Abstract
Objective
This study evaluated the effect of two home-based exercise interventions (one culturally-adapted and one standard) on changes in Social Cognitive Theory (SCT) variables, physical activity (PA) and sedentary time (ST), and to determine the association between changes in SCT variables and changes in PA and ST in Hispanic breast cancer survivors.
Method
Project VIVA! was a 16-week randomized controlled pilot study to test the effectiveness and feasibility of a culturally-adapted exercise intervention for Mexican American and Puerto Rican breast cancer survivors in Houston, Texas and San Juan, Puerto Rico, respectively. Women (N=89) completed questionnaires on SCT variables, PA and ST and were then randomized to a 16-week culturally-adapted exercise program, a non-culturally adapted standard exercise intervention or a wait-list control group. Multiple regression models were used to determine associations between changes in SCT variables and changes in PA and ST.
Results
Participants were in their late 50s (58.5 ± 9.2 years) and obese (31.0 ± 6.5 kg/m2). Women reported doing roughly 34.5 minutes/day of PA and spending over 11 hours/day in sedentary activities. Across groups, women reported significant increases in exercise self-efficacy and moderate-intensity, vigorous-intensity, and total physical activity from baseline to follow-up (p<.05). Increased social support from family was associated with increases in vigorous-intensity PA. Increases in social modeling were associated with increases in moderate-intensity and total PA and decreases in ST from baseline to follow-up (p<.05).
Conclusions
Hispanic cancer survivors benefit from PA interventions that focus on increasing social support from family and friends and social modeling.
BACKGROUND
The prevalence of cancer survivors in the U.S. is projected to increase by 31% over the next decade [1]. Women with breast cancer are one of the largest groups of cancer survivors, accounting for 22% of the survivor population, and 90% are expected to survive ≥5 years post diagnosis [2]. As this number increases and the population ages, there is a greater risk of developing other chronic diseases, such as cardiovascular disease and diabetes [3, 4]. However, recent evidence suggests that simple lifestyle changes (e.g., moving more, sitting less) could decrease mortality and increase survivorship [5].
Physical activity lowers the risk of recurrence and development of other chronic diseases in cancer survivors [6], yet 95.5% of long-term cancer survivors are insufficiently active [7]. Among breast cancer survivors, specifically, cohort studies have shown that women who are physically active post-diagnosis experience a 30–50% reduced risk of dying from breast cancer [8]. Despite the known protective effect of physical activity, Hispanic breast cancer survivors are less likely to maintain a healthy weight and be physically active than Caucasian breast cancer survivors [9–11], highlighting the need for culturally-adapted physical activity promotion efforts that address the specific needs of Hispanic breast cancer survivors [12].
Social cognitive theory (SCT) has been used to understand physical activity adoption and maintenance in the general adult population through understanding core determinants of behavior [13]. These core determinants influence motivation to engage in healthful or health risk behaviors, and, operating through multiple mechanisms, suggest that social cognitive influences may mediate changes in health behaviors, such as engaging in physical activity or reducing sedentary behavior [14]. Perceived self-efficacy, social modeling and social support are key constructs in SCT that help explain how people both initiate and maintain physical activity and reduce sedentary behaviors over time [15–18].
Recent studies have sought to understand how perceived self-efficacy, social modeling and social support influence physical activity adoption in breast cancer survivors in home- and lab-based settings [19, 20], and have consistently identified SCT constructs as determinants of physical activity adherence among cancer survivors [21, 22]. However, no study to date has explored SCT influences on physical activity and sedentary time exclusively among Hispanic cancer survivors, who are at greater risk of not meeting leisure-time physical activity guidelines and disproportionately suffer from comorbidities (e.g., cardiovascular disease and diabetes) [10, 11]. Culturally-adapted interventions that incorporate specific cultural values and tradition have shown promise for improving health outcomes in the general Hispanic adult population and take into account factors that may promote health behavior change that may be unique to Hispanics [23, 24]. However, culturally-adapted interventions typically lack a strong theoretical framework [19, 24], and it is still unknown whether a culturally-adapted home-based intervention will lead to changes in SCT determinants and how those changes are related to changes in physical activity and sedentary time among Hispanic breast cancer survivors.
Thus, the primary purpose of this study was to assess the effect of two home-based exercise interventions (one culturally-adapted and one standard) on changes in SCT variables, including exercise self-efficacy, barrier self-efficacy, social modeling and social support, physical activity and sedentary time in Hispanic breast cancer survivors. A secondary purpose of this study was to explore the relationship between changes in SCT variables and changes in physical activity and sedentary time. We hypothesized that (1) participants in the culturally-adapted intervention group would experience greater changes in SCT variables, physical activity and sedentary time than participants in the standard exercise intervention and control groups and (2) that changes in SCT variables would be associated with increased physical activity and decreased sedentary time.
