of which in 19/21 (90.5 %) there was concordance.
Discussion
In last 10 years several studies that proved CEUS value in liver focal lesions characterization were published, conferring CEUS a diagnostic role for indeterminate lesions detected at conventional ultrasound [7–10]. Regarding the accuracy, a multicenter study (DEGUM) pointed out that, for liver lesions, results are superimposable to those obtained with CT and MRI [2, 3]. Contrast medium injection addition to a conventional ultrasound study increases considerably accuracy and diagnostic confidence [11–13], therefore imposing CEUS application in liver focal lesions characterization detected at conventional ultrasound. Furthermore, it is reported CEUS application after non-diagnostic investigations (CT, MRI or CT-PET) [14–19].
In last National Health Institute Italian guidelines is recommended the use of CEUS for the characterization of focal liver lesions detected at conventional ultrasound [6]. The National Institute of Health and Care Excellence recommends contrast medium ultrasonography application not only for the evaluation of liver focal lesions with indeterminate features at conventional ultrasound, but also for those patients who cannot have CT or MRI examinations [20].
The discovery at CEUS of a typical benign lesion evidence could be sufficient for the diagnosis, without additional medical deepening need that would represent an useless additional cost. In reverse, atypical features impose additional deepening, as certainly expected and recommended [2, 3]. D’Onofrio et al. report a sensitivity of 95 % in the differential diagnosis among benign and malignant lesions investigated with contrast-enhanced ultrasound, resulting CEUS even better that CT in hypervascular focal lesions detection [21]. Furthermore, there are several papers centered also on the metastatic lesions identification at CEUS in comparison with referred imaging methods or pathological, that reported the high accuracy of CEUS [22–26]. However, if CEUS proves to be a reliable method in the ability of differentiating benign from malignant lesions, in the diagnosis of malignant liver focal lesion it is essential the integration with CT and/or MRI for the disease staging, for the greater panoramic view of these two imaging methods [9, 10].
EFSUMB guidelines recommend contrast media ultrasonography application in clinical practice for liver focal lesions evaluation [3–5].
This study is a survey and as a survey it has intrinsic limits in the evaluation model that can only take a picture of CEUS application in different involved centers. It means that it does not have the opportunity to show statistical analysis about method accuracy. Moreover, this study is a retrospective study and it is based only on the re-reading of medical reports, conferring to CT and MRI a gold standard role.
From this survey it deduces that in benign lesions evaluation, 71.3 % of patients who had CEUS did not undergo further additional research investigations, in particular, 74.9 % of patients with diagnosis of hemangioma at CEUS did not have other examinations; furthermore, CT and MRI studies post-CEUS done in patients group with diagnosis of hemangioma showed a concordance rate with contrast-enhanced ultrasound, respectively, 78.9 and 72.5 %.
Patients with benign lesions diagnosed at CEUS who had only studies pre-CEUS were 145/561 (25.8 %), those who had no investigations pre- or post-CEUS were 255/561(45.5 %). Summing up these data, it is highlighted how in 71.3 % of cases (400/561) CEUS was used as a “problem solving” method for the first-line diagnosis, as reported in literature and as recommended from guidelines previously mentioned. It is important to stress that CEUS is the cheapest imaging method for indeterminate focal liver lesion characterization detected at conventional ultrasound. In particular, it was proved that CEUS resulted particularly effective in benign liver lesions second-level evaluation in “pharmacoeconomic” terms [27–31].
Regarding malignant lesions characterization, CEUS showed a global concordance rate with CT and MRI pre- and post-CEUS of 79.4 %. From malignant lesions diagnosed at CEUS, only the 4.3 % of cases did not have any previous or further studies. We consider that this factor, in case of liver malignant lesion diagnosis, reveals a more panoramic imaging method need, that it can supply a complete systemic staging of disease.
Comparing statistical series of radiological institutes with ones of non-radiological institutes, it is shown how the number of research investigations done is higher in radiological centers, nevertheless there is no significant difference in concordance rate for diagnosis and enhancement features among CEUS and CT or MRI studies in different centers; in particular in radiological centers only 13 % of patients was evaluated only with contrast-enhancement ultrasound compared with the 43.1 % of non-radiological centers. These data are most likely suggestive of the high number of complex patients at the radiological centers. Indeed it is necessary to keep in mind that 59 % of lesions valued in radiological centers were malignant, compared to 29.1 % of those in non-radiological centers.
