We present an unusual case of a 52-year-old man diagnosed with multiple myeloma 7 years ago, with osteolytic lesions of the cranium, vertebrae and pelvic bone. Treatment included radiation therapy, chemotherapy and bisphosphonates, followed by autologous stem-cell transplantation. After that, he was treated with maintenance immunotherapy to maintain disease remission. Three years ago, the patient presented with painless swelling of the left testicle. Ultrasonography revealed an enlarged inhomogeneous left testicle, with increased vascularity. After biopsy (a plasmacytoma was diagnosed) and failed radiotherapy, radical orchiectomy was performed. Six months ago, the patient had an initial increase in volume of the right testicle; ultrasonography showed a modest increase in testicular volume (approximately 4 cm) surrounded by an anechoic septated fluid collection diagnosed as hematocele. Four months ago, ultrasound showed a further increase in testicular volume (approximately 5 cm), with an unchanged fluid collection around the testicle. A further control after 2 months showed further volume increase (approximately 7 cm) of the testicle, which appeared inhomogeneous and hypervascularized (Figs. 1, 2). After a biopsy (the diagnosis of plasmacytoma was confirmed) and failed radiotherapy, a second radical orchiectomy was performed. Pathology confirmed the diagnosis of plasmacytoma and chronic hematocele.
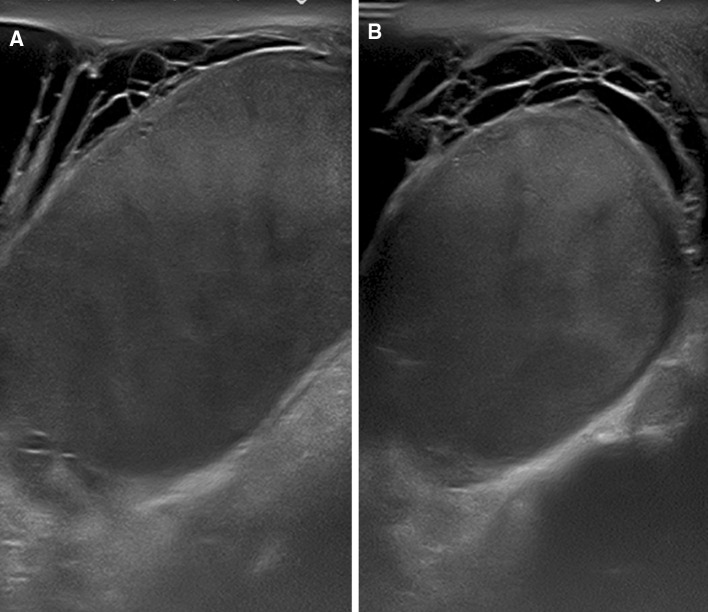
Fig. 1.
Last sonography control before radical orchiectomy. Scrotal ultrasound, sagittal (a) and transverse (b) view, show a diffusely enlarged heterogeneously echogenic right testicle surrounded by an anechoic septated fluid collection, diagnosed as hematocele
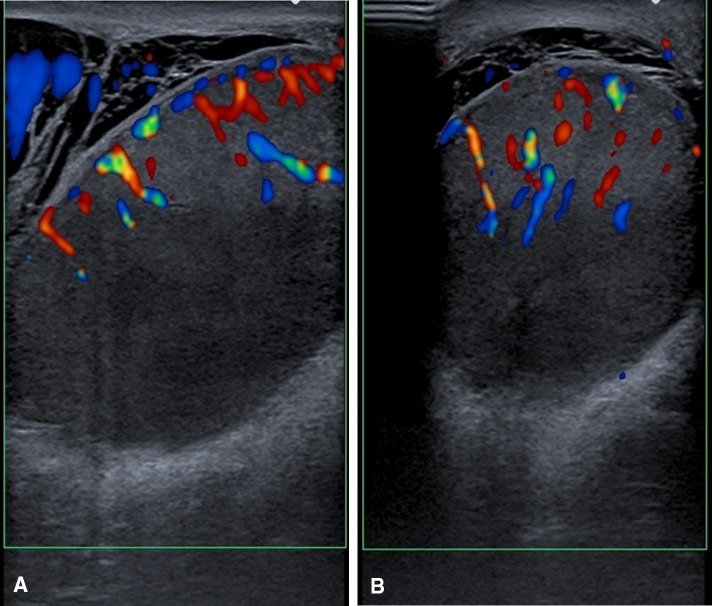
Fig. 2.