METHODS
Study Design, Setting and Participant Selection
Project VIVA! was a 16-week randomized controlled pilot study to test the effectiveness and feasibility of a culturally adapted exercise intervention for Mexican American and Puerto Rican breast cancer survivors in Houston, Texas and San Juan, Puerto Rico, respectively. Project VIVA! procedures and materials were reviewed and approved by Institutional Review Boards of The University of Texas MD Anderson Cancer Center and the Medical Sciences Campus of the University of Puerto Rico, and participants provided written informed consent prior to participation.
The setting for this study was two urban metropolitan areas, Houston, Texas and San Juan, Puerto Rico. Houston has a population of 5.8 million (43.8% Hispanic or Latino), and Houston residents are mostly (62.2%) English-speaking (28.9% speak Spanish at home), 30.9% earned a Bachelor’s degree or higher, and 15.7% are below the federal poverty level [25]. Although educational attainment is similar in San Juan to Houston (26.6% earned a Bachelor’s degree or higher), 93.5% of San Juan residents speak Spanish at home (6.2% speak English) and 40.5% of the population lives below the federal poverty level, which was $23,550 for a family of 4 in 2013 [25, 26].
Sedentary women 21 years of age and older who self-identified as Mexican American residing in Houston or Puerto Rican residing in San Juan were recruited to the study in Houston between 2011 and 2013. Participants were recruited from the MD Anderson Cancer Center Breast Clinic and from previous studies. Women recruited from the Breast Clinic were identified by research team members via medical records and were called and given more information about the study. Women diagnosed with breast cancer (stages I-IV) who were at least three months post-treatment, not meeting current physical activity recommendations [27], able to read and write in English or Spanish, and able to provide informed consent were eligible to participate and were consented in person or by mail. Participants completed an in-person health assessment and questionnaires at baseline and 16-week follow-up with a trained research staff member. Only participants (N=89, 45 in Houston and 44 in Puerto Rico) who successfully completed both assessments were included in this study. In the final sample, 30 participants (15 each in Houston and Puerto Rico) were included from the culturally-tailored exercise intervention, 29 (15 in Houston and 14 in Puerto Rico) from the standard exercise intervention, and 30 (15 each in Houston and Puerto Rico) from the control group. All recruitment and data collection activities took place between November 2011 and July 2014.
Procedures
Upon arrival at their assessment, participants completed interviewer-administered questionnaires, if not completed prior to their assessment. Women were then randomized using a minimization procedure to a culturally-adapted exercise intervention, a non-culturally-adapted standard exercise intervention, or a wait-list control treatment group.
Women randomized to the culturally-adapted and standard exercise interventions completed a 16-week comprehensive exercise program that targeted aerobic exercise, muscular strength, and flexibility training. The intervention was primarily home-based, and the intensity and duration levels of exercise were developed based on individual participants’ baseline fitness assessments and medical history and were consistent with ACSM guidelines [28]. Participants in the intervention groups were given two sets of resistance bands, a pedometer, an exercise book and a video with the prescribed exercises for use at home and were asked to complete their exercises twice a week. Group exercise sessions were held once a month, and participants were encouraged to attend at least two throughout the program.
In addition to the exercise program, women in the exercise intervention groups received biweekly phone calls to check on their progress and biweekly newsletters. Women in the culturally-adapted exercise intervention received newsletters that were tailored to Latinas and breast cancer survivors. Tailored materials included information on self-efficacy, social modeling and social support and used culturally relevant images, messages and examples, whereas women in the standard exercise intervention received newsletters that were not tailored to Latinas. For example, a culturally-adapted newsletter on the importance of social support would highlight the importance of “la familia” and emphasize doing exercises, like salsa dancing, with the family. Women in the wait-list control group were asked to continue with their normal activities and did not receive any additional programs, materials or incentives.
Measures
Sociodemographics
A short demographic survey was administered to all eligible participants at baseline. Information on age, race and ethnicity, educational level and household income were collected. Height and weight were measured on a calibrated stadiometer and scale and used to calculate body mass index (BMI=kg/m2).
SCT Variables
Exercise self-efficacy was assessed using a questionnaire developed by the research team based on scales by McAuley [29–32] The questionnaire assess survivors’ confidence in completing a graded series of exercise tasks. For example, the stem, “How confident are you that you can…,” was used with items like “walk briskly without stopping for 5 minutes?” Responses range from 1 (not at all confident) to 5 (extremely confident). The time frame used for minutes of walking ranged from 2 minutes to 1 hour (2 minutes, 5 minutes, 10 minutes, 20 minutes, 30 minutes, 45 minutes, 1 hour). Responses to the seven individual items were summed to obtain an overall score ranging from 7 to 35. Internal consistency (Cronbach’s alpha) was r=0.96 in this sample.