Also with previously described limits, we consider that our study proves the contrast-enhanced ultrasound correct application, pursuant to the official guidelines in the involved centers.
Compliance with ethical standards
Conflict of interest
The Authors declare that they have no conflict of interest.
Human rights statement and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5) and all patients provided written informed consent. The study was conducted in accordance with all institutional and national guidelines for the care.
References
- 1.Harvey CJ, Albrecht T (2001) Ultrasound of focal liver lesions. Eur Radiol [DOI] [PubMed]
- 2.Seitz K, Strobel D, Bernatik T, Blank W, Friedrich-Rust M, Herbay AV, Dietrich CF, Strunk H, Kratzer W, Schuler A. Contrast-enhanced ultrasound (CEUS) for the characterization of focal liver lesions—prospective comparison in clinical practice: CEUS vs. CT (DEGUM multicenter trial). Parts of this manuscript were presented at the Ultrasound Dreiländertreffen 2008, Davos. Ultraschall Med. 2009;30(4):383–389. doi: 10.1055/s-0028-1109673. [DOI] [PubMed] [Google Scholar]
- 3.Seitz K, Bernatik T, Strobel D, Blank W, Friedrich-Rust M, Strunk H, Greis C, Kratzer W, Schuler A. Contrast-enhanced ultrasound (CEUS) for the characterization of focal liver lesions in clinical practice (DEGUM Multicenter Trial): CEUS vs. MRI–a prospective comparison in 269 patients. Ultraschall Med. 2010;31(5):492–499. doi: 10.1055/s-0029-1245591. [DOI] [PubMed] [Google Scholar]
- 4.Claudon M, Cosgrove D, Albrecht T, Bolondi L, Bosio M, Calliada F, Correas JM, Darge K, Dietrich C, D’Onofrio M, Evans DH, Filice C, Greiner L, Jäger K, Jong ND, Leen E, Lencioni R, Lindsell D, Martegani A, Meairs S, Nolsøe C, Piscaglia F, Ricci P, Seidel G, Skjoldbye B, Thorelius L, Tranquart F, Weskott HP, Whittingham T. Guidelines and good clinical practise recommendation for contrast-enhanced ultrasound (CEUS) Ultraschall Med. 2008;29(1):28–44. doi: 10.1055/s-2007-963785. [DOI] [PubMed] [Google Scholar]
- 5.Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsøe CP, Piscaglia F, Wilson SR, Barr RG, Chammas MC, Chaubal NG, Chen MH, Clevert DA, Correas JM, Ding H, Forsberg F, Fowlkes JB, Gibson RN, Goldberg BB, Lassau N, Leen EL, Mattrey RF, Moriyasu F, Solbiati L, Weskott HP, Xu HX. World Federation for Ultrasound in Medicine; European Federation of Societies for Ultrasound. Guidelines and good clinical practice recommendations for Contrast Enhanced Ultrasound (CEUS) in the liver—update 2012: A WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultrasound Med Biol. 2013;39(2):187–210. doi: 10.1016/j.ultrasmedbio.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 6.- Sistema nazionale per le linee guida, Istituto superiore di sanità. Impiego della diagnostica per immagini delle lesioni focali epatiche. 2011
- 7.Tranquart F, Le Gouge A, Correas JM, et al. Role of contrast-enhanced ultrasound in the blinded assessment of focal lesions in comparison with MDCT and CEMRI: results from a multicenter clinical trial. EJC Suppl. 2008;6:9–15. doi: 10.1016/j.ejcsup.2008.06.003. [DOI] [Google Scholar]
- 8.Sporea I, Badea R, Martie A, et al. Contrast enhanced ultrasound for the evaluation of focal liver lesions in daily practice. A multicentre study. Med Ultrason. 2012;14:95–100. [PubMed] [Google Scholar]