Last color Doppler control before radical orchiectomy. Scrotal color Doppler, sagittal (a) and transverse (b) view show increased intratesticular vascularity
The term plasmacytoma encompasses a spectrum of diseases ranging from indolent conditions to the more aggressive multiple myeloma, with a wide range of clinical manifestations [1]. Testicular plasmacytoma is a rare disease, either as a primary lesion or as a reflection of underlying multiple myeloma [2–4] and only a few cases of testicular forms have been reported in the literature, almost all affecting elderly patients [5]. The incidence of clinical testicular plasmacytoma is assumed to range from 0.03 to 0.1 % of all testis tumors. Bilateral involvement is extremely infrequent [6]. Clinically, testicular plasmacytoma presents as a gradually enlarging scrotal mass [2]. Physical examination reveals an enlarged, painless testicle, with a hard consistency and nodular surface [7]. Histopathology demonstrates diffuse infiltration of the interstitial tissue by abnormal plasma cells with seminiferous tubules retaining their architecture [7]. Ultrasound detected a gradual increase in testicular volume; however, the testicle maintains a relatively homogeneous echogenicity, unlike in other testicular malignancies [8]. The color Doppler examination shows increased vascularity, but this is often more modest than in other testicular tumors [9] and more similar to that of pseudotumors [10]. Sheath localizations are not described, unlike other testicular cancers [9, 11]. There are no consensus guidelines for testicular plasmacytoma treatment, but it is radiosensitive and radiation therapy provides excellent disease control in most cases; chemotherapy and surgery are to be considered when radiation therapy fails (Figs. 1, 2).
We decided to present this case because of its rarity (less than 50 cases reported in the literature) and to emphasize the sonographic appearance of testicular plasmacytoma, whose main features are the gradual volume increase of the testis, related to the infiltration of plasma cells, the slight inhomogeneity and the hypervascularization.
Compliance with ethical standards
Conflict of interest
The authors have no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. All patients provided written informed consent to enrolment in the study and to the inclusion in this article of information that could potentially lead to their identification.
Human and animal studies
The study was conducted in accordance with all institutional and national guidelines for the care and use of laboratory animals.
References
- 1.Ahnach M, Marouan S, Rachid M, et al. Extramedullary plasmocytoma relapsing at different sites: an unusual presentation. Pan Afr Med J. 2013;14:34. doi: 10.11604/pamj.2013.14.34.1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khan M, Rajarubendra N, Azer S et al (2015) Plasmacytoma of the testis in a patient with relapsed and refractory multiple myeloma: Case report and review of the literature. Urol Ann 7(4):530–533 [DOI] [PMC free article] [PubMed]
- 3.Roels P, Mattelaere P, Claikens B. Testicular plasmacytoma, an unusal testicular tumor. JBR-BTR. 2014 Mar-Apr;97(2):115-7 [DOI] [PubMed]
- 4.Lue K, Emtage JB, Pariñas MA, Dhillon J, Pow-Sang J (2015) An extramedullary plasmacytoma in the testicle: a case report and review of the literature. Can Urol Assoc J 9(3–4):E240–E242 [DOI] [PMC free article] [PubMed]
- 5.Raspollini MR (2014) Histologic variants of seminoma mimicking lymphatic malignancies of the testis: a literature review with a report of case series focusing on problems in differential diagnosis. Appl Immunohistochem Mol Morphol 22(5):348–357 [DOI] [PubMed]
- 6.Garrido Abad P, Coloma Del Peso A, Bocardo Fajardo G et al (2008) Secondary bilateral testicular plasmacytoma. Case report and review of the literature. Actas Urol Esp 32(10):1039–1042 [DOI] [PubMed]
- 7.Rosenberg S, Shapur N, Gofrit O, Or R. Plasmacytoma of the testis in a patient with previous multiple myeloma: is the testis a sanctuary site? J Clin Oncol. 2010;28(27):e456–e458. doi: 10.1200/JCO.2009.27.6519. [DOI] [PubMed] [Google Scholar]
- 8.Draghi F, Campani R, Calliada F. Color Doppler ultrasonography of the scrotum. Radiol Med. 1995;90(4):360–366. [PubMed] [Google Scholar]
- 9.Draghi F, Bonardi M, Dellabianca C, Tarantino CC, Alessi S. Lymphoma of the scrotum in patients with Down’s syndrome: US appearance. Mini-pictorial essay. J Ultrasound. 2011;14(4):216–219. doi: 10.1016/j.jus.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Depaoli R, Bartolucci F, Draghi F. Testicular adrenal rest tissue in a patient with classical congenital adrenal hyperplasia: color Doppler findings. J Ultrasound. 2013;16(2):81–84. doi: 10.1007/s40477-013-0015-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Draghi F, Schiavina G, Ferrozzi G, Bandini V, Consonni M (1996) Color Doppler findings of secondary carcinoma of the tunica vaginalis testis. J Clin Ultrasound 24(3):141–144 [DOI] [PubMed]