Barriers self-efficacy was measured using the Cancer Survivors’ Exercise Barriers Self-efficacy Scale, which is based on questionnaires developed by Marcus [33–35] and was adapted to include items based on elicitation interviews with breast cancer survivors from a previous study [35, 36]. The scale included 14 items that measured a participant’s confidence in continuing exercise in the face of common barriers. For example, items used the stem, “How confident I am that I can exercise…,” with items like “…when I am tired” and “when I am traveling.” Responses to the 14 individual items were summed to obtain an overall score ranging from 14 to 70, and Cronbach’s alpha was r=0.88 in this study.
Social modeling of physical activity was assessed using 8 items developed for a previous study in endometrial cancer survivors [37]. Participants were given a list of things that happened that day (e.g. “You noticed people exercising,” “A friend or family member offered to exercise with you,” and “You read or heard news stories about people exercising”) and were asked to respond “yes” or “no”. The total number of “yes” responses was summed to obtain an overall score ranging from 0 to 8, and internal consistency was r=0.75 in this sample.
The Social Support for Exercise Survey was used to assess the level of support participants felt they received from family and friends while making changes to their physical activity behavior [38]. The survey includes ten items to measure family and friend support using a 5-point scale, ranging from 1 (none) to 5 (very often). The instrument has shown high internal consistency (αs=0.61–0.91) and test re-test reliability (ICC= 0.55–0.79) [38], and Cronbach’s alpha was r=0.88 in this study.
Physical Activity and Sedentary Time
The International Physical Activity Questionnaire (IPAQ) short form was used to measure physical activity and sedentary time over the past seven days [39]. Walking, moderate- and vigorous-intensity, and total physical activity was reported in hours and/or minutes per day and days per week and yielded total minutes of physical activity per week. Sitting time was self-reported as the amount of time in hours and/or minutes participants usually spent sitting on a weekday during the past seven days. The IPAQ short form instrument is designed for population surveillance of physical activity in diverse populations, is widely used and reliable (r=0.8), with acceptable validity (r=0.3) compared to accelerometry [39].
Sedentary behavior was also measured using a modified version of the Past-day Adults’ Sedentary Time (PAST) Questionnaire [40]. The questionnaire included seven items to assess time spent sitting or lying down and watching television/videos, using the computer/internet, reading, socializing with friends/family, driving/riding in a car or public transport, doing hobbies or doing other activities over the past week, in order to be comparable to IPAQ physical activity data. The PAST Questionnaire has shown fair to good fair to good test-retest reliability among breast cancer survivors (ICC=0.50).
Data Analysis
Baseline and 16-week follow-up data were used to determine the relationship between SCT variables and physical activity and sedentary time in a sample of Hispanic breast cancer survivors. Analysis of variance (ANOVA) and independent samples t-tests were used to test for significant differences in demographics, SCT variables, physical activity and sedentary time by study site (Texas, Puerto Rico) and treatment group (culturally-adapted, standard, control). Repeated measures ANOVAs were used to assess changes in SCT variables, physical activity and sedentary behaviors from baseline to post-intervention by treatment group and site. Multiple regression models were used to estimate the association between changes in SCT variables (follow-up – baseline) and physical activity and sedentary time at follow-up, adjusting for baseline physical activity/sedentary time, age, site and treatment group. To determine whether treatment group moderated the effect of changes in SCT variables on changes in physical activity and sedentary time, the culturally-adapted and standard exercise interventions were collapsed and compared to the control group and additional regression models with interaction terms were included in analyses. A significant interaction term indicated a differential relationship between an SCT variable and treatment group, providing support for a potential moderating effect of the intervention on physical activity and sedentary time. All statistical analyses were conducted in SPSS 22.0 (IBM SPSS Statistics, Armonk, NY), and effects were tested using a non-parametric bootstrapping procedure using 5,000 resamples from the data set. The significance level for all analyses was set at .05, and the effect was considered significant if the confidence interval of the effect did not include the value zero.
RESULTS
Participant Characteristics
On average, Hispanic breast cancer survivors were in their late 50s (M age=58.5 years, SD=9.2), obese (M BMI=31.0 kg/m2, SD=6.5), and roughly one-quarter (28.1%) graduated from college with a bachelor degree or higher. Puerto Rican women were older (M=58.5 versus 52.5 years, t=−2.931, p=.004) and had a higher BMI (M=32.8 versus 29.3 kg/m2, t=−2.638, p=.010) than women in Texas. On average, women attended 57.5% (M=2.3, SD=1.162) of the exercise group sessions and read 84.3% (M=5.9, SD=1.767) of the newsletters received. Participants in both the culturally-adapted and standard exercise interventions found the newsletters easy to understand (88.3% agreed or completely agreed) and helpful (82.4% agreed or completely agreed). Means (and SD) for SCT variables, physical activity and sedentary time are shown in Table 1.
Table 1.