- 9.Sporea I, Badea R, Popescu A, Spârchez Z, Sirli RL, Dănilă M, Săndulescu L, Bota S, Calescu DP, Nedelcu D, Brisc C, Ciobâca L, Gheorghe L, Socaciu M, Martie A, Ioaniţescu S, Tamas A, Streba CT, Iordache M, Simionov I, Jinga M, Anghel A, Cijevschi Prelipcean C, Mihai C, Stanciu SM, Stoicescu D, Dumitru E, Pietrareanu C, Bartos D, Manzat Saplacan R, Manzat Saplacan R, Pârvulescu I, Vădan R, Smira G, Tuţă L, Săftoiu A. Contrast-enhanced ultrasound (CEUS) for the evaluation of focal liver lesions—a prospective multicenter study of its usefulness in clinical practice. Ultraschall Med. 2014;35:259–266. doi: 10.1055/s-0033-1355728. [DOI] [PubMed] [Google Scholar]
- 10.Gaiani S, Celli N, Piscaglia F, Cecilioni L, Losinno F, Giangregorio F, Mancini M, Pini P, Fornari F, Bolondi L. Usefulness of contrast-enhanced perfusional sonography in the assessment of hepatocellular carcinoma hypervascular at spiral computed tomography. J Hepatol. 2004;41:421–426. doi: 10.1016/j.jhep.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 11.Quaia E, Calliada F, Bertolotto M, Rossi S, Garioni L, Rosa L, Pozzi-Mucelli R. Characterization of focal liver lesions with contrast-specific US modes and a sulfur hexafluoride filled microbubble contrast agent: diagnostic performance and confidence. Radiology. 2004;232(2):420–430. doi: 10.1148/radiol.2322031401. [DOI] [PubMed] [Google Scholar]
- 12.Bartolotta TV, Taibbi A, Midiri M, Matranga D, Solbiati L, Lagalla R. Indeterminate focal liver lesions incidentally discovered at gray-scale US: role of contrast-enhanced sonography. Invest Radiol. 2011;46(2):106–115. doi: 10.1097/RLI.0b013e3181f44184. [DOI] [PubMed] [Google Scholar]
- 13.Leen E, Ceccotti P, Kalogeropoulou C, Angerson W, Moug S, Horgan P. Prospective multicenter trial evaluating a novel method of characterizing focal liver lesions using contrast-enhanced sonography. AJR. 2006;186:1551–1559. doi: 10.2214/AJR.05.0138. [DOI] [PubMed] [Google Scholar]
- 14.Catalano O, Sandomenico F, Nunziata A, Vallone P, Raso MM, Setola SV, Gallipoli D’Errico A. Source and clinical motivation of orders for contrast-enhanced sonography (CEUS) of the liver: a prospective single-center survey. J Ultrasound. 2011;14:66–74. doi: 10.1016/j.jus.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lanka B, Jang HJ, Kim TK, Burns PN, Wilson SR. Impact of contrast-enhanced ultrasonography in a tertiary clinical practice. J Ultrasound Med. 2007;26:1703–1714. doi: 10.7863/jum.2007.26.12.1703. [DOI] [PubMed] [Google Scholar]
- 16.Laghi F, Catalano O, Maresca M, Sandomenico F, Siani A. Indeterminate, subcentimetric focal liver lesions in cancer patients: additional role of contrast-enhanced ultrasound. Ultraschall Med. 2010;31:283–288. doi: 10.1055/s-0029-1245383. [DOI] [PubMed] [Google Scholar]
- 17.Maruyama H, Takahashi M, Ishibashi H, Yoshikawa M, Yokosuka O. Contrast-enhanced ultrasound for characterisation of hepatic lesions appearing non-hypervascular on CT in chronic liver diseases. Br J Radiol. 2012;85:351–357. doi: 10.1259/bjr/20440141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoshizumi H, Maruyama H, Okugawa H, Kobayashi S, Akiike T, Yoshikawa M, Ebara M, Yokosuka O, Matsutani S, Kondo F, et al. How to characterize non-hypervascular hepatic nodules on contrast-enhanced computed tomography in chronic liver disease: feasibility of contrast enhanced ultrasound with a microbubble contrast agent. J Gastroenterol Hepatol. 2008;23(10):1528–1534. doi: 10.1111/j.1440-1746.2007.05184.x. [DOI] [PubMed] [Google Scholar]
- 19.Quaia E, De Paoli L, Angileri R, Cabibbo B, Cova MA. Indeterminate solid hepatic lesions identified on non-diagnostic contrast-enhanced computed tomography: assessment of the additional diagnostic value of contrast-enhanced ultrasound in the non-cirrhotic liver. Eur J Radiol. 2014;83:456–462. doi: 10.1016/j.ejrad.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 20.NICE diagnostics guidance. SonoVue (sulphur hexafluoride microbubbles)—contrast agent for contrast-enhanced ultrasound imaging of the liver. 2012