Social cognitive variables, physical activity and sedentary time by site and time point
| Texas (N=45) | Puerto Rico (N=44) | |||
|---|---|---|---|---|
|
| ||||
| Baseline M±SD | Follow-up M±SD | Baseline M±SD | Follow-up M±SD | |
| Social Cognitive Theory Variables | ||||
| Exercise self-efficacya,b | 3.6±0.9 | 4.0±0.8 | 3.1±1.1 | 3.4±0.9 |
| Barriers self-efficacy | 2.6±0.7 | 2.5±0.9 | 2.5±0.7 | 2.6±0.8 |
| Social modelinga | 1.5±1.6 | 2.1±1.9 | 3.3±2.2 | 3.3±2.4 |
| Social support from familyc | 20.2±7.6 | 19.8±9.5 | 15.7±6.7 | 19.2±9.8 |
| Social support from friends | 16.9±8.3 | 17.6±9.2 | 16.2±9.2 | 16.1±8.6 |
| Physical Activity and Sedentary Time | ||||
| IPAQ walking (minutes/week)b,c | 177.8±301.6 | 193.3±288.3 | 153.8±306.0 | 213.5±296.4 |
| IPAQ moderate-intensity (minutes/week)b,c | 73.2±194.2 | 140.7±290.9 | 21.6±67.9 | 99.8±245.7 |
| IPAQ vigorous-intensity (minutes/week)b,c | 49.0±96.8 | 96.6±210.6 | 8.2±38.5 | 71.2±156.3 |
| IPAQ total (minutes/week)b,c | 300.0±183.6 | 430.5±628.9 | 183.6±346.2 | 384.5±503.3 |
| IPAQ sitting time (minutes/week) | 1701.8±1307.2 | 2046.2±1543.0 | 1622.7±1520.0 | 1500.7±1473.4 |
| Total sedentary time (hours/week) | 36.8±39.2 | 31.6±24.0 | 47.0±35.6 | 42.4±30.3 |
Statistically significant difference by site at baseline and follow-up, p<.05
Statistically significant difference by time point across sites, p<.01
Statistically significant difference by site at baseline, but not follow-up, p<.05
Changes over Time
Repeated measures ANOVA did not show any significant time by group (culturally-adapted, standard and control) interaction effects, but there was a main effect for time for exercise self-efficacy (F(1,77)=9.170, p=.003) and moderate-intensity (F(1,76)=7.659, p=.007), vigorous-intensity (F(1,76)=6.465, p=.013), and total (F(1,76)=9.323, p=.003) physical activity. There was a significant time by site interaction for social support from family (F(1,78)=6.729, p=.011); women in Texas reported decreased social support from family from baseline to follow-up, while women in Puerto Rico reported increased social support from family over time. There were no other significant time by site effects, but there was a main effect for time for exercise self-efficacy (F(1,78)=9.093, p=.003) and moderate-intensity (F(1,77)=7.766, p=.007), vigorous-intensity (F(1,77)=6.383, p=.014), and total (F(1,77)=9.462, p=.003) physical activity.
Regression Models
Multiple regression models were used to assess the association between changes in SCT variables and changes in physical activity and sedentary time. In unadjusted models, changes in exercise self-efficacy were significantly associated with changes in walking (B=67.044, SE=29.393, p=.031, 95% CI: 5.942, 123.577, R2=.059), and this association remained significant (B=62.848, SE=31.390, p=.046, 95% CI: 0.958, 124.517, R2=.068) after adjusting for age, site and treatment group, suggesting that increases in exercise self-efficacy were associated with increases in walking from baseline to follow-up.
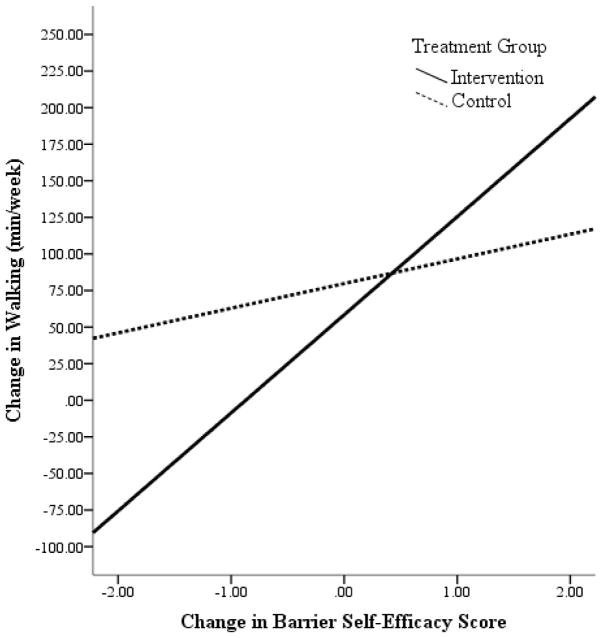
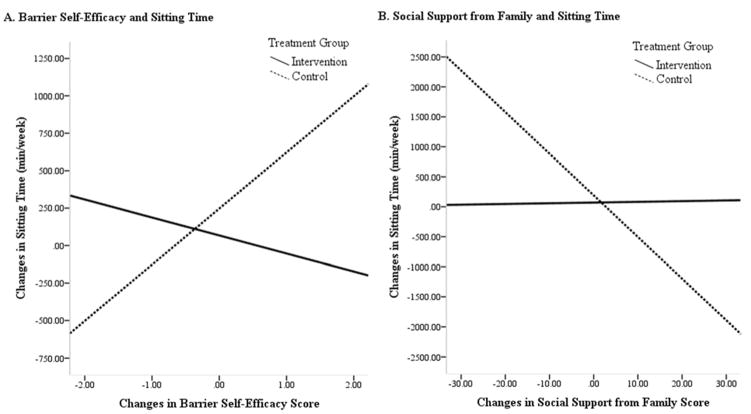
Treatment group moderated the effects of barrier self-efficacy on walking and sitting time and the effects of social support from family on sitting time. Figure 1 illustrates that as barrier self-efficacy increased, walking increased in both groups, but women in the intervention group experienced greater changes in walking than those in the control group. Figure 2A illustrates that as barrier self-efficacy increased, women in the intervention group reported decreases in sitting time while women in the control group reported increases in sitting time, and Figure 2B illustrates the opposite effect, indicating that as social support from family increased, women in the intervention group reported slight increases in sitting time while women in the control group reported large decreases in sitting time.
Figure 1.
Moderating effects of treatment group on the relationship between changes in barrier self-efficacy and walkinga
aModel adjusted for baseline physical activity or sedentary time, age and site.
This figure depicts the moderating effect of treatment group on the relationship between changes in barrier self-efficacy and walking. Increases in barrier self-efficacy were associated with reported increases in walking in the intervention group, whereas women in the control group reported only slight increases in walking from baseline to 16-week post-intervention (B=41.978, SE=21.129, p=.052, 95% CI: 1.160, 82.463, R2=.066).
Figure 2.
Moderating effects of treatment group on the relationship between changes in sitting time and (A) barrier self-efficacy and (B) social support from familya
aModels adjusted for baseline physical activity or sedentary time, age and site.
This figure depicts the moderating effect of treatment group on the relationships between (A) changes in barrier self-efficacy and sitting time and (B) changes in social support from family and sitting time. Figure A shows that increases in barrier self-efficacy were associated with reported decreases in sitting time in the intervention group, whereas women in the control group reported large increases in sitting time from baseline to 16-week post-intervention (B=727.443, SE=371.008, p=.051, 95% CI: 15.864, 1479.691, R2=.414). Figure B shows that increases in social support from family were associated with little change in sitting time in the intervention group, but women in the control group reported decreases in sitting time from baseline to 16-week post-intervention (B=−90.736, SE=38.824, p=.013, 95% CI: −153.778, −7.661, R2=.425).
CONCLUSIONS
This study found that changes in SCT variables resulting from participation in an exercise intervention led to increased physical activity and decreased sedentary time in Hispanic breast cancer survivors. Results suggest that exercise self-efficacy had the greatest influence on physical activity across groups. Moderation analyses revealed that barrier self-efficacy and social support from family differentially influenced physical activity and sedentary time in women by treatment group, suggesting that the exercise intervention was most effective for increasing barrier self-efficacy, leading to increased walking and decreased sedentary time. Although there were no significant differences in the effects of the culturally-adapted versus the standard exercise intervention as hypothesized, findings suggest that an SCT-driven exercise intervention may be effective for getting Hispanic survivors to meet current American Cancer Society lifestyle behavior recommendations, including moving more and sitting less [41]. Findings from this study are of great public health interest, given the considerable health benefits and reduced mortality rates associated with increased physical activity and reduced sedentary time [5] and the characteristically low levels of physical activity in Hispanics cancer survivors at a population level [7, 9–11].
The results from this study contribute to our understanding of the influence of social cognitive factors on health behaviors in cancer survivors. There are only two other known studies that have tested the efficacy of adapted or tailored print materials for promoting physical activity and reducing sedentary time among cancer survivors, the Move More for Life study [20, 42, 43] and the FRESH START trial [44]. Though similar, there are a number of differences between these trials and Project VIVA! that make comparison of findings difficult. First, although all three studies were theoretically driven and used SCT constructs, Move More for Life and FRESH START individually tailored newsletters and print materials for cancer survivors based on SCT constructs, whereas Project VIVA! culturally adapted newsletters and print materials to Hispanics and breast cancer survivors. Second, Move More for Life and FRESH START included mostly non-Hispanic whites, while Project VIVA! included Hispanic women, whom are largely underrepresented in the cancer survivorship literature. Lastly, Project VIVA! included face-to-face and brief telephone contact, where participants received a single one-on-one instructional training, opportunities to attend an exercise class once a month, and check-ins via telephone every two weeks, in addition to print materials, which may have impacted findings. Both the Move More for Life and FRESH START trials used only mailed print materials, which make comparison difficult.