- 21.D’Onofrio M, Rozzanigo U, Masinielli BM, Caffarri S, Zogno A, Malagò R, Procacci C. Hypoechoic focal liver lesions: characterization with contrast enhanced ultrasonography. J Clin Ultrasound. 2005;33(4):164–172. doi: 10.1002/jcu.20111. [DOI] [PubMed] [Google Scholar]
- 22.Quaia E, D’Onofrio M, Palumbo A, Rossi S, Bruni S, Cova M. Comparison of contrast enhanced ultrasonography versus baseline ultrasound and contrast-enhanced computed tomography in metastatic disease of the liver: diagnostic performance and confidence. Eur Radiol. 2006;16(7):1599–1609. doi: 10.1007/s00330-006-0192-7. [DOI] [PubMed] [Google Scholar]
- 23.Krix M, Plathow C, Essig M, Herfarth K, Debus J, Kauczor HU, Delorme S. Monitoring of liver metastases after stereotactic radiotherapy using low-MI contrast-enhanced ultrasound initial results. Eur Radiol. 2005;15(4):677–684. doi: 10.1007/s00330-004-2620-x. [DOI] [PubMed] [Google Scholar]
- 24.Bleuzen A, Tranquart F. Incidental liver lesions: diagnostic value of cadence contrast pulse sequencing (CPS) and SonoVue. Eur Radiol. 2004;14(Suppl 8):P53–P62. doi: 10.1007/s10406-004-0079-0. [DOI] [PubMed] [Google Scholar]
- 25.Quaia E, Calliada F, Bertolotto M, et al. Characterization of focal liver lesions by contrast-specific US modes and a sulfur hexafluoride-filled microbubble contrast agent: diagnostic performance and confidence. Radiology. 2004;232:420–430. doi: 10.1148/radiol.2322031401. [DOI] [PubMed] [Google Scholar]
- 26.Dietrich CF, Kratzer W, Strobe D, Danse E, Fessl R, Bunk A, Vossas U, Hauenstein K, Koch W, Blank W, Oudkerk M, Hahn D, Greis C. Assessment of metastatic liver disease in patients with primary extrahepatic tumors by contrast-enhanced sonography versus CT and MRI. World J Gastroenterol. 2006;12:1699–1705. doi: 10.3748/wjg.v12.i11.1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Faccioli N, D’Onofrio M, Comai A, Cugini C. Contrast enhanced ultrasonography in the characterisation of benign focal liver lesion: activity-based cost analysis. Radiol Med. 2007;112:810–820. doi: 10.1007/s11547-007-0185-x. [DOI] [PubMed] [Google Scholar]
- 28.Romanini L, Passamonti M, Aiani L, Cabassa P, Raieli G, Montermini I, Martegani A, Grazioli L, Calliada F. Economic assessment of contrast-enhanced ultasonography for evaluation of focal liver lesions: a multicentre Italian experience. Eur Radiol. 2007;17(S6):99–106. doi: 10.1007/s10406-007-0234-5. [DOI] [PubMed] [Google Scholar]
- 29.Tranquart F, Correas JM, LadamMarcus V, Manzoni P, Vilgrain V, Aube C, Elmaleh A, Chami L, Claudon M, Cuilleron M, Diris B, Garibaldi F, Lucidarme O, Marion D, Beziat C, Rode A, Tasu JP, Trillaud H, Bleuzen A, Le Gouge A, Giraudeau B, Rusch E. Real-time contrast-enhanced ultrasound in the evaluation of focal liver lesions: diagnostic efficacy and economical issues from a French multicentric study. J Radiol. 2009;90(1 Pt 2):109–122. doi: 10.1016/S0221-0363(09)70089-7. [DOI] [PubMed] [Google Scholar]
- 30.Şirli R, Sporea I, Martie A, Popescu A, Dănilă M. Contrast enhanced ultrasound in focal liver lesions—a cost efficiency study. Med Ultrasonogr. 2010;12(4):280–285. [PubMed] [Google Scholar]
- 31.Piscaglia F, Leoni S, Cabibbo G, et al. Cost analysis of recall strategies for non-invasive diagnosis of small hepatocellular carcinoma. Dig Liver Dis. 2010;42:729–734. doi: 10.1016/j.dld.2010.03.003. [DOI] [PubMed] [Google Scholar]