Previous studies that have used culturally-tailored print media to promote physical activity in generally healthy populations have had mixed success [45]. Those reporting positive effects often individually tailor and culturally target materials to their audience to go beyond a basic understanding of theoretical concepts and incorporate individuals’ culture, life course and social support [23, 46]. Therefore, the null effect of the culturally-adapted versus standard exercise intervention group reported in the current study may be due to a lack of individual tailoring of SCT constructs in print materials. Participants in the current study received individual fitness goals based on their baseline fitness levels, which may have further minimized differences in physical activity and sedentary time outcomes between the culturally-adapted and standard exercise intervention groups.
All Project VIVA! participants reported significant increases in moderate, vigorous and total physical activity over time. This suggests that simply enrolling in a physical activity intervention and undergoing a physical assessment may be sufficient to promote behavior change among cancer survivors. Previous studies have similarly shown improvements in health behaviors in control participants, indicating the eagerness of individuals newly diagnosed with cancer and cancer survivors for health promotion and behavior change interventions [44, 47]. Even though there were no differences in changes in physical activity between intervention and control participants, women in the intervention groups (culturally-adapted and standard exercise) reported increases in barrier self-efficacy, which led to increases in walking and decreases in sedentary time, suggesting that the current study addressed the previously reported needs of Hispanic cancer survivors [48]. Although women in the intervention and control groups reported increases in social support from family, this only led to reduced sedentary time in the control group. This could be because the intervention groups were receiving support to do more moderate- and vigorous-intensity physical activity to meet national physical activity recommendations for cancer survivors [28], while women in the control groups’ family were supporting them to simply move more and sit less [6].
To our knowledge, Project VIVA! is the first study to date to explore the effects of changes in SCT variables on changes in physical activity and sedentary time in Hispanic breast cancer survivors, exclusively. The culturally-adapted and standard exercise interventions were systematically developed based on SCT principles and used evidence-based strategies for physical activity promotion among cancer survivors. This study included samples of Mexican American and Puerto Rican women in Houston, Texas and San Juan, Puerto Rico, respectively, maximizing geographic variability and increasing generalizability. Although unique, this study is not without limitations. Due to low adherence and sample size at follow-up, we were unable to assess objective measures of physical activity and sedentary time. For the subsample of participants on whom accelerometer-measured physical activity was available, there was a moderate (r=.380, p=.048) correlation between accelerometer-measured and self-reported physical activity. Most participants attended at least two group exercise sessions during the program, but women often cited childcare and scheduling conflicts as the primary reasons they were unable to attend sessions. Onsite childcare and additional group exercise session offerings (e.g., day and evening times) may have improved attendance and outcomes. Although this study included a homogenous sample of Mexican American and Puerto Rican breast cancer survivors, we cannot be certain that the results of this study are generalizable to breast cancer survivors not represented in this study, including low-income and other Hispanic populations. Finally, differences between the culturally-adapted and standard exercise interventions may have been too subtle to detect differences in outcomes between groups.
Hispanic breast cancer survivors are a vulnerable population in need of engaging in physical activity and pursuing health behavior change [11]. Culturally-adapted and theoretically grounded lifestyle interventions may help increase physical activity and reduce sedentary time in this population, leading to improved health outcomes and reduced mortality. Women who participated in Project VIVA! reported significant increases in physical activity regardless of group assignment, and women in the intervention group experienced significant increases in barrier self-efficacy, which contributed to increased physical activity and reduced sedentary time. Further research is needed to assess effects in other Hispanic and ethnic minority populations and to determine whether individually tailored and culturally targeted print materials may be more effective for increasing physical activity and reducing sedentary time among Hispanic breast cancer survivors.
Supplementary Material
Acknowledgments
This project was supported by the Center for Energy Balance in Cancer Prevention and Survivorship, Duncan Family Institute for Cancer Prevention and Risk Assessment, at The University of Texas MD Anderson Cancer Center (MDACC) and by the following NIH awards: U54 CA96297; U54 CA153511; K01 CA134550 (PI: Hughes); and P30 CA016672 (PROSPR Shared Resource). Scherezade Mama was supported by a cancer prevention fellowship through the MDACC Cancer Prevention Research Training Program (R25T CA057730, PI: Chang).
References
- 1.de Moor JS, et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22(4):561–70. doi: 10.1158/1055-9965.EPI-12-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62(1):10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 3.Avis NE, Deimling GT. Cancer survivorship and aging. Cancer. 2008;113(12 Suppl):3519–29. doi: 10.1002/cncr.23941. [DOI] [PubMed] [Google Scholar]
- 4.Rowland JH, Yancik R. Cancer survivorship: the interface of aging, comorbidity, and quality care. J Natl Cancer Inst. 2006;98(8):504–5. doi: 10.1093/jnci/djj154. [DOI] [PubMed] [Google Scholar]
- 5.World Cancer Research Fund International. Continuous Update Project Report: Diet, Nutrition, Physical Activity, and Breast Cancer Survivors. 2014 cited 2014 October 17; Available from: www.wcrf.org/sites/default/files/Breast-Cancer-Survivors-2014-Report.pdf.
- 6.Doyle C, et al. Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA Cancer J Clin. 2006;56(6):323–53. doi: 10.3322/canjclin.56.6.323. [DOI] [PubMed] [Google Scholar]
- 7.Smith WA, et al. Physical activity among cancer survivors and those with no history of cancer- a report from the National Health and Nutrition Examination Survey 2003–2006. Am J Transl Res. 2011;3(4):342–50. [PMC free article] [PubMed] [Google Scholar]
- 8.Schmitz K. Physical activity and breast cancer survivorship. Recent Results Cancer Res. 2011;186:189–215. doi: 10.1007/978-3-642-04231-7_8. [DOI] [PubMed] [Google Scholar]
- 9.Linsky A, Nyambose J, Battaglia TA. Lifestyle behaviors in Massachusetts adult cancer survivors. J Cancer Surviv. 2011;5(1):27–34. doi: 10.1007/s11764-010-0162-6. [DOI] [PubMed] [Google Scholar]
- 10.Weaver KE, et al. Cardiovascular risk factors among long-term survivors of breast, prostate, colorectal, and gynecologic cancers: a gap in survivorship care? J Cancer Surviv. 2013;7(2):253–61. doi: 10.1007/s11764-013-0267-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yaghjyan L, et al. Racial disparities in healthy behaviors and cancer screening among breast cancer survivors and women without cancer: National Health Interview Survey 2005. Cancer Causes Control. 2014;25(5):605–14. doi: 10.1007/s10552-014-0365-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Cancer Society. Cancer Facts & Figures for Hispancis/Latinos 2012–2014. Atlanta, GA: American Cancer Society; 2012. [Google Scholar]
- 13.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 14.Bandura A. The explanatory and predictive scope of self-efficacy theory. J Soc Clin Psychol. 1986;4(3):359–373. [Google Scholar]
- 15.Sharpe PA, et al. Correlates of physical activity among African American and white women. Am J Health Behav. 2008;32(6):701–13. doi: 10.5555/ajhb.2008.32.6.701. [DOI] [PubMed] [Google Scholar]
- 16.Fjeldsoe BS, Miller YD, Marshall AL. Social cognitive mediators of the effect of the MobileMums intervention on physical activity. Health Psychol. 2013;32(7):729–38. doi: 10.1037/a0027548. [DOI] [PubMed] [Google Scholar]
- 17.Van Dyck D, et al. Mediators of physical activity change in a behavioral modification program for type 2 diabetes patients. Int J Behav Nutr Phys Act. 2011;8:105. doi: 10.1186/1479-5868-8-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stahl T, et al. The importance of the social environment for physically active lifestyle--results from an international study. Soc Sci Med. 2001;52(1):1–10. doi: 10.1016/s0277-9536(00)00116-7. [DOI] [PubMed] [Google Scholar]
- 19.Pinto BM, Ciccolo JT. Physical activity motivation and cancer survivorship. Recent Results Cancer Res. 2011;186:367–87. doi: 10.1007/978-3-642-04231-7_16. [DOI] [PubMed] [Google Scholar]
- 20.Short CE, et al. Main outcomes of the Move More for Life Trial: a randomised controlled trial examining the effects of tailored-print and targeted-print materials for promoting physical activity among post-treatment breast cancer survivors. Psychooncology. 2015;24(7):771–8. doi: 10.1002/pon.3639. [DOI] [PubMed] [Google Scholar]
- 21.Pinto BM, Rabin C, Dunsiger S. Home-based exercise among cancer survivors: adherence and its predictors. Psychooncology. 2009;18(4):369–76. doi: 10.1002/pon.1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rogers LQ, et al. Exploring social cognitive theory constructs for promoting exercise among breast cancer patients. Cancer Nurs. 2004;27(6):462–73. doi: 10.1097/00002820-200411000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Keller CS, Coe K, Moore N. Addressing the demand for cultural relevance in intervention design. Health Promot Pract. 2014;15(5):654–63. doi: 10.1177/1524839914526204. [DOI] [PubMed] [Google Scholar]
- 24.Osborn CY, et al. A brief culturally tailored intervention for Puerto Ricans with type 2 diabetes. Health Educ Behav. 2010;37(6):849–62. doi: 10.1177/1090198110366004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.U.S. Census Bureau. 2013 American Community Survey. 2013 cited 2015 August 27; Available from: http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk.
- 26.U.S. Department of Health and Human Services. 2013 Poverty Guidelines. 2013 Jan 24;2013 cited 2015 August 27; Available from: http://aspe.hhs.gov/2013-poverty-guidelines. [Google Scholar]
- 27.Office of Disease Prevention and Health Promotion (ODPHP) 2008 Physical Activity Guidelines for Americans. U.S. Department of Health and Human Services; Washington, D.C: 2008. [Google Scholar]
- 28.Pescatello LS, editor. ACSM’s Guidelines for Exercise Testing and Prescription. 9. American College of Sports Medicine; Baltimore, MD: 2010. [DOI] [PubMed] [Google Scholar]
- 29.Duncan TE, McAuley E. Social support and efficacy cognitions in exercise adherence: a latent growth curve analysis. J Behav Med. 1993;16(2):199–218. doi: 10.1007/BF00844893. [DOI] [PubMed] [Google Scholar]
- 30.McAuley E. The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. J Behav Med. 1992;15(1):65–88. doi: 10.1007/BF00848378. [DOI] [PubMed] [Google Scholar]
- 31.McAuley E, et al. Enhancing exercise adherence in middle-aged males and females. Prev Med. 1994;23(4):498–506. doi: 10.1006/pmed.1994.1068. [DOI] [PubMed] [Google Scholar]
- 32.McAuley E, et al. Exercise self-efficacy in older adults: social, affective, and behavioral influences. Ann Behav Med. 2003;25(1):1–7. doi: 10.1207/S15324796ABM2501_01. [DOI] [PubMed] [Google Scholar]
- 33.Marcus BH, Owen N. Motivational readiness, self-efficacy and decision making for exercise. Journal of Applied Social Psychology. 1992;22:3–16. [Google Scholar]
- 34.Marcus BH, Rakowski W, Rossi JS. Assessing motivational readiness and decision making for exercise. Health Psychol. 1992;11(4):257–61. doi: 10.1037//0278-6133.11.4.257. [DOI] [PubMed] [Google Scholar]
- 35.Marcus BH, et al. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63(1):60–6. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 36.Basen-Engquist K, et al. Validity and reliability of a cancer survivors’ exercise barriers self-efficacy scale. Ann Behav Med. 2009;37(Suppl):S185. [Google Scholar]
- 37.Basen-Engquist K, et al. Design of the Steps to Health Study of Physical Activity in Survivors of Endometrial Cancer: Testing a Social Cognitive Theory Model. Psychol Sport Exerc. 2011;12(1):27–35. doi: 10.1016/j.psychsport.2010.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sallis JF, et al. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–36. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 39.Craig CL, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 40.Clark BK, et al. Adults’ past-day recall of sedentary time: reliability, validity, and responsiveness. Med Sci Sports Exerc. 2013;45(6):1198–207. doi: 10.1249/MSS.0b013e3182837f57. [DOI] [PubMed] [Google Scholar]
- 41.Rock CL, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62(4):243–74. doi: 10.3322/caac.21142. [DOI] [PubMed] [Google Scholar]
- 42.Short CE, et al. Move more for life: the protocol for a randomised efficacy trial of a tailored-print physical activity intervention for post-treatment breast cancer survivors. BMC Cancer. 2012;12:172. doi: 10.1186/1471-2407-12-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Short CE, James EL, Plotnikoff RC. Theory-and evidence-based development and process evaluation of the Move More for Life program: a tailored-print intervention designed to promote physical activity among post-treatment breast cancer survivors. Int J Behav Nutr Phys Act. 2013;10:124. doi: 10.1186/1479-5868-10-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Demark-Wahnefried W, et al. Main outcomes of the FRESH START trial: a sequentially tailored, diet and exercise mailed print intervention among breast and prostate cancer survivors. J Clin Oncol. 2007;25(19):2709–18. doi: 10.1200/JCO.2007.10.7094. [DOI] [PubMed] [Google Scholar]
- 45.Yap TL, Davis LS. Physical activity: the science of health promotion through tailored messages. Rehabil Nurs. 2008;33(2):55–62. doi: 10.1002/j.2048-7940.2008.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 46.Bull FC, Kreuter MW, Scharff DP. Effects of tailored, personalized and general health messages on physical activity. Patient Educ Couns. 1999;36(2):181–92. doi: 10.1016/s0738-3991(98)00134-7. [DOI] [PubMed] [Google Scholar]
- 47.Gritz ER, et al. Successes and failures of the teachable moment: smoking cessation in cancer patients. Cancer. 2006;106(1):17–27. doi: 10.1002/cncr.21598. [DOI] [PubMed] [Google Scholar]
- 48.Spector D, Battaglini C, Groff D. Perceived exercise barriers and facilitators among ethnically diverse breast cancer survivors. Oncol Nurs Forum. 2013;40(5):472–80. doi: 10.1188/13.ONF.472-